Abstract
Background Patella resurfacing in total knee arthroplasty is a contentious issue. The literature suggests that resurfacing of the patella is based on surgeon preference, and little is known about the role and timing of resurfacing and how this affects outcomes.
Methods We analyzed 134,799 total knee arthroplasties using data from the Australian Orthopaedic Association National Joint Replacement Registry. Hazards ratios (HRs) were used to compare rates of early revision between patella resurfacing at the primary procedure (the resurfacing group, R) and primary arthroplasty without resurfacing (no-resurfacing group, NR). We also analyzed the outcomes of NR that were revised for isolated patella addition.
Results At 5 years, the R group showed a lower revision rate than the NR group: cumulative per cent revision (CPR) 3.1% and 4.0%, respectively (HR = 0.75, p < 0.001). Revisions for patellofemoral pain were more common in the NR group (17%) than in the R group (1%), and “patella only” revisions were more common in the NR group (29%) than in the R group (6%). Non-resurfaced knees revised for isolated patella addition had a higher revision rate than patella resurfacing at the primary procedure, with a 4-year CPR of 15% and 2.8%, respectively (HR = 4.1, p < 0.001).
Interpretation Rates of early revision of primary total knees were higher when the patella was not resurfaced, and suggest that surgeons may be inclined to resurface later if there is patellofemoral pain. However, 15% of non-resurfaced knees revised for patella addition are re-revised by 4 years. Our results suggest an early beneficial outcome for patella resurfacing at primary arthroplasty based on revision rates up to 5 years.
Early knee arthroplasty designs without patella resurfacing were associated with higher rates of patello-femoral problems including anterior knee pain, patella subluxation, and patella erosion (Insall et al. Citation1976). Aglietti et al. (Citation1975) described the design of a patella component based on the area of articulation and loading in the cadaveric patellofemoral joint.
Resurfacing of the patella at primary surgery has always been a contentious issue, and recent studies remain conflicting. Boyd et al. (Citation1993) suggested that replacement of the patella in patients with osteoarthritis and rheumatoid arthritis prevents early revision. This was supported by Burnett and Bourne (Citation2003) who analyzed results from 5 randomized controlled trials (Schroeder-Boersch et al. Citation1988, Bourne et al. Citation1995, Feller et al. Citation1996, Barrack et al. Citation2001, Wood et al. Citation2002), and showed that of 451 knees having total arthroplasty, 11% without patella resurfacing required revision as compared to 5% of knees with patella resurfacing. Anterior knee pain was the most common complication in the non-resurfaced groups. These results have been supported by other literature suggesting resurfacing of the patella leads to lower rates of revision (Forster Citation2004, Pakos et al. Citation2005, O'Shea et al. Citation2006, Garneti et al. Citation2008) or increased patient satisfaction (Schroeder-Boersch et al. Citation1998, Mayman et al. Citation2003, Waters and Bentley Citation2003, Burnett et al. Citation2004, Gildone et al. Citation2005, Parvizi et al. Citation2005, Berti et al. Citation2006, van Hemert et al. Citation2009). Despite promising results, other studies have suggested that resurfacing of the patella does not change rates of revision, patient satisfaction, or clinical outcome (Grace and Sim Citation1988, Healy et al. Citation1995, Robertsson et al. Citation2000, Wood et al. Citation2002, Citation2005, Burnett et al. Citation2004, Citation2007, Campbell et al. Citation2006, Myles et al. Citation2006, Oztürk et al. Citation2006, Smith et al. Citation2006, Citation2008, Epinette and Manley Citation2008). Most studies to date have been under-powered and the role of patella resurfacing in total knee arthroplasty is not clearly defined.
