ABSTRACT
Aim: To determine if pro-forma based management improves standards of care delivered by junior doctors in chronic obstructive pulmonary disease (COPD) patients in the Emergency Department (ED). Introduction: National COPD audits have found large variations in ED standards of care compared to guidelines. They concluded that the publication of guidelines itself does not translate to an improvement in care. Method: A pro-forma based on the British Thoracic Society Guidelines on COPD, 1997, NICE Guidelines CG12, 2004 and Non Invasive Ventilation (NIV), 2002 was devised and implemented following targeted education. Data were collected pre and post pro-forma implementation and analysed. The primary end point was categorisation of respiratory failure as it was felt that this concept was fundamental in COPD management. Secondary endpoints included the administration of controlled oxygen, repeat blood gases and appropriate referral for NIV. Results: There were a total of 55 patients in each group. The correct categorisation of respiratory failure improved significantly from 4% in the pre- compared to 89% (p < 0.0001) in the post-intervention group. Similarly the administration of controlled oxygen (47% compared to 92%, p < 0.0001), repeat arterial blood gases (50% compared to 83%, p = 0.0098), and appropriate referral for NIV (33% compared to 100%, p = 0.0023) showed significant improvement after the pro-forma was introduced. Conclusion: Pro-forma aided management significantly improves the standards of care in COPD patients in the ED.
INTRODUCTION
Acute exacerbations of chronic obstructive pulmonary disease (COPD) are the second commonest cause of acute medical admission in the United Kingdom (UK), accounting for over 12% of the total (Citation1). These acute episodes carry a mortality rate of up to 15%, and, a third requires readmission within 90 days (Citation2–4). A significant proportion of these patients are admitted via Emergency Departments (ED) so a consistent, evidence-based approach to the management of these patients is vital.
Table 1. Pre- and postintervention main results
The British Thoracic Society (BTS) published guidelines on the management of COPD in primary and secondary care in 1997 (Citation5), followed by the National Institute for Health and Clinical Excellence (NICE) in 2004 (Citation6). In spite of these guidelines, national audits in 1997, 2001 and 2003 have found large variations in standards of care between hospitals (Citation3, Citation7). Similarly, audits done on a local level looking at adherence to other BTS/NICE guidelines have shown poor compliance (Citation8–12).
Departmental management algorithms in the form of pre-printed paperwork have been shown to be effective in improving guideline adherence in a number of clinical areas within the ED (Citation13–18). This study aimed to demonstrate whether targeted education and the introduction of a departmental pro forma would lead to an improvement in the correct categorisation of respiratory failure and management of patients presenting to the ED with acute exacerbations of COPD in accordance with guidelines.
METHODS
Study design and participants
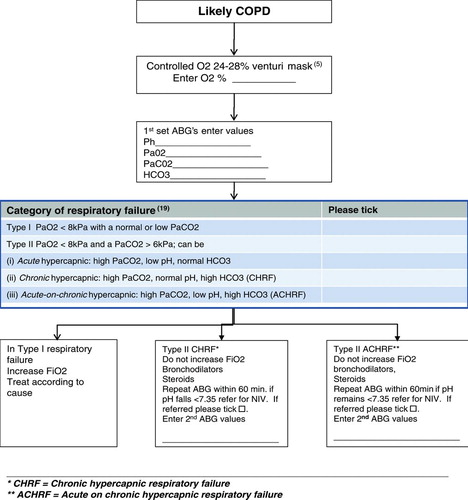
The study was carried out in a busy inner city University Teaching Hospital Emergency Department from Feb 2006 to July 2007. The ED sees around 70 acute COPD cases per month. All patients are initially seen by ED junior staff. Patients requiring ongoing care are admitted to a Medical Admission Unit (MAU) where patient care is taken over by inpatient teams. Indications for admission are based on the COPD guidelines (Citation5-6). Acidaemic patients are referred to ICU staff for NIV. The pro-forma design focused on correct categorisation of respiratory failure (Citation19) as it was felt to be fundamental to the understanding to further management of COPD.
