Abstract
The use of rhythmic music is beneficial in assisting with the exercise intensity at home. This paper investigated the effects of paced walking to music at home with an 80% VO2 peak for patients with COPD. A prospective randomized clinical trial consisting of a treatment group (n = 20) assigned to a 12-week period of paced walking to music at home, while the patients in the control group (n = 21) were only given educational information. The treatment response was measured based on the patient's score in the maximal exercise capacity test using the incremental shuttle walking test (ISWT), lung function, health- related quality of life (HRQOL) using the Saint George Respiratory Questionnaire (SGRQ) and their health care utilization during baseline, 4, 8, 12 and 16 weeks. The treatment group increased their distance in the ISWT from 243.5 ± 135.4 at baseline to 16 weeks (306.0 ± 107.3, p < 0.001), Borg RPE-D decreased from 2.2 ± 1.3 at baseline to 0.8 ± 1.1 (p < 0.001) at 16 weeks, and Borg RPE-L decreased from 1.2 ± 1.4 at baseline to 0.3 ± 0.7 (p < 0.05) at 16 weeks, and improved all of the domains of the SGRQ, compared to the control group. The paced walking to music at home program helps patients to achieve a higher-intensity exercise. It is easily incorporated into the care of COPD patients, providing them with a convenient, safe and enjoyable exercise.
| Abbreviations | ||
| Borg RPE-D: | = | the rating of perceived exertion for dyspnoea on the Borg category-ratio scale |
| Borg RPE-L: | = | the rating of perceived exertion for leg fatigue on the Borg category-ratio scale |
| CONSORT: | = | Consolidated Standards of Reporting Trials |
| COPD: | = | chronic obstructive pulmonary disease |
| DAS: | = | distractive auditory stimuli |
| FEV1: | = | forced expiratory volume in 1 second |
| GDS: | = | Geriatric Depression Scale |
| GEE: | = | Generalized Estimating Equations |
| GOLD: | = | Global Initiative for Chronic Obstructive Lung Disease |
| HRQOL: | = | health-related quality of life |
| ISWT: | = | incremental shuttle walking test |
| MCID: | = | minimum clinically important difference |
| PFT: | = | pulmonary function test |
| SGRQ: | = | Saint George Respiratory Questionnaire |
| QOL: | = | quality of life |
| RAS: | = | Rhythmic Auditory Stimulation |
| SPMSQ: | = | Short Portable Mental Status Questionnaire |
| SpO2: | = | oxygen saturation by pulse oxymeter |
| VO2 peak: | = | peak oxygen uptake. |
Introduction
Progressive exercise intolerance and exertional dyspnea, the subjective experience of uncomfortable breathing, are often common features of chronic obstructive pulmonary disease (COPD) (Citation1), which contribute to a reduced health-related quality of life (HRQOL) (Citation2, 3). In addition, exercise intolerance may result from ventilatory and gas exchange limitations, cardiovascular impairment, skeletal muscle dysfunction, and nutritional impairment (Citation4–6).
One study found that patients with COPD progressively reduced the time they spent outdoors by 0.14 hours per day per year (Citation7). Patients with COPD can benefit from exercise training programs (Citation5, Citation8, Citation9) because exercise reduces impairment and improves exercise tolerance (Citation10). Two randomized controlled trials (RCTs) demonstrated the beneficial effects of exercise for COPD improvements in exercise capacity and HRQOL, decrease in dyspnea, hospital admission and mortality rates (Citation11, 12).
Rationale for home-based exercise
Home-based exercise is feasible for both patients and families in part because patients are accustomed to the environment. Previous COPD exercise programs were mainly performed in hospitals (Citation8, Citation13, Citation14). Although COPD patients are usually home bound because of exercise intolerance or acute exacerbations (Citation7), they are better able to maintain their exercises and progressively improve compared to patients following the in-hospital program. In a study by Stribos et al. (Citation15), individuals, who engaged in home-based exercise maintained an improved exercise tolerance and a reduced dyspnea compared to patients enrolled in the outpatient program. However, following an exercise program at home has its limitations (Citation15, 16).
In the last decade, a number of studies have demonstrated an improved exercise capacity and HRQOL as a result of home-based exercise programs in COPD (Citation17, 18). When the intensity of the training is high enough, a physiological effect can be achieved in the home setting as well (Citation19). However, existing home-based studies have shown that only 50% of patients adhere to the intensity guidelines advised by health-care professionals (Citation20). In Taiwan, Liu et al. (2008) pioneered the use of cell phones and music paced to set the walking speed at home for patients with moderate-to-severe COPD (N = 48). Their data suggests improvements in the distance of the incremental shuttle walking test (ISWT) and the generic quality of life (Citation17). The purpose of our study was to assess the impact music has on maintaining a sustained walking pace at home.