Whether to resurface the patella at primary surgery or as a subsequent reoperation is also unclear. Surgeons commonly believe that resurfacing as a secondary procedure is as beneficial as resurfacing at the initial operation. Surgeons who choose not to resurface the patella in the primary arthroplasty may consider it easy to resurface the patella later if the patient experiences complications such as patellofemoral pain. However, Khatod et al. (Citation2004) and Muoneke et al. (Citation2003) reported that only half of these patients will have satisfactory results. To date, there has been no literature suggesting that the revision rate is the same when resurfacing at primary surgery or at revision, in the context of total knee arthroplasty.
Much of the literature concerning patella resurfacing in total knee arthroplasty states outcome for osteoarthritis alone (Feller et al. Citation1996, Burnett et al. Citation2004, Campbell et al. Citation2006). Boyd et al. (Citation1993) suggested a beneficial outcome for resurfacing irrespective of the diagnosis. Despite this, there has been no specific comparison of the outcomes of patella resurfacing by diagnosis; thus, the outcome of resurfacing the patella for different diagnoses remains uncertain.
We used data from the Australian Orthopaedic Association (AOA) National Joint Replacement Registry (NJRR) to investigate the use of patella resurfacing in total knee arthroplasty.
Patients and methods
Ethics approval was obtained from the Prince Charles Hospital Human Research and Ethics Committee prior to requesting data.
The purpose of the Commonwealth Government funded AOA NJRR is to improve the quality of care for patients undergoing joint replacement surgery. Similar registries exist in other countries, including the Swedish Knee Arthroplasty Register, which has been in operation since 1976 (Knutson et al. Citation1994). The AOA NJRR commenced data collection in 1999 and has collected full national data since mid-2002, with a greater than 97% capture rate. All 289 hospitals (public and private) currently undertaking joint replacement surgery in Australia provide information to the Registry. The 2007 annual report analyzed 172,349 knee procedures performed between September 1, 1999 and December 31, 2006, of which 134,799 were total knee arthroplasties. Data obtained at the time of surgery include patient details, hospital, type of procedure, joint replaced, side (left or right), diagnosis, and details of all components used. Although some identifying information including names are collected, no patient, surgeon, or hospital is identified in any data released by the AOA NJRR (Graves et al. Citation2004).
The main outcome reported by the registry is time to first revision. As the registry is still in its infancy, data reflect early rates of revision, although the very substantial number of procedures collected make it a valuable source of information to compare outcomes (Graves et al. Citation2004, Robertsson Citation2007).
Statistics
The cumulative per cent revision (CPR) of primary total knee arthroplasty at each of the first 5 years following implant was estimated using the Kaplan-Meier method. Our main interest was to compare revision rates between resurfaced patellas at primary arthroplasty (the resurfacing group, R) and non-resurfaced patellas at primary arthroplasty (the no-resurfacing group, NR). Of secondary interest was the outcome of revision procedures after the primary arthroplasty (R and NR) where the components inserted at the time of revision surgery were the “patella only” or the “patella and insert” (thus excluding “insert only”). Finally, revision rates for R and NR were compared between primary diagnosis of osteoarthritis and all other diagnoses. Here “other diagnosis” refers for example to rheumatoid arthritis, other inflammatory arthritis, avascular necrosis, tumors, and chondrocalcinosis.
Unadjusted CPR values are reported with 95% confidence interval (CI). Adjustment for age and sex was made, where appropriate, when comparing revisions over the entire period, using either log-rank tests or hazards ratios from proportional hazards models as appropriate. All tests were two-tailed at the 5% level of significance.
Descriptive analyses including primary diagnosis, reasons for revision, and type of revision are also reported. Type of revision was categorized into major (involving femoral and/or tibial components) or minor (not involving femoral and/or tibial components).
Analyses were performed using SAS software version 9.1 (SAS Institute Inc., Cary, NC).
Results
Of the 134,799 primary total knee arthroplasties reported in the 2007 annual report, 57,359 (43%) involved patella resurfacing. In the R group, 93% were cemented.