All patients with a known history of COPD were included. During the study period there were several groups of junior doctors who rotated through the department. Pro-forma () education occurred during the induction period (first 2 weeks) after commencement. This education was reinforced in practise. Results were analysed in pre and post pro-forma periods. Data for pre pro-forma groups were collected from ED case notes and post intervention data was collected from the pro-formas. The primary end point was the ability to correctly categorise respiratory failure by junior doctors. Secondary end points included the administration of controlled oxygen, repeat arterial blood gases if indicated (pH ≤ 7.35, PaO2 < 8kPa, PaCO2 > 6 kPa) and appropriate referral for NIV.
STATISTICAL ANALYSIS
Sample size
Based on unpublished data from a pilot study we anticipated that less than 35% of patients with respiratory failure would be categorised correctly in accordance with British Thoracic Society guidelines before implementation of the COPD Performa. Using a corrected Chi-square test it was estimated that 56 subjects pre-proforma implementation and 56 post-implementation would be required to detect a 30% change in the proportion of patients correctly categorised with a power of 85% and an alpha of 0.05.
Analysis
The pre-post intervention difference in the proportion of patients assigned the correct COPD categorisation by junior doctors was calculated using StatsDirect software (version 2.2.78, CamCode, Ashwell, UK) and p-values and 95% confidence intervals reported. A p-value of <0.05 was considered as representing statistical significance. Sensitivity and specificity have been reported to indicate ‘diagnostic’ accuracy of the need to refer patients for NIV.
As this study involved the closure of an audit loop, with a change of practise based on best evidence from national guidelines, approval was sought from the local audit department. Ethical approval was therefore not required.
RESULTS
The median age in each group is similar, 76 years (IQR 66–82, range 46–90) compared to 72 years (IQR 66–78, range 54–88), with some variance of gender distribution, 36% compared to 56% male in the pre. and post intervention groups respectively.
The main pre and postintervention results are shown in . The categorisation of respiratory failure improved markedly after the introduction of the pro-forma. Similarly administration of controlled oxygen, repeat ABGs and referral for NIV showed significant improvement after using the pro-forma.
The sensitivity (true positive rate) of junior doctors in identifying patients requiring NIV was 33% (95% CI 10 to 65%) and their specificity (true negative rate) was 95% (95% CI 84 to 99%) prior to the implementation of the pro-forma.
Table 2. ‘Diagnosis’ of need for niv referral pre-pro-forma
Table 3. ‘Diagnosis’ of need for NIV referral post-pro-forma
The positive predictive value of their independent identification of patients needing NIV (the probability of patients they identified as actually requiring NIV) was 67% (95% CI 22 % to 96%) and the negative predictive value (the probability of patients they identified as not requiring NIV) was 84% (95% CI 70% to 92%). After the introduction of the pro-forma, the junior doctors sensitivity in identifying patients requiring NIV rose to 100% (95% CI 66 to 100%) as did their specificity (95% CI 92 to 100%).
Table 4. Pre- post-proforma differences in the proportion of acidaemic patients receiving controlled O2
The positive predictive value of junior doctors’ identification of patients needing NIV when supported by the pro-forma increased to 100% (95% CI 66 to 100%) as did the negative predictive value (95% CI 92 to 100%). The post pro-forma 67% increase in the proportion of patients requiring NIV who were correctly identified by junior doctors (sensitivity) is statistically significant (95% CI for difference +29 to +87%, P = 0.0023) although this is not the case for the relatively small 5% increase in specificity (95% CI for difference -3 to +15%, P = 0.1153). The increases in positive and negative predictive values were also not statistically significant, Tables , , .
compares the percentage of acidaemic (pH < 7.45) patients who received controlled oxygen pre and postintervention. Although there was no significant between-groups difference in the proportion of patients who were acidaemic there was a statistically significant improvement in junior doctors administering controlled oxygen post pro-forma.