Rationale of high-intensity exercise for COPD patients
The intensity of the exercise is considered an important determinant of the training response (Citation21). Low intensity exercise is <70% of VO2 peak, moderate is 70–79%; and high intensity is between 80–89% (Citation6). A recently reviewed article (Citation21) analyzed three studies to make a comparison between higher and lower-intensity training. They found that there was insufficient data to draw any conclusions on exercise capacity, symptoms and HRQoL. However, they found that higher intensity training had a greater physiological improvement (Citation5, 6, Citation22), in maximal exercise capacity, FVC and work efficiency (Citation23), than lower intensity training for patients with COPD. Casaburi and colleagues (Citation24) also showed that high intensity exercise at 80% of maximum exercise capacity for patients with severe COPD improved the overall exercise tolerance due to more efficient exercise and lower-minute ventilation.
To date, there are only a scant few well-designed studies available on high intensity at home training for COPD patients. Only one research study investigated the use of an at- home paced-walking exercise intervention for COPD patients (Citation17). No previous studies ever assessed the effect of an at-home paced-walking program on the disease-specific quality of life for COPD patients. In addition, no previous studies ever combined the use of a repeated measure with Generalized Estimating Equations (GEE). This strategy is useful because it can correct for potential missing data caused by patients dropping out, which may result in biased treatment comparisons affecting the overall statistical power of clinical trials (Citation25). Thus, because of the gaps in the literature, we developed and examined the impact of a paced walking to music at home program and compared it with the control group that received educational care only. We hypothesized that COPD patients who followed the paced walking to music at home for 12 weeks would improve in the following areas: (1) exercise capacity, (2) pulmonary function, (3) HRQOL and (4) reduce their health care utilization compared to the control group.
Methods
Design
We conducted a prospective, randomized, controlled intervention that was focused on home-based walking exercise. The exercise capacity was measured by the ISWT, pulmonary function, HRQOL, and the health care utilization of the COPD patients. Data were collected between July 1, 2009 and August 30, 2010.
Participants and setting
Inclusion criteria for the intervention were: (1) stable COPD patients diagnosed by a pulmonary physician, (2) FEV1/FVC ratio < 70%, (3) no acute exacerbation within the last month, (4) did not use O2. Exclusion criteria were: (1) past experience of supervised pulmonary rehabilitation. (2) Geriatric Depression Scale (GDS) > 10 or (3) cognitive deficits with a Short Portable Mental Status Questionnaire (SPMSQ) < 7 (4), having an unstable heart disease (5), having a muscular skeletal disease, or (6) having a visual or hearing impairment, and (7) or any other condition that could affect their ability to perform the required exercise.
Procedures
Participants who met the inclusion criteria were given a brief explanation of the study by primary care physicians. They also were given, as well as an explanation of the exercise program coupling with an invitation to participate by the outpatient chest clinic at a medical center and two regional teaching hospitals in northern Taiwan. If they agreed to attend the program, the research nurse referred them to the next step which was obtaining their informed consent. After they answered the baseline questionnaire, patients were randomly assigned to either the paced walking to music at home group or to the routine-care group. Randomization was in blocks of 8, using random allocation software (Citation26). Owing to the nature of the intervention, participants were difficult to blind. An assessor, blinded to group allocation, collected all of the outcome measures. Another assessor delivered the intervention and performed the data analysis. The study was approved by the Institutional Review Board of Tri-Service General Hospital, Wei-Gong Memorial Hospital, and Saint Paul's Hospital before commencing the study.
Interventions
Control group - receiving the usual care. Patients assigned to the control group were given routine care and a brochure that contained information on COPD self-care, and an overview of the benefits of exercise, as well as precautions to take when exercising. Primary care physicians encouraged participants to do their usual exercise at least 5 times per week. To ensure that the participants calculated their home-exercise adherence on a monthly basis, they were asked to daily record the amount of exercise they performed in a diary. Participants that reported at least 30 minutes of exercise each day, 5 times per week, scored 100%.
The paced walking to music at home group
The participants that were assigned to the paced walking to music group received the “usual care” as described above, plus an individualized exercise program to teach them the principles of warm-up and cool-down. The initial training speed was set at 80% VO2 peak and then increased gradually, based on the distance of ISWT each month. The VO2 peak (mL/min/kg) was 4.19 + 0.025 × ISWT distance (Citation27). The levels of the endurance training walk were divided into 16 grades, increasing by 0.25 (km/h) per grade (Citation17). One investigator then visual counted the number of steps by asking patients to walk run a shuttle at the required level of endurance training. The at-home walking speed (km/h) was adjusted once a month based on the distance of ISWT (Citation28). If a participant increased the length of their stride, then we slowed down the tempo of the music (beat per minute) according to the formula as follows: the tempo of the music = walking speed × 100 × steps per shuttle/60 (Citation17).
