Abstract
Objectives: To introduce a psychological model of behaviour; the COM-B model and describe how this has been used in combination with the behaviour change wheel (BCW) in developing an intervention which aims to promote regular, long-term use of hearing aids by adults with acquired hearing loss. Design: Qualitative structured interview study using the COM-B model to identify the determinants of behavioural planning on the part of audiologists; a potentially important factor in encouraging long-term hearing-aid use. Study sample: Ten audiologists drawn from a random sample of five English audiology departments. Results: The analysis suggests that behavioural planning might be more likely to occur if audiologists’ psychological capability, physical and social opportunity, and reflective and automatic motivation were addressed. This analysis forms the basis of an intervention design, using the BCW, to encourage behavioural planning by audiologists and subsequent hearing-aid use by people with hearing loss. Conclusions: The COM-B model and BCW can be applied successfully in the context of audiology to analyse the behaviour of both people with hearing loss and professionals working with them, supplying information that is being used in intervention design. The effectiveness of the intervention will be tested in a clinical trial.
The use of theory is advocated by the Medical Research Council (MRC) framework for the development and evaluation of complex interventions (Campbell et al, Citation2000; Craig et al, Citation2008) and by others working in implementation research (Eccles et al, Citation2012; French et al, Citation2012). In development, it should result in interventions that are more likely to be successful and, in evaluation, it can elucidate why and how different components of an intervention contribute to overall effectiveness. The MRC framework is relevant for audiology because much of what audiologists do when interacting with people with hearing loss could be considered self-management support (SMS); that is, helping people develop the knowledge and skills they need to manage their hearing loss more effectively. SMS processes have been operationalized as those that inform the patient and those that involve the patient (Pearson et al, Citation2007). The multi-component nature of SMS means it is a classic example of a complex intervention (Campbell et al, Citation2000).
There are many theories of behaviour change often with overlapping, but differently named, constructs (Michie et al, Citation2014). In addition, there is little guidance on how to choose an appropriate theory for a particular context (Michie et al, Citation2011). This diversity and complexity has been cited as a potential reason why theory is under-used in intervention design and evaluation making replication, implementation, evaluation and improvement more difficult (Eccles et al, Citation2012; Michie et al, Citation2011). Researchers working in this area argue that there is a need for a comprehensive supra-theory model of behaviour applicable across contexts.
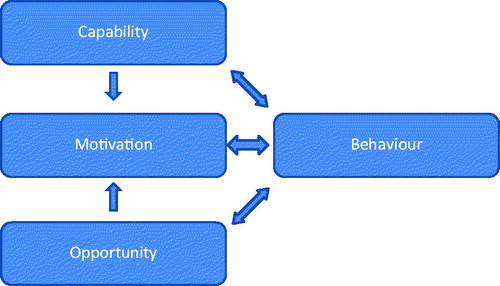
Michie et al (Citation2014) propose that people need capability (C), opportunity (O) and motivation (M) to perform a behaviour (B) and developed the COM-B model to guide understanding of behaviour in context and develop behavioural targets as a basis for intervention design. The model provides a simple starting point and can signpost to specific psychological theories of, for example, motivation if a more granular theoretical understanding of behaviour is required.
The model proposes that for someone to engage in a particular behaviour (B) at a given moment they must be physically and psychologically able (C) and have the social and physical opportunity (O) to do the behaviour and, in addition, want or need to do the behaviour more than any other competing behaviours at that moment. This inclusive definition of motivation (M) covers basic drives and automatic processes such as habit and impulses as well as reflective processes such as intention and choice. If a desired behaviour is not occurring (or an undesirable behaviour occurring) then an analysis of the determinants of the behaviour will help to define what needs to shift in order for the desired behaviour to occur (or the unwanted behaviour to cease).