Primary total knee arthroplasty in the R group had a lower revision rate than in the NR group (adjusted HR = 0.75, CI: 0.69–0.80; p < 0.001) (). At 5 years, the CPR of total knee procedures for the R group was 3.1% as compared to 4.0% for the NR group ().
Figure 1. Cumulative percent revision (CPR) of primary total knee arthroplasty by patella resurfacing.
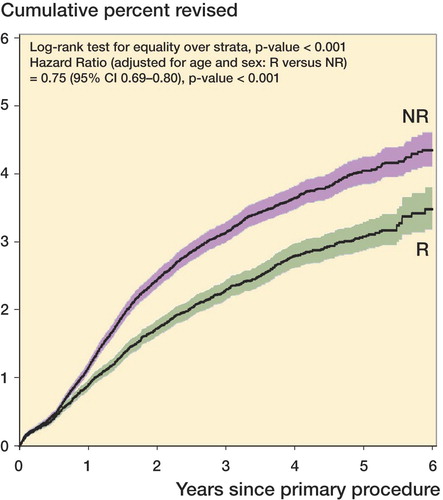
Table 1. Annual cumulative percent revision (CPR) of primary total knee arthroplasty by patella resurfacing
The most common reasons for revision in both groups were loosening and infection. However, in the R group, loosening (36%) and infection (27%) were more common than in the NR group (29% loosening, 19% infection) (). Conversely, in the NR group, patellofemoral pain (17%) and knee pain (13%) were more common reasons for revision than in the R group (1.1% patellofemoral pain, 7.0% knee pain) ().
Table 2. Reason for revision of primary total knee arthroplasty by patella resurfacing
There were 1,092 revisions of knees in the R group, of which 65 were for isolated patella revision (6%) while 626 were for tibia and/or femoral components (57%). Major revisions in the R group constituted 1.2% of all procedures with patella resurfacing. There were 1,979 revisions of knees in the NR group, of which 566 were for isolated patella addition (29%) and 762 for tibia and/or femoral components (39%). Major revisions in the NR group constituted 1.1% of all procedures without patella resurfacing. Patients in the R group showed a higher proportion of major revisions (p < 0.001) while those in the NR group showed a higher proportion of minor revisions (p < 0.001).
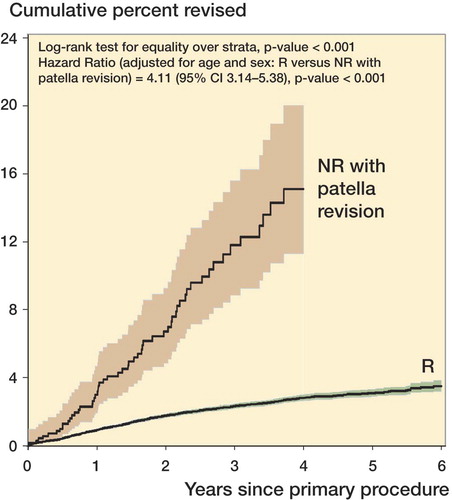
There was a higher CPR in revisions for patella addition in the NR group than in the R group (adjusted HR = 4.1, CI: 3.1–5.4, p < 0.001). At 4 years, the CPR for the R group was 2.8% as compared to 15% for the NR group revised for patella addition (), most (74%) of these being for patellofemoral pain.
Figure 2. Cumulative percent revision (CPR) comparing patella resurfacing at primary surgery with non-resurfacing at primary surgery revised for patella resurfacing
Diagnosis at primary arthroplasty was similar for both groups, with 96% of the R group having osteoarthritis as compared to 97% of the NR group. For the NR group, the 5-year CPR for the diagnosis of osteoarthritis was 4.9% and for other diagnoses it was 4.0% (adjusted HR = 1.1, CI: 0.8–1.2; p = 0.7). For the R group, the 5-year CPR for the diagnosis of osteoarthritis was 3.1% and for other diagnoses it was 2.6% (adjusted HR = 1.7, CI: 1.2–2.4; p = 0.003) (). Other covariates including age at primary procedure, sex, and mean time to revision had no influence on revision rate between the diagnosis groups (data not shown).
