Introduction
Total hip arthroplasty
History
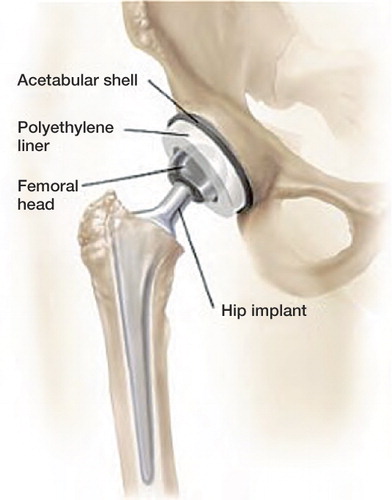
Today total hip arthroplasty (THA) is one of the most common orthopedic procedures worldwide. In total hip arthroplasty the diseased cartilage and bone of the femoral head and acetabulum is replaced with an artificial ball joint, which includes a stem inserted into the femur with a ball on the top and an artificial acetabular socket with a liner inside. These three parts are referred to as the prosthesis or arthroplasty ().
The most common reason for primary THA surgery is primary osteoarthritis accounting for more than 75% of patients treated with a THA (Pedersen et al. Citation2005). Other reasons include fresh fracture of the femoral neck, late sequelae from fracture of the proximal femur, acetabular fracture, traumatic hip dislocation, atraumatic necrosis of the femoral head, rheumatoid arthritis, Mb. Bectherew, congenital hip dislocation, Mb. Calve-Legg-Perthes, epiphysiolysis, and acetabular dysplasia. Primary THA surgery is usually considered when conservative treatment including pain medication and physiotherapy is insufficient.
The evolution of the modern THA was started in 1960 by the English surgeon Sir John Charnley (Charnley, Citation1961). He introduced the Charnley Low-friction total hip arthroplasty where he replaced the acetabular component with polyethylene, whereas the femoral component was made of metal. The combination of polyethylene and a small 22 mm diameter femoral head reduced the wear rates. These improvements to THA not only provided pain relief and improved hip function in patients, but also decreased the failure rates due to loosening of the implant, thus refining THA surgery to a truly successful operation in orthopedic surgery (Charnley and Cupic, Citation1973). The Charnley prosthesis is still one of the most frequently used THAs (Garellick et al. Citation1998, Malchau et al. Citation2002).
The burden of THA surgery
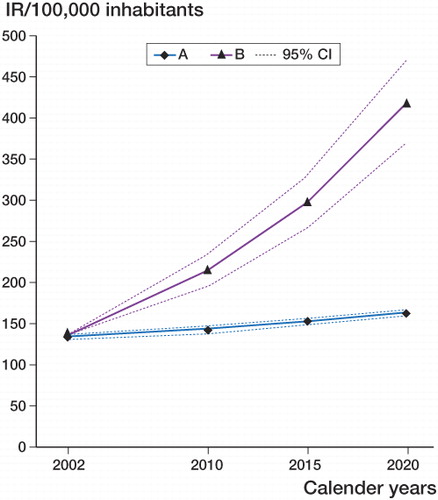
The crude incidence rates of primary THA procedures in Europe, United States, Canada and Australia differ substantially (Merx et al. Citation2003). However, the annual number of THA procedures is consistently rising worldwide due to improved surgical techniques and an ageing population (Wells et al. Citation2002). In Denmark the incidence rates of primary THA procedures were 101 and 131 per 100.000 inhabitants in 1998 and 2002 respectively. From 2002 to 2020 the expected future demands of THAs in Denmark have been estimated to increase with between 22% and 210% () (Pedersen et al. Citation2005). As a consequence the incidence rates for revisions will also increase in the future. Such a development will represent a serious economic challenge for the health care system. Therefore, factors that can improve the prognosis after primary THA are both a public health and economical priority.
Figure 2. Expected incidence rates (IRs) of primary THAs in Denmark in the years 2010, 2015, and 2020, based on constant age-specific IRs of primary THAs (2002) A: with expected changes in age distribution, B: with expected changes in age distribution combined with the continued annual age and sex-specific increase in the standardized IRs of primary THA based on figures from 1996–2002 (Pedersen et al. Citation2005).
Prognostic factors for primary THA outcome
Traditionally the primary outcome of interest in studies on THA prognosis has been implant failure. Implant failure is defined as a situation where a part of or the whole implant is removed and exchanged in a revision procedure (Lucht, Citation2000). Further, much focus has been on the specific indications for revision of which aseptic loosening of either the acetabular cup or femoral stem is the most frequent. Other important indications for revision include deep infection, dislocation, periprosthetic femoral fracture, pain, osteolysis/granuloma formation, and a number of miscellaneous causes.
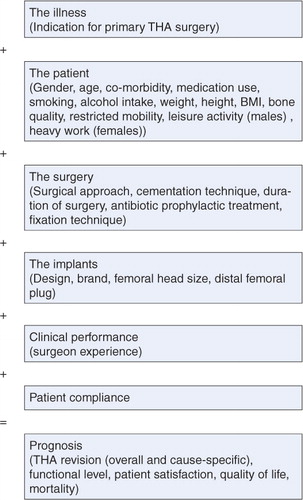
Prognosis is a prediction of the course of disease following its onset (Fletcher and Fletcher, Citation2005). In this thesis prognosis relates to the prediction of the course after primary THA surgery. Prognostic factors are conditions that are associated with an outcome of the disease (primary THA), and they help to identify groups of patients with the same disease but different outcomes. Although the majority of these factors are able to predict implant failure, they are not necessarily the direct cause of failure. presents a comprehensive model of prognostic factors.
Studies of prognosis are important for the clinician to predict, understand and change the outcomes of disease. But prognostic factors are also important to patients who want to know how they can improve their prognosis. Further, studies of prognosis are important to health policy makers in order to ensure appropriate allocation of resources.
Patient-related prognostic factors
The overall failure rates after primary THA surgery have been reported to vary between 5–20 % after 5–15 years of follow-up after primary THA (Maloney, Citation2001, Furnes et al. Citation2001). However the quality of primary THA in terms of implant survival has been improving during the last decades. Research on implant design and surgical technique has traditionally received a lot of interest within orthopedic surgery and the improvements in prognosis have therefore also primarily been ascribed to technical improvements (Herberts and Malchau, Citation1997, Herberts and Malchau, Citation2000). In contrast there have not been paid much attention to patient-related prognostic factors of implant failure and as a consequence the information on patient-related prognostic factors after THA surgery is limited. However, basic characteristics of patients such as age, gender, reason for primary THA, and comorbidity index have been reported as prognostic factors in THA surgery in a number of studies (Malchau et al. Citation1993, Furnes et al. Citation2001, Flugsrud et al. Citation2002, Nercessian et al. Citation2003, Older, Citation2002) (Johnsen et al. Citation2006, Thillemann et al. Citation2008). Lifestyle factors such as smoking, alcohol intake, and level of activity have so far only been examined in relation to the prognosis after THA surgery in one study (Espehaug et al. Citation1997). This study was a case control study from the Norwegian Arthroplasty Registry, which also reported on the association between use of a range of medications and the risk of early THA revision (Espehaug et al. Citation1997). The study was conducted as a mail survey where patients filled in the form at the time of follow-up. Use of anti-diabetic drugs, systemic steroids, local pulmonary steroids, NSAIDs, and analgesics were all associated with an increased risk of implant failure. Furthermore, in relation to failure due to specific causes, patients who were treated with antibiotics for at least one month (not necessarily due to signs of infection in the hip) in the follow-up period had an increased risk of implant failure due to infections (Espehaug et al. Citation1997).
At present this is to our knowledge the only study that has evaluated use of medications in relation to implant failure after primary THA. The study was limited by recall bias as knowledge of the outcome may have influenced the classification of drug use. Recall bias may be an issue although it most likely is minor, as patients were to report their actual drug use. Further, the study only reported prognostic factors for early revision risk. Further studies of medication use in THA surgery is therefore of in high demand.
Research techniques in THA surgery
Since the introduction of the total hip arthroplasty (THA) in 1960, many alternative prostheses have been introduced. In 1994, 62 different THA designs were identified on the British market alone, and of these, only 21 had been evaluated in studies published in peer-reviewed journals (Murray et al. Citation1995). This situation was disturbing since it was likely that there were variation in effectiveness and safety between such a large number of products. The need for further research in THA was essential.
Traditionally, orthopedic procedures have been evaluated by means of case series, and this is particularly true for alternative hip prostheses (Morris, Citation1988). Case series may be helpful as a hypothesis generating tool, but the lack of a reference group makes it impossible to do direct comparisons between different implants based on these studies. Case series often represent single center or single surgeon results with differences in the selection of the patients and definition of outcome and are therefore also often limited by uncertain generalizability.
It is widely recognized that randomized controlled trials (RCT) are the gold standard for evaluation and comparison of implants in terms of efficacy, efficacy describing the extent to which an implant produces a beneficial result under ideal conditions. RCTs should be used when appropriate, practical, and ethical (Black, Citation1996). However, RCTs are also associated with several limitations when the outcome of interest is implant survival after THA, which is a relatively infrequent outcome that requires a large study population in order to obtain results of sufficient precision. RCTs are in this context often not a realistic option as they due to high costs are inappropriate for evaluating interventions that are designed to prevent rare outcomes occurring over a long follow-up period such as implant failure after THA. Finally, RCTs may have problems with the external validity because they often present single center studies of selected patients who are offered a level of care which not necessarily reflect everyday practice.
The hip arthroplasty registers were developed to function as a surveillance tool to identify inferior implants as early as possible. Register-based observational studies may assess effectiveness, i.e. the extent to which THA fulfills its objective in routine clinical settings. For practical purposes, effectiveness may be a more relevant measure in THA research than efficacy as measured in RCTs. Further, observational studies may also provide important information on patient safety, quality of care and prognosis. The use of clinical registers in THA research has in general a number of advantages: 1) clinical registers provide timely and early dissemination of information on outcome of THA surgery; 2) large sample sizes of unselected patients give high precision of estimates and ensures external validity; 3) the costs of observational studies based on clinical studies may be reduced considerably; and 4) collection of information in clinical registers is done prospectively and therefore independently of outcome, reducing the risk of information bias.
The first register on THA surgery was the Swedish Arthroplasty Register, which started registration in 1979 as a response to the many new types of implants that had been introduced without documentation from clinical studies. With the establishment of a nationwide register, it was possible to conduct comparative outcome studies in THA surgery to provide for a more scientific choice of implant technology. Subsequently, hip arthroplasty registers have been initiated in a number of countries, including Norway, Denmark, Finland, Australia, and the United Kingdom.
Medication use and prognosis following THA
In THA surgery close on 80% of patients are older than 60 years, thus many of these patients are suffering from chronic medical diseases for which they are taking medicine. However, there is only limited information on the implications of medical treatments on the implant survival after primary THA surgery although, it is recognized that commonly used drugs in this age affects bone metabolism or bone remodeling.
In this Thesis we focus on statins, thiazid diuretics, loop diuretics, and bisphosphonates which all have well-described effects on bone.
Literature search
PubMed literature was reviewed using MeSH terms “hip arthroplasty” with “statins”, “loop diuretics”, “thiazid diuretics” and “bisphosphonates”, respectively. Further, we reviewed the PubMed literature using MeSH terms “bone” with “statins”, “loop diuretics”, “thiazid diuretics” and “bisphosphonates”, respectively. Finally the Pub Med literature was reviewed using MeSH terms “fracture” with “statins”, “loop diuretics”, “thiazid diuretics” and “bisphosphonates”, respectively. Additional articles not obtained in the primary search were identified by assessment of literature referenced in the reviewed articles.
Study I: Statins
Today, statins are widely used drugs that effectively reduce the risk of cardiovascular events (LaRosa et al. Citation1999). Statins are hydroxymethylglutaryl-CoA reductase inhibitors (HMG-CoA reductase inhibitors) that inhibit the rate limiting step in the mevalonate pathway, thus inhibiting cholesterol synthesis in the liver. As a result of less produced cholesterol in the liver serum cholesterol is lowered.
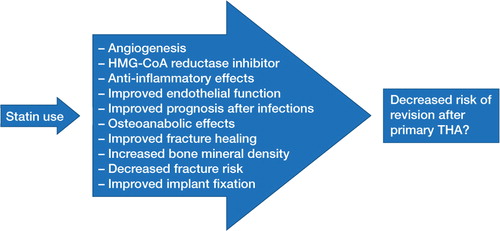
The mevalonate pathway is ubiquitous in nature and involved in many crucial cellular reactions. It is perhaps therefore not surprising that statins have been associated with pleiotropic effects. Consequently statins have been associated with angiogenesis, anti-inflammatory effects, and improved endothelial function among others (Bellosta et al. Citation2000). Further statins have been associated with improved prognosis after infections (Mortensen et al. Citation2005, Mortensen et al. Citation2008, Thomsen et al. Citation2008, Almog et al. Citation2004). These effects may play a role in implant survival after primary THA surgery (.). However, statins have also been associated with changes in bone metabolism, which will be discussed in more detail as it may be more relevant in relation to implant durability after THA surgery.