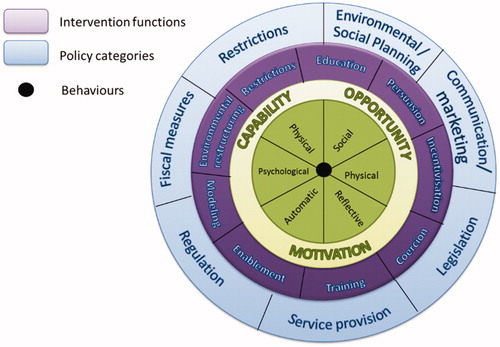
The COM-B model shown in has been developed as part of a larger system of behaviour shown in called the behaviour change wheel (BCW) (Michie et al, Citation2011, Citation2014) which is designed to help intervention designers move from a behavioural analysis of the problem to intervention design using the evidence-base.
The BCW allows developers to identify, in a systematic and transparent way, intervention functions and policy categories that could bring about change. Definitions of the nine interventions functions and seven policy categories are given in .
Table 1. Intervention function and policy category definitions from the BCW.
Once intervention functions and policy categories have been selected, the final step in intervention design is to step outside the Wheel and identify specific behaviour change techniques and modes of delivery that are likely to be effective and that can be linked back to psychological theory. The BCW guide (Michie et al, Citation2014) provides advice on how to do this. This linking of theory with intervention design is consistent with the advice given in the MRC guidance on the development and evaluation of complex interventions (Campbell et al, Citation2000; Craig et al, Citation2008).
The COM-B model has been applied successfully in a number of contexts (e.g. Alexander et al, Citation2014; Jackson et al, Citation2014) but not yet in audiology. This paper therefore details a worked example of how the COM-B model and BCW have been applied in the context of hearing healthcare to guide the development and design of an intervention to improve adherence to hearing-aid use.
The first step in intervention design, according to the BCW, is to define the problem in behavioural terms (Michie et al, Citation2014). Despite evidence that hearing-aid use can ameliorate some of the negative consequences of hearing loss (Chisolm et al, Citation2004; Chisolm & Arnold, Citation2012; Mulrow et al, Citation1990), the charity Action On Hearing Loss estimate that, although 2 million people in the UK have hearing aids, only 1.4 million use them regularly. This is supported by surveys of hearing-aid use with estimates of non-use varying from 5–40% (Gimsing, Citation2008; Hougaard & Ruf, Citation2011; Kochkin, Citation2000; Lupsakko et al, Citation2005; Smeeth et al, Citation2002; Vuorialho et al, Citation2006). Thus, the behaviour of interest in this case is the regular, long-term use of hearing aids by adults with acquired hearing loss.
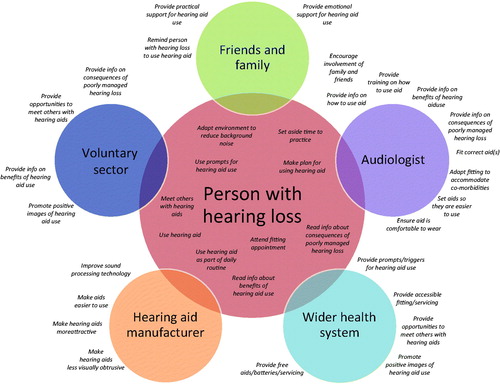
All behaviours, including hearing-aid use, occur within a system of other competing or contributing behaviours. The second step of the BCW process is to select a target behaviour which could address the behavioural problem. In the case of hearing-aid use, research suggests that this patient behaviour may be partly dependent on a range of other peoples’ behaviour, including hearing healthcare professionals. This inter-relationship of patient and professional behaviour in mediating outcome is embodied in conceptual frameworks of healthcare systems such as the chronic care model (CCM) (Bodenheimer et al, Citation2002). The results of a scoping review of reasons for non-use of hearing aids (McCormack & Fortnum, Citation2013), supplemented with additional potentially relevant behaviours informed by psychological theory, results in a ‘conceptual map’ of the system of behaviours that might be relevant in encouraging long-term, regular hearing-aid use amongst adults with acquired hearing loss, as shown in .