Table 3. Type of revision for primary total knee arthroplasty comparing the use of patella resurfacing and no resulfacing
Table 4. Annual cumulative percent revision (CPR) of primary total knee arthroplasty by patella resurfacing and primary diagnosis
Discussion
We used registry data obtained from the AOA NJRR to compare rates of early revision in patients with and without patella resurfacing. We have addressed the pitfall of many previous studies, which lacked sufficient power to show any difference between rates of revision. The strengths of our study include a large sample size, the use of data reflecting current practice, and incorporation of data from many centers both public and private. The limitations of the study are that the only outcome was the rate of revision, while other measures such as Knee Society scores, patient satisfaction, and extensor function were not available. There are also many implant types with different individual variations in design, and as such any discrepancy in outcomes of patella resurfacing from each individual design was not adjusted for. Data from the registry reflect early revisions up to approximately 5 years.
In the recent literature, it has been proposed that revision rates are lower in patients who have received patella resurfacing in total knee arthroplasty (Lindstrand et al. Citation2001, Forster Citation2004, Pakos et al. Citation2005, O'Shea et al. Citation2006, Garneti et al. Citation2008). This was confirmed in our study, as we found that the R group had a lower revision rate than the NR group, with a hazards ratio of 0.75 (p < 0.001).
We found that patients in the NR group were more likely to be revised for patellofemoral pain, and more likely to be revised with isolated patella addition. Surgeons may be more inclined to revise a non-resurfaced knee by secondary patella addition if the patient presents later with knee pain, given that option is still available. While the etiology of anterior knee pain following total knee arthroplasty is not proven, the interplay of forces on the patellofemoral joint is thought to be the culprit (Mochizuki and Schurman Citation1979). However, in patients for whom there are other causes for anterior knee pain (e.g. subclinical infection, component rotation, anatomical abnormality, patella maltracking), a tendency to offer patella addition may not correct the cause of pain or could lead to incorrect treatment and the need for further major re-revision. Sharkey et al. (Citation2002) discussed the concept of failing total knee arthroplasties and pointed out that early failure might be due to a number of mechanisms. In approximately 8% of patients who are generally dissatisfied with their knee arthroplasty (Robertsson et al. Citation2000), the ability to offer a minor revision in the absence of a diagnosis may further increase the rate of early revision.
If a patella is inserted at revision surgery we showed a higher rate of re-revisions than revisions of a knee where the patella was replaced at the primary operation (). The 4-year cumulative per cent revision for NR with patella addition was 15%, with most revisions for loosening and infection requiring major re-revision. These results suggest patella resurfacing is more effective in terms of early revision when performed at the primary arthroplasty rather than at the first revision. We support reports suggesting that isolated patella addition in the non-resurfaced knee is associated with poor clinical outcomes and high rates of re-revision (Berry and Rand Citation1993, Leopold et al. Citation2003, Muoneke et al. Citation2003, Khatod et al. Citation2004), although this is the first study to compare primary and revision outcomes of patella resurfacing.
We identified a statistically significantly higher proportion of major revisions than minor revisions in the R group, and minor revisions compared to major in NR, with a higher proportion of revisions for loosening and infection in the R group than in the NR group. These rates support early data from the Swedish Knee Arthroplasty Register (Robertsson et al. Citation2001). Major revisions tended to occur later in the R group than major revisions in the NR group. Although these results were significant, the difference is probably related to a tendency to offer minor revisions to patients with no resurfacing as mentioned previously, particularly patients who are generally dissatisfied. A relatively simple patella addition is not available for patients with resurfacing, and this being the case surgeons may be inclined to wait and operate later with a major revision. This could account for both the lower proportion of major revisions and the lower proportion of loosening and infection (rather than patellofemoral pain) in the NR. As the registry does not collect data on operation time or the use of other infection control measures, we are unable to report on whether there may be a link between operation time and infection rates for resurfacing of the patella at the primary procedure; however, this is clearly a subject for further research.