The first evidence that statins could be beneficial to bone was reported by Mundy et al. in Citation1999. They demonstrated that statins stimulate in vivo bone formation in rodents and increased new bone volume in cultures from mouse calvarias (Mundy et al. Citation1999). In essence an anabolic effect on bone in an experimental study was demonstrated and since then evidence on statins effects on bone metabolism have been growing. The anabolic effect of statins on bone was confirmed in a study on rats that showed an increase in cancellous bone mass and increase in cancellous bone compressive strength in animals treated orally with statins compared to the control group (Oxlund et al. Citation2001). Further, transdermal application of lovastatin in rats also proved to increase bone formation rates and bone volume as measured by bone mineral density and quantitative histomorphometry (Gutierrez et al. Citation2006). In contrast simvastatin was unable to prevent bone loss caused by ovariectomy in rats (Maritz et al. Citation2001).
Statins effects on fracture healing in rodents have also been addressed in experimental studies. One study reported improved fracture healing in mice treated orally with simvastatin in terms of a larger transverse area of the callus and improved mechanical properties (Skoglund et al. Citation2002). However, the animals were treated in doses that were exceedingly high. These high dosages are not acceptable for patients. Consequently, studies on topical application of statins have been performed. These studies are consistent and report likewise improved fracture healing in rodents treated with statins topically (Skoglund and Aspenberg, Citation2007, Wang et al. Citation2007, Garrett et al. Citation2007).
Shortly after the first evidence of statins osteoanabolic effects, the first observational studies on humans followed. A case control study in osteoporotic women over 60 years of age in the USA showed that regular use of statins in a two year period was associated with a more than 50% reduction in non-pathological fracture risk (Chan et al. Citation2000). Similarly long-term statin use was associated with 48% reduction in vertebral fracture risk in a prospective cohort study from Rotterdam (Schoofs et al. Citation2004). Further, observational studies from Denmark supported the association between statin treatment and reduced overall fracture risk and risk of hip fractures (Rejnmark et al. Citation2004, Rejnmark et al. Citation2006c). The results from available observational studies and trials have, however been conflicting. Hence, Ray et al observed a protective effect of both statins and non-statin lipid lowering drugs on the risk of hip fracture and they explained their findings by unmeasured confounding factors (Ray et al. Citation2002). Furthermore, a case control study in more than 160.000 patients aged 50 years or older in the United Kingdom reported no reduction in risk of fractures in statin users (van Staa et al. Citation2001). Similarly, a secondary analysis of the randomized controlled LIPID trial did not find any reduce the risk of fractures among patients randomized to statin treatment (Reid et al. Citation2001).
Similarly, the potential beneficial effects of statin treatment on bone mineral density have been conflicting. However, in a meta-analysis it was concluded that statin use was associated with a moderate increase in bone mineral density in the hip but not in the spine (Uzzan et al. Citation2007).
A part from the potential osteoanabolic effect of statin treatment more implant specific experimental studies have been performed. In rats treated with a titanium implant topically applied fluvastatin increased the peri-implant bone formation measured by histomorphometry and increased the mechanical properties compared to the control group (Ayukawa et al. Citation2004, Moriyama et al. Citation2008). This indicated that statins may improve osseosintegration of titanium implants. Moreover, experimental studies have described positive effects of statins on conditions mimicking the course of aseptic loosening of orthopaedic implants (von Knoch et al. Citation2005a, Laing et al. Citation2008).
In conclusion, many factors that may potentially affect the implant survival after primary THA have been elicited. However no studies on humans have evaluated statin treatment in the context of implant failure after primary THA surgery.
Study II: Thiazid and loop diuretics
Thiazid diuretics
Diuretics, including thiazid and loop diuretics, are widely used drugs for treatment of hypertension and congestive heart failure.
Thiazid diuretics reduce the renal calcium excretion, without reducing intestinal calcium absorption, thereby shifting external calcium balance in a positive direction. It has therefore been proposed that thiazid diuretics affects bone metabolism in an osteoprotective manner (Rose, Citation1991, Rejnmark et al. Citation2003). Experimental studies have shown that thiazid diuretics exert direct effects on bone cells by altering intracellular calcium regulation and increasing osteocalcin secretion in osteoblast like cells (Barry et al. Citation1997, Aubin et al. Citation1996). Further, thiazid diuretics directly inhibited osteoclastic bone resorption in an in vitro model (Hall and Schaueblin, Citation1994). These potentially beneficial effects of thiazid diuretics on bone have also been addressed in several large observational studies. Several of these studies have reported a protective effect of thiazid diuretics on the risk of hip fractures and that the risk reduction was dose and duration dependent (Jones et al. Citation1995, Herings et al. Citation1996, Rejnmark et al. Citation2005b). Further, Schoofs et al. (Citation2003) reported that thiazid use was associated with reduced fracture risk although not in a dose dependent matter and that the association disappeared 4 months after use was discontinued. Moreover, another observational study reported that only recent thiazid diuretic use was associated with decreased fracture risk (Felson et al. Citation1991). Only one study did not find any protective association between thiazid diuretic use and the risk of fracture (Heidrich et al. Citation1991).
Furthermore, concerning osteoprotective effects, thiazid diuretics have also been associated with an increased skeletal mineral density as well as hip bone mineral density in randomized controlled trials. However, only a modest effect on bone mineral density was reported and that is after more than 2 years of thiazid treatment (Bolland et al. Citation2007, Reid et al. Citation2000, LaCroix et al. Citation2000). This finding was confirmed in a observational study that reported an increased bone mineral density in 70 year old women (Sigurdsson and Franzson, Citation2001).
In conclusion, the literature provides evidence of a beneficial effect of thiazid diuretics effects on bone but no studies have evaluated thiazid use in relation to survival of orthopedic implants.
Loop diuretics
Unlike thiazid diuretics, loop diuretics increases the renal calcium excretion (Rose, Citation1991). Consequently, loop diuretics may change bone metabolism. However, studies have provided diverging results. The first evidence of loop diuretics effect on bone came in 1991 where an observational study reported an adjusted 3.9-fold increased risk of hip fracture in users of loop diuretics (Heidrich et al. Citation1991). Several follow-up studies and case control studies have later on confirmed these results (Tromp et al. Citation2000, Rejnmark et al. Citation2006b, Partanen et al. Citation2002). In contrast, other studies showed no association between loop diuretic use and the risk of fractures, and it was recently suggested that differences in health may explain earlier results of increased fracture risk in users of loop diuretics (Carbone et al. Citation2009). However, a RCT have reported a decreased bone mineral density in patients treated with loop diuretics along with increased bone turnover in terms of increased biochemical bone resorption markers (Rejnmark et al. Citation2006a). Another RCT in 40 healthy postmenopausal women also reported a dose dependent increased bone turnover in subjects treated with loop diuretics (Rejnmark et al. Citation2003). Further evidence of loop diuretics potential harm full effects on bone have been reported in a cohort study among older men. Bone mineral density was measured, and it was found that use of loop diuretics was associated with increased rates of hip bone loss after 4.6 years of follow-up (Lim et al. Citation2008). However, a previous cross sectional study from the same cohort did not find any association between use of loop diuretics and decreased bone mineral density. Furthermore, two other cross sectional studies, showed diverging results concerning the association between loop diuretic use and bone mineral density in healthy elderly women (Ooms et al. Citation1993, Rejnmark et al. Citation2005a). Although reports are conflicting, evidence of loop diuretics potential harmful effect on bone remains. In conclusion, no previous studies have examined whether these harmful effects on bone are sufficient to impair the results after hip arthroplasty surgery.
Study III: Bisphosphonates
Bisphosphonates are the primary treatment against osteoclast mediated bone loss due to osteoporosis, Paget's disease, malignancies, multiple myeloma, and hypercalcemia of malignancies. Further bisphosphonates are used in the treatment of diseases characterized by low bone mineral density such as osteogenesis imperfecta (Drake et al. Citation2008). At a tissue level bisphosphonates inhibit bone resorption, bone turnover, and therefore bone loss. At a cellular level bisphosphonates inactivate osteoclastic bone resorption directly or/and indirectly (Rodan and Fleisch, Citation1996).
Due to these beneficial effects on bone metabolism, bisphosphonates are responsible for an increased bone mineral density and decreased risk of fractures in patients with osteoporosis (Liberman et al. Citation1995, Lyles et al. Citation2007). Bishosphonates is thus a well-established treatment in osteoporosis.
However, the antiresorptive properties of bisphosphonates have also shown encouraging results in the context of THA surgery.
Experimental studies have indicated that bisphosphonates applied topically as well as systemically improve early osseosintegration, fixation and mechanical stability of implants. These are all factors that may improve implant survival (Tanzer et al. Citation2005, Bobyn et al. Citation2005, Peter et al. Citation2005, Eberhardt et al. Citation2006). Although findings are conflicting, many RCTs have reported beneficial effects of bisphosphonates on periprosthetic bone mineral density and decreased stress shielding after primary THA (Yamaguchi et al. Citation2003, Yamasaki et al. Citation2007, Venesmaa et al. Citation2001, Fokter et al. Citation2005, Arabmotlagh et al. Citation2006). This increase in bone mineral density may even persist years after discontinuation of bisphosphonates treatment (Arabmotlagh et al. Citation2006).
Wear debris particles from the implants is a major factor in the process of aseptic loosening as the particles induce osteoclast mediated periprosthetic bone resorption. This particle induced periprosthetic osteolysis was inhibited by bisphosphonates in experimental studies in dogs (Shanbhag et al. Citation1997, Millett et al. Citation2002, von Knoch et al. Citation2005b, Wedemeyer et al. Citation2005). However, in a clinical setting of patients with demonstrated aseptic loosening who were awaiting revision surgery, six months treatment with bisphosphonates did not alter the need for revision surgery (Lyons et al. Citation2009). This has also been described in an experimental canine study suggesting that short-term treatment with bisphosphonates is not the solution to already loose implants (Soballe et al. Citation2007).
Furthermore, clinical studies have demonstrated that peri-operative treatment with bisphosphonates, either topically or systemically, was effective in reducing tibial component migration (Hilding et al. Citation2000, Hilding and Aspenberg, Citation2006, Hilding and Aspenberg, Citation2007). Postoperative migration in total joint replacements is a predictor for late revision due to loosening of implants (Karrholm et al. Citation1994, Ryd et al. Citation1995). Therefore, authors proposed that oral clodronate in the peri-operative period might also decrease migration in total hip arthroplasties and thus reduce risk of revision due to loosening of implants.
In conclusion, there is today a lot of evidence of potential beneficial effects of bisphosphonates on implant failure. Therefore bisphosphonates have also been proposed as a treatment that potentially could improve durability of hip replacements (Shanbhag, Citation2006). However, to date the effects of bisphosphonates on THA surgery have not been studied with revision surgery as the primary endpoint.
Aims of Thesis
This thesis presents three pharmaco-epidemiological studies based on data from the Danish Hip Arthroplasty Register (DHR) focusing on drug use and its association with prognosis after primary THA surgery. The specific aims of thesis were:
To examine the association between uses of statins in the postoperative period and the risk of implant failure following primary THA.
To examine the association between use of loop and thiazid diuretics in the postoperative period and the risk of implant failure following primary THA.
To examine the association between uses of bisphosphonates in the pre- and postoperative period and the risk of implant failure following primary THA.
Materials and Methods
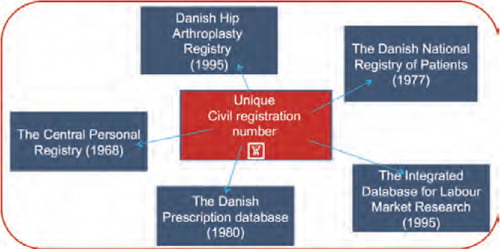
In Denmark the National Health Service provides tax-supported healthcare for all inhabitants, allowing free access to general practitioners and hospitals. In addition, reimbursement is provided for a part of the costs of prescribed drugs, including statins, thiazid diuretics, loop diuretics and bisphosphonates. Through the use of the civil registration number, which is unique to every Danish citizen and encodes sex and date of birth, unambiguous linkage between population-based registers can be made.
In the Danish healthcare system, the responsibility for financing, planning, running and management of hospitals lies within five regions. The Danish health care provides free medical care, including both emergency and other admissions to hospitals and outpatient clinics, after referral from the general practitioner. More than 95% of patients are registered with one practitioner of their choice. After referral from the general practitioner, patients have free hospital choice in the entire country, which also includes some of the private hospitals.