First, the patients selected their favorite type of music, i.e., folk songs, old songs, or popular music. Then we played their individualized speed pacing music in digital MIDI format on an MP4 player (1G, 1.8; Net Team Inc; Taipei, Taiwan) and asked the participants to match their walking speed to the tempo of the music on the MP4 player. The tempo of the music was adjusted once a month. The cost of the MP4 player was 20 USD, and the participants kept the MP4 player until the follow-up was completed at 16 weeks.
The investigator spent 3–5 minutes to set the tempo of the music on the MP4 players according to the ISWT once a month. The aim of the paced walking to music was to walk at least 30 minutes a day, 5 days a week for 12 weeks. The duration of the daily exercise was increased over time if it did not create a discomfort for the participant.
Outcomes measures
Exercise capacity. ISWT is an incremental, symptom-limited exercise test and was evaluated according to the standard guidelines (Citation29). The reasons for using the ISWT were as follows: (1) The primary result of the ISWT is obtained by pacing guided by an external signal. The pacing or walking speed is not affected by the emotion nor by the motivation of the patient. (2) The ISWT starts with a slow walking pace which gradually increases over time. This makes it more suitable for testing the maximal exercise capacity of patients with a moderate-to-severe degree of COPD. (3) The ISWT is a standardized test for the purpose of assessing the exercise capacity of COPD patients. It was used to calculate the speed of endurance training at home during this study.
The participants were required to walk around a 10-meter course. The walking speed was regulated by controlling the computer signals. The initial walking speed started off at 0.5 m/s, and increased each minute by 0.17 m/s for a maximum of 12 levels. No encouragement was given throughout the ISWT. Before and after the ISWT, the oxygen saturation (SpO2) and heart rate were measured using a hand-held pulse oxymeter (Nonin PalmSat 2500; Nonin Medical Inc; Plymouth, MN), and the rating of the perceived exertion for dyspnea (Borg RPE-D) and leg fatigue (Borg RPE-L) were measured using the Borg CR-10 scales (Citation30), and the pulmonary function test (PFT) was measured as well. The participants’ heart rate and SpO2 were supervised during the measuring process. The criteria to terminate the ISWT were as follows: (1) feeling discomfort such as dyspnea, leg fatigue; or, (2) the participant could not follow the speed to achieve the end stop before the time up. Test-retest reliability = 0.98∼0.99 (Citation29).
Pulmonary function test. The outcome of the pulmonary function includes the forced expiratory volume in one second (FEV1), forced vital capacity (FVC), FEV1% predicted and FEV1/FVC measured with a Spirometer (Spirolab II; SDI Diagnostics Inc; Waukesha, WI), performed according to guidelines (Citation31).
Health-related quality of life. HRQOL was assessed using the Chinese version of the Saint George Respiratory Questionnaire (SGRQ) (Citation32), which consists of 50 items focusing on (1) symptoms, (2) activity, and (3) impact (Citation33). Each component of the weighted score ranges between 0 (worst health) and 100 (best health). For the COPD patients, reliability was between 0.77–0.95 (Citation34).
Healthcare utilization. The use of healthcare for COPD by the participants was assessed every month by reviewing the participant's chart and asking them about how often they admitted to the hospital during the past 4 weeks, how long each time, how often did they go to the hospital for an emergency or an unscheduled clinic visit.
Sample size calculation
The minimum sample size on the basis of the primary outcome –distance of ISWT with previous research (Citation35), estimated that at least 15 patients in each group would be required to detect a 50 meters change, standardized difference of 1.2 (m) in ISWT, with a 90% power at the 5% significance level. Allowing for 30% loss to follow-up, a total of 38 recruits (19 per group) were needed.
Statistical analysis
The baseline characteristics between the two groups were compared using unpaired t-tests for the means or Fisher's exact χ2 for the categorized variables. The GEE (Citation36) for repeated measures was used to compare intervention and control group change from the baseline to each of the 4-month follow-up visits on the outcomes of exercise capacity, pulmonary function, and HRQOL. We used the GEE because it adjusts for the follow-up assessments by intention-to-treat analyses measures correlated across visit weeks 1, 4, 8, 12 and 16.
Age, lifetime years of smoking, years since COPD diagnosis, severity of airflow obstruction (grade- IV) by the GOLD criteria, and acute exacerbation were considered as covariates. In addition to treatment and time, covariates were forced into the model to perform the GEE. An interaction term for trial × time was included to control for p < 0.05 compared to the control group. We used the t test to compare the mean values of the mean differences between groups for health care utilization. All analyses were conducted using Predictive Analytics Software (PASW) Statistics 18.0, and a p < 0.05 was considered statistically significant.