It remains to be seen whether early outcome will be similar to long-term outcome. Currently, data are only available for the last 5 years, and the possibility of patella resurfacing having an adverse long-term effect on major components cannot be excluded without continuous data collection and further analysis. In addition, the integrity of the patella and its implanted button is also a long-term issue that remains to be investigated, and patella-related outcomes should be explored when further data become available. Given the close relationship between patella-related outcomes from the Australian and Swedish registries, it is possible that Australian long-term outcome may reflect Swedish long-term outcome. Current data from the Swedish Knee Arthroplasty Register annual report from 2007 show that for patella implants performed since 1996, non-resurfacing is associated with a 1.3-times higher cumulative revision rate than resurfacing in the setting of osteoarthritis, and 1.9-times higher for rheumatoid arthritis. The authors suggested that this is directly related to the need for secondary patella resurfacing because of patellofemoral pain (Robertsson and Lidgren Citation2007). These promising results suggest that the mechanical forces of the patella prosthesis may not affect tibial or femoral components in the medium to long term, and they present an ideal opportunity for follow-up in the future.
Osteoarthritis is currently the major reason for total knee arthroplasty performed in Australia, constituting 97% of initial diagnoses. We found that the 5-year CPR was lower in the R group in the setting of both osteoarthritis and other diagnoses. These values in the setting of other diagnoses (such as rheumatoid arthritis) support data from the Swedish Knee Arthroplasty Register (Robertsson and Lidgren Citation2007); however, generally speaking the published literature has yet to show a difference in outcome for resurfaced patellas in terms of revision rates (Shoji et al. Citation1989, Kajino et al. Citation1997, Moran and Horton Citation2000, Gioe et al. Citation2007). Potentially confounding factors such as age, gender, and mean time to revision had no effect on our results.
Our study defined both “patella only” and “insert and patella” as patella additions, and this took account of surgeons who may have routinely changed the insert at revision. Revision procedures for “insert only” were not part of our analysis. Our data suggest that there was no difference in the revision rate between “insert and patella” revisions and “patella only” revisions, and both “‘insert and patella” and “patella only” in the NR group had a higher revision rate than in the R group (p < 0.001 and p < 0.001, respectively; data not shown).
WC and RC: conceived the study and drafted the manuscript. LM: performed statistical analysis and drafted the manuscript. SW: conceived the study, performed statistical analysis, and drafted the manuscript. SG and PR: drafted the manuscript.
The authors thank the Prince Charles Hospital and the Australian Orthopaedic Association National Joint Replacement Registry.
No competing interests declared.
- Aglietti P, Insall JN, Walker PS, Trent P. A new patella prosthesis. Design and application. Clin Orthop 1975;(107):175-87.
- Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L. Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Joint Surg (Am) 2001;83(9):1376-81.
- Berry DJ, Rand JA. Isolated patellar component revision of total knee arthroplasty. Clin Orthop 1993;(286):110-5.
- Berti L, Benedetti MG, Ensini A, Catani F, Giannini S. Clinical and biomechanical assessment of patella resurfacing in total knee arthroplasty. Clin Biomech (Bristol, Avon) 2006;21(6):610-6.
- Bourne RB, Rorabeck CH, Vaz M, Kramer J, Hardie R, Robertson D. Resurfacing versus not resurfacing the patella during total knee replacement. Clin Orthop 1995;(321):156-61.
- Boyd AD, Ewald FC, Thomas WH, Poss R, Sledge CB. Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg (Am) 1993;75(5):674-81.
- Burnett RS, Bourne RB. Indications for patellar resurfacing in total knee arthroplasty. J Bone Joint Surg (Am) 2003;85(4):728-45.