This map demonstrates the complexity inherent in most behavioural contexts. In their guide (Michie et al, Citation2014), the developers of the BCW suggest using the following criteria to identify which behaviour(s) to target:
Likely impact
Ease of implementation
Likely spillover (collateral impact)
Ease of measurement
Applying these criteria to the behaviours in the system in suggests that four behaviours present promising targets for intervention development:
Providing information about the benefits of hearing-aid use
Providing information about the consequences of poorly managed hearing loss, i.e. the negative consequences of non-use
Providing prompts or triggers for hearing-aid use
Developing a plan to promote habitual hearing-aid use
Early development work following the BCW process and other research suggests that these behaviours are not currently taking place in audiology appointments (Grenness et al, Citation2015) but that they may be relatively easy to implement. Changing these behaviours is likely to influence patient behaviour (Mead & Bower, Citation2002; Rogers et al, Citation2005; Legare et al, Citation2010; Lally & Gardner, Citation2013) and their implementation should be reasonably easy to measure.
The third step of the BCW involves developing a clear specification of who will perform the target behaviours, what they need to do differently to achieve change, where and when they need to do it and, if necessary, how often and with whom. This specification is given in .
Table 2. Specification of the target behaviours.
Audiologists will need to provide the written material, discuss cues for hearing-aid use, and engage in collaborative planning to promote habitual hearing-aid use with people with hearing loss.
The fourth step is to use the COM-B model to analyse whether the targets of the intervention, audiologists in this case, have the capability, opportunity, and motivation to carry out the behaviour. The first three specified behaviours are relatively simple. Audiologists demonstrably already have the physical and psychological capability, social opportunity, and reflective and automatic motivation to distribute written material because this already forms part of their standard practice. The only thing they currently lack is the physical opportunity afforded by actually adding to the content of the currently supplied material and making it accessible.
The final behaviour is more complex. In the context of hearing healthcare, informing and involving self-management support (SMS) processes have been delineated and advocated but not clearly behaviourally defined (Grenness et al, Citation2014a,Citationb) and surveys of patient experiences of auditory rehabilitation show that SMS processes such as collaborative behavioural planning are not integrated into routine clinical practice (Laplante-Levesque et al, Citation2010, Citation2012; Kelly et al, Citation2013; Grenness et al, Citation2014a, Citation2015) despite the fact that stakeholders, including people with hearing loss, agree they should be (Barker et al, Citation2015).
This paper describes the methods and results of a qualitative structured interview study based on the COM-B model that was used to investigate what needs to change in terms of capability, opportunity, and motivation for audiologists to engage in collaborative behavioural planning for hearing-aid use.
Methods
A sample of 10 audiologists participated in this study. They were recruited by randomly sampling five audiology services from a comprehensive list of NHS audiology departments in England, compiled by combining information from lists provided by regional audiology leads at the British Academy of Audiology and third sector providers. Within each of these departments, two staff members were randomly sampled to take part in data collection. The figure of 10 audiologists represented a balance between the constraints of data collection and analysis and the wish to obtain a representative sample of variation in behaviour and its determinants. Audiologists working autonomously in any NHS audiology department in England were eligible for inclusion. This included part-time staff and student audiologists who were working without direct supervision. It excluded student audiologists who were seeing patients but only with another member of staff present in a supervisory capacity.
The topic guide for the structured interviews, developed using BCW guidance (Michie et al, Citation2014), is given in Appendix 1. No amendments were felt necessary following pilot interviews with two experienced audiologists. One researcher (FB) conducted all the interviews which took place in participants’ audiology departments, with only the audiologist and researcher present. The interviews were video recorded to allow for accurate transcription prior to analysis. Video recording was used for convenience as it had been used in a parallel observational study of audiologist behaviour during hearing-aid fittings immediately before the structured interview took place. The video recordings were transcribed by one of the researchers (FB) and the video recording was then erased. A three-stage process was used for transcription to minimize errors. The video was viewed initially without transcription so that the researcher could re-familiarize herself with the material. The main transcription process then took place followed by a third viewing where any errors were corrected.
Anonymized transcripts of the structured interviews were analysed independently by two researchers using NVivo 10 software. The COM-B model was used as a deductive framework for the analysis (Boyatzis, Citation1998). The researchers then compared their coding and resolved discrepancies by discussion to produce an analysis of what would help or hinder the creation of a collaborative behavioural plan in the context of hearing aid fittings.
