Abstract
Background and purpose In the last decade, intramedullary limb lengthening has become a viable alternative to traditional external systems. We retrospectively analyzed the use of an intramedullary motorized nail (Fitbone) in a consecutive series of 32 patients.
Patients and methods During the period September 2006 to December 2008, 32 consecutive patients with a median age of 17 (IQR: 15–19) years were treated with a fully implantable, motorized intramedullary lengthening device (Fitbone). The median leg length discrepancy was 35 (IQR: 30–44) mm at the femur (n = 21) and 28 (IQR: 25–30) mm at the tibia (n = 11).
Results Leg lengthening was successful in 30 of 32 cases, with no residual relevant discrepancy (± 5 mm). No intraoperative complications were observed. The consolidation index was significantly different (p = 0.04) between femoral lengthening (mean 35 days/cm) and tibial lengthening (mean 48 days/cm) but did not depend on age older/younger than 16 or previous operations at the affected site. 3 problems, 3 obstacles, and 4 complications (3 minor, 1 major) were encountered in 8 patients, 5 of which were implant-associated.
Interpretation This technique even allows correction in patients with multiplanar deformities. Compared to external devices, intramedullary systems provide comfort and reduce complication rates, give improved cosmetic results, and lead to fast rehabilitation since percutaneous, transmuscular fixation is prevented. This results in reasonable overall treatment costs despite the relatively high costs of implants.
Operative leg length equalization includes techniques such as contralateral epiphysiodesis during growth, or shortening and lengthening procedures. In the last decade, lower complication rates and greater patient comfort (Baumgart et al. Citation1997, Guichet Citation1999, Cole et al. Citation2001) have made intramedullary limb lengthening a valuable alternative to traditional external fixation distractor systems (Guichet et al. Citation2003, Hankemeier et al. Citation2005, Leidinger et al. Citation2006, Krieg et al. Citation2008). Two mechanical devices, namely the Albizzia nail and the ISKD (intramedullary skeletal kinetic distractor) nail, and one motorized nail (Fitbone) have been reported (Betz et al. Citation1990, Cole et al. Citation2001, Guichet et al. Citation2003).
Here we present the indications and limitations, and the results and complications of the Fitbone nail. We identified possible factors that may influence the clinical outcome. In addition, we did a comparative cost analysis of different treatment methods.
Patients and methods
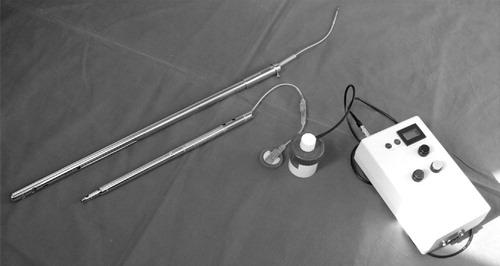
During the period September 2006 to December 2008, 32 consecutive patients with a median age of 16.9 (IQR: 15.3–19.4) years were treated with a fully implantable, motorized intramedullary lengthening device (the Fitbone Sliding Active Actuator (SAA) nail and the Telescope Active Actuator (TAA) nail; WITTENSTEIN Intens GmbH, Igersheim, Germany) (). The median leg length discrepancy was 35 (IQR: 30–44) mm at the femur and 28 (IQR: 25–30) mm at the tibia.
Figure 1. Fitbone TAA (Telescope Active Actuator) and SAA (Sliding Active Actuator) with control and transmitter unit.
The underlying pathologies and the number of operations at the affected site are listed in . None of the cases had a history of osteomyelitis within the previous 2 years, nor showed any reduced bone quality. 9 patients presented with shortening as the only deformity, 14 presented with two deformities, and 9 had three deformities.
Table 1. Patient characteristics and results
The indication for surgery was based on a minimum LLD of more than 2 cm, clinical/functional symptoms, and ability to independently handle the lengthening device. Lengthening for cosmetic reasons only was not accepted.
The SAA, which is restricted to femoral use, is mostly implanted through an antegrade approach. As the SAA features a slotted sliding hole in its middle part, this device allows lengthening as well as bone transport. TAA nails are available for both the femur and the tibia. They are implanted through a retrograde approach at the femur and an antegrade approach at the tibia. The femoral TAA is a straight nail; the tibial one is available as either a straight nail or one with a proximal Herzog angulation. In contrast to the SAA, lengthening with the TAA is accomplished by a telescoping mechanism. Various sizes, different designs, and even custom-made implants of both nail types are available.