- Burnett RS, Haydon CM, Rorabeck CH, Bourne RB. Patella resurfacing versus nonresurfacing in total knee arthroplasty: results of a randomized controlled clinical trial at a minimum of 10 years' followup. Clin Orthop 2004;(428):12-25.
- Burnett R, McCarthy KP, Boone JL, Seth R, Robert LB. A prospective, double-blind, randomized, controlled trial of patellar resurfacing in bilateral total knee arthroplasty: A minimum 10-year follow-up study. J Arthroplasty 2007;22(2):306.
- Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, Stevenson TM. Patellar resurfacing in total knee replacement: A ten-year randomised prospective trial. J Bone Joint Surg (Br) 2006;88(6):734-9.
- Epinette JA, Manley MT. Outcomes of patellar resurfacing versus nonresurfacing in total knee arthroplasty. J Knee Surg 2008;21:293-8.
- Feller JA, Bartlett RJ, Lang DM. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg (Br) 1996;78:226-8.
- Forster MC. Patellar resurfacing in total knee arthroplasty for osteoarthritis: a systematic review. The Knee 2004;11(6):427-30.
- Garneti N, Mahadeva D, Khalil A, McLaren CA. Patellar resurfacing versus no resurfacing in Scorpio total knee arthroplasty. J Knee Surg 2008;21(2):97-100.
- Gildone G, Manfredini M, Biscione R, Faccini R. Patella resurfacing in posterior stabilised total knee arthroplasty: a follow-up study in 56 patients. Acta Orthop Belg 2005;71(4):445-51.
- Gioe TJ, Novak C, Sinner P, Ma W, Mehle S. Knee arthroplasty in the young patient: survival in a community registry. Clin Orthop 2007;(464):83-7.
- Grace JN, Sim FH. Fracture of the patella after total knee arthroplasty. Clin Orthop 1988;(230):168-75.
- Graves SE, Davidson D, Ingerson L, Ryan P, Griffith EC, McDermott BFJ, McElroy HJ, Pratt NL. The Australian Orthopaedic Association National Joint Replacement Registry. Med J Aust 2004;180:31-4.
- Healy WL, Wasilewski SA, Takei R, Oberlander M. Patellofemoral complications following total knee arthroplasty. Correlation with implant design and patient risk factors. J Arthroplasty 1995;10(2):197-201.
- Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg (Am) 1976;58(6):754-65.
- Kajino A, Yoshino SI, Kameyama S, Kohda M, Nagashima S. Comparison of the Results of bilateral total knee arthroplasty with and without patellar replacement for rheumatoid arthritis. A follow-up note. J Bone Joint Surg (Am) 1997;79(4):570-4.
- Khatod M, Codsi M, Bierbaum B. Results of resurfacing a native patella in patients with a painful total knee arthroplasty. J Knee Surg 2004;17(3):151-5.
- Knutson K, Lewold S, Robertsson O, Lidgren L. The Swedish knee arthroplasty register. A nation-wide study of 30,003 knees 1976-1992. Acta Orthop Scand 1994;65(4):375-86.
- Leopold SS, Silverton CD, Barden RM, Rosenberg AG. Isolated revision of the patellar component in total knee arthroplasty. J Bone Joint Surg (Am) 2003;85(1):41-7.
- Lindstrand A, Robertsson O, Lewold S, Toksvig-Larsen S. The patella in total knee arthroplasty: resurfacing or nonresurfacing of patella. Knee Surg Sports Traumatol Arthrosc (Suppl 1) 2001;9:21-3.
- Mayman D, Bourne RB, Rorabeck CH, Vaz M, Kramer J. Resurfacing versus not resurfacing the patella in total knee arthroplasty: 8- to 10-year results. J Arthroplasty 2003;18(5):541-5.
- Mochizuki RM, Schurman DJ. Patellar complications following total knee arthroplasty. J Bone Joint Surg (Am) 1979;61(6):879-83.