The study has demonstrated a significant improvement in compliance to NICE Guidelines, CG12 (Citation6).
Controlled Oxygen Therapy: The administration of controlled oxygen improved from 47% to 93%;
Repeat Arterial Blood Gases: this improved from 50% to 83%;
Appropriate Referral for NIV: this improved from 33% to 100%.
DISCUSSION
This study shows that pro-forma based care significantly improves COPD management in the Emergency Department. The pro-forma focused primarily on the categorisation of respiratory failure as it was felt that this was fundamental to the understanding of further management of COPD. Previous unpublished department surveys of COPD patient indicated that guidelines were not being followed and patient management including referrals for NIV was occurring randomly.
The authors felt that education the category of respiratory failure was fundamental to COPD management as there remains confusion regarding the subdivisions of Type II respiratory failure. The classification of respiratory failure category published by the British Thoracic Society in 2002 (Citation19), was felt to be the most widely accepted and was thus used in the pro-forma. Several junior doctors commented that they found this box very useful.
The challenge faced by authors was implementing pro-forma's and ensuring their continued use and this depends on education during induction, re-enforcement in practise and the ease of availability of the guidelines. The Department achieved this by making it universally available on the Hospital Intranet. Since completion of the study the pro-forma has been incorporated in the ED Junior Doctors Handbook, which is available as a hard copy and electronically in the department.
In the latest national audit of COPD care practice in NHS units (Citation8), Then, 70% of patients were placed on controlled oxygen pre-ABG compared with 93% in the present study. In addition, only 79% of acidaemic patients (pH < 7.35) nationally had a repeat ABG within 24 hours compared with 83% within 4 hours in this study.
Since the national guidelines were introduced, 90-day mortality rate has dropped from 15.5% to 13.9% and median length of hospital stay from 6 to 5 days across the UK. Our study has shown that the implementation of simple educational measures and the introduction of a management pro-forma has significantly improved the diagnosis and management of this patient group indicating the answer perhaps lies in adopting National Guidelines and championing them locally.
The study shows that a pro-forma can be an effective screening tool in the Emergency Department to highlight those patients at risk. Clinical implications are that the introduction of a relatively simple tool and can result in a consequent change in practise and lead to an improvement in clinical care for patients.
Limitations
The study has limitations. Data for the pre-intervention group was collected from ED case notes. All fields were complete in 60% of cases. Patients with incomplete notes were discarded. It may be criticised that this is not a true representation of ED patients, however, given the nature of the patients presenting with acute COPD it was felt that variation was minimal and the case range was acceptable. It took 18 months to complete the post-pro-forma group indicating a low pro-forma utilisation rate. This is acknowledged and is a common challenge faced by the real world of a busy ED, and it is hoped with the integration of the pro-forma in the ED Junior Doctor's Handbook this will improve. A further study is required to confirm if continuing education and ease of access improves pro-forma utilisation.
It is possible that improvements in junior doctor's medical school education concerning the diagnosis and management of COPD may have been a confounding factor in this study due to the time difference and the change of personnel between data collection intervals pre- and post-proforma introduction. However the lead author's experience of teaching junior staff during this entire interval suggests this was unlikely to be the case.
CONCLUSION
This study has demonstrated that pro-forma guided management in the ED results in significant improvements in both the correct categorisation and the management of COPD patients by junior doctors in the Emergency Department. Although useful for guiding management decisions in doctors-in-training pro-forma's may be suitable for use by other health care professionals in the ED setting.
Further research is required to determine if the interventions described in this study result in a greater reduction in mortality and morbidity, length of inpatient stay and costs to the health service than already witnessed nationally.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Lost in Translation. Bridging the communication gap in COPD (June 2006) British Lung Foundation Survey.