Preoperatively, standardized anteroposterior and lateral long standing radiographs of both legs were taken and a preoperative planning was performed, based on the protocol for retrograde corrective planning described by Baumgart (Citation2009). Mechanical axis alignment, LLD and projected joint angles, such as the mechanical lateral distal femoral angle (mLDFA, physiological range 85–90°) or the medial proximal tibial angle (MPTA, physiological range 85–90°), were documented pre- and postoperatively.
Percutaneous osteotomies were performed using a 4.0-mm drill and a chisel for completion, which causes minimal thermal damage to the bone and preserves the periosteal sleeve, for optimal callus formation.
Every patient received detailed oral and written instructions on the use of the device as well as an individual schedule with timing, rate, and total amount of lengthening. We aimed at starting distraction 5 days postoperatively at a distraction rate of 1.3 mm/day in femurs and starting 7 days postoperatively at 1.0 mm/day in tibias.
All patients were counseled regularly regarding the device and were followed radiographically on a biweekly basis during and at 4-week intervals after distraction until full consolidation. The range of motion of hip, knee, and ankle joints was recorded in addition to pain (visual analog scale), wound status, and complications. All patients underwent an intensive rehabilitation program under the guidance of physiotherapists not any less frequently than twice a week, at least until consolidation.
Consolidation was defined as corticalization of at least 3 sides of the callus on the biplane radiographs, with subsequent transition to full weight bearing. Insufficient callus formation was defined as a consolidation period more than 3 times longer than the distraction period (femur) or more than 4 times longer (tibia).
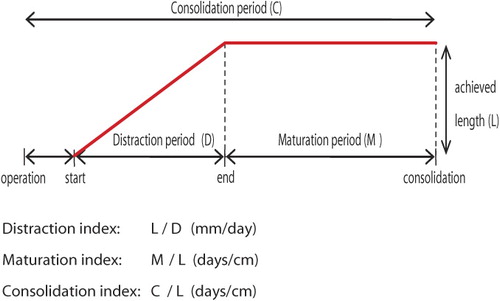
Every single lengthening period (distraction, maturation, consolidation) and the appropriate indices () were calculated and evaluated, with respect to the anatomical location, previous operations at the affected site, and age older or younger than 16.
Leg lengthening was considered successful in cases with no residual relevant discrepancy of ± 5 mm. For deformity correction in the frontal plane, the mechanical axis deviation (MAD) was evaluated preoperatively and intraoperatively with respect to the contralateral side and/or normal physiological conditions (Paley et al. Citation1994). Intraoperatively, mechanical axis alignment was determined by use of a grid plate with radio-opaque straight lines, which was placed underneath the patient on a radiolucent table. The Paley outcome score system designed for femora was used (Paley et al. Citation1997) and a modified version introduced by Krieg et al. (Krieg et al. 2008) was used for tibias.
Complications were differentiated as problems (grade 1), obstacles (grade 2), and minor or major complications (grade 3) (Paley Citation1990).
The calculation of total costs for a Fitbone treatment was based on the current local reimbursement rates for a public patient, 1 segment affected, implantation and explantation, hospital stay of 3 weeks in total (implantation and explantation), and physiotherapy twice a week for 1 year. Likewise, overall costs for leg length equalization by means of orthotic devices were calculated by a local orthopedic technician assuming a non-private patient with a leg length discrepancy of more than 2 cm requiring shoe lifts and necessary additional insoles twice a year for 60 years. In addition, implant costs for the Taylor Spatial Frame were taken from the manufacturer's price list.
The median follow-up time was 16 months (IQR: 12–22; range 12–27 months). By the end of the observation period, all but 2 nails had been explanted after a median of 14 months (IQR: 13–17; range 6.6–23 months).
Statistics
Data are given as means, medians, and interquartile range (IQR). Comparisons between patient subgroups were assessed using Fisher's exact test for binary endpoints and by the Mann-Whitney U-test for continuous endpoints. A p-value of ≤ 0.05 was taken to indicate statistical significance. Statistical analysis was performed using SPSS software version 17.0.
