Abstract
Background and purpose Dual-energy X-ray absorptiometry (DXA) is a precise method to study changes in bone mineral density (BMD), including the pattern of bone remodeling around an implant. Results from implant studies are usually presented as changes in BMD as a function of time. The baseline and reference value for such calculations is the first measurement after the operation. The baseline measurement has been performed at different time points in different studies. If there is rapid bone loss immediately after an operation, this will influence the reference value and hence the results. To evaluate DXA as a method, we studied the very early changes by doing 3 DXA measurements within the first 2 weeks after surgery.
Patients and methods We included 23 hips in 23 patients who were operated with an uncemented total hip prosthesis (THP). Each Gruen region was measured with DXA at 1, 5, and 14 days, and 3 and 12 months after the operation. 16 of the patients completed all 5 follow-ups.
Results There was no detectable change in BMD in the first 14 days after the operation. In all zones, the lowest BMD was measured after 3 months.
Interpretation We conclude that DXA measurements done within 14 days after the operation can be used as reference measurements for later follow-up studies.
The bone remodeling around hip prostheses appears to vary a great deal with different fixation methods and stem designs (Kiratli et al. Citation1996, Boden et al. Citation2004, Rahmy et al. Citation2004, Grant et al. Citation2005). Even with the same implant, researchers have reported a variety of bone mineral density (BMD) changes. In implant research, BMD results are most often given in percentage change relative to the first postoperative measurement. The postoperative measurement is used as a reference to avoid measuring the changes in BMD due to the operation (Kroger et al. Citation1996). During surgery, bone is removed and compacted due to rasping and insertion of the stem. The reference measurement is of importance because it influences all later results. Aamodt (Citation2004) presented 2-year dual-energy X-ray absorptiometry (DXA) results, with 23% bone loss in Gruen zone 7 for the ABG-1 stem. Van der Wal et al. (Citation2008) reported 2 patient groups with 12% and 15% reduction in BMD in zone 7 for the same femoral stem. The only obvious difference in these 2 studies was the timing of the first measurement. Van der Wal performed the baseline measurement at 10 days postoperatively while Aamodt performed the first postoperative measurement 3–5 days after the operation. Rapid bone loss from day 3–5 to day 10 could therefore have explained the difference in bone loss at 2 years.
It is not fully known whether the bone loss starts immediately after the operation or after a few weeks. In the early postoperative period, BMD might change because of disuse atrophy (McCarthy et al. Citation1991) or because of the trauma to the bone (Karlsson et al. Citation2000). We hypothesized there is a rapid bone loss in the first days after operation, which would be an important source of bias to postoperative reference measurements.
Patients and methods
We included 23 patients (15 women) who were operated with an uncemented HA-coated Corail stem (DePuy International Ltd., Leeds, UK). The inclusion criterion was indication for THA with an uncemented stem. Exclusion criteria were infection, revision arthroplasty, marked bone loss, medication with bone-active drugs, or severe morbidity. Mean age at time of operation was 64 (34–82) years. Recruitment was through informed consent. The Norwegian Data Inspectorate and the regional ethics committee approved the study, and it was carried out according to the Helsinki declaration.
BMD was measured with DXA by experienced technicians. 2 different DXA machines were used in 2 different institutions (Prodigy; Lunar, Madison, WI and Hologic QDR; Hologic Inc., Bedford, MA). Each patient was measured on the same machine on all occasions. The patients were placed supine on the scan table with a foot support to achieve a standard rotation of the hip. Orthopaedic software (Lunar version 1.2 and Hologic QDR version 12.3) was used to analyze periprosthetic BMD in 7 regions of interest (ROIs). The ROIs were based on the Gruen zones. The patients were measured 1–2 days postoperatively, and on days 5 and 14. For follow-up, they were measured after 3 months and 1 year. 16 patients underwent all 5 measurements.
Statistics
The results were calculated as change in percent. Differences were compared by Wilcoxon signed rank test (non-parametric) using PASW statistics software version 18.0 (SPSS). To calculate precision error, all examinations were repeated on the same day with repositioning between the scans. The differences between these paired BMD measurements were used to calculate the coefficient of variation (CV) for each ROI: CV% = 100 × [(δ/√2)/μ] for each ROI, where δ represents the standard deviation of the difference between the paired BMD measurements, and μ is the overall mean of all the BMD measurements for each individual ROI.
Results
The precision (CV) of DXA measurements varied from 0.8% in Gruen zone 4 to 5.1% in zone 7. Mean CV was 1.8% ().