Data sources
The following data sources were used:
The Danish Hip Arthroplasty Registry
The DHR is a nationwide clinical database that was established January 1 1995 with the purpose of improving the quality of both primary and revision total hip arthroplasty surgery in Denmark (Lucht, Citation2000). All orthopaedic departments (n=45) report to the register, including 8 departments located on private hospitals. The registration of primary THA and revisions in the DHR is compulsory for all public and private clinics. Pre-, intra- and postoperative data are collected prospectively using standardized forms. The intra-operative data are filled in by the operating surgeon immediately after the surgery. The DHR has been validated and the quality of data found to be high (Pedersen et al. Citation2004)
The following preoperative data is registered: the civil registration number, the laterality of the affected hip, previous surgery on the same hip, primary diagnosis, hospital code, and function according to Charnley (Charnley, Citation1972). In addition departments can register the Harris Hip Score as a measure of hip function and the patient´s mobility before surgery (Harris, Citation1969). The peri-operative data include: date of surgery, the surgeon´s code number, type of operation gowns and theatre, use of antibiotic and antithrombotic prophylaxis treatment, type of anaesthesia, prophylaxis against ectopic bone formation, duration of surgery, surgical approach and method, trochanteric osteotomy, type of femoral head component and fixation, transplantation of bone to the acetabulum and/or femur, peri-operative complications, material and diameter of the femoral head, and material type of liner. In case of revision, defined as exchange of a part of or the whole prosthesis or removal of the prosthesis, the following is registered: cause of revision, previous surgery, extent of revision, the number of earlier revisions, and classification of bone loss related to revision of acetabular and/or femoral component. The postoperative data, including the personal identification number, laterality of the hip, date of the latest surgery, date of follow-up examination, status at the follow-up examination, hospital code, function according to Charnley, postoperative complications, patient´s own assessment of the satisfaction with the surgery and Harris Hip Score are registered at the follow-up examination. Because of the lack of general guidelines about the use and timing of follow-up examination, patients can be followed for only few months or several years after THA depending on the specific hospital's protocol.
The registry has published annual reports on the registry website http://www.dhr.dk since 2004.
The Danish Register of Medicinal Product Statistics
Data on outpatient drug prescriptions since January 1. 1995 are available from the nationwide prescription database maintained by the Danish Medicine Agency. All pharmacies in Denmark are equipped with a computerized accounting system, which sends key data on outpatient drug prescriptions redeemed by the patient directly to the prescription database. Using the personal identification number, we were able to obtain the complete history of redeemed prescriptions of each study patient from January 1. 1995 to December 31. 2005. The registry holds information on age, sex, information on the dispensed drug (ATC-code, name, package size, formulation and quantity) and date of transaction.
The Integrated Database for Labour Market Research
The Integrated Database for Labour Market Research contains information on each Danish citizen's socioeconomic status including data on gross income, employment status and marital status since 1980. The data in the Integrated Database for Labour Market Research are based on other registries in Statistics Denmark such as the central person registry, the registry from the tax authority, and the registry regarding unemployment (CRAM).
The database is maintained by the Statistics Denmark (Frank, Citation2000).
The National Registry of Patients
The National Registry of Patients, holds data on all discharges from public somatic hospitals in Denmark since 1977 (Andersen et al. Citation1999), including dates of all admissions and discharges, and up to 20 diagnoses for every discharge, as well as surgical procedures performed. The diagnoses have been classified according to the Danish version of the International Classification of Diseases 10th edition since 1994. All discharge diagnoses are assigned by the physician who discharges the patient. Using the National Registry of Patients it is possible to construct the complete hospitalisation history for each patient.
The Civil Registration System
All Danish citizens are assigned a unique 10-digit personal identification number at birth, which is used in all public registries. The Civil Registration System keeps records on changes in vital status of all Danish citizens including changes in address, date of emigration and the date of death since 1968. Unambiguous record linkage on individual-level between public Danish registers is possible due to the personal identification number.
Study populations
All studies were designed as nested case-control studies based on prospectively collected data from the Danish Hip Arthroplasty Register and the above-mentioned registers ().
Study I and II included all primary THA procedures performed in the period between January 1 1996 and December 31 2005 (n=57581), we excluded patients who were not residents in Denmark or changed their civil registration number (n=213) and therefore could not be properly followed up.
Study III included all osteoporosis patients from the Danish Hip Arthroplasty Register treated with a primary THA in the period between January 1, 1996 and December 31, 2006 (n=16145). We defined osteoporosis patients as patients with a diagnosis from the National Registry of Patients of either osteoporosis or osteoporotic fracture before primary THA surgery. Osteoporotic fractures were defined as a vertebral fracture, proximal humeral fracture, forearm fracture or hip fracture at the age of 50 years or older and before the date of primary THA.
Identification of THA cases with revision
Information on revision status is obtained from the Danish Hip Arthroplasty Register. The laterality of the relevant hip is registered both for primary THA and revision which ensures accordance between primary and revision surgery.
In study I and II, we identified a total of 2512 cases of primary THA which sustained revision during the study period. In study III we identified 633 cases from the study population of osteoporosis patients with a primary THA who sustained revision during the study period.
In all studies the primary outcome was revision defined as partial or complete removal or exchange of the implant components. Patients were followed until revision, death, emigration or 31. December 2006. Information on revision of primary THA was available in the source population with a previously reported completeness of 90.1% (Pedersen et al. Citation2004).
Secondary outcomes in study I were revision due to specific causes, i.e. deep infection, aseptic loosening of one or both of the components, periprosthetic fracture, dislocation, pain, implant failure and miscellaneous. Miscellaneous included anisomelia, ectopic bone formation and technical problems.
In study II the secondary outcomes were cause-specific revision, i.e., deep infection, aseptic loosening of one or both of the components, periprosthetic fracture, dislocation of THA and miscellaneous. Miscellaneous included, pain, implant failure, anisomelia, ectopic bone formation and technical problems.
In study III secondary outcomes were cause-specific revision, i.e., deep infection, aseptic loosening of one or both of the components, and dislocation of THA.
Identification of THA controls without revision
In all studies we sampled controls using the incidence-density matching technique, which involves matching each case to a control sample of those who are at risk at the same time of case occurrence. This matching design enables cases and controls to be matched on time at risk. The same individual can serve as a control for more than one case and a control that subsequently are revised can also serve as a case. By using the incidence density matching technique unbiased estimates of the relative risk is obtained (Wacholder et al. Citation1992).
In study I we aimed to identify one primary THA without revision as a control. Statin users may be “healthy users” as younger, better educated, and socioeconomically more privileged people may be more likely to seek and use preventive treatments than frail people (Glynn et al. Citation2006)”. In order to account for any “healthy user” effects we used propensity matching (Greedy method) when sampling controls in order to ensure that cases and controls were equally balanced on baseline predictors for statin use (Marcelo Coca-Perraillon, Citation2007). The propensity score was estimated for all THA procedures registered in the Danish Hip Arthroplasty Register by logistic regression. The following variables associated with the probability of statin use were included in the propensity model: sex, age, year of primary THA surgery, marital status (widow(er), divorced, married and single), education (vocational training, basic school, higher education 1–2 years, 2–4 years and >4 years), gross income (<20.000$, 20–30.000$, 30–50.000$ and >50.000$), county of residence, co-morbid chronic diseases (i.e. included as the 19 groups of chronic diseases used in the Charlson co-morbidity index (Charlson et al. Citation1987)) and current use of other medication (i.e., having redeemed a prescription within 90 days before the date of primary THA for the following drugs associated with statin use: platelet inhibitors, warfarin, ACE inhibitors and AT-II antagonists, beta blockers, calcium channel blockers, diuretics, anti-arrhythmia, non-statin lipid lowering drugs, NSAIDs and hormone replacement therapy). The propensity score matching decreased the absolute standardized differences of each covariate to values below 0.1 indicating that an adequate balance was achieved. In total, we were able to identify an appropriate control for 2349 cases (93.5%).
In study II and III we aimed to identify two unique controls (THA patients who did not undergo revision) for each case with revision.
In study II controls were matched on age at primary THA, gender and year of primary THA operation. We were able to match 2491 revised patients to 4943 unique non-revised primary THA patients. 39 Cases were matched to only one control. We excluded 21 unmatched revised patients. In study III controls were matched on age at primary THA (± 1 year), gender and year of primary THA operation (±1 year). We were able to match 632 revised patients to 1264 unique non-revised primary THA patients. We excluded one unmatched revised patient.
Drug use
In all studies we defined postoperative use of the particular drug as having redeemed at least one prescription of the particular drug in the period from primary THA until revision for cases or censoring for controls. Non-users of a particular drug were for all three studies defined as cases and controls that had not redeemed a prescription of the drug in question for a period of one year before primary THA to revision or censoring.
Study I: Data on all prescriptions for statins redeemed by cases and controls in the postoperative period were obtained. The average length of a statin prescription in Denmark is approximately 90 days. For dose response analysis we therefore used the number of redeemed prescriptions to define the categories of estimated postoperative length of statin treatment: 3 months to 1 year (1–4 prescriptions), 1–2 years (5–8 prescriptions), 2–3 years (9–12 prescriptions) and more than 3 years of treatment (more than 12 prescriptions).
Study II: Data on all prescriptions for thiazid and loop diuretics redeemed by cases and controls in the postoperative period were obtained. The average length of a diuretic prescription in Denmark is approximately 90 days. For dose response analysis we therefore used the number of redeemed prescriptions to define the categories of estimated postoperative length of thiazid and loop diuretic treatment: three months to one year (one to four prescriptions), and more than one year (more than four prescriptions).
Study III: The prognostic factor of interest was postoperative use of bisphosphonates. We further subdivided postoperative use into nitrogen and non-nitrogen containing bisphosphonates which are more and less potent inhibitors of osteoclastic bone resorption, respectively (van Beek et al. Citation2003). Finally, in order to study dose-response association we classified duration of postoperative use of bisphosphonates into defined daily dosages (DDD) according to the definition by the World Health Organisation (http://www.whocc.no/atcddd/). We categorized bisphosphonates use into patients who redeemed 14–120 DDD, 120–240 DDD, and more than 240 DDD in the postoperative period.
Covariates
In all three studies we included a number of covariates in the analysis because of their potential association to the risk of revision.
We included information on the following covariates: Sex, age, fixation technique (i.e. cemented, uncemented and hybrid), diagnosis for primary THA, and year of primary THA were obtained from the Danish Hip Arthroplasty Register.
Socio-demographic data including marital status, education, gross income, and county or region of residence was obtained from The Integrated Database for Labour Market Research.
Information on drug use in the postoperative period was obtained from the Danish Register of Medicinal Product Statistics. We included 13 categories of therapeutic drugs other than the drug at exposure.
From the National Registry of Patients we obtained data on co-morbidity at the time of surgery. Co-morbidity was assessed by computing the Charlson co-morbidity index (Charlson et al. Citation1987). The index applies a weighting of 1, 2, 3 or 6 points to each of the 19 disease categories according to their impact on patient survival which are then summated. We separated the patients into 3 levels: low index (0), which corresponds to patients with no previously recorded disease categories in the Charlson co-morbidity index; medium index (patients with 1 or 2 disease categories); and high index (patients with more than 2 disease categories). Furthermore, we included some of the 19 disease groups as individual covariates.
Statistical analysis
In all studies we calculated the 10 years revision rate for the underlying cohort of primary THAs from the Danish Hip Arthroplasty Register using time to event analysis.
We used conditional logistic regression to estimate the relative risk (RR) and 95% confidence intervals for revision according to prognostic factors of interest whilst controlling for potential confounding.
Study I: In the conditional logistic regression analysis we adjusted for: age, gender, fixation technique, Charlson co-morbidity index, and diagnosis for primary THA.
Dose response analysis was calculated according to length of statin use. We included the number of redeemed statin prescriptions as a continuous variable in the multivariate logistic regression model and used the Wald test as a test for trend in the association between length of treatment and revision risk.
Study II: In the conditional logistic regression analysis we controlled for: gender, age, family type, education, gross income, county of residence, medication use, co-morbidity, Charlson co-morbidity index, year of primary THA, fixation technique, and diagnosis for primary THA surgery. Further we mutually adjusted for either thiazid or loop diuretic use.
Dose response analysis was calculated according to length of thiazid and loop diuretic use, respectively.
Study III: Covariate selection for confounder adjustment in the conditional logistic regression analyses was based on the change-in-estimate approach. Covariates were collapsed if the crude and adjusted RR for revision differed less than 5% of the adjusted RR (Mickey and Greenland, 1989). We included the following seven covariates in the further analysis: region of residence, use of statins, use of corticosteroid, diabetes I and II, year of primary THA, diagnosis for primary THA, and diagnosis for inclusion in study. Dose respond analysis was calculated according to length of bisphosphonates use in terms of Defined Daily Dosages (DDD) as defined by the World Health Organisation and we used the Wald test as a test for trend in the association between length of treatment and revision risk.
Results
Below follows a summary of the main results for the three studies.
In study I and II the 10-year THA failure rate in the underlying cohort was 8.9% (95% CI: 8.4–9.4), whereas the 10-year THA failure rate for the underlying cohort of osteoporosis patients in study III was 8.3% (95% CI: 7.3–9.3).