The study received NHS ethical approval from NRES committee Yorkshire and the Humber - Leeds West and from the University of Surrey Ethics Committee (REC reference 14/YH/1252). Data collection took place in April and May 2015.
Results
Of the five departments initially approached, two declined to take part and two further departments were selected, again at random, both of whom consented to take part. The five participating departments covered a wide geographical area of England. The gender ratio of the audiologists was 8:2 female:male. All the audiologists were qualified and had a range of experience from eighteen months to over ten years in post. Despite this range of experience, there was considerable consistency in the audiologists’ responses such that data saturation was reached after six interviews. Consistent with the COM-B model and interview structure, responses were grouped into those relating to capability, opportunity and motivation.
Capability
Audiologists reported that they felt that physical capability was not an issue for them in terms of making a behavioural plan with patients; the behaviour itself requires few physical skills beyond typing and no physical strength or stamina e.g.
‘No you don’t need to have… any physical strength for that.’ - Audiologist 7
When considering psychological capability however, they reported that it would be important for them to know why they were making the behavioural plan because being able to see benefits for either themselves or their patients was an important motivating factor:
‘I think you’ve got to have the understanding behind it and the belief that it is doing some good otherwise you can’t really see the point in doing it.’ - Audiologist 1
They also reported that knowing how to make the plan would be important because it would impact on how easily and quickly they could do it and how confident they were or appeared to be in front of their patients:
‘Yeah in order to build any confidence for the patient they need to feel confident in you. So if you look like you don’t know what you’re doing… that to them… as a patient myself in other departments you definitely feel like ‘do they know what they’re doing here?’ You definitely need to feel confident in doing it.’ - Audiologist 3
Participants reported that other psychological skills such as being adaptable were also important for being able to develop a plan with each patient but that they already possessed these skills due to the nature of the other tasks they have to perform as audiologists:
‘I think you would already have the skills because already we’re adapting depending on who we see.’ - Audiologist 10
However, they also reported that this was a skill that developed with experience:
‘It might not come so easily in the beginning but I’m sure the more you do it, it’s like anything, you’d… you’d become more adept at doing it over time.’ - Audiologist 9
Mental stamina in the form of tiredness at the end of a long clinic was also reported to be a potential barrier to behavioural planning for some of the audiologists:
‘When you’ve got the same appointment over and over again it can get quite tiring.’ - Audiologist 1
Opportunity
Both physical and social opportunity were reported as important in determining whether behavioural planning was likely to occur. Nine of the ten audiologists were concerned that they already felt pressured for time in their fitting appointments. Juggling the other processes that need to happen in a fitting (such as real-ear measurement, explaining how to use the hearing aid, batteries, and controls, and discussing expectations) with the need to do something new or different within the time available was a significant area of concern:
‘Yes, especially if you’re under pressure and things like that… time… that’s important. Already you’re struggling sometimes so… something else as well, that’s going to put pressure on that.’ - Audiologist 6
Participants also reported that having access to a template onscreen that could be easily linked to the existing electronic patient record was important as it would impact on how easy it was to access the information at subsequent appointments, making it more likely that they would see a benefit in completing the plan and also impacting on their use of time:
‘Then it’s just a click of a button and it’s… if it was just a two minute thing you could do it every time.’ - Audiologist 2
Having some sort of prompt or trigger to remind them to make the plan was also reported to be important:
‘It would just nudge me, remind me to do it.’ - Audiologist 8
The social opportunity afforded by being part of a team or culture where everyone implemented the plan together was important for all the participants. This was a factor both in terms of the relationship to motivation and in terms of the ready availability of practical advice and support should something not go as expected:
‘If you see somebody hasn’t done it there is the temptation to just think ‘well they haven’t done it, why would I?’ You know if time’s running out ‘if they didn’t do it, so I can leave it.’ - Audiologist 3
If something goes wrong or you’re unsure or something there’s always someone to ask whereas if it’s just you or a couple of you that’s… you’re just on your own really.’ - Audiologist 6
Visible managerial support for the plan was also seen as important although less so than the practical support offered by peers.