Results
Length gain
Leg length equalization was successful in 30 of 32 cases (± 5mm). 2 showed a remaining LLD of 7 mm and 10 mm, which was clinically irrelevant. At the femur, the target length was achieved with a standard deviation of ± 6.1%. Regarding the tibia, the equalization was accomplished with a standard deviation of ± 7.3%.
Distraction index and hospital stay
Distraction was started at an average of 6 (3–12) days postoperatively with a median distraction index of 1.0 (IQR: 0.9–1.2) mm/day and a median distraction period of 30 (IQR: 28–42) days. The median hospital stay was 12 (IQR: 10–14) days.
Maturation
There was no statistically significant difference in the maturation index in terms of the influencing variables examined.
The median maturation period was 75 (IQR: 60–106) days for femurs (n = 21) and 96 days (IQR: 66–112) for tibias (n = 11). The median maturation index was 22 days/cm (IQR: 16–30) for femurs and 36 (IQR: 22–40) days/cm for tibias.
Consolidation
The median consolidation index was 35 (IQR: 27–44) days/cm for the femur and 48 (IQR: 34–63) days/cm for the tibia. A statistically significant difference between femurs and tibias was seen, but not regarding other influencing variables.
Deformity corrections
The median preoperative mechanical axis deviation (MAD) in patients with a varus axis (n = 8) was 13 (6–50) mm medially to the center of the knee joint, whereas the median postoperative MAD was 4 mm medially (38 mm medially to 11 mm laterally). In patients with a valgus axis (n = 9), the median preoperative MAD was 13 (5–54) mm laterally as compared to a postoperative median of 0 mm (10 mm medially to 28 mm laterally).
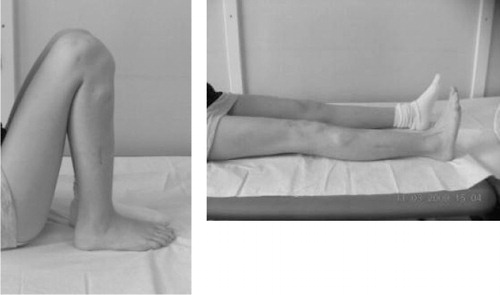
In patients with additional rotatory and/or sagittal corrective osteotomies (n = 5), a bilaterally equal range of motion of the hip and knee joint was seen immediately postoperatively ().
Joint motion
The functional outcome was excellent in 26 patients, good in 5, and fair in 1. All but one had regained or even improved upon their preoperative range of motion of the hip, knee, and ankle joint (n = 8) ().
Complications
No intraoperative complications and no postoperative bone or soft tissue infections occurred. We observed 3 problems, 3 obstacles, and 4 complications (3 minor, 1 major) in 8 patients (). Insufficient callus formation was found in 2 tibias of smokers who both refused weight bearing. One (patient 14) was treated with autologous tricortical iliac bone grafting 8 months postoperatively. The other showed slow consolidation without need of further operative intervention.
In 1 case with a history of lengthening by external fixation (patient 12), a progressive knee extension-contracture required manual mobilization under anesthesia 5 months after the end of distraction.
One motor stopped because of overstraining of the mechanical implant by full weight bearing early on the patient's own authority, during the initial distraction period and after discharge from the hospital. It had to be exchanged, but this did not affect the final result. In 3 cases we observed running back of the telescopic part of the nail during the initial consolidation phase, which was twice associated with loosening of locking bolts. Another bolt loosened without loss of length. The persisting equinus of the foot in 1 patient (patient 24) was successfully corrected by a combined calcaneus and talus osteotomy using the Taylor Spatial frame.
Costs
Total costs of approximately 100,000 euros were calculated to equalize a leg length discrepancy of more than 2 cm by means of orthotic devices. For a Fitbone treatment, total costs of approximately 38,000 euros were calculated (see Patients and methods). Pure implant costs amount to approximately 11,000 euros for the Fitbone nail, and to 7,500 euros for a standard Taylor Spatial Frame.