Study I
190 Cases (8.8% of cases) and 473 controls (20.1% of controls) redeemed at least 1 statin prescription in the postoperative period.
Statin users had a reduced adjusted RR of revision of 0.34 (95% CI: 0.28–0.41) compared with never-users. As the number of statin prescriptions increased the RR for revision decreased, except for patients redeeming more than 12 statin prescriptions ().
Table 1. Crude and adjusted relative risk for revision after primary THA according to postoperative statin use
When including the number of redeemed prescriptions as a continuous variable in the logistic regression model and calculating the Wald test we found a 5.9% (95% CI: 3.3–6.9) lower risk of revision per redeemed statin prescription, indicating a dose response relationship. However, we found no linear association between the number of statin prescriptions and the RR for revision in patients redeeming more than 12 prescriptions.
We found a significant lower risk of revision in postoperative statin users concerning the RR of revision due to deep infection, aseptic loosening, dislocation, periprosthetic fracture and other causes. In contrast statin use had no statistical significant association with risk of revision due to pain or implant failure ().
Table 2. Crude and adjusted RR for revision due to all causes and specific indications for revision in patients redeeming at least 1 statin prescription in the postoperative period
Study II
Thiazid diuretic use
1539 patients including 516 cases (20.6% of cases = 516/2491) and 1023 controls (20.7% of controls = 1023/4943) redeemed at least one thiazid prescription in the period from primary THA operation to revision or censoring.
Thiazid users had an overall adjusted RR for revision of 0.98 (95% CI: 0.85–1.12) compared with non-users. As regards revisions due to deep infection, periprosthetic fracture, aseptic loosening, dislocation of THA and periprosthetic fracture, we found no association with the risk of revision in patients redeeming at least one thiazid prescription in the postoperative period. In contrast, thiazid use was associated with an increased adjusted RR of revision of 1.79 (95% CI: 1.00–3.17) due to miscellaneous causes ().
Table 3. Adjusted RR for specific indications for revision in patients redeeming at least one diuretic prescription in the period postoperative period divided into thiazid and loop diuretics
We found no association between duration of thiazid use and the risk of revision due to all causes that could indicate a dose response relationship.
Loop diuretic use
1214 patients, including 439 cases (17.6% of cases = 439/2491) and 775 controls (15.7% of controls = 775/4943) redeemed at least one loop diuretic prescription in the postoperative period.
Loop diuretic users had an overall adjusted RR for revision of 1.14 (95% CI: 0.98–1.32) compared with non-users.
We found an increased risk of revision due to periprosthetic fracture and deep infection in patients redeeming at least one loop diuretic prescription in the postoperative period. The adjusted RRs of revision due to periprosthetic fracture and deep infection were 6.39 (95% CI: 1.84–22.60) and 1.71 (95% CI: 1.15–2.55), respectively. In contrast, loop diuretic use was not associated with risk of revision due to aseptic loosening, dislocation and miscellaneous causes ().
The adjusted RR of revision due to any cause in patients redeeming one to four loop diuretic prescriptions (three months to one year of treatment) and more than four loop diuretic prescriptions (more than one year of treatment) was 1.30 (95% CI: 1.09–1.54) and 0.93 (95% CI: 0.76–1.15), respectively.
Study III
201 patients including 72 cases (11.4% of cases) and 129 controls (10.2% of controls) redeemed at least one prescription of bisphosphonates in the period from primary THA operation to revision or censoring. Alendronate accounted for 50% and etidronate accounted for 47% of the prescriptions.
Postoperative users of bisphosphonates had an overall adjusted RR for revision of 1.34 (95% CI: 0.93–1.93) compared with non-users. As regards revisions due to aseptic loosening and dislocation of THA, we found no association with the risk of revision in patients using bisphosphonates in the postoperative period. In contrast, use of bisphosphonates in the postoperative period was associated with an increased adjusted RR of revision due to deep infection of 2.59 (95% CI: 1.30–6.53) (). Dividing postoperative use into nitrogen and non-nitrogen containing bisphosphonates revealed comparable risk estimates of revision.
Table 4. Adjusted Relative Risk (RR) following primary THA for specific indications for revision in patients redeeming at least one prescription of bisphosphonates in the postoperative period
As the number of redeemed DDDs of bisphosphonates increased in the postoperative period the RR of revision due to all causes decreased. The adjusted RR of revision due to all causes in patients redeeming 14–120 DDDs, 120–240 DDDs, and more than 240 DDDs of bisphosphonates was 2.77 (95% CI: 1.65–4.64), 1.33 (95% CI: 0.63–2.72), and 0.58 (95% CI: 0.32–1.05), respectively. However, when calculating the Wald test we found no significant association that could indicate a dose response relationship (p = 0.25)
Methodological strengths and limitations
In the assessing of the validity of the findings from studies, three alternative explanations for the findings have to be examined: bias (selection and information), confounding and random error.
Selection bias
Selection bias occurs when the association between exposure and outcome differs for those who participate and those who do not participate in the study (Rothman, Citation2002). We used nationwide population-based databases with data of high validity limiting the possibility of selection bias (Pedersen et al. Citation2004). However, not all revisions may have been captured in the Danish Hip Arthroplasty Register, although the completeness of the registration of revisions in the Danish Hip Arthroplasty Register is high (i.e., 91.1%) (Pedersen et al. Citation2004). Indeed, extensive efforts are made in order to ensure the completeness and validity of the Danish Hip Arthroplasty Register. Accordance between registered procedures in the National Registry of Patients and the Danish Hip Arthroplasty Register is routinely verified. Departments are contacted every third month in order to ensure that procedures missing in the Danish Hip Arthroplasty Register but registered in the National Registry of Patients are reported to the Danish Hip Arthroplasty Register. Further, evident registration errors such as reporting two primary operations on the same side are corrected continuously.
The revision rates among users of the drugs of investigation would have been underestimated if the majority of patients with unregistered revisions were users of the relevant drug. However, we have no reason to believe that any misclassification of revision should be differential, i.e. dependent on the use of the relevant drug.
In all studies the outcome was implant revision. However, implant revision is not a completely clear-cut end-point as it does not necessarily strictly reflect a mechanical need or biological process. Revision is an endpoint which can be affected by the willingness of the surgeon or patient to perform the revision surgery and thereby produce confounding by indication. Selection bias can occur if there is association between drug use and the cut-off point for revision, for example, if surgeons are less likely to refer to and perform revision on users of the relevant drug than on non-users. Patients with severe disease may not overcome a revision procedure and is therefore not offered a required revision. If these patients are more likely to receive the drug at study it would underestimate the association.
Information bias
Information bias in case control studies may occur if information on exposure is subject to misclassification, i.e. systematic error. Misclassification can be either differential (the exposure category is misclassified differential according to outcome status, or vice versa) or non-differential (the exposure category is misclassified independently of outcome status, or vice versa). In general, if the misclassification is differential it will lead to an over or underestimation of the true association, whereas non–differential misclassification in most situations will produce bias towards the null (Rothman, Citation2002).
In our studies information on drug exposure and revision was prospectively collected from two different registries. Information on drug exposure is therefore collected independent of the outcome and any misclassification will therefore most likely be non-differential.
For all studies we used redeeming a prescription of the relevant drug as a proxy for the patients' actual drug use. Danish statin users have been reported to have a high compliance in terms of persistence and continuity (Larsen et al. Citation2002). In contrast there are no data on the adherence to thiazid diuretics, loop diuretics or bisphosphonates. However, patients paid for a part of the cost of the drug which increases the likelihood of compliance. Furthermore, the beneficial clinical effects of diuretics on cardiovascular disease would be expected to increase adherence. Most patients in our studies redeemed and payed for several prescriptions of the relevant drug and are therefore most likely adherent to treatment. Nevertheless, any non-adherence of the drugs of interest would be independent of latter revision status, and thereby biased our findings towards the null.
Information bias can also occur if the confounding variables are misclassified. Non differential misclassification of confounding will impede our ability to control for confounding and thereby under- or overestimate the association, depending on the direction of the confounding.
Confounding
For a variable to be a confounder, it must be associated with both the drug exposure and the outcome of interest without being in the causal pathway between the drug exposure and the outcome, and its presence must be imbalanced between groups (Collet and Boivin, Citation2000). In other words it must be an independent risk factor.
There are several techniques to account for confounding in observational studies of which we in the three sub-studies have used restriction, matching and multivariate regression analysis (McMahon, Citation2003).
In all studies we used multivariate regression analysis in order to account for confounding variables.
In study I, we also used propensity score matching to minimize any possible “healthy user” effect. We were concerned that statin users may differ from non-users with regard to different lifestyle factors e.g. health, education, and socioeconomic status which may also influence the risk of revision (Glynn et al. Citation2006). Adherence bias is a related phenomenon that may be a problem in any observational study showing beneficial effects of drug given to prevention of disease i.e. adherence to statin is associated with a better prognosis (Dormuth et al. Citation2009). However, if the confounding due to adherence bias was an important issue in our studies, we would have expected that long-term use of all types of drugs prescribed for prevention of disease was associated with decreased risk of revision. However, both loop and thiazid diuretic use was not associated with a decreased risk of revision and therefore confounding due to adherence bias most likely only play a minor role in our studies.
In study II and III we matched cases and controls on age, gender, and year of primary THA, and further used multivariate regression model.
In study III, we also restricted the source population to patients with osteoporosis (defined as either a hospital discharge diagnosis of osteoporosis or a diagnosis of osteoporotic fracture). Our definition of the source population does not necessarily indicate that all patients have osteoporosis but by using restriction we obtain a more homogenous study population with some degree of frail bones. Further, it is reasonable to use vertebral, proximal humeral, forearm or hip fractures in patients older than 50 years as a proxy of osteoporosis in the absence of densitometry as most of these fractures are attributable to osteoporosis (Phillips et al. Citation1988, Ray et al. Citation1997).
These procedures have most likely accounted for a major part of the possible confounding in our studies. However, as in all observational studies, we cannot entirely exclude the possibility of residual and unaccounted confounding (e.g. health awareness, smoking, physical activity level, and body weight). Data on the latter variables were unfortunately not available in our study.
However, in study I and II, we studied the association between two classes of drugs used for cardiovascular prevention and the risk of revision. Diuretic users and statin users are likely to be comparable in terms of sedentary life, limited activity and other aspects of life style. Although the study populations were the same for both studies we found no association between thiazid diuretic use and the risk of revision, whereas statin use considerably reduced the risk of revision. This difference indicates that the possible extent of unaccounted confounding in these studies are most likely minor.
Random error
Random error is the error that remains after systematic error is eliminated and presents the variability of data that one cannot readily explain. The concept of random error is thus closely related to precision. Large studies are comparatively more precise and there would be little random error in the estimation. In this thesis, study I and II were large compared to study III, the risk estimates relatively precise as indicated by the very reasonable size of most of the estimated confidence intervals and the role of random error consequently only minor. In contrast was the study population in study III much smaller (only approximately 25% of the size of study I and II) since the study population was restricted to patients with osteoporosis. The precision in study III was therefore lower than in the two other studies and more caution is therefore needed when interpreting the study findings, in particular the analyses on revision due to specific causes and a possible dose response association. Although the precision in study III is a concern, this study also reflects the advantage of large nationwide register-based studies of rare exposures and outcomes which would be impractical or impossible to examine in RCTs.
Overall discussion and clinical implications
The following section will discuss the findings in our studies in this thesis in relation to the existing literature and the clinical implications of our findings.
To our knowledge, these studies are the first to examine the association between postoperative use of statins, diuretics and bisphosphonates and the risk of THA revision.
Study I (statin study)
The mechanism underlying the association between post-operative statin use and reduced revision risk is unclear. However, based on results from experimental studies, it has been suggested that simvastatin may improve the osseosintegration in titanium implants (Ayukawa et al. Citation2004). Whether this is the case for other implant materials and in primary THA is yet unclear. Moreover, statins have been found to have osteoanabolic and osteo-anticatabolic effects in experimental studies (Mundy et al. Citation1999, Oxlund et al. Citation2001, Skoglund et al. Citation2002, Maeda et al. Citation2001). These effects on the bone remodelling cycle may improve the fixation of the THA both in the short and long term. Further, based on results from an experimental model mimicking the course of aseptic loosening due to polyethylene particle induced osteolysis, it has been suggested that statins may prevent aseptic loosening after primary THA (Laing et al. Citation2008). This may be responsible for parts of the decreased risk of revision due to aseptic loosening in our study. Although experimental studies cannot directly be transcribed to clinical practice, many of these experimental studies imply that statins may have beneficial effects on bone health and this may partly explain our results.
Previous observational studies in patients have found statin use to be associated with decreased fracture risk with the greatest risk reduction observed for hip fracture. This association was however, not apparent in RCTs (Toh and Hernandez-Diaz, Citation2007). Further, previous observational studies have found statins to be associated with increased bone mineral density, improved prognosis after infections (Mortensen et al. Citation2005, Mortensen et al. Citation2008, Thomsen et al. Citation2008) and anti-inflammatory effects (Almog, Citation2003).