Results
Patients characteristics
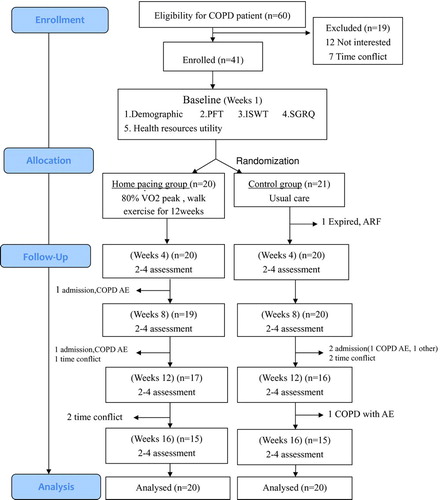
summarizes the participation flow and trial retention based on the 2010 CONSORT (Consolidated Standards of Reporting Trials) statement (Citation37). We identified 60 eligible patients that met our study criteria. Of these, 19 (31.7%) had no interest or they had a time conflict, and did not enroll in the study. The remaining 41 patients were randomized to receive paced walking to music at home exercise (n = 20) and the other group received the usual care, and served as the control group (n = 21). Then, 4.9%, 7.3% and 14.6% of the participants withdrew or were withdrawn from the study at 8, 12 and 16 weeks, respectively. The 3-month follow-up assessments were carried out with 73.2% (n = 30, 15 in each group) of the original patients.
Demographics
Overall, the mean age was 74.0 ±10.3 years, and 34% had stage III COPD, and 39% had stage II COPD as per the Gold definition (Citation10). The average number of years since first diagnosed with COPD was from 0.3 to 20 (7.3 ± 5.5) years, smoking pack-year from 13-56 (39.4 ± 40.8). None of the participants had cognitive or emotional problems that affected the performance of the exercises. The participants in both groups were homogeneous in sex distribution, age, BMI, smoking history, and number of years of COPD history (). There were homogeneous in the parameters of exercise capacity, spirometry, SGRQ total, activity, impact, and symptom scores, or health care utilization ().
Table 1. Characteristics of the study subjects at baseline
Table 2. Mean ± SD of outcome variables at baseline
Effects of exercise training on exercise capacity
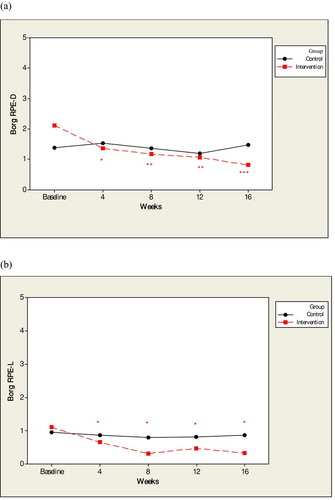
After controlling for covariates, the GEE results revealed that the two groups differed significantly for the ISWT distance from baseline to each successive period. The paced walking to music at home group increased from 243.5 ± 135.4 at baseline to 306.0 ± 107.3 (95% CI = 79.7 ∼ 152.0, p < 0.001) at 16 weeks compared to the control group means of 237.6 ± 124.4 to 218.5 ± 119.4 across the 5 visits (). In addition, the 2 groups differed significantly in their ratings of exertion measured by Borg RPE-D from baseline to each successive period. The intervention group decreased from 2.2 ± 1.3 at baseline to 0.8 ± 1.1(95% CI = –2.1 ∼ –0.7, p < 0.001) at 16 weeks compared to the control group's means of 1.4 ± 1.6 to 1.5 ± 1.6 across the 5 visits (); and Borg RPE-L decreased from 1.2 ± 1.4 at baseline to 0.3 ± 0.7(95% CI = –1.2 ∼ –0.2, p < 0.05) at 16 weeks which was also a significant improvement over that of the control group ().
Figure 2. The mean values for the walking distance (m) of the incremental shuttle walking test at visits at baseline to 16 weeks. *p < 0.05, **p < 0 .01, ***p < 0.001Notes: The home pacing group increased from 243.5 ± 135.4 at baseline to 4 weeks (285.5 ± 136.2, x2 = 13.3, p < 0.001), 8 weeks (288.4 ± 136.2, x2 = 73.7, p < 0.001), 12 weeks (280.6 ± 139.1, x2 = 99.6, p < 0.001), and 16 weeks (306.0 ± 107.3, x2 = 40.1, p < 0.001) compared to the control group means of 237.6 ± 124.4, 204.3 ± 96.4, 206.4 ± 102.8, 209.9 ± 11.2, 218.47 ± 119.41 across the 5 visits.