Discussion
The use of mechanically driven intramedullary nails for limb lengthening and deformity correction has been reported repeatedly (Baumgart et al. Citation1997, Cole et al. Citation2001, Guichet Citation1999, Hankemeier et al. Citation2005, Guichet et al. Citation2003, Leidinger et al. Citation2006, Krieg et al. 2008, Betz et al. Citation1990, Garcia-Cimbrelo et al. Citation2002, Singh et al. Citation2006, Baumgart et al. Citation2006). The ISKD and the Albizzia are mechanically driven nails and provide all the advantages of intramedullary leg lengthening (Cole et al. Citation2001). Distraction with the ISKD is achieved by physiological gait movements. Thus, the distraction rate is less predictable, which may contribute to insufficient callus formation (Leidinger et al. Citation2006). In contrast, the Albizzia sometimes causes severe pain and discomfort at the osteotomy site since lengthening is accomplished by rotational maneuvers. Some authors have even reported re-admission for distraction under anesthesia (Garcia-Cimbrelo et al. Citation2002, Guichet et al. Citation2003). The Fitbone nail is the only intramedullary motorized lengthening device. In order to avoid high complication rates, the distribution was limited to a small number of selected surgeons by the company during the thorough implant development process.
Since most peer-reviewed literature on intramedullary lengthening involves a small number of patients (), we considered that it would be useful to add this relatively large case series.
Table 2. Summary of case series in peer-reviewed literature
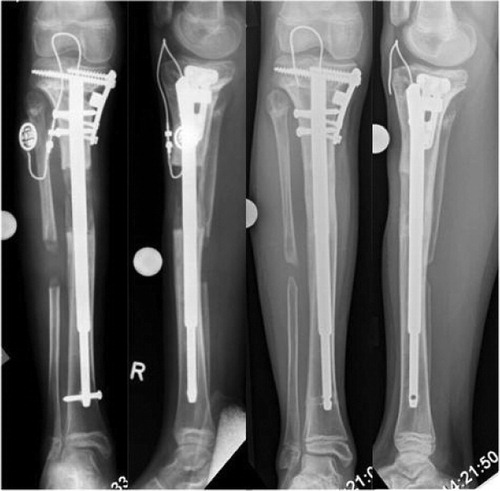
Unlike the application of external fixators, a solid intramedullary device requires defined anatomical preconditions that have to be adhered to, both during the preoperative planning and intraoperatively. However, for the accomplishment of corrections in 3 dimensions, reaming of the intramedullary cavity with straight and rigid reamers (not flexible ones) is as a prerequisite. Only the use of rigid reamers, which do not follow the line of minor resistance, allows to carry out the correlations anticipated during preoperative planning. In this context, adequate medullar dimensions respecting a minimal nail diameter of 11 mm at its shaft are one of the most important limitations of the Fitbone TAA. Further restrictions derive from its short overall length and a mandatory osteotomy level 7–11 cm from the joint line to ensure stable interlocking conditions. Marked angular deformities and a center of rotation and angulation far from the planned osteotomy are additional geometric obstacles, and may make segmental translation unavoidable (). Axis alignment or implant position cannot be changed postoperatively. Hence, intraoperative acknowledgment of the preoperative planning is important (Baumgart (Citation2009). In contrast, external fixators—and particularly the Taylor Spatial Frame (TSF)—are more forgiving by allowing postoperative and even computer-assisted adjustments (Blondel et al. Citation2009). However, even complex deformities may be overcome ().
Figure 4. Frontal plane double deformity of the tibia with LLD of 5.5 cm in a patient with a history of osteomyelitis in early childhood and of previous operations.

Figure 5. Anteroposterior and lateral radiographs 3 months (left) and 9 months (right) after surgery.
Application of solid lengthening nails in children is limited by open growth plates. However, data on children treated for tumors and also unpublished observations of experienced surgeons (regarding limb lengthening) suggest that the growth potential may remain unaffected when smooth polished implants are inserted through the central portion of a physis (Neel et al. Citation2004, Baumgart et al. Citation2006).
In keeping with the results of Fischgrund et al. (Citation1994), we found a statistically significant difference in the consolidation index of patients with femoral lengthening and of those with tibial lengthening. However, as additional consideration of the maturation index did not reveal any statistically significant disparity, this may rather be explained by an earlier distraction start and higher daily rates at the femur. It is our experience that a distraction rate of about 1.3 mm/day at the femur is well accepted and sometimes even required in children, due to the enormous regeneration potential. This might be due to the excellent soft tissue coverage and the gentle osteotomy technique, which further contribute to rapid bone formation and consolidation.