Most interestingly these reports support our results of a decreased risk of revision due to deep infections, aseptic loosening, and periprosthetic fractures after primary THA. The lack of any associations with risk of revision due to pain and implant failure also lends support to the hypothesis of a possible causal association between statin use and overall revision risk as there, to our knowledge, are no studies or biological rationale supporting an association with these revision causes. In contrast, we cannot find any support to the finding that statin users had a decreased risk of revision due to dislocation or other causes.
Clinical implications
Today statin use is widespread due to the beneficial effects on cardiovascular disease. The indications for treatment with statins have been extended considerably in recent years and many patients undergoing primary THA in the future will therefore be on statin therapy. For these patients it is important to know that statins does not impair, but may rather improve the prognosis after primary THA.
An interesting question is whether statins should be initiated at the time of primary THA surgery and whether this treatment should be continued postoperatively in healthy patients that are not previously treated with statins. This question is however not answered in our study and therefore statins should not be prescribed to THA patients in order to improve the longevity of the implants before further research have clarified this question. However, in the settlement of a general recommendation of statin therapy in THA patients several aspects should be considered including 1) the possible causality of the association between statin use and revision risk 2) the low 10 years THA revision rate, 3) the effects and the safety of statin therapy in other conditions, and 4) the price of statin therapy.
Study II (diuretic study)
Thiazid diuretic use
We expected a beneficial effect of thiazid diuretics on the risk of revision after primary THA surgery exerted by thiazid diuretics' positive effects on bone metabolism by decreasing renal calcium excretion without decreasing calcium absorption (Lemann, Jr. et al., Citation1985). Further, direct effects of thiazid diuretics on osteoblast-like cells have been described by Barry et al. (Barry et al. Citation1997). They demonstrated that thiazid diuretics altered the intracellular calcium regulation in rat osteoblast-like cells, thus providing evidence of direct effects of thiazid diuretics on bone cells. In RCTs, thiazid diuretics have been associated with a modest positive effect on bone mineral density at the hip (LaCroix et al. Citation2000, Bolland et al. Citation2007, Reid et al. Citation2000). In accordance with these studies, thiazid diuretic use has been associated with reduced hip fracture rates as reported in observational studies (Reid et al. Citation2000, Bolland et al. Citation2007, Rejnmark et al. Citation2005b, Herings et al. Citation1996, Schoofs et al. Citation2003). However, these potential positive effects of thiazid diuretics on bone health were modest and therefore a long-term treatment period may be needed to improve implant fixation and thereby reduce the risk of revision. The relatively short follow-up period in our study may explain why we did not observe any protective effect of thiazid diuretics on the risk of revision.
Loop diuretic use
The most obvious explanation for our finding of an increased risk of revision in loop diuretic users is the hypercalciuria induced by loop diuretic treatment potentially altering bone metabolism (Rose, Citation1991).
In both a RCT and an observational study loop diuretics have been associated with changes in bone mineral density and bone turnover. From these studies it was suggested that loop diuretics exerts continuous bone loss and increases bone turnover (Rejnmark et al. Citation2005a, Lim et al. Citation2008). These negative effects on bone metabolism may be responsible for an inferior implant fixation and thus for the overall increased risk of revision after primary THA in loop diuretic users as reported in our study.
In previous studies, loop diuretics have also been associated with an overall increased fracture risk which, along with a decreased BMD in loop diuretic users, may explain the increased risk of revision due to periprosthetic fracture after primary THA in our study (Rejnmark et al. Citation2006b, Heidrich et al. Citation1991, Tromp et al. Citation2000). Further, fall related mechanisms, i.e., dizziness and orthostatic hypotension may also account for part of the increased risk of revision due to periprosthetic fractures in loop diuretic users, particularly in short-term loop diuretic users. These adverse effects may be the reason of discontinuation of loop diuretic treatment and the reason why we did not find any clear dose response association.
Clinical implications
The increased relative risk of revision in loop diuretic users is relatively small in relation to the overall cumulated failure rate reported for the underlying cohort in this study. Loop diuretics are well documented, effective and cheap in the treatment of arterial hypertension and congestive heart failure (Turnbull, Citation2003, Wu et al. Citation2005, Faris et al. Citation2006). In that context we do not recommend loop diuretics to be avoided in primary THA patients, but the potentially increased risk of implant failure for diuretic users should be taken into account and discussed with THA patients.
Study III (bisphosphonate study)
The mechanism responsible for the increased risk of revision due to deep infections after primary THA in users of bisphosphonates is unclear. However, bacterial pathogens can stimulate osteoclastogenesis and potentiate bone resorption leading to bone destruction (Somayaji et al. Citation2008, Meghji et al. Citation1998). This may be an appropriate response to infection in order to clear the infection. The osteoclast inhibition by bisphosphonates may therefore be inappropriate in the response to periprosthetic infection and exacerbate the course of infection. Recently, an experimental study showed that bisphosphonates increased the bacterial growth and impaired the bacterial clearance from infected bone tissue in a murine osteomyelitis model. The authors suggested that osteoclastic bone resorption is required to remove necrotic bone that harbours the bacteria (Gromov K et al., Citation2008). This is a relatively new finding which however, supports our results of an increased risk of revision due to deep infection in bisphosphonates users.
In a previous study of canine THA, relevant wear debris was introduced around the femoral components intraoperatively. Oral alendronate treatment protected the dogs from osteoclast mediated bone loss and thus implant loosening (Shanbhag et al. Citation1997). Further experimental studies have confirmed these finding of inhibited particle induced bone resorption in bisphosphonates treated animals (Millett et al. Citation2002, von Knoch et al. Citation2005b, Wedemeyer et al. Citation2005). However, in all studies wear particles were introduced intraoperatively and treatment with bisphosphonates was initiated directly after surgery. This supports our findings of a beneficial association between use of bisphosphonates and the risk of revision in long-term users. The long-term users have probably been treated with bisphosphonates from the beginning of wear particle exposure whereas; short term users may have been exposed to wears particles without concomitant treatment with bisphosphonates. This is also in accordance with a study of the effect of alendronate in patients with demonstrated aseptic loosening who were awaiting revision surgery (21). In this cohort six months oral treatment conferred no advantage to the patients and did not alter the need for revision surgery. Similarly, an experimental canine study also suggested that short-term treatment with bisphosphonates is ineffective whenever an implant is already loose (Soballe et al. Citation2007). However, if some of the patients in our study with already aseptically loose implants were treated with bisphosphonates as an attempt to prevent revision this may explain the apparent increase in revision risk among short-term bisphosphonate users in our study.
The finding of a dose response association between bisphosphonates use and the risk of revision may also be explained by the fact that long-term treatment with bisphosphonates is essential to provide beneficial effects on bone mass (Tonino et al. Citation2000).
Clinical studies concerning bisphosphonates in orthopedic implants have been promising. Although findings are conflicting, many clinical randomized trials have reported beneficial effects of short-term treatment with bisphosphonates on periprosthetic bone mineral density and deceased stress shielding after primary THA (Yamaguchi et al. Citation2003, Yamasaki et al. Citation2007, Venesmaa et al. Citation2001, Fokter et al. Citation2005, Arabmotlagh et al. Citation2006). Improved fixation of the implants due to bisphosphonates has therefore been suggested. This potentially improved fixation of implants even after short-term treatment with bisphosphonates was however, not reflected in terms of improved implant revision rate in our study.
Recently, a RCT reported that daily administered oral clodronate six months following primary total knee arthroplasty reduced tibial component migration (Hilding et al. Citation2000, Hilding and Aspenberg, Citation2006). Postoperative migration in total joint replacements is a predictor for late revision due to loosening of implants (Karrholm et al. Citation1994, Ryd et al. Citation1995). Therefore, authors proposed that oral clodronate in the perioperative period might also decrease migration in total hip arthroplasties and thus reduce risk of revision due to loosening of implants. This is partly confirmed in our study as use of bisphosphonates for more than 240 days in the postoperative period was associated with a decreased risk of revision due to all causes. However, we do not confirm that use of bisphosphonates in the perioperative period decreases the risk of revision after primary THA surgery.
Clinical implications
This study emphasizes the importance of pharmaco-epidemiologic studies to examine potential side effects to medications. Knowing that bisphosphonates may increase the risk of revision due to deep infection enables surgeons and patients to pay attention to symptoms of infection and to initiate the relevant treatment early in the course of infection in order to prevent THA revision.
Our study showed that the association between bisphosphonate use and the risk of revision is not unequivocal. Short-term use may be harmful whereas long-term use may be beneficial to THA survival. Our results indicate that a decision on whether to start treatment with bisphosphonates in primary THA patients may not be trivial. Further studies are necessary to clarify the nature of the associations found in this study and effectiveness and safety of bisphosphonates in THA patients.
Main conclusions
Based on the results obtained and our considerations of potential bias and confounding in the three studies, we drew the following conclusions:
Study I (statin study)
We found that postoperative statin use was associated with a substantially reduced risk of revision following primary THA surgery. Although the reduced risk may partly reflect a healthy user bias, our findings do indicate that biological effects of statins may play an important role for sustainability of hip prostheses.
Study II (diuretic study)
We found that loop diuretics but not thiazid diuretics may be associated with an increased risk of revision after primary THA. Particularly, loop diuretic users had an increased risk of revision due to deep infection and periprosthetic fracture.
Study III (bisphosphonate study)
We found that postoperative use of bisphosphonates was associated with an increased risk of revision due to deep infections. Further, we found evidence of an increased risk of revision in short-term postoperative users whereas the risk of revision was decreased in long-term postoperative bisphosphonate users.
Perspectives
The studies presented in this thesis demonstrate that data linkage between the Danish Arthroplasty Register and other national registries in Denmark is a valuable tool to investigate the implications of drug use and the risk of revision after primary THA. This data linkage was an effective and appropriate method to extend the usability of the Danish Arthroplasty Register. The usability of the Danish Arthroplasty Register may prove to be even greater because of the unique possibility in Denmark for linking of data to other population based data sources. Other possibilities for record linkage could be the Cancer Registry, the Danish Transfusion Database, and a number of clinical biochemical and microbiological databases. In addition, data from the Danish Arthroplasty Register can be merged with primary data from cohort or survey studies.
Recently, the Nordic Arthroplasty Register Association (NARA) a collaboration between the Norwegian, the Swedish and the Danish hip arthroplasty registers were established (Havelin et al. Citation2009). The NARA can be considered as the start on the long way to assisting in the development of a standardized registry data, which could help in developing corporation between registries internationally in the future. In the future both the NARA and further international linkages between arthroplasty registers can be a valuable tool in the study between groups of patients that would be too small to study in individual countries, i.e. rare indications for primary THA including patients with childhood hip disorders, vascular necrosis of the femoral head or fracture sequelae, and patients with co-morbid diseases including Parkinson disease, rheumatoid arthritis, or dementia. Similarly both rare exposures and outcomes could potentially be studied with a satisfactory statistically precision. Therefore, research based on international registers may prove to widen the horizon for future research and be a valuable tool for improving the quality of THA surgery.
The presented studies have shown notable differences in the risk of revision related to use of statins, diuretics, and bisphosphonates. Other medications including corticosteroids, NSAIDs, anti-diabetics and oral anti-coagulants also merit further investigation as these drugs may also affect bone metabolism or other factors (i.e. anti-inflammatory, immune response modulation, metabolism, bleeding) that may be associated with the prognosis of primary THA.
THA surgery is already a very successful procedure. During the last decades much emphasis has been on research in implant design and surgical technique. In contrast there have not been paid much attention to patient-related prognostic factors of implant failure. In the future, linkage between the DHR and other national or international registries should also be used to investigate patient-related prognostic factors for implant survival including co-morbidities, socio-economic factors, medications, and lifestyle factors. Information on these issues is essential for further improvements in THA surgery, as it is necessary to obtain a more holistic picture of the patient in order to accommodate THA surgery to the individual while accounting for patient related prognostic factors.
In this thesis the outcomes of interest were revision and cause specific revision. From the patient's point of view these outcomes are not necessarily synonymous with a successful treatment. For further improvements of the quality of THA surgery there is therefore also a need for studying other aspects of quality including postoperative complication rates, functional status, patient reported outcome scores, and the quality of life. Implementation of these additional outcomes in the Danish Arthroplasty Register is a future challenge that however is essential in order to secure its long-term quality and research potential.
Summary
Introduction
The quality of primary total hip arthroplasty surgery in terms of implant survival has been improved during the last decades. These improvements have primarily been ascribed to technical improvements, neglecting the effect of patient-related prognostic factors on implant failure. Consequently, the information on the implications of for example drug use after primary total hip arthroplasty surgery is limited. The aims of the thesis were therefore to to examine the association between uses of 1) statins, 2) loop and thiazid diuretics, and 3) bisphosphonates and the risk of implant failure following primary THA.