- Moran CG, Horton TC. Total knee replacement: the joint of the decade. A successful operation, for which there's a large unmet need. BMJ 2000;320(7238):820.
- Muoneke HE, Khan AM, Giannikas KA, Hägglund E, Dunningham TH. Secondary resurfacing of the patella for persistent anterior knee pain after primary knee arthroplasty. J Bone Joint Surg (Br) 2003;85(5):675-8.
- Myles CM, Rowe PJ, Nutton RW, Burnett R. The effect of patella resurfacing in total knee arthroplasty on functional range of movement measured by flexible electrogoniometry. Clin Biomech (Bristol, Avon) 2006;21(7):733-9.
- O'Shea K, Bale E, Murray P. Prospective randomised comparison of patellar resurfacing versus non-resurfacing in primary total knee replacement. J Bone Joint Surg (Br) (Supp I) 2006;88:28.
- Oztürk A, Bilgen S, Atici T, Ozer O, Bilgen OF. The evaluation of patients undergoing total knee arthroplasty with or without patellar resurfacing. Acta Orthop Traumatol Turc 2006;40(1):29-37.
- Pakos EE, Ntzani EE, Trikalinos TA. Patellar resurfacing in total knee arthroplasty. A meta-analysis. J Bone Joint Surg (Am) 2005;87(7):1438-45.
- Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, Mont MA. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop 2005;(438):191-6.
- Robertsson O. Knee arthroplasty registers. J Bone Joint Surg (Br) 2007;89(1):1-4.
- Robertsson O, Lidgren L. Annual Report 2007, The Swedish Knee Arthroplasty Register, Department of Orthopaedics, Lund University Hospital 2007:9-13.
- Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: A report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand 2000;71:262-7.
- Robertsson O, Knutson K, Lewold S, Lidgren L. The Swedish Knee Arthroplasty Register 1975-1997: An update with special emphasis on 41,223 knees operated on in 1988-1997. Acta Orthop 2001;72(5):503-13.
- Schroeder-Boersch H, Scheller G, Synnatschke M, Arnold P, Jani L. Patellar resurfacing. Results of a prospective randomized study. Orthopaedics 1988;27:642-50.
- Schroeder-Boersch H, Scheller G, Fischer J, Jani l. Advantages of patellar resurfacing in total knee arthroplasty. Two-year results of a prospective randomized study. Arch Orthop Trauma Surg 1998;117:73-8.
- Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Why are total knee arthroplasties failing today? Clin Orthop 2002;(404):7-13.
- Shoji H, Yoshino S, Kajino A. Patellar replacement in bilateral total knee arthroplasty. A study of patients who had rheumatoid arthritis and no gross deformity of the patella. J Bone Joint Surg (Am) 1989;71(6):853-6.
- Smith AJ, Lloyd DG, Wood DJ. A kinematic and kinetic analysis of walking after total knee arthroplasty with and without patellar resurfacing. Clin Biomech (Bristol, Avon) 2006;21(4):379-86.
- Smith AJ, Wood DJ, Li MG. Total knee replacement with and without patellar resurfacing: a prospective, randomised trial using the profix total knee system. J Bone Joint Surg (Br). 2008;90(1):43-9.
- van Hemert WL, Senden R, Grimm B, Kester AD, van der Linde MJ, Heyligers IC. Patella retention versus replacement in total knee arthroplasty; functional and clinimetric aspects. Arch Orthop Trauma Surg 2009;129(2):259-65.
- Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty: A prospective, randomized study. J Bone Joint Surg (Am) 2003;85(2):212-7.
- Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK. Patellar resurfacing in total knee arthroplasty: A prospective, randomized trial. J Bone Joint Surg (Am) 2002;84(2):187-93.
- Wood DJ, Smith AJ, Lloyd DG. Clinical outcomes and walking analysis after total knee arthroplasty with and without patellar resurfacing: A prospective randomised trial. J Bone Joint Surg (Br) (Suppl III) 2005;87:338-9.