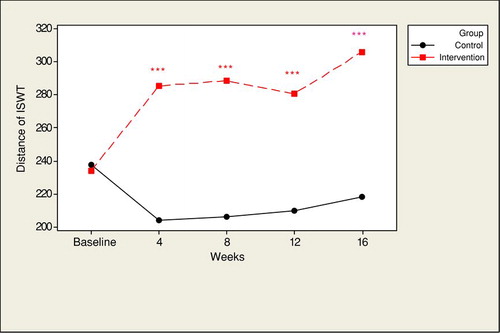
Figure 3. The mean values for Borg RPE-D (3a) and Borg RPE-L (3b) at visits at baseline to 16 weeks. *p < 0.05, **p < 0.01, ***p < 0.001.
However, there was no differential change between the 2 groups from baseline to any of the other four visits in the mean resting heart rate and SpO2 (p > 0.05). The adherence rate 1 month post exercise training was 84.3% ± 34.7 vs 30.8 ± 45.4% during the study!]t = –3.6, 95% CI = –83.7 ∼ –23.3, p < 0.01 ).
Effects of exercise training on the pulmonary function test
There was also no differential change between the 2 groups from baseline to any of the other four visits for the mean FEV1 and% of FEV1 of predicted.
Effects of exercise training on HRQOL
There was a significant improvement for the intervention group in the score from the baseline to most of the subsequent four visits for the SGRQ total, symptom, and impact domain scores compared to the control group. In addition, the 2 groups differed in their change from the baseline in their SGRQ activity scores after 8 weeks (see ).
Table 3. Health care utilization during the 4 months study period
Table 4. Mean values for SGRQ scores at visits baseline to 16 weeks and GEE analysis to verify the effectiveness of home-based exercise
Effects of Exercise Training On Health Care Utilization
During the 4 months of the intervention, there was a statistically significant difference in unscheduled clinic visits between the treatment group and the control group (p < 0.001) (). In fact, 10% (n = 2) of the patients in the treatment group and 9.5% (n = 2) of the patients in the control group were admitted to the hospital. However, there were no significant differences between the two groups when it comes to the hospitalization of patients due to COPD with acute exacerbation during the four month follow up. Finally, there was no significant difference regarding the number of hospitalization days and the frequency of visiting the emergency department between the two groups.
Discussion
Our study is the first to establish that a paced walking to music at home program leads to significantly higher disease-specific improvements in QOL compared to the control group. The intervention also promoted the capacity to exercise among the participants. Our study confirms previous studies which indicate that patients with COPD can perform high intensity home walking training exercises (Citation22). The strengths of this study were that we were able to provide a customized paced walking program to each of the COPD patients. The walking speed for home training ranged from 2.3 to 5.3 (3.6 ± 0.9) km/hour, while the pacing music ranged from 60–135 (94.8 ± 18.8) beats/min based on the individual's personal ISWT distance.
Second, we used the symptom-limited ISWT to quantify a patient's maximal exercise tolerance, and then gradually increased the time and intensity starting at 80% VO2 peak in order to achieve high-intensity exercise. We are aware that if the intensity of the training reaches a certain threshold, the participants will experience a greater physiological effect (Citation23, Citation38). However, high-intensity exercise can induce greater patient discomfort, such as dyspnea, which may ultimately lead to exercise intolerance (Citation5). Therefore our level of exercise was gradually increased over time in order to maintain high-intensity training (Citation6).
The use of paced walking to music at home for COPD patients
The present study shows that paced walking to music is a good way to learn how to exercise effectively. The role of music in our study (Citation1) made it easier for patients to achieve the desired exercise intensity by having them follow the tempo of the music. Thaut et al. (Citation39), utilized Rhythmic Auditory Stimulation (RAS) to slowly increase the rhythm of the music, which increased the walking speed, velocity, step cadence, and stride length in stroke patients (Citation2). As a form of distractive auditory stimulus (DAS), music may affect a person's mood and decrease perceived dyspnea (Citation1, Citation40–42). In the United States (US), one study found that patients who walked and listened to music had less perceived exertional dyspnea during activities of daily living (ADLs) as well as an improved walking distance (Citation42). That same author conducted another trial using music as a form of DAS with different speeds during an upper extremity program (Citation41), and found a decrease in the dyspnea sensation in COPD patients. Thus, the use of music during exercise training can be effective (Citation3). Paced walking with music helps subjects to enjoy doing their exercise. One study found that although 5 different types of music were used during the walking exercise, the type of music played was not statistically significant for the Borg RPE-D outcomes (Citation43), 60% of the patients enjoyed walking while listening to music. We provided 40 songs including folk songs, old songs, and popular music for pacing walk.
It's difficult to determine the effects of different types of music on the outcome variables because the participants have the choice of many different types of music with the same tempo. The most important issue was that they selected their favorite music to do their exercise so as to increase their enjoyment while walking and keep them motivated.