Table 1. The coefficient of variation (CV%) of the BMD measurements in different Gruen zones and overall
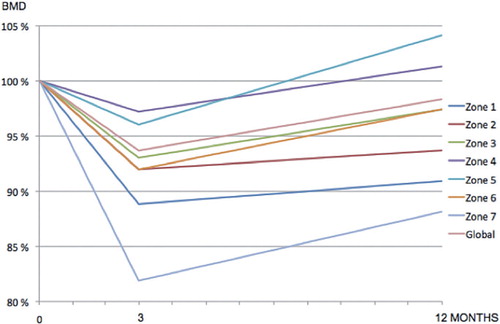
There was no change in BMD in the first 2 weeks postoperatively (). Between 14 days and 3 months, there was a mean bone loss of 8%, ranging from 18% in zone 7 to 4% in zones 4 and 5 (p < 0.05 for all zones). There was restoration of bone in all zones from the 3-month to the 12-month follow-up (). This restoration was from 2% to 8% and was statistically significant in zones 2–6 (p = 0.02, p < 0.001, p < 0.001, p = 0.001, and p = 0.05). The BMD decreased most in zone 7: by 18% after 3 months ().
Figure 1. Changes in bone mineral density (BMD) in different regions over the first 14 days after insertion of an uncemented femoral stem. Results are medians, given as percentages of the first postoperative value.
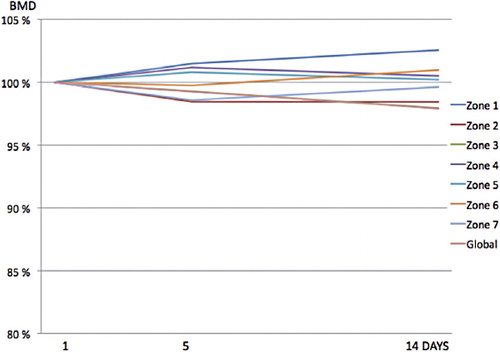
Table 2. Median bone mineral density in different regions after insertion of an uncemented femoral stem. Results are percent (range) after 5 days, 14 days, 3 months, and 12 months
Discussion
We found similar BMD values during the first 14 days after implantation of an uncemented femoral stem. Baseline measurement for bone remodeling studies with DXA can therefore be done at any time in this interval.
Bone changes around implants have been an area of continued interest. Aseptic loosening is thought to be the consequence of bone loss (often attributed to stress shielding) and an inflammatory process induced by foreign body particles (Bobyn et al. Citation1992, Van Rietbergen et al. Citation1993, Hoenders et al. Citation2008). The most informative and frequently used way to present periprosthetic bone remodeling is relative change as a function of time. Since there are different forms of bias related to use of preoperative measurements, such as disuse atrophy, sclerotic bone and peroperative bone loss, the recommended baseline is the first postoperative measurement (Venesmaa et al. Citation2001). Van der Wal et al. (Citation2008) stated that studies comparing BMD after operation with THA should be matched for preoperative BMD and sex. A correlation between preoperative BMD and postoperative bone loss indicates that the lower the BMD before operation, the higher is the bone loss after the operation (Venesmaa et al. Citation2003, Rahmy et al. Citation2004, Alm et al. Citation2009). Kiratli et al. (Citation1996) defined 4 ROIs in the proximal femur of the operated hip and did not find any correlation between preoperative BMD and the postoperative bone-remodeling pattern. Their first postoperative measurement, done less than 5 days after the operation, showed an increased BMD in all 4 ROIs. All values almost returned to baseline within 1 month.
The most marked postoperative bone loss takes place in the first months after the operation. Bone loss of up to 21% has been reported in the first 3 months in Gruen zones 1 and 7 ( Boden and Adolphson Citation2004). As in our study, Trevisan et al. (Citation1997) also found an increase in BMD in the greater trochanter early after the operation. They took the first postoperative measurements at 2 months and compared these values with preoperative values. BMD appears to stabilize after approximately 6 months (Kroger et al. Citation1997). The main reason for bone loss is thought to be partial weight bearing and stress shielding. Boden and Adolphson (Citation2004) compared BMD in 20 patients randomized to partial or full weight bearing. The group with partial weight bearing had lost more bone in Gruen zones 1, 4, and 5 after 3 months than those with full weight bearing. Differences in BMD between study groups appear to level off with time. In the material of Boden and Adolphson, the difference due to weight bearing only remained for 2 years in zone 1. Thien et al. (Citation2010) compared a polymethyl methacrylate-coated (PMMA-coated) stem, a polished stem, and a matte stem. Initially, the polished stem lost less bone and subsided more then the other two. After 5 years of follow–up, there was no difference. In our own study on Taperloc stems (Bøe et al. Citation2011), there was a significant difference in bone remodeling in the major trochanter between 2 different hydroxyapatite-coated stems during the first 2 years.