Motivation
Participants reported that both reflective and automatic motivation played a role in determining the likelihood of them carrying out behavioural planning. In terms of reflective motivation, all the respondents reported that if they believed the plan was a good thing to do then they would be more likely to do it. This was mediated by their psychological capability in knowing why they were doing it. Some of the participants reported that they had or were carrying out other behaviours which they believed were a waste of time and that these were the things that they tended to omit or do quickly if they were under time pressure:
‘I think you’ve got to have the understanding behind it and the belief that it is doing some good otherwise you can’t really see the point in doing it.’ - Audiologist 1
‘If I’m short of time that will be the thing… the things that I will not do are the things that I don’t believe in.’ - Audiologist 8
All the participants reported that making a plan in advance for how they would incorporate the behavioural plan into their fitting appointments would be helpful and make it more likely that they would remember to do it and not miss it out for some other reason such as time pressure:
‘It’s really important to have a plan. You always have a plan of what you’re going to do in an appointment anyway, the order that you’re going to do it in, which helps you to structure your appointment and time manage it better.’ - Audiologist 3
In terms of automatic motivation involving emotional reactions, desires (wants and needs), impulses, reflex responses, and habits, some audiologists reported being more motivated by the desire to see a positive outcome either directly for themselves or indirectly through evidence of benefit to the patient:
‘You feel like if you’re getting something out of it then it’s that positive reinforcement… you want to do it again and again.’ - Audiologist 2
Others reported being more motivated by the need to avoid a negative consequence should they fail to make a plan with their patients, again either for themselves or indirectly though patient outcomes:
‘You know if you miss that out then it’s not going to be as beneficial. You’re also affecting the patients getting used to the hearing aid which will then, they might not wear it, it’s a waste of resources. Erm if you’re always not doing it then it’s going to come back on you.’ - Audiologist 1
All the respondents said that incorporating the plan into their clinical routine and making it habitual would be helpful as they would be less likely to forget to do it and would be able to do it without thinking which required less mental effort:
‘You don’t have to think about it each time. You can just erm sort of get on and do it and it doesn’t take so much thinking. You can just do it much more easily.’ - Audiologist 9
In summary, therefore, the audiologists interviewed in this study reported psychological capability, physical and social opportunity, and reflective and automatic motivation as important drivers for behavioural planning in hearing-aid fitting appointments.
Discussion
This study formed part of an intervention development process and aimed to sample a representative group of audiologists currently carrying out routine hearing-aid fittings and to seek their opinion on the factors mediating the introduction and maintenance of a new behaviour in this context. The sample was drawn from varied locations across England and included recently qualified audiologists up to those with at least 10 years’ experience in adult rehabilitation. Despite the small heterogeneous sample, there was considerable consistency in the responses. A structured approach based on the COM-B model allowed identification of internal and external drivers of behaviour including both volitional and non-volitional factors. The implications of this research are that hearing-aid use is a complex behavioural problem, likely to be influenced in part by collaborative behaviours between people with hearing loss and their audiologists such as creating a behavioural plan for hearing-aid use. Such collaborative behaviours are not currently part of routine audiological practice. Changing this so that collaborative behavioural planning becomes part of routine practice will require a complex intervention that addresses psychological capability, physical and social opportunity, reflective and automatic motivation.