Effects of exercise training on exercise capacity
Singh, Jones, Evans, and Morgan (2008) estimated that a 47.5 meter increase or decrease in the ISWT promoted a significant clinical difference in exercise capacity (Citation44). Thus, there was a statistically significant difference between the 2 groups at week 16, which is consistent with other study (Citation17). However, Hernandez et al. (2000) asked patients to perform their walking exercise for 1 hour every day, but did not find a statistically significant difference in the distance walked and in the pulmonary function (Citation45). It should be noted that this was for a different intensity of exercise, 74.3% maximal speed of ISWT in Hernandez et al., which was lower than our study, which had an intensity of exercise at 80%.
We also found that the home pacing walk group had a significant improvement in resting dyspnea and fatigue scores after 16 weeks of exercise. This result is similar to the results of some previous reports (Citation8, Citation15, Citation28). Despite the benefits, it is important to note that we observed no significant differences in physiologic parameters such as heart rate and SpO2 between the 2 groups. These finding are consistent with previous home based exercise interventions (Citation15). Other studies also reported that there was no difference between resting heart rate between groups after home exercise training (Citation45), including those in an outpatient program (Citation23). This is in contrast with a 12-week high-intensity study by Camillo et al. (Citation38) which showed that only high-intensity training leads to physiologic gains; in particular, improvement in the heart rate (Citation5). We developed a convenient method for paced walking and controlling the walking speed, but it was limited to the unsupervised performance at home. Further studies need to be developed in order to understand how people will adhere to the program when supervised.
Effects of exercise training on HRQOL
Our study is the first to find that paced walking to music at home leads to significantly higher disease-specific QOL than the control group. In addition, a change of four units in the SGRQ total score in clinical trials of COPD represents a minimal clinically significant change (Citation46). A previous study (Citation17) only confirmed that the benefit of paced walking at home made a difference in the generic QOL, however, they did not examine the disease specific QOL in patients suffering from COPD.
It is worth noting that one study found that home-based intervention did not improve the SGRQ scores (Citation41). The reason for the findings in both studies might be due to the fact that they required patients to just walk while listening to music not walk to the beat of the music. However, our study is of higher intensity as it asks the patients to walk to the beat of the music, and is based on RAS and DAS, not DAS only.
Effects of exercise training on health care utilization
However, no significant differences were found with regards to hospital admissions. One study by Griffiths and colleagues (Citation47) also found that the number of hospital admissions was similar between the intervention group and the control group. Rasekaba et al. (2009) reported a reduction in hospital days and emergency frequency 12 months post-treatment, compared with the non-exercise (control) group (Citation48). In our study, although we provided an exercise regimen of higher intensity and frequency, our follow up included only one follow–up at 1 month post exercise training, and was insufficient to evaluate the effect on health care utilization. Further studies should extend the follow-up period of the post paced walking to music at home program.
Limitations and future implications
Although the benefits of our study are significant, some limitations need to be addressed. First, participants were selected based on their ability to perform the exercises we had in mind. Additionally, our sample consisted primarily of older men who were able to utilize an mp4 player. Therefore, the findings of this study cannot be generalized to women. The prevalence of COPD among women is rapidly increasing (Citation49). Future research needs to focus on this population, their exercise experiences, and should explore the effect of gender on exercise. Second, the participants’ withdrawal rate was 27%. The major reasons of high withdrawal rate were: (1) Patients withdrew if they experienced acute exacerbation or hospital admission, (2) Some clients had technological difficulties with the mp4 player and the exercise diary due to literacy issues; and (3) stable cases of COPD went back to visiting a clinic once every 3 months if they didn't have any attacks. Consequently, they would no longer participate in our study. Finally, additional research needs to focus on a longer time period in order to investigate the long-term effects of this intervention.
Conclusions
Our study extends the knowledge of previous studies by providing an easy and enjoyable method of assisting patients in establishing a high-intensity exercise program at home. Paced walking to music at home provides patients with an exercise program of consistent intensity. It is not merely music to distract the patient. The proposed paced walking to music at home intervention showed a significantly lower level of exertional dyspnea, leg fatigue, improved exercise tolerance and a greater improvement in HRQOL compared to the control group.
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Notice of correction: Changes have been made to this article since its original online publication date of 29 May, 2012.
References
- von Leupoldt A, Taube K, Schubert-Heukeshoven S, Magnussen H, Dahme B. Distractive auditory stimuli reduce the unpleasantness of dyspnea during exercise in patients with COPD. Chest 2007 Nov;132(5):1506–1512.
- Belfer MH, Reardon JZ. Improving exercise tolerance and quality of life in patients with chronic obstructive pulmonary disease. J Am Osteopath Assoc 2009 May;109(5):268–278; quiz 80–81.
- Laveneziana P, Wadell K, Webb K, O'Donnell DE. Exercise limitation in chronic obstructive pulmonary disease. Curr Respir Med Rev 2008;4.
- Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, Bourbeau J, Carone M, Celli B, Engelen M, Fahy B, Garvey C, Goldstein R, Gosselink R, Lareau S, MacIntyre N, Maltais F, Morgan M, O'Donnell D, Prefault C, Reardon J, Rochester C, Schols A, Singh S, Troosters T. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006 /06/09 ed 2006. p. 1390–413.
- Rochester CL. Exercise training in chronic obstructive pulmonary disease. J Rehabil Res Dev 2003 Sep–Oct;40 (5 Suppl 2):59–80.
- Butcher SJ, Jones RL. The impact of exercise training intensity on change in physiological function in patients with chronic obstructive pulmonary disease. Sports Med 2006;36(4):307–325.
- Donaldson GC, Wilkinson TM, Hurst JR, Perera WR, Wedzicha JA. Exacerbations and time spent outdoors in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2005 Mar 1;171(5):446–452.
- Ergun P, Kaymaz D, Gunay E, Erdogan Y, Turay UY, Demir N, Canak E, Sengul F, Egesel N, Kose SK. Comprehensive out-patient pulmonary rehabilitation: Treatment outcomes in early and late stages of chronic obstructive pulmonary disease. Ann Thorac Med 2011 Apr;6(2):70–76.
- Berry MJ. The relationship between exercise tolerance and other outcomes in COPD. COPD 2007 Sep;4(3):205-16.
- Global Strategy for the Diagnosis, Management and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2010; 2010 [cited 2011 9.26]; Available from: http://www.goldcopd.org/.
- Lacasse Y, Martin S, Lasserson TJ, Goldstein RS. Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. A Cochrane systematic review. Eura Medicophys 2007 Dec;43(4):475–485.
- Puhan MA, Scharplatz M, Troosters T, Steurer J. Respiratory rehabilitation after acute exacerbation of COPD may reduce risk for readmission and mortality—a systematic review. Respir Res 2005;6:54.
- Hui KP, Hewitt AB. A simple pulmonary rehabilitation program improves health outcomes and reduces hospital utilization in patients with COPD. Chest 2003 Jul;124(1):94–97.
- von Leupoldt A, Hahn E, Taube K, Schubert-Heukeshoven S, Magnussen H, Dahme B. Effects of 3-week outpatient pulmonary rehabilitation on exercise capacity, dyspnea, and quality of life in COPD. Lung 2008 Nov–Dec;186(6):387–391.
- Strijbos JH, Postma DS, van Altena R, Gimeno F, Koeter GH. A comparison between an outpatient hospital-based pulmonary rehabilitation program and a home-care pulmonary rehabilitation program in patients with COPD. A follow-up of 18 months. Chest 1996 Feb;109(2):366–372.
- Hill NS. Pulmonary rehabilitation. Proc Am Thorac Soc 2006;3(1):66–74.
- Liu WT, Wang CH, Lin HC, Lin SM, Lee KY, Lo YL, Hung SH, Chang YM, Chung KF, Kuo HP. Efficacy of a cell phone-based exercise programme for COPD. Eur Respir J 2008 Sep; 32(3):651–659.
- Ghanem M, Elaal EA, Mehany M, Tolba K. Home-based pulmonary rehabilitation program: Effect on exercise tolerance and quality of life in chronic obstructive pulmonary disease patients. Ann Thorac Med 2010 Jan;5(1):18–25.
- Wijkstra PJ. Home based rehabilitation for patients with COPD. Is it equally effective as compared to outpatient rehabilitation? Monaldi Arch Chest Dis 2003 Oct–Dec;59(4):335–337.
- Hunter J, Singh SJ, Morgan MDL. Objective monitoring of adherence with home exercise training during pulmonary rehabilitation for chronic obstructive pulmonary disease. Physiotherapy 2006; 92(1):50–54.
- Zainuldin R, Mackey MG, Alison JA. Optimal intensity and type of leg exercise training for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2011;11:CD008008.
- Punzal PA, Ries AL, Kaplan RM, Prewitt LM. Maximum intensity exercise training in patients with chronic obstructive pulmonary disease. Chest 1991 Sep; 100(3):618–623.
- Hsieh MJ, Lan CC, Chen NH, Huang CC, Wu YK, Cho HY, Tsai YH. Effects of high-intensity exercise training in a pulmonary rehabilitation programme for patients with chronic obstructive pulmonary disease. Respirology 2007 May; 12(3):381–388.
- Casaburi R, Patessio A, Ioli F, Zanaboni S, Donner CF, Wasserman K. Reductions in exercise lactic acidosis and ventilation as a result of exercise training in patients with obstructive lung disease. Am Rev Respir Dis 1991 Jan;143(1):9–18.
- Myers WR. Handling missing data in clinical trials. Drug Infor J 2000;34.
- Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol 2004 Nov 9;4:26.