Materials and methods
All studies were conducted as nested case control studies. We used data from the Danish Hip Arthroplasty Register that was linked with four national registers in Denmark including the Danish Register of Medicinal Product Statistics, the Integrated Database for Labour Market Research, the National Registry of Patients, and the Civil Registration System.
Results
Study I: Postoperative statin use was associated with an adjusted relative risk (RR) of revision of 0.34 (95% CI: 0.28–0.41) compared with never-use. In particular, statin use was associated with a reduced risk of revision due to deep infections, aseptic loosening, dislocation and periprosthetic fracture. No difference in risk of revision due to pain or implant failure was found between statin users and never-users.
Study II: Postoperative thiazid diuretic use was not associated with any risk of revision compared to non-use. Postoperative loop diuretic use was associated with an adjusted RR of revision of 1.14 (95% CI: 0.98–1.32) compared with non-use. The adjusted RR of revision due to deep infection and periprosthetic fracture in loop diuretic users was 1.71 (95% CI: 1.15–2.55) and 6.39 (95% CI: 1.84–22.21), respectively.
Study III: Use of bisphosphonates was associated with an adjusted relative risk of revision due to deep infections of 2.59 (95% CI: 1.30–6.53). Further, duration of bisphosphonates use was inversely related with the risk of revision.
Interpretation
In summary, this thesis provides evidence that use of preventive medications including statins, loop diuretics and bisphosphonates are associated with the risk of revision following primary total hip arthroplasty surgery. Information from our study could be used by clinicians to better estimate THA patient's individual risks for implant failure and improve the quality of THA surgery. However, as these studies are observational our results concerning beneficial associations between use of medications and the risk of revision should be confirmed by further studies before applied in clinical practice.
Reference list
- Almog Y. Statins, inflammation, and sepsis: hypothesis. Chest 2003; 124(2):740-743.
- Almog Y, Shefer A, Novack V, Maimon N, Barski L, Eizinger M, Friger M, Zeller L, Danon A. Prior statin therapy is associated with a decreased rate of severe sepsis. Circulation 2004; 110(7):880-885.
- Andersen TF, Madsen M, Jorgensen J, Mellemkjoer L, Olsen JH. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 1999; 46(3):263-268.
- Arabmotlagh M, Rittmeister M, Hennigs T. Alendronate prevents femoral periprosthetic bone loss following total hip arthroplasty: prospective randomized double-blind study. J Orthop Res 2006; 24(7):1336-1341.
- Aubin R, Menard P, Lajeunesse D. Selective effect of thiazides on the human osteoblast-like cell line MG-63. Kidney Int 1996; 50(5):1476-1482.
- Ayukawa Y, Okamura A, Koyano K. Simvastatin promotes osteogenesis around titanium implants. Clin Oral Implants Res 2004; 15(3):346-350.
- Barry EL, Gesek FA, Kaplan MR, Hebert SC, Friedman PA. Expression of the sodium-chloride cotransporter in osteoblast-like cells: effect of thiazide diuretics. Am J Physiol 1997; 272(1 Pt 1):C109-C116.
- Bellosta S, Ferri N, Bernini F, Paoletti R, Corsini A. Non-lipid-related effects of statins. Ann Med 2000; 32(3):164-176.
- Black N. Why we need observational studies to evaluate the effectiveness of health care. BMJ 1996; 312(7040): 1215-1218.
- Bobyn JD, Hacking SA, Krygier JJ, Harvey EJ, Little DG, Tanzer M. Zoledronic acid causes enhancement of bone growth into porous implants. J Bone Joint Surg Br 2005; 87(3):416-420.
- Bolland MJ, Ames RW, Horne AM, Orr-Walker BJ, Gamble GD, Reid IR. The effect of treatment with a thiazide diuretic for 4 years on bone density in normal postmenopausal women. Osteoporos Int 2007; 18(4):479-486.
- Carbone LD, Johnson KC, Bush AJ, Robbins J, Larson JC, Thomas A, LaCroix AZ. Loop diuretic use and fracture in postmenopausal women: findings from the Women's Health Initiative. Arch Intern Med 2009; 169(2):132-140.
- Chan KA, Andrade SE, Boles M, Buist DS, Chase GA, Donahue JG, Goodman MJ, Gurwitz JH, LaCroix AZ, Platt R. Inhibitors of hydroxymethylglutaryl-coenzyme A reductase and risk of fracture among older women. Lancet 2000; 355(9222):2185-2188.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40(5):373-383.
- Charnley J. Arthroplasty of the hip. A new operation. Lancet 1961; 1(7187):1129-1132.
- Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br 1972; 54(1):61-76.
- Charnley J, Cupic Z. The nine and ten year results of the low-friction arthroplasty of the hip. Clin Orthop Relat Res 1973;(95): 9-25.
- Collet JP, Boivin JF. Pharmacoepidemiology. John Wiley & sons, Ltd., 2000.
- Dormuth CR, Patrick AR, Shrank WH, Wright JM, Glynn RJ, Sutherland J, Brookhart MA. Statin adherence and risk of accidents: a cautionary tale. Circulation 2009; 119(15):2051-2057.
- Drake MT, Clarke BL, Khosla S. Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clin Proc 2008; 83(9):1032-1045.
- Eberhardt C, Stumpf U, Brankamp J, Schwarz M, Kurth AH. Osseointegration of cementless implants with different bisphosphonate regimens. Clin Orthop Relat Res 2006; 447:195-200.
- Espehaug B, Havelin LI, Engesaeter LB, Langeland N, Vollset SE. Patient-related risk factors for early revision of total hip replacements. A population register-based case-control study of 674 revised hips. Acta Orthop Scand 1997; 68(3):207-215.
- Faris R, Flather MD, Purcell H, Poole-Wilson PA, Coats AJ. Diuretics for heart failure. Cochrane Database Syst Rev 2006;(1): CD003838.
- Felson DT, Sloutskis D, Anderson JJ, Anthony JM, Kiel DP. Thiazide diuretics and the risk of hip fracture. Results from the Framingham Study. JAMA 1991; 265(3):370-373.
- Fletcher RW, Fletcher SW. Clinical epidemiology: The essentials. Lippincott Williams and Wilkins, Baltimore, 2005.
- Flugsrud GB, Nordsletten L, Espehaug B, Havelin LI, Meyer HE. Risk factors for total hip replacement due to primary osteoarthritis: a cohort study in 50,034 persons. Arthritis Rheum 2002; 46(3):675-682.
- Fokter SK, Komadina R, Repse-Fokter A, Yerby SA, Kocijancic A, Marc J. Etidronate does not suppress periprosthetic bone loss following cemented hip arthroplasty. Int Orthop 2005; 29(6):362-367.
- Frank L. Epidemiology. When an entire country is a cohort. Science 2000; 287(5462):2398-2399.
- Furnes O, Lie SA, Espehaug B, Vollset SE, Engesaeter LB, Havelin LI. Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987-99. J Bone Joint Surg Br 2001; 83(4):579-586.
- Garellick G, Malchau H, Herberts P, Hansson E, Axelsson H, Hansson T. Life expectancy and cost utility after total hip replacement. Clin Orthop Relat Res 1998;(346): 141-151.
- Garrett IR, Gutierrez GE, Rossini G, Nyman J, McCluskey B, Flores A, Mundy GR. Locally delivered lovastatin nanoparticles enhance fracture healing in rats. J Orthop Res 2007; 25(10):1351-1357.
- Glynn RJ, Schneeweiss S, Wang PS, Levin R, Avorn J. Selective prescribing led to overestimation of the benefits of lipid-lowering drugs. J Clin Epidemiol 2006; 59(8):819-828.
- Gromov K, Huang W, Li D, Ulrich-Vinter M, Lu A, Søballe K, O'Keefe RJ, Schwartz E. Osteoclastic bone resorption in chronic osteomyelitis. The Danish Orthopaedic Society's Annual Meeting 2008. 2008.
- Ref Type: Personal Communication.
- Gutierrez GE, Lalka D, Garrett IR, Rossini G, Mundy GR. Transdermal application of lovastatin to rats causes profound increases in bone formation and plasma concentrations. Osteoporos Int 2006.
- Hall TJ, Schaueblin M. Hydrochlorothiazide inhibits osteoclastic bone resorption in vitro. Calcif Tissue Int 1994; 55(4):266-268.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969; 51(4):737-755.
- Havelin LI, Fenstad AM, Salomonsson R, Mehnert F, Furnes O, Overgaard S, Pedersen AB, Herberts P, Karrholm J, Garellick G. The Nordic Arthroplasty Register Association. Acta Orthop 2009; 1-9.
- Heidrich FE, Stergachis A, Gross KM. Diuretic drug use and the risk for hip fracture. Ann Intern Med 1991; 115(1):1-6.
- Herberts P, Malchau H. How outcome studies have changed total hip arthroplasty practices in Sweden. Clin Orthop Relat Res 1997;(344): 44-60.
- Herberts P, Malchau H. Long-term registration has improved the quality of hip replacement: a review of the Swedish THR Register comparing 160,000 cases. Acta Orthop Scand 2000; 71(2):111-121.
- Herings RM, Stricker BH, de BA, Bakker A, Sturmans F, Stergachis A. Current use of thiazide diuretics and prevention of femur fractures. J Clin Epidemiol 1996; 49(1):115-119.
- Hilding M, Aspenberg P. Postoperative clodronate decreases prosthetic migration: 4-year follow-up of a randomized radiostereometric study of 50 total knee patients. Acta Orthop 2006; 77(6):912-916.
- Hilding M, Aspenberg P. Local peroperative treatment with a bisphosphonate improves the fixation of total knee prostheses: a randomized, double-blind radiostereometric study of 50 patients. Acta Orthop 2007; 78(6):795-799.
- Hilding M, Ryd L, Toksvig-Larsen S, Aspenberg P. Clodronate prevents prosthetic migration: a randomized radiostereometric study of 50 total knee patients. Acta Orthop Scand 2000; 71(6):553-557.
- Johnsen SP, Sorensen HT, Lucht U, Soballe K, Overgaard S, Pedersen AB. Patient-related predictors of implant failure after primary total hip replacement in the initial, short- and long-terms: A nationwide follow-up study including 36,984 patients. J Bone Joint Surg Br 2006; 88(10):1303-1308.
- Jones G, Nguyen T, Sambrook PN, Eisman JA. Thiazide diuretics and fractures: can meta-analysis help? J Bone Miner Res 1995; 10(1):106-111.
- Karrholm J, Borssen B, Lowenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg Br 1994; 76(6):912-917.
- LaCroix AZ, Ott SM, Ichikawa L, Scholes D, Barlow WE. Low-dose hydrochlorothiazide and preservation of bone mineral density in older adults. A randomized, double-blind, placebo-controlled trial. Ann Intern Med 2000; 133(7):516-526.
- Laing AJ, Dillon JP, Mulhall KJ, Wang JH, McGuinness AJ, Redmond PH. Statins attenuate polymethylmethacrylate-mediated monocyte activation. Acta Orthop 2008; 79(1):134-140.
- LaRosa JC, He J, Vupputuri S. Effect of statins on risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA 1999; 282(24):2340-2346.
- Larsen J, Andersen M, Kragstrup J, Gram LF. High persistence of statin use in a Danish population: compliance study 1993-1998. Br J Clin Pharmacol 2002; 53(4):375-378.
- Lemann J, Jr., Gray RW, Maierhofer WJ, Cheung HS. Hydrochlorothiazide inhibits bone resorption in men despite experimentally elevated serum 1,25-dihydroxyvitamin D concentrations. Kidney Int 1985; 28(6):951-958.
- Liberman UA, Weiss SR, Broll J, Minne HW, Quan H, Bell NH, Rodriguez-Portales J, Downs RW, Jr., Dequeker J, Favus M. Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study Group. N Engl J Med 1995; 333(22):1437-1443.
- Lim LS, Fink HA, Kuskowski MA, Taylor BC, Schousboe JT, Ensrud KE. Loop Diuretic Use and Increased Rates of Hip Bone Loss in Older Men: The Osteoporotic Fractures in Men Study. Arch Intern Med 2008; 168(7):735-740.
- Lucht U. The Danish Hip Arthroplasty Register. Acta Orthop Scand 2000; 71(5):433-439.
- Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C, Zhang J, Mesenbrink P, Hodgson PK, Abrams K, Orloff JJ, Horowitz Z, Eriksen EF, Boonen S. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 2007; 357(18):1799-1809.
- Lyons AR, Owen JE, Freeholm DA, Effect of alendronate on periprosthetic bone mass. Transactions of the 10th Combined Meeting of the Orthopaedic Association of the English Speeking World, Auckland, New Zealand, February 1-6, 1998, p 209. 2009.
- Maeda T, Matsunuma A, Kawane T, Horiuchi N. Simvastatin promotes osteoblast differentiation and mineralization in MC3T3-E1 cells. Biochem Biophys Res Commun 2001; 280(3):874-877.