The COM-B model and BCW are relatively recent developments in behavioural psychology and have been untested in the context of audiology. In this example, the COM-B model was helpful in supplementing the results of a scoping review of reported reasons for non-use of hearing aids to develop a comprehensive conceptual map of the system of behaviours that might influence hearing-aid use. The individual studies cited in the scoping review collected data in a range of ways using surveys, interviews or focus groups; sometimes using closed questions and sometimes seeking open responses from participants. However, gathering data using only patient feedback without using a comprehensive behavioural model to guide data collection and analysis risks missing potentially important determinants such as habit over which people may have limited insight. Using a comprehensive supra-theory model such as COM-B, as opposed to a single theory focusing on, for example, reflective motivational processes, helped develop a map of the full system of behaviours that might influence the behavioural problem of hearing-aid use and facilitated a comprehensive behavioural analysis of the determinants of behavioural planning by audiologists. The inclusion of non-volitional processes in the model highlighted the potential importance of habit formation for both patients and audiologists in this context. The formation and maintenance of habitual behaviour has not been studied in the context of hearing healthcare. Habits can be defined as behaviours enacted automatically in response to a context in which the behaviour has taken place in the past on a repeated basis (Lally & Gardner, Citation2013). This is potentially relevant to hearing-aid use where, over the long term, hearing-aid use needs to be repeated on a regular basis and also to clinical behaviour where care processes need to be repeated on a regular basis. Because this area has not been studied, we do not know whether habitual hearing-aid use is more likely to be maintained than non-habitual use but research in other behavioural contexts suggests that it might (Verplanken et al, Citation1998; Lally et al, Citation2008; Lally & Gardner, Citation2013).
In much of the literature on behaviour change, healthcare professional behaviour and patient behaviour are treated separately. Often separate models are used to analyse healthcare professional behaviour and patient behaviour. For example, normalization process theory (NPT) has been proposed as a method for analysing healthcare professional behaviour and embedding new clinical behaviours into a clinical routine (May et al, Citation2009).This introduces additional levels of complexity and, taken to its logical conclusion, this would imply that different psychological models are necessary in every context. The COM-B model suggests the reverse; that a truly comprehensive model can be flexible enough to analyse any behaviour, incorporating the context, not as a separate construct but as a natural consequence of using the model.
Involving audiologists in intervention development at the stage of identifying and analysing what needs to change parallels involving patients in self-management. Using the COM-B model to investigate determinants of audiologist behaviour means that the intervention is not researcher-led but audiologist-led, consistent with the principles of community-based participatory research (Israel et al, Citation1998; Greenhalgh et al, Citation2004) and means implementation is person-centred (Yardley et al, Citation2015). The COM-B model facilitates this because it is possible to use the same model to investigate both sets of inter-related behaviour.
On a practical level, the entry level simplicity of the COM-B model is potentially useful for non-psychologists yet it can also be linked back to specific psychological theories of, for example, motivation for those who need to explore at a deeper theoretical level. Thus, it can be used alongside individual theories of behaviour such as social cognitive theory but provides a useful common language that can be used to link and compare the range of individual theories. Linking the COM-B model to the BCW allows a systematic approach to be taken in subsequent intervention development and evaluation (Michie et al, Citation2011, Citation2014). This should be appealing to funding bodies, elucidating the path taken in intervention development from problem identification through theory to intervention design and implementation.
Future research
The developers of the COM-B model and BCW provide a systematic way to move from behavioural analysis to identifying potential intervention functions and policy categories which might bring about change. The step-by-step operationalization from problem definition to intervention development and evaluation is one that can be followed across behaviours and contexts. shows the grid which can be used to move towards identifying intervention functions.
Table 3. Identifying intervention functions.
The shaded squares highlight where evidence or consensus suggests that a function may be effective for addressing a particular behavioural determinant. From this grid it is possible to see how one intervention function may serve to influence more than one determinant, i.e. training can be used to address physical and psychological capability, physical opportunity, and automatic motivation. However, a choice then needs to be made about which intervention functions are most appropriate or have the best potential chance of success in bringing about change in a particular context. This can be done using the APEASE criteria (Michie et al, Citation2014) which are detailed in .
Table 4. The APEASE criteria.
Using these criteria along with the grid and the behavioural analysis taken from the structured interviews with audiologists, a complex intervention has been designed that uses a combination of the intervention functions of education, persuasion, coercion, training, environmental restructuring, and enablement that aims to reduce barriers to and increase the likelihood of audiologists providing information about the benefits of hearing-aid use and consequences of non-use, discussing prompts for hearing-aid use and making behavioural plans with patients in hearing-aid fittings. The effectiveness of this intervention will be tested using mixed methods to evaluate which elements of the intervention are the most effective in changing audiologist and patient behaviour. This is consistent with the MRC framework for the development and evaluation of complex interventions (Craig et al, Citation2008) and NICE guidance on behaviour change (National Institute for Health and Care Excellence, Citation2014).