In addition to having reliable reference measurement, longitudinal studies depend on reproducibility. Rotation of the femur appears to be the most significant factor affecting reproducibility (Cohen and Rushton Citation1995). Repositioning of the patient between 2 measurements on the same day should give us reliable feedback on the precision of DXA measurements. In our study, a coefficient of variation below 5% indicated good precision, and daily scanning of a phantom allowed us to check for drift of the DXA machines.
Another factor influencing BMD around implants is operation technique. Compaction is a bone-saving technique compared to conventional bone-removing techniques by a rasp with similar shape as the stem. Using a dog model, Kold et al. (Citation2005a) showed that operation with compaction around an HA-coated implant increased the peri-implant bone density and bone implant contact. This indicates that compaction may be an advancement in human joint replacement to enhance initial fixation. Even though compaction represents autograft of non-vital bone, which is resorbed over time, the fixation does not appear to be inferior after bone resorption (Kold et al. Citation2005b). To our knowledge, the technique has not been tested in a human clinical trial. Perhaps compaction is the reason for increased BMD immediately after surgery, since most of the rasps that are used can probably both compact and remove bone. It is of some concern that the risk of femoral fractures increases with compaction (Kold et al. Citation2003).
Bone remodeling after implantation of prostheses may be compared to remodeling after partial weight bearing because of fractures. Eyres and Kanis (Citation1995) found a definite and persistent loss of BMD in the distal tibia 5–11 years after fracture. At the fracture site, there was sclerosis and a higher BMD than on the control side. In that material, there was no improvement in BMD with weight bearing. Fractures sustained in childhood did not lead to bone loss in the distal tibia. There have been several publications indicating that bone loss may be the result of a fracture, and not necessary the cause of it (Andersson and Nilsson Citation1979, Eyres and Kanis Citation1995, Karlsson et al. Citation2000). Karlsson et al. (Citation2000) published BMD results from both legs, both hips, spine, and total body in patients who were operated with tibial osteotomy for localized medial osteoarthritis. They found substantial bone loss in the whole body, the spine, and the contralateral hip after 9 and 15 months. In the leg with osteotomy, the bone loss was significant in the distal femur after 4 months (compared to baseline) and in the shaft of the tibia after 9 and 15 months. The conclusion from that work was that bone loss following an osteotomy is rapid, affects both fractured and unfractured bones, and is not completely reversible. The same mechanisms may be responsible for the bone remodeling seen after implantation of prostheses, but the exact reason for this “post-traumatic” bone loss is unknown.
BB wrote the protocol and designed the study, performed the DXA analysis, wrote the manuscript, and did the statistical evaluation. LN designed the study, included patients, and helped write the manuscript. TH included, followed, and operated on most patients.
We thank Professor Tore Kvien and Anne Katrine Kongtorp for allowing us to use the DXA densitometer and personnel at the Rheumatology Department of Diakonhjemmet Hospital. No benefits in any form have been received from a commercial party by any of the authors in connection with this article.
- Aamodt A. Migrasjon og benremodelering etter innsetting av usementerte femurstammer med ulik geometri. En prospektiv og randomisert RSA- og DXA-studie. Vitenskapelige forhandlinger (Abstract) 2004.
- Alm JJ, Makinen TJ, Lankinen P, Moritz N, Vahlberg T, Aro HT. Female patients with low systemic BMD are prone to bone loss in Gruen zone 7 after cementless total hip arthroplasty. Acta Orthop 2009; 80(5):531-7.
- Andersson SM, Nilsson BE. Post-traumatic bone mineral loss in tibial shaft fractures treated with a weight-bearing brace. Acta Orthop Scand 1979; 50(6 Pt 1):689-91.
- Bobyn JD, Mortimer ES, Glassman AH, Engh CA, Miller JE, Brooks CE. Producing and avoiding stress shielding. Laboratory and clinical observations of noncemented total hip arthroplasty. Clin Orthop 1992; (274):79-96.
- Boden H, Adolphson P. No adverse effects of early weight bearing after uncemented total hip arthroplasty: a randomized study of 20 patients. Acta Orthop Scand 2004; 75(1):21-9.
- Boden H, Adolphson P, Oberg M. Unstable versus stable uncemented femoral stems: a radiological study of periprosthetic bone changes in two types of uncemented stems with different concepts of fixation. Arch Orthop Trauma Surg 2004; 124(6):382-92.
- Bøe BG, Röhrl SM, Heier T, Snorrason F, Nordsletten L. A prospective randomized study comparing electrochemically deposited hydroxyapatite and plasma-sprayed hydroxyapatite on titanium stems. 55 hips followed for 2 years with RSA and DXA. Acta Orthop 2011; 82(1):13-9.
- Cohen B, Rushton N. Accuracy of DEXA measurement of bone mineral density after total hip arthroplasty. J Bone Joint Surg (Br) 1995; 77(3):479-83.