Without transfixation of skin and muscles, lengthening nails facilitate full joint motion in the first few days after surgery, whereas external fixators decrease the range of motion even before the lengthening process has started (Maffulli et al. Citation2001). Thus, re-establishment of full range of motion with external fixators mostly exceeds rehabilitation times with intramedullary devices by far, as seen in our study.
The complication rates of external fixators range from 24% to 117% (Paley Citation1990, Tjernstrom et al. Citation1994, Paley et al. Citation1997, Blondel et al. Citation2009) and from 11% to 47% (Cole et al. Citation2001, Garcia-Cimbrelo et al. Citation2002, Guichet et al. Citation2003, Leidinger et al. Citation2006) for mechanically driven intramedullary devices, depending on the distraction length and the experience of the surgeon.
A complication rate of 12.5% in our series (4 of 32 patients) is in keeping with the findings of Baumgart et al. Citation2006) who reported a 13% complication rate in a larger number of patients (n = 150) treated with Fitbone TAA and SAA nails. These low complication rates may be attributed to the electronically-actuated lengthening mechanism and its reliable controllability—with consistent distraction rates as a consequence.
Technical complications or implant breakage rarely occur with Fitbone. In the series of 150 patients, Baumgart et al. (Citation2005) reported technical difficulties in 6% of cases and implant breakage in 5%, with only a 3% rate of implant exchanges in total. Partial loss of gained length, as seen in 3 of our 32 patients, may occur due to loosened locking bolts or running back of the telescoping part. The latter will presumably be prevented now with the new generation of nails that have a running-back barrier.
The overall cost of lengthening with Fitbone was less than for conservative treatment, assuming the conditions mentioned earlier. Compared to external fixators such as the Taylor Spatial Frame, the Fitbone nail is somewhat more expensive. However, the much higher complication rate of external fixation—probably associated with additional hospital stays, medication (pain relief, antibiotics), and physiotherapy sessions—warrant differentiation between pure implant costs and costs of treatment, in addition to “soft” factors such as cosmetics, patient satisfaction, and quality of life during and after the lengthening procedure (Tjernstrom et al. Citation1994, Paley Citation1990, Song et al. Citation2005).
Paley et al. (Citation1997), who published a similar cost report, put forward mean costs of about $24,000 ($18,000 to $28,000) for unilateral femoral lengthening over an intramedullary nail compared to $19,000 ($18,000 to $29,000) for unilateral Ilizarov femoral lengthening. Likewise, they included hospital charges as well as fees for the index procedure and removal of the external fixator (factors such as duration of hospital stay were not listed in detail) but did not include the costs for rehabilitation and additional costs due to complications. Even so, these considerations should be taken into account in order to compare overall costs. Healthcare providers especially—who tend to refuse reimbursement of new and at first sight expensive innovative methods—should be made to understand that such treatment options may prove to be less expensive if the wider picture of overall cost is taken into account.
Apart from the explicit desire of the majority of our patients to have the implants removed after the lengthening procedure, we consider the removal mandatory in order to avoid difficulties in the future, such as removal of an ingrown nail or interference with arthroplastic devices later on. Furthermore, the analysis of each explanted device by the manufacturer contributes to the quality of management and promotes development and perfection of the nail.
Our study was limited by the lack of a matched control group, treated with different lengthening devices. Furthermore, long-term results on lengthening with Fitbone nails are still not available.
In summary, the outcome achieved in our patients is a respectable result, and there was a low complication rate. There was a significant difference in the consolidation index in the treatment of femurs and tibias. The high implant costs are compensated for by competitive treatment costs. Intramedullary leg lengthening is, however, a demanding procedure.
AHK and CCH planned the study and BMS analyzed the data. AHK and UL wrote the first draft of the manuscript. AHK, UL, BMS, and CCH contributed to interpretation of the results and revised the manuscript.
No external funding was received for this study from the manufacturer or other sources. There are no competing interests.
- Baumgart R. The reverse planning method for lengthening of the lower limb using a straight intramedullary nail with or without deformity correction. A new method. Oper Orthop Traumatol 2009; 21 (2): 221-33.