Conclusions
Although relatively new and untested in the context of audiology, the use of the COM-B model has laid solid foundations for intervention development that can be linked back to psychological theory to address the problem of hearing-aid use. This worked example shows that the COM-B model and BCW can be used in intervention development in the context of audiology.
| Abbreviations | ||
| BCW | = | Behaviour change wheel |
| CCM | = | Chronic care model |
| COM-B | = | Capability, opportunity, motivation to perform a behaviour |
| LTC | = | Long term condition |
| MRC | = | Medical research council |
| NPT | = | Normalization process theory |
| SMS | = | Self-management support |
Supplemental Material
Download MS Word (18.2 KB)Acknowledgements
The authors would like to thank the participating departments and individual clinicians who took part in this research.
Declaration of interest
The authors report no conflicts of interest.
References
- Alexander K.E., Brijnath B. & Mazza D. 2014. Barriers and enablers to delivery of the Healthy Kids Check: an analysis informed by the Theoretical Domains Framework and COM-B model. Implement Sci, 9, 60
- Barker F., Munro K.J. & de Lusignan S. 2015. Supporting living well with hearing loss: A Delphi review of self-management support. Int J Audiol, 54(10), 691–699.
- Bodenheimer T., Wagner E.H. & Grumbach K. 2002. Improving primary care for patients with chronic illness. JAMA, 288, 1775–1779.
- Boyatzis R.E. 1998. Transforming Qualitative Information: Thematic Analysis and Code Development. London: Sage.
- Campbell M., Fitzpatrick R., Haines A., Kinmonth A.L., Sandercock P., et al. 2000. Framework for design and evaluation of complex interventions to improve health. BMJ, 321, 694–696.
- Chisolm T.H., Abrams H.B. & McArdle R. 2004. Short- and long-term outcomes of adult audiological rehabilitation. Ear Hear, 25, 464–477.
- Chisolm, T.H. & Arnold, M. 2012. Evidence about the effectiveness of aural rehabilitation programs for adults In: L. Wong & L. Hickson (eds.), Evidence-Based Practice in Audiology, San Diego, CA: Plural p. 237.
- Craig P., Dieppe P., Macintyre S., Michie S., Nazareth I. & Petticrew M. 2008. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ, 337, 1655.
- Eccles M.P., Grimshaw J.M., MacLennan G., Bonetti D., Glidewell L., et al. 2012. Explaining clinical behaviors using multiple theoretical models. Implement Sci, 7, 99.
- French S.D., Green S.E., O’Connor D.A., McKenzie J.E., Francis J.J., et al. 2012. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci, 7, 38.
- Gimsing S. 2008. Use of hearing aids five years after issue. Ugeskrift for Laeger, 170, 3407–3411.
- Greenhalgh T., Robert G., Macfarlane F., Bate P. & Kyriakidou O. 2004. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q, 82, 581–629.
- Grenness C., Hickson L., Laplante-Levesque A. & Davidson B. 2014a. Patient-centred audiological rehabilitation: perspectives of older adults who own hearing aids. Int J Audiol, 53, S68–S75.
- Grenness C., Hickson L., Laplante-Levesque A. & Davidson B. 2014b. Patient-centred care: A review for rehabilitative audiologists. Int J Audiol, 53, S60–S67.
- Grenness C., Hickson L., Laplante-Levesque A., Meyer C. & Davidson B. 2015. The nature of communication throughout diagnosis and management planning in initial audiologic rehabilitation consultations. J Am Acad Audiol, 26, 36–50.
- Hougaard S. & Ruf S. 2011. EuroTrak I: A consumer survey about hearing aids in Germany. France, and the UK. Hearing Rev, 18, 12–28.
- Israel B.A., Schulz A.J., Parker E.A. & Becker A.B. 1998. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health , 19, 173–202.