- Singh SJ, Morgan MD, Hardman AE, Rowe C, Bardsley PA. Comparison of oxygen uptake during a conventional treadmill test and the shuttle walking test in chronic airflow limitation. Eur Respir J 1994 Nov;7(11):2016–2020.
- Revill SM, Morgan MD, Singh SJ, Williams J, Hardman AE. The endurance shuttle walk: a new field test for the assessment of endurance capacity in chronic obstructive pulmonary disease. Thorax 1999 Mar;54(3):213–222.
- Singh SJ, Morgan MD, Scott S, Walters D, Hardman AE. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax 1992 Dec;47(12):1019–1024.
- Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982;14(5):377–381.
- Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J. Standardisation of spirometry. Eur Respir J 2005 Aug;26(2):319–338.
- Wang KY, Chiang CH, Maa SH, Shau WY, Tarn YH. Psychometric assessment of the Chinese language version of the St. George's Respiratory Questionnaire in Taiwanese patients with bronchial asthma. J Formos Med Assoc 2001 Jul;100(7):455–460.
- Jones PW, Quirk FH, Baveystock CM. The St George's Respiratory Questionnaire. Respir Med 1991 Sep;85 Suppl B:25–31; discussion 3–7.
- Ferrer M, Villasante C, Alonso J, Sobradillo V, Gabriel R, Vilagut G, Masa JF, Viejo JL, Jimenez-Ruiz CA, Miravitlles M. Interpretation of quality of life scores from the St George's Respiratory Questionnaire. Eur Respir J 2002 Mar;19(3):405–413.
- Man WD, Polkey MI, Donaldson N, Gray BJ, Moxham J. Community pulmonary rehabilitation after hospitalisation for acute exacerbations of chronic obstructive pulmonary disease: randomised controlled study. BMJ 2004 Nov 20;329(7476):1209.
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics 1986 Mar; 42(1):121–130.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010; 340:c332.
- Camillo CA, Laburu Vde M, Goncalves NS, Cavalheri V, Tomasi FP, Hernandes NA, Ramos D, Marquez Vanderlei LC, Cipulo Ramos EM, Probst VS, Pitta F. Improvement of heart rate variability after exercise training and its predictors in COPD. Respir Med 2011 Jul;105(7):1054–1062.
- Thaut MH, Leins AK, Rice RR, Argstatter H, Kenyon GP, McIntosh GC, Bolay HV, Fetter M. Rhythmic auditory stimulation improves gait more than NDT/Bobath training in near-ambulatory patients early poststroke: a single-blind, randomized trial. Neurorehabil Neural Repair 2007 Sep-Oct; 21(5):455–459.
- Thornby MA, Haas F, Axen K. Effect of distractive auditory stimuli on exercise tolerance in patients with COPD. Chest 1995 May;107(5):1213–1217.
- Bauldoff GS, Rittinger M, Nelson T, Doehrel J, Diaz PT. Feasibility of distractive auditory stimuli on upper extremity training in persons with chronic obstructive pulmonary disease. J Cardiopulm Rehabil 2005 Jan–Feb; 25(1):50–55.
- Bauldoff GS, Hoffman LA, Zullo TG, Sciurba FC. Exercise maintenance following pulmonary rehabilitation: effect of distractive stimuli. Chest 2002 Sep; 122(3):948–954.
- Pfister T, Berrol C, Caplan C. Effects of music on exercise and perceived symptoms in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil 1998 May–Jun;18(3):228–232.
- Singh SJ, Jones PW, Evans R, Morgan MD. Minimum clinically important improvement for the incremental shuttle walking test. Thorax 2008 Sep;63(9):775–777.
- Hernandez MT, Rubio TM, Ruiz FO, Riera HS, Gil RS, Gomez JC. Results of a home-based training program for patients with COPD. Chest 2000 Jul; 118(1):106–114.
- Jones PW. St. George's Respiratory Questionnaire: MCID. COPD 2005 Mar; 2(1):75–79.
- Griffiths TL, Burr ML, Campbell IA, Lewis-Jenkins V, Mullins J, Shiels K, Turner-Lawlor PJ, Payne N, Newcombe RG, Ionescu AA, Thomas J, Tunbridge J. Results at 1 year of outpatient multidisciplinary pulmonary rehabilitation: a randomised controlled trial. Lancet 2000 Jan 29;355(9201):362–8.
- Rasekaba TM, Williams E, Hsu-Hage B. Can a chronic disease management pulmonary rehabilitation program for COPD reduce acute rural hospital utilization? Chron Respir Dis 2009; 6(3):157–163.
- van Haren-Willems J, Heijdra Y. Increasing evidence for gender differences in chronic obstructive pulmonary disease. Womens Health (Lond Engl) 2010 Jul; 6(4):595–600.