- Roberts CM, Ryland I, Lowe D, Kelly Y, Bucknall CE, Pearson MG. Clinical audit indicators of outcome following admission to hospital with acute exacerbations of Chronic Obstructive Pulmonary Disease. Thorax 2002; 57:137–141.
- Price LC, Lowe D, Hosker HSR, Pearson, Roberts CM. UK National COPD Audit 2003: impact of hospital resources and organisation of care on patient outcome following admission for acute COPD exacerbation. Thorax 2006; 61:837–842.
- Roberts CM, Barnes S, Lowe D, Pearson MG. Evidence for a link between mortality in acute COPD and hospital type and resources. Thorax 2003; 58:947–949.
- The British Thoracic Society (BTS). Guidelines for the management of COPD. Thorax 1997; 52:1–28.
- Chronic Obstructive Pulmonary Disease. National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary care. Thorax March 2004; 59 Suppl. 1;1–232.
- The Academy of Royal Colleges and managed by the Clinical Effectiveness Evaluation Unit of the Royal College of Physicians. Audit of process and outcome in cases of acute exacerbations of COPD admitted to hospital’. A pilot study commissioned by The Academy of Royal Colleges and managed by the Clinical Effectiveness Evaluation Unit of the Royal College of Physicians supported by the Audit Subcommittee of the Standards of Care committee of the British Thoracic Society. 2002
- Royal College of Physicians and British Thoracic Society. (2008). Report of the National Chronic Obstructive Pulmonary Disease Audit 2008. COPD exacerbations admitted to acute HNS units. Retrieved March 10, 2009, from http://www.rcplondon.ac.uk/clinical-standards/ceeu/Currentwork/ncrop/Documents/Report-of-The-National-COPD-Audit-2008-clinical-audit-of-COPD-exacerbations-admitted-to-acute-NHS-units-across-the-UK.pdf.
- Meyer RJ, Town GI, Harre E, Koning M, Hurrell M, Beard ME, Chambers ST. An audit of the assessment and management of adults admitted to Christchurch Hospital with community acquired pneumonia. New Zeal Med J 1997; 110:349–352.
- Soulsby T. British Thoracic Society guidelines for the management of spontaneous pneumothorax: do we comply with them and do they work? J Acc Emerg Med 1998; 15:317– 321.
- Mendis D, El-Shanawany T, Mathur A, Redington AE. Management of spontaneous pneumothorax: are British Thoracic Society guidelines being followed? Postgrad Med J 2002; 78:80–84.
- Hart SR, Davidson AC. Acute adult asthma – assessment of severity and management and comparison with British Thoracic Society Guidelines. Respir Med 1999; 93:8–10.
- Cohen S, Taitz J, Jaffe A. Paediatric prescribing of asthma drugs in the UK: are we sticking to the guideline? Arch Dis Child 2007; 92:847–849.
- Robinson SM, Harrison BDW, Lambert MA. Effect of a pre-printed form on the management of acute asthma in an accident and emergency department. J Acc Emer Med 1996; 13:93–97.
- Nicol MF. A risk management audit: are we complying with the national guidelines for sedation by non-anaesthetists. J Acci Emerg Med 1999; 16:120–122.
- Steurer-Stey C, Grob U, Jung S, Vetter W, Steurer J. Education and a standardized management protocol improve the assessment and management of asthma in the emergency department. Swiss Med Week 2005; 135:222–227.
- Medford AR, Pepperell JC. Management of spontaneous pneumothorax compared to British Thoracic Society (BTS) 2003 guidelines: A district general hospital audit. Prim Care Respi J 2007; 16:291–298.
- Self TH, Usery JB, Howard-Thompson AM, Sands C. Asthma treatment protocols in the emergency department: are they effective? J Asthma 2007; 44:243–248.
- BTS. Guidelines for non-invasive ventilatory support in respiratory failure. Thorax 2002; 57:192–211.