- Malchau H, Herberts P, Ahnfelt L. Prognosis of total hip replacement in Sweden. Follow-up of 92,675 operations performed 1978-1990. Acta Orthop Scand 1993; 64(5):497-506.
- Malchau H, Herberts P, Eisler T, Garellick G, Soderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am 2002; 84-A Suppl 2: 2-20.
- Maloney WJ. National Joint Replacement Registries: has the time come? J Bone Joint Surg Am 2001; 83-A(10):1582-1585.
- Marcelo Coca-Perraillon. SAS Global Forum 185-2007, Harvard Medical School, Boston. 2007.
- Maritz FJ, Conradie MM, Hulley PA, Gopal R, Hough S. Effect of statins on bone mineral density and bone histomorphometry in rodents. Arterioscler Thromb Vasc Biol 2001; 21(10):1636-1641.
- McMahon AD. Approaches to combat with confounding by indication in observational studies of intended drug effects. Pharmacoepidemiol Drug Saf 2003; 12(7):551-558.
- Meghji S, Crean SJ, Hill PA, Sheikh M, Nair SP, Heron K, Henderson B, Mawer EB, Harris M. Surface-associated protein from Staphylococcus aureus stimulates osteoclastogenesis: possible role in S. aureus-induced bone pathology. Br J Rheumatol 1998; 37(10):1095-1101.
- Merx H, Dreinhofer K, Schrader P, Sturmer T, Puhl W, Gunther KP, Brenner H. International variation in hip replacement rates. Ann Rheum Dis 2003; 62(3):222-226.
- Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol 1989; 129(1):125-137.
- Millett PJ, Allen MJ, Bostrom MP. Effects of alendronate on particle-induced osteolysis in a rat model. J Bone Joint Surg Am 2002; 84-A(2):236-249.
- Moriyama Y, Ayukawa Y, Ogino Y, Atsuta I, Koyano K. Topical application of statin affects bone healing around implants. Clin Oral Implants Res 2008; 19(6):600-605.
- Morris RW. A statistical study of papers in the Journal of Bone and Joint Surgery [BR] 1984. J Bone Joint Surg Br 1988; 70(2):242-246.
- Mortensen EM, Pugh MJ, Copeland LA, Restrepo MI, Cornell JE, Anzueto A, Pugh JA. Impact of statins and angiotensin-converting enzyme inhibitors on mortality of subjects hospitalised with pneumonia. Eur Respir J 2008; 31(3):611-617.
- Mortensen EM, Restrepo MI, Anzueto A, Pugh J. The effect of prior statin use on 30-day mortality for patients hospitalized with community-acquired pneumonia. Respir Res 2005; 6:82.
- Mundy G, Garrett R, Harris S, Chan J, Chen D, Rossini G, Boyce B, Zhao M, Gutierrez G. Stimulation of bone formation in vitro and in rodents by statins. Science 1999; 286(5446):1946-1949.
- Murray DW, Carr AJ, Bulstrode CJ. Which primary total hip replacement? J Bone Joint Surg Br 1995; 77(4):520-527.
- Nercessian OA, Joshi RP, Martin G, Su BW, Eftekhar NS. Influence of demographic and technical variables on the incidence of osteolysis in Charnley primary low-friction hip arthroplasty. J Arthroplasty 2003; 18(5):631-637.
- Older J. Charnley low-friction arthroplasty: a worldwide retrospective review at 15 to 20 years. J Arthroplasty 2002; 17(6):675-680.
- Ooms ME, Lips P, Van LA, Valkenburg HA. Determinants of bone mineral density and risk factors for osteoporosis in healthy elderly women. J Bone Miner Res 1993; 8(6):669-675.
- Oxlund H, Dalstra M, Andreassen TT. Statin given perorally to adult rats increases cancellous bone mass and compressive strength. Calcif Tissue Int 2001; 69(5):299-304.
- Partanen J, Heikkinen J, Jamsa T, Jalovaara P. Characteristics of lifetime factors, bone metabolism, and bone mineral density in patients with hip fracture. J Bone Miner Metab 2002; 20(6):367-375.
- Pedersen A, Johnsen S, Overgaard S, Soballe K, Sorensen HT, Lucht U. Registration in the danish hip arthroplasty registry: completeness of total hip arthroplasties and positive predictive value of registered diagnosis and postoperative complications. Acta Orthop Scand 2004; 75(4):434-441.
- Pedersen AB, Johnsen SP, Overgaard S, Soballe K, Sorensen HT, Lucht U. Total hip arthroplasty in Denmark: incidence of primary operations and revisions during 1996-2002 and estimated future demands. Acta Orthop 2005; 76(2):182-189.
- Peter B, Pioletti DP, Laib S, Bujoli B, Pilet P, Janvier P, Guicheux J, Zambelli PY, Bouler JM, Gauthier O. Calcium phosphate drug delivery system: influence of local zoledronate release on bone implant osteointegration. Bone 2005; 36(1):52-60.
- Phillips S, Fox N, Jacobs J, Wright WE. The direct medical costs of osteoporosis for American women aged 45 and older, 1986. Bone 1988; 9(5):271-279.
- Ray NF, Chan JK, Thamer M, Melton LJ, III. Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone Miner Res 1997; 12(1):24-35.
- Ray WA, Daugherty JR, Griffin MR. Lipid-lowering agents and the risk of hip fracture in a Medicaid population. Inj Prev 2002; 8(4):276-279.
- Reid IR, Ames RW, Orr-Walker BJ, Clearwater JM, Horne AM, Evans MC, Murray MA, McNeil AR, Gamble GD. Hydrochlorothiazide reduces loss of cortical bone in normal postmenopausal women: a randomized controlled trial. Am J Med 2000; 109(5):362-370.
- Reid IR, Hague W, Emberson J, Baker J, Tonkin A, Hunt D, MacMahon S, Sharpe N. Effect of pravastatin on frequency of fracture in the LIPID study: secondary analysis of a randomised controlled trial. Long-term Intervention with Pravastatin in Ischaemic Disease. Lancet 2001; 357(9255):509-512.
- Rejnmark L, Olsen ML, Johnsen SP, Vestergaard P, Sorensen HT, Mosekilde L. Hip fracture risk in statin users--a population-based Danish case-control study. Osteoporos Int 2004; 15(6):452-458.
- Rejnmark L, Vestergaard P, Heickendorff L, Andreasen F, Mosekilde L. Effects of long-term treatment with loop diuretics on bone mineral density, calcitropic hormones and bone turnover. J Intern Med 2005a; 257(2):176-184.
- Rejnmark L, Vestergaard P, Heickendorff L, Andreasen F, Mosekilde L. Loop diuretics increase bone turnover and decrease BMD in osteopenic postmenopausal women: results from a randomized controlled study with bumetanide. J Bone Miner Res 2006a; 21(1):163-170.
- Rejnmark L, Vestergaard P, Mosekilde L. Reduced fracture risk in users of thiazide diuretics. Calcif Tissue Int 2005b; 76(3):167-175.
- Rejnmark L, Vestergaard P, Mosekilde L. Fracture risk in patients treated with loop diuretics. J Intern Med 2006b; 259(1):117-124.
- Rejnmark L, Vestergaard P, Mosekilde L. Statin but not non-statin lipid-lowering drugs decrease fracture risk: a nation-wide case-control study. Calcif Tissue Int 2006c; 79(1):27-36.
- Rejnmark L, Vestergaard P, Pedersen AR, Heickendorff L, Andreasen F, Mosekilde L. Dose-effect relations of loop- and thiazide-diuretics on calcium homeostasis: a randomized, double-blinded Latin-square multiple cross-over study in postmenopausal osteopenic women. Eur J Clin Invest 2003; 33(1):41-50.
- Rodan GA, Fleisch HA. Bisphosphonates: mechanisms of action. J Clin Invest 1996; 97(12):2692-2696.
- Rose BD. Diuretics. Kidney Int 1991; 39(2):336-352.
- Rothman KJ. Epidemiology, an introduction. Oxford University Press, New York 2002.
- Ryd L, Albrektsson BE, Carlsson L, Dansgard F, Herberts P, Lindstrand A, Regner L, Toksvig-Larsen S. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg Br 1995; 77(3):377-383.
- Schoofs MW, Sturkenboom MC, van der KM, Hofman A, Pols HA, Stricker BH. HMG-CoA reductase inhibitors and the risk of vertebral fracture. J Bone Miner Res 2004; 19(9):1525-1530.
- Schoofs MW, van der KM, Hofman A, de Laet CE, Herings RM, Stijnen T, Pols HA, Stricker BH. Thiazide diuretics and the risk for hip fracture. Ann Intern Med 2003; 139(6):476-482.
- Shanbhag AS. Use of bisphosphonates to improve the durability of total joint replacements. J Am Acad Orthop Surg 2006; 14(4):215-225.
- Shanbhag AS, Hasselman CT, Rubash HE. The John Charnley Award. Inhibition of wear debris mediated osteolysis in a canine total hip arthroplasty model. Clin Orthop Relat Res 1997;(344): 33-43.
- Sigurdsson G, Franzson L. Increased bone mineral density in a population-based group of 70-year-old women on thiazide diuretics, independent of parathyroid hormone levels. J Intern Med 2001; 250(1):51-56.
- Skoglund B, Aspenberg P. Locally applied Simvastatin improves fracture healing in mice. BMC Musculoskelet Disord 2007; 8:98.
- Skoglund B, Forslund C, Aspenberg P. Simvastatin improves fracture healing in mice. J Bone Miner Res 2002; 17(11):2004-2008.
- Soballe K, Chen X, Jensen TB, Kidder L, Bechtold JE. Alendronate treatment in the revision setting, with and without controlled implant motion: an experimental study in dogs. Acta Orthop 2007; 78(6):800-807.
- Somayaji SN, Ritchie S, Sahraei M, Marriott I, Hudson MC. Staphylococcus aureus induces expression of receptor activator of NF-kappaB ligand and prostaglandin E2 in infected murine osteoblasts. Infect Immun 2008; 76(11):5120-5126.
- Tanzer M, Karabasz D, Krygier JJ, Cohen R, Bobyn JD. The Otto Aufranc Award: bone augmentation around and within porous implants by local bisphosphonate elution. Clin Orthop Relat Res 2005; 441:30-39.
- Thillemann TM, Pedersen AB, Johnsen SP, Soballe K. Implant survival after primary total hip arthroplasty due to childhood hip disorders: results from the Danish Hip Arthroplasty Registry. Acta Orthop 2008; 79(6):769-776.
- Thomsen RW, Riis A, Kornum JB, Christensen S, Johnsen SP, Sorensen HT. Preadmission use of statins and outcomes after hospitalization with pneumonia: population-based cohort study of 29,900 patients. Arch Intern Med 2008; 168(19):2081-2087.
- Toh S, Hernandez-Diaz S. Statins and fracture risk. A systematic review. Pharmacoepidemiol Drug Saf 2007; 16(6):627-640.
- Tonino RP, Meunier PJ, Emkey R, Rodriguez-Portales JA, Menkes CJ, Wasnich RD, Bone HG, Santora AC, Wu M, Desai R, Ross PD. Skeletal benefits of alendronate: 7-year treatment of postmenopausal osteoporotic women. Phase III Osteoporosis Treatment Study Group. J Clin Endocrinol Metab 2000; 85(9):3109-3115.
- Tromp AM, Ooms ME, Popp-Snijders C, Roos JC, Lips P. Predictors of fractures in elderly women. Osteoporos Int 2000; 11(2):134-140.
- Turnbull F. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003; 362(9395):1527-1535.
- Uzzan B, Cohen R, Nicolas P, Cucherat M, Perret GY. Effects of statins on bone mineral density: a meta-analysis of clinical studies. Bone 2007; 40(6):1581-1587.
- van Beek ER, Cohen LH, Leroy IM, Ebetino FH, Lowik CW, Papapoulos SE. Differentiating the mechanisms of antiresorptive action of nitrogen containing bisphosphonates. Bone 2003; 33(5):805-811.
- van Staa TP, Wegman S, de Vries F, Leufkens B, Cooper C. Use of statins and risk of fractures. JAMA 2001; 285(14):1850-1855.
- Venesmaa PK, Kroger HP, Miettinen HJ, Jurvelin JS, Suomalainen OT, Alhav EM. Alendronate reduces periprosthetic bone loss after uncemented primary total hip arthroplasty: a prospective randomized study. J Bone Miner Res 2001; 16(11):2126-2131.
- von Knoch F, Wedemeyer C, Heckelei A, Saxler G, Hilken G, Brankamp J, Sterner T, Landgraeber S, Henschke F, Loer F, von Knoch M. Promotion of bone formation by simvastatin in polyethylene particle-induced osteolysis. Biomaterials 2005a; 26(29):5783-5789.