- Jackson C., Eliasson L., Barber N. & Weinman J. 2014. Applying COM-B to medication adherence. Eur Health Psychol, 16, 7–17.
- Kelly T.B., Tolson D., Day T., McColgan G., Kroll T. & Maclaren W. 2013. Older people's views on what they need to successfully adjust to life with a hearing aid. Health Soc Care Comm, 21, 293–302.
- Kochkin S. 2000. MarkeTrak V: “Why my hearing aids are in the drawer”: the consumers' perspective. Hearing J, 53, 34–42.
- Lally P., Chipperfield A. & Wardle J. 2008. Healthy habits: efficacy of simple advice on weight control based on a habit-formation model. Int J Obes (Lond), 32, 700–707.
- Lally P. & Gardner B. 2013. Promoting habit formation. Health Psychol Rev, 7, S137–S158.
- Laplante-Levesque A., Hickson L. & Worrall L. 2010. Rehabilitation of older adults with hearing impairment: a critical review. J Aging Health, 22, 143–153.
- Laplante-Levesque A., Knudsen L.V., Preminger J.E., Jones L., Nielsen C., et al. 2012. Hearing help-seeking and rehabilitation: perspectives of adults with hearing impairment. Int J Audiol, 51, 93–102.
- Legare F., Ratte S., Stacey D., Kryworuchko J., Gravel K., et al. 2010. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev, CD006732.
- Lupsakko T.A., Kautiainen H.J. & Sulkava R. 2005. The non-use of hearing aids in people aged 75 years and over in the city of Kuopio in Finland. Eur Arch Otorhinolaryngol, 262, 165–169.
- May C.R., Mair F., Finch T., MacFarlane A., Dowrick C., et al. 2009. Development of a theory of implementation and integration: Normalization Process Theory. Implement Sci, 4, 29
- McCormack A. & Fortnum H. 2013. Why do people fitted with hearing aids not wear them? Int J Audiol, 52, 360–368.
- Mead N. & Bower P. 2002. Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ Couns, 48, 51–61.
- Michie S., Atkins L. & West R. 2014. The behaviour Change Wheel: A Guide to Designing Interventions, 1st edn. London: Silverback.
- Michie S., West R., Campbell R., Brown J. & Gainforth H. 2014. ABC of Behaviour Change Theories, 1st edn. London: Silverback.
- Michie S., van Stralen M.M. & West R. 2011. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci, 6, 42.
- Mulrow C.D., Aguilar C., Endicott J.E., Velez R., Tuley M.R., et al. 1990. Association between hearing impairment and the quality of life of elderly individuals. J Am Geriatr Soc, 38, 45–50.
- National Institute for Health and Care Excellence. 2014. Behaviour Change: Individual Approaches (PH49). [Online] Available from: http://guidance.nice.org.uk/PH49 [Accessed: 11th August 2014].
- Pearson M.L., Mattke S., Shaw R., Ridgely M.S. & Wiseman S.H. 2007. Patient Self-Management Support Programs. Rockville, MD: Agency for Healthcare Research and Quality.
- Rogers A., Kennedy A., Nelson E. & Robinson A. 2005. Uncovering the limits of patient-centeredness: implementing a self-management trial for chronic illness. Qual Health Res, 15, 224–239.
- Smeeth L., Fletcher A.E., Ng E.S., Stirling S., Nunes M., et al. 2002. Reduced hearing, ownership, and use of hearing aids in elderly people in the UK-the MRC Trial of the Assessment and Management of Older People in the Community: a cross-sectional survey. Lancet, 359, 1466–1470.
- Verplanken B., Aarts H., Knippenberg A. & Moonen A. 1998. Habit versus planned behaviour: A field experiment. Brit J Soc Psychol, 37, 111–128.
- Vuorialho A., Sorri M., Nuojua I. & Muhli A. 2006. Changes in hearing aid use over the past 20 years. Eur Arch Otorhinolaryngol, 263, 355–360.
- Yardley L., Morrison L., Bradbury K. & Muller I. 2015. The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res, 17, 30.