- Baumgart R, Betz A, Schweiberer L. A fully implantable motorized intramedullary nail for limb lengthening and bone transport. Clin Orthop 1997; (343): 135-43.
- Baumgart R, Thaller P, Hinterwimmer S. A fully implantable, programmable distraction nail (Fitbone): new perspectives for corrective and reconstructive limb surgery. Springer 2005.
- Baumgart R, Thaller P, Hinterwimmer S, Krammer M, Hierl T, Mutschler W. A fully implantable, programmable distraction nail (Fitbone) - new perspectives for corrective and reconstructive limb surgery. In: Practice of Intramedullary Locked Nails. New developments in Techniques and Applications ( eds. Leung KS, Taglang G, Schnettler R) Heidelberg, New York 2006.
- Betz A, Baumgart R, Schweiberer L. First fully implantable intramedullary system for callus distraction--intramedullary nail with programmable drive for leg lengthening and segment displacement. Principles and initial clinical results. Chirurg 1990; 61 (8): 605-9.
- Blondel B, Launay F, Glard Y, Jacopin S, Jouve JL, Bollini G. Limb lengthening and deformity correction in children using hexapodal external fixation: Preliminary results for 36 cases. Orthop Traumatol Surg Res 2009; 95 (6): 425-30.
- Cole JD, Justin D, Kasparis T, DeVlught D, Knobloch C. The intramedullary skeletal kinetic distractor (ISKD): first clinical results of a new intramedullary nail for lengthening of the femur and tibia. Injury (Suppl 4) 2001; 32: SD129-39.
- Fischgrund J, Paley D, Suter C. Variables affecting time to bone healing during limb lengthening. Clin Orthop 1994; (301): 31-7.
- Garcia-Cimbrelo E, Curto de la Mano A, Garcia-Rey E, Cordero J, Marti-Ciruelos R. The intramedullary elongation nail for femoral lengthening. J Bone Joint Surg (Br) 2002; 84 (7): 971-7.
- Guichet JM. Leg lengthening and correction of deformity using the femoral Albizzia nail. Orthopade 1999; 28 (12): 1066-77.
- Guichet JM, Deromedis B, Donnan LT, Peretti G, Lascombes P, Bado F. Gradual femoral lengthening with the Albizzia intramedullary nail. J Bone Joint Surg (Am) 2003; 85 (5): 838-48.
- Hankemeier S, Gosling T, Pape HC, Wiebking U, Krettek C. Limb lengthening with the Intramedullary Skeletal Kinetic Distractor (ISKD). Oper Orthop Traumatol 2005; 17 (1): 79-101.
- Krieg AH, Speth BM, Foster BK. Leg lengthening with a motorized nail in adolescents : an alternative to external fixators? Clin Orthop 2008; (466) (1): 189-97.
- Leidinger B, Winkelmann W, Roedl R. Limb lengthening with a fully implantable mechanical distraction intramedullary nail. Z Orthop Ihre Grenzgeb 2006; 144 (4): 419-26.
- Maffulli N, Nele U, Matarazzo L. Changes in knee motion following femoral and tibial lengthening using the Ilizarov apparatus: a cohort study. J Orthop Sci 2001; 6 (4): 333-8.
- Neel MD, Heck R, Britton L, Daw N, Rao BN. Use of a smooth press-fit stem preserves physeal growth after tumor resection. Clin Orthop 2004; (426): 125-8.
- Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop 1990; (250): 81-104.
- Paley D, Herzenberg J, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 1994; 25 (3): 425.
- Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg (Am) 1997; 79 (10): 1464-80.
- Singh S, Lahiri A, Iqbal M. The results of limb lengthening by callus distraction using an extending intramedullary nail (Fitbone) in non-traumatic disorders. J Bone Joint Surg (Br) 2006; 88 (7): 938-42.
- Song H, Oh C, Mattoo R, Park B, Kim S, Park I, Jeon I, Ihn J. Femoral lengthening over an intramedullary nail using the external fixator: risk of infection and knee problems in 22 patients with a follow-up of 2 years or more. Acta Orthop 2005; 76 (2): 245-52.
- Tjernstrom B, Olerud S, Rehnberg L. Limb lengthening by callus distraction. Complications in 53 cases operated 1980-1991. Acta Orthop Scand 1994; 65 (4): 447-55.