- von Knoch M, Wedemeyer C, Pingsmann A, von Knoch F, Hilken G, Sprecher C, Henschke F, Barden B, Loer F. The decrease of particle-induced osteolysis after a single dose of bisphosphonate. Biomaterials 2005b; 26(14):1803-1808.
- Wacholder S, Silverman DT, McLaughlin JK, Mandel JS. Selection of controls in case-control studies. III. Design options. Am J Epidemiol 1992; 135(9):1042-1050.
- Wang JW, Xu SW, Yang DS, Lv RK. Locally applied simvastatin promotes fracture healing in ovariectomized rat. Osteoporos Int 2007; 18(12):1641-1650.
- Wedemeyer C, von Knoch F, Pingsmann A, Hilken G, Sprecher C, Saxler G, Henschke F, Loer F, von Knoch M. Stimulation of bone formation by zoledronic acid in particle-induced osteolysis. Biomaterials 2005; 26(17):3719-3725.
- Wells VM, Hearn TC, McCaul KA, Anderton SM, Wigg AE, Graves SE. Changing incidence of primary total hip arthroplasty and total knee arthroplasty for primary osteoarthritis. J Arthroplasty 2002; 17(3):267-273.
- Wu J, Kraja AT, Oberman A, Lewis CE, Ellison RC, Arnett DK, Heiss G, Lalouel JM, Turner ST, Hunt SC, Province MA, Rao DC. A summary of the effects of antihypertensive medications on measured blood pressure. Am J Hypertens 2005; 18(7):935-942.
- Yamaguchi K, Masuhara K, Yamasaki S, Nakai T, Fuji T. Cyclic therapy with etidronate has a therapeutic effect against local osteoporosis after cementless total hip arthroplasty. Bone 2003; 33(1):144-149.
- Yamasaki S, Masuhara K, Yamaguchi K, Nakai T, Fuji T, Seino Y. Risedronate reduces postoperative bone resorption after cementless total hip arthroplasty. Osteoporos Int 2007; 18(7):1009-1015.
Appendix
Theses from the Orthopaedic Research Group
PhD and Doctoral Theses from the Orthopaedic Research Group, www.orthoresearch.dk, University Hospital of Aarhus, Denmark
PhD Theses
Step-by-step development of a novel orthopaedic biomaterial: A nanotechnological approach.
Thomas H. L. Jensen, September 2009
Polyethylene Wear Analysis. Experimental and Clinical Studies in Total Hip Arthroplasty.
Maiken Stilling, June 2009
Surgical Advances in Periacetabular Osteotomy for Treatment of Hip Dysplasia in Adults
Anders Troelsen, March 2009
Acta Orthopaedica (Suppl 332) 2009; 80
The Influence of Local Bisphosphonate Treatment on Implant Fixation
Thomas Vestergaard Jakobsen, December 2008
Adjuvant therapies of bone graft around non-cemented experimental orthopaedic implants. Stereological methods and experiments in dogs
Jørgen Baas, July 2008
Acta Orthopaedica (Suppl 330) 2008; 79
CoCrMo alloy, in vitro and in vivo studies
Stig Storgaard Jakobsen, June 2008
Rehabilitation outcome after total hip replacement; prospective randomized studies evaluating two different postoperative regimes and two different types of implants
Mette Krintel Petersen, June 2008
Efficacy, effectiveness, and efficiency of accelerated perioperative care and rehabilitation intervention after hip and knee arthroplasty
Kristian Larsen, May 2008
Rehabilitation of patients aged over 65 years after total hip replacement - based on patients' health status
Britta Hørdam, February 2008
Evaluation of Bernese periacetabular osteotomy; Prospective studies examining projected load-bearing area, bone density, cartilage thickness and migration
Inger Mechlenburg, August 2007
Acta Orthopaedica (Suppl 329) 2008;79
Combination of TGF-ß1 and IGF-1 in a biodegradable coating. The effect on implant fixation and osseointegration and designing a new in vivo model for testing the osteogenic effect of micro-structures in vivo
Anders Lamberg, June 2007
On the longevity of cemented hip prosthesis and the influence on implant design
Mette ørskov Sjøland, April 2007
Reaming procedure and migration of the uncemented acetabular component in total hip replacement
Thomas Baad-Hansen, February 2007
Studies based on the Danish Hip Arthroplasty Registry
Alma B. Pedersen, 2006
DEXA-scanning in description of bone remodeling and osteolysis around cementless acetabular cups
Mogens Berg Laursen, November 2005
www.statsbiblioteket.dk
Biological response to wear debris after total hip arthroplasty using different bearing materials
Marianne Nygaard, June 2005
The influence of RGD peptide surface modification on the fixation of orthopaedic implants
Brian Elmengaard, December 2004
Stimulation and substitution of bone allograft around non-cemented implants
Thomas Bo Jensen, October 2003
Surgical technique's influence on femoral fracture risk and implant fixation. Compaction versus conventional bone removing techniques
Søren Kold, January 2003
The influence of hydroxyapatite coating on the peri-implant migration of polyethylene particles
Ole Rahbek, October 2002
Gene delivery to articular cartilage
Michael Ulrich-Vinther, September 2002
In vivo and vitro stimulation of bone formation with local growth factors
Martin Lind, January 1996
Doctoral Theses
Gene therapy methods in bone and joint disorders. Evaluation of the adeno-associated virus vector in experimental models of articular cartilage disorders, periprosthetic osteolysis and bone healing
Michael Ulrich-Vinther, March 2007
Acta Orthopaedica (Suppl 325) 2007;78
Adult hip dysplasia and osteoarthritis. Studies in radiology and clinical epidemiology
Steffen Jacobsen, December 2006
Acta Orthopaedica (Suppl 324) 2006; 77
Calcium phosphate coatings for fixation of bone implants. Evaluated mechanically and histologically by stereological methods
Søren Overgaard, 2000
Acta Orthop Scand (Suppl 297) 2000; 71
Growth factor stimulation of bone healing. Effects on osteoblasts, osteomies, and implants fixation
Martin Lind, October 1998
Acta Orthop Scand (Suppl 283) 1998; 69
Hydroxyapatite ceramic coating for bone implant fixation. Mechanical and histological studies in dogs
Kjeld Søballe, 1993
Acta Orthop Scand (Suppl 255) 1993;54
Theses from the Department of Clinical Epidemiology
PhD and Doctoral Theses from the department of Clinical Epidemiology, www.clin-epi.dk, University Hospital of Aarhus, Denmark
Ane Marie Thulstrup: Mortality, infections and operative risk in patients with liver cirrhosis in Denmark. Clinical epidemiological studies. 2000.
Nana Thrane: Prescription of systemic antibiotics for Danish children. 2000.
Charlotte Søndergaard. Follow-up studies of prenatal, perinatal and postnatal risk factors in infantile colic. 2001.
Charlotte Olesen: Use of the North Jutland Prescription Database in epidemiological studies of drug use and drug safety during pregnancy. 2001.
Yuan Wei: The impact of fetal growth on the subsequent risk of infectious disease and asthma in childhood. 2001.
Gitte Pedersen. Bacteremia: treatment and prognosis. 2001.
Henrik Gregersen: The prognosis of Danish patients with monoclonal gammopathy of undertermined significance: register-based studies. 2002.
Bente Nørgård: Colitis ulcerosa, coeliaki og graviditet; en oversigt med speciel reference til forløb og sikkerhed af medicinsk behandling. 2002.
Søren Paaske Johnsen: Risk factors for stroke with special reference to diet, Chlamydia pneumoniae, infection, and use of non-steroidal anti-inflammatory drugs. 2002.
Elise Snitker Jensen: Seasonal variation of meningococcal disease and factors associated with its outcome. 2003.
Andrea Floyd: Drug-associated acute pancreatitis. Clinical epidemiological studies of selected drugs. 2004.
Pia Wogelius: Aspects of dental health in children with asthma. Epidemiological studies of dental anxiety and caries among children in North Jutland County, Denmark. 2004.
Kort-og langtidsoverlevelse efter indlæggelse for udvalgte kræftsygdomme i Nordjyllands, Viborg og århus amter 1985-2003. 2004.
Reimar W. Thomsen: Diabetes mellitus and community-acquired bacteremia: risk and prognosis. 2004.
Kronisk obstruktiv lungesygdom i Nordjyllands, Viborg og århus amter 1994-2004. Forekomst og prognose. Et pilotprojekt. 2005.
Lungebetændelse i Nordjyllands, Viborg og århus amter 1994-2004. Forekomst og prognose. Et pilotprojekt. 2005.
Kort- og langtidsoverlevelse efter indlæggelse for nyre, bugspytkirtel- og leverkræft i Nordjyllands, Viborg, Ringkøbing og århus amter 1985-2004. 2005.
Kort- og langtidsoverlevelse efter indlæggelse for udvalgte kræftsygdomme i Nordjyllands, Viborg, Ringkøbing og århus amter 1995-2005. 2005.
Mette Nørgaard: Haematological malignancies: Risk and prognosis. 2006.
Alma Becic Pedersen: Studies based on the Danish Hip Arthroplastry Registry. 2006. Særtryk: Klinisk Epidemiologisk Afdeling - De første 5 år. 2006.
Blindtarmsbetændelse i Vejle, Ringkjøbing, Viborg, Nordjyllands og århus Amter. 2006.
Andre sygdommes betydning for overlevelse efter indlæggelse for seks kræftsygdomme i Nordjyllands, Viborg, Ringkjøbing og århus amter 1995-2005. 2006.
Ambulante besøg og indlæggelser for udvalgte kroniske sygdomme på somatiske hospitaler i århus, Ringkjøbing, Viborg, og Nordjyllands amter. 2006.
Ellen M Mikkelsen: Impact of genetic counseling for hereditary breast and ovarian cancer disposition on psychosocial outcomes and risk perception: A population-based follow-up study. 2006.
Forbruget af lægemidler mod kroniske sygdomme i århus, Viborg og Nordjyllands amter 2004-2005. 2006.
Tilbagelægning af kolostomi og ileostomi i Vejle, Ringkjøbing, Viborg, Nordjyllands og århus Amter. 2006.
Rune Erichsen: Time trend in incidence and prognosis of primary liver cancer and liver cancer of unknown origin in a Danish region, 1985-2004. 2007.
Vivian Langagergaard: Birth outcome in Danish women with breast cancer, cutaneous malignant melanoma, and Hodgkin's disease. 2007.
Cynthia de Luise: The relationship between chronic obstructive pulmonary disease, comorbidity and mortality following hip fracture. 2007.
Kirstine Kobberøe Søgaard: Risk of venous thromboembolism in patients with liver disease: A nationwide population-based case-control study. 2007.
Kort- og langtidsoverlevelse efter indlæggelse for udvalgte kræftsygdomme i Region Midtjylland og Region Nordjylland 1995-2006. 2007.
Mette Skytte Tetsche: Prognosis for ovarian cancer in Denmark 1980-2005: Studies of use of hospital discharge data to monitor and study prognosis and impact of comorbidity and venous thromboembolism on survival. 2007.
Estrid Muff Munk: Clinical epidemiological studies in patients with unexplained chest and/or epigastric pain. 2007.
Sygehuskontakter og lægemiddelforbrug for udvalgte kroniske sygdomme i Region Nordjylland. 2007
Vera Ehrenstein: Association of Apgar score and postterm delivery with neurologic morbidity: Cohort studies using data from Danish population registries. 2007.
Annette østergaard Jensen: Chronic diseases and non-melanoma skin cancer. The impact on risk and prognosis. 2008.
Use of medical databases in clinical epidemiology. 2008.
Majken Karoline Jensen: Genetic variation related to high-density lipoprotein metabolism and risk of coronary heart disease. 2008.
Blodprop i hjertet - forekomst og prognose. En undersøgelse af førstegangsindlæggelser i Region Nordjylland og Region Midtjylland. 2008.
Asbestose og kræft i lungehinderne. Danmark 1977-2005. 2008.
Kort- og langtidsoverlevelse efter indlæggelse for udvalgte kræftsygdomme i Region Midtjylland og Region Nordjylland 1996-2007. 2008.
Akutte indlæggelsesforløb og skadestuebesøg på hospiter i Region Midtjylland og Region Nordjylland 2003-2007. Et pilotprojekt. 2009.
Peter Jepsen: Prognosis for Danish patients with liver cirrhosis. 2009.
Lars Pedersen: Use of Danish health registries to study drug-induced birth defects – A review with special reference to methodological issues and maternal use of non-steroidal anti-inflammatory drugs and Loratadine. 2009.
Steffen Christensen: Prognosis of Danish patients in intensive care. Clinical epidemiological studies on the impact of preadmission cardiovascular drug use on mortality. 2009.
Morten Schmidt: Use of selective cyclooxygenase-2 inhibitors and nonselective nonsteroidal antiinflammatory drugs and risk of cardiovascular events and death after intracoronary stenting. 2009.
Jette Bromman Kornum: Obesity, diabetes and hospitalization with pneumonia. 2009.