- Eyres KS, Kanis JA. Bone loss after tibial fracture. Evaluated by dual-energy X-ray absorptiometry. J Bone Joint Surg (Br) 1995; 77(3):473-8.
- Grant P, Aamodt A, Falch JA, Nordsletten L. Differences in stability and bone remodeling between a customized uncemented hydroxyapatite coated and a standard cemented femoral stem A randomized study with use of radiostereometry and bone densitometry. J Orthop Res 2005; 23(6):1280-5.
- Hoenders CS, Harmsen MC, van Luyn MJ. The local inflammatory environment and microorganisms in “aseptic” loosening of hip prostheses. J Biomed Mater Res B Appl Biomater 2008; 86(1):291-301.
- Karlsson MK, Josefsson PO, Nordkvist A, Akesson K, Seeman E, Obrant KJ. Bone loss following tibial osteotomy: a model for evaluating post-traumatic osteopenia. Osteoporos Int 2000; 11(3):261-4.
- Kiratli BJ, Checovich MM, McBeath AA, Wilson MA, Heiner JP. Measurement of bone mineral density by dual-energy x-ray absorptiometry in patients with the Wisconsin hip, an uncemented femoral stem. J Arthroplasty 1996; 11(2):184-93.
- Kold S, Mouzin O, Bourgeault C, Soballe K, Bechtold JE. Femoral fracture risk in hip arthroplasty: smooth versus toothed instruments. Clin Orthop 2003; (408):180-8.
- Kold S, Rahbek O, Toft M, Ding M, Overgaard S, Soballe K. Bone compaction enhances implant fixation in a canine gap model. J Orthop Res 2005a; 23(4):824-30.
- Kold S, Rahbek O, Zippor B, Soballe K. No adverse effects of bone compaction on implant fixation after resorption of compacted bone in dogs. Acta Orthop 2005b; 76(6):912-9.
- Kroger H, Miettinen H, Arnala I, Koski E, Rushton N, Suomalainen O. Evaluation of periprosthetic bone using dual-energy x-ray absorptiometry: precision of the method and effect of operation on bone mineral density. J Bone Miner Res 1996; 11(10):1526-30.
- Kroger H, Vanninen E, Overmyer M, Miettinen H, Rushton N, Suomalainen O. Periprosthetic bone loss and regional bone turnover in uncemented total hip arthroplasty: a prospective study using high resolution single photon emission tomography and dual-energy X-ray absorptiometry. J Bone Miner Res 1997; 12(3):487-92.
- McCarthy CK, Steinberg GG, Agren M, Leahey D, Wyman E, Baran DT. Quantifying bone loss from the proximal femur after total hip arthroplasty. J Bone Joint Surg (Br) 1991; 73(5):774-8.
- Rahmy AI, Gosens T, Blake GM, Tonino A, Fogelman I. Periprosthetic bone remodelling of two types of uncemented femoral implant with proximal hydroxyapatite coating: a 3-year follow-up study addressing the influence of prosthesis design and preoperative bone density on periprosthetic bone loss. Osteoporos Int 2004; 15(4):281-9.
- Thien TM, Thanner J, Karrholm J. Randomized comparison between 3 surface treatments of a single anteverted stem design: 84 hips followed for 5 years. J Arthroplasty 2010; 25(3):437-44.
- Trevisan C, Bigoni M, Randelli G, Marinoni EC, Peretti G, Ortolani S. Periprosthetic bone density around fully hydroxyapatite coated femoral stem. Clin Orthop 1997; (340):109-17.
- Van der Wal BC, Rahmy A, Grimm B, Heyligers I, Tonino A. Preoperative bone quality as a factor in dual-energy X-ray absorptiometry analysis comparing bone remodelling between two implant types. Int Orthop 2008; 32(1):39-45.
- Van Rietbergen B, Huiskes R, Weinans H, Sumner DR, Turner TM, Galante JO. ESB Research Award 1992. The mechanism of bone remodeling and resorption around press-fitted THA stems. J Biomech 1993; 26(4-5):369-82.
- Venesmaa PK, Kroger HP, Miettinen HJ, Jurvelin JS, Suomalainen OT, Alhava EM. Monitoring of periprosthetic BMD after uncemented total hip arthroplasty with dual-energy X-ray absorptiometr–a 3-year follow-up study. J Bone Miner Res 2001; 16(6):1056-61.
- Venesmaa PK, Kroger HP, Jurvelin JS, Miettinen HJ, Suomalainen OT, Alhava EM. Periprosthetic bone loss after cemented total hip arthroplasty: a prospective 5-year dual energy radiographic absorptiometry study of 15 patients. Acta Orthop Scand 2003; 74(1):31-6.