Abstract
Background and purpose In a previous radiostereometric (RSA) trial the uncoated, uncemented, Interax tibial components showed excessive migration within 2 years compared to HA-coated and cemented tibial components. It was predicted that this type of fixation would have a high failure rate. The purpose of this systematic review and meta-analysis was to investigate whether this RSA prediction was correct.
Materials and methods We performed a systematic review and meta-analysis to determine the revision rate for aseptic loosening of the uncoated and cemented Interax tibial components.
Results 3 studies were included, involving 349 Interax total knee arthroplasties (TKAs) for the comparison of uncoated and cemented fixation. There were 30 revisions: 27 uncoated and 3 cemented components. There was a 3-times higher revision rate for the uncoated Interax components than that for cemented Interax components (OR = 3; 95% CI: 1.4–7.2).
Interpretation This meta-analysis confirms the prediction of a previous RSA trial. The uncoated Interax components showed the highest migration and turned out to have the highest revision rate for aseptic loosening. RSA appears to enable efficient detection of an inferior design as early as 2 years postoperatively in a small group of patients.
Aseptic loosening remains a major reason for revision surgery in total knee arthroplasty (TKA) (Cloke et al. Citation2008, SKAR report 2010). Since revision rates are generally low, it is necessary to follow up hundreds if not thousands of patients for a long period of time (10 years) to be able to detect inferior designs (Michelson et al. Citation1989).
A method for early detection of aseptic loosening based on few patients would be of value. Radiostereometric analysis (RSA) enables accurate measurement of migration of prosthetic components relative to bone (Selvik Citation1989), migration that has been shown to be associated with late aseptic loosening (Grewal et al. Citation1992, Karrholm et al. Citation1994, Ryd et al. Citation1995).
Although these findings are promising, few studies have actually investigated whether the RSA predictions are correct (Grewal et al. Citation1992, Karrholm et al. Citation1994, Ryd et al. Citation1995, Hauptfleisch et al. Citation2006). In TKA, the question thus remains: does TKA with increased early migration have higher revision rates for aseptic loosening?
We have already shown in a randomized RSA trial that uncoated Interax tibial components have increased early migration compared to HA-coated and cemented tibial components (Nelissen et al. Citation1998). We predicted that uncoated components would have a high failure rate. The aim of the present study was therefore to investigate whether this prediction of the previous RSA trial was correct. We performed a meta-analysis to evaluate the failure rate of these components.
Material and methods
Design of the meta-analysis, and rationale
The design was based on the Cochrane standards, and reporting of this meta-analysis follows the PRISMA guidelines (Liberati et al. Citation2009). In order to exclude confounding due to differences in prosthesis design, the meta-analysis was restricted to studies involving exactly the same implant as in the previously published RSA trial (Nelissen et al. Citation1998): the cruciate retaining (CR) Interax TKA tibial component (Howmedica/Stryker, Rutherford, NJ) with 2 polyethylene half bearings. The fixation of the components is either by cement or by bone ingrowth on uncoated or hydroxyapatite- (HA-) coated prosthetic surfaces. The cemented components had a diamond surface on the side that was within bone, whereas the uncemented components had a wire-mesh surface (2.25 mm2, corresponding to a circular pore diameter of 1,690 μm) with or without an HA coating.
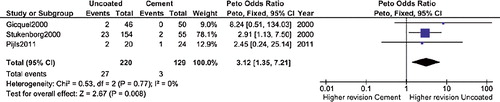
The outcome of interest was the number of revisions or recommended revisions for aseptic loosening of the tibial component, for each fixation separately. This outcome was compared to the early migration results of the RSA trial (Nelissen et al. Citation1998), which showed increased early migration of the uncoated tibial component compared to the cemented and HA-coated tibial components (). Uncemented components show high initial migration followed by stabilization (Nilsson et al. Citation1991, Onsten et al. Citation1998, Carlsson et al. Citation2005, Nilsson et al. Citation2006, Henricson et al. Citation2008, Dunbar et al. Citation2009, Wilson et al. Citation2012). Thus, we also present the migration rate of MTPM (mm/year) determined from the migration measured with the postoperative RSA examination as reference ().
Figure 1. Summary of the migration results of the previous RSA trial (Nelissen et al. Citation1998). The plot shows the mean migration —expressed as maximal total point motion (MTPM)—with 95% CI for each type of fixation of the tibial components: red dashed line for uncoated; green dotted line for HA-coated, and blue solid line for cemented. The uncoated tibial components showed the most migration.
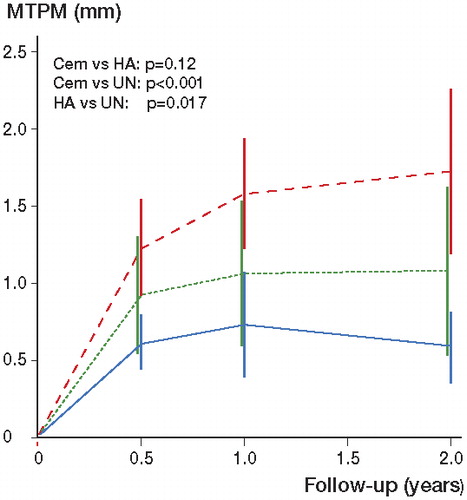
Table 1. Mean migration rate (MTPM) expressed in mm/year. The uncoated components showed the highest migration rate. The migration rate was determined from the migration measured with the postoperative RSA examination as reference
Literature search
The literature search is the foundation on which a systematic review and meta-analysis is built. Inadequate search strategies have been shown to give biased results (Vochteloo et al. Citation2010). We therefore adopted a thorough search strategy in collaboration with a medical librarian, JWS. The following bibliographies were searched up to and including March 2011: PubMed, EMBASE (OVID version), Web of Science, the Cochrane Library, Current Contents Connect, CINAHL (Ebscohost-version), and Academic Search Premier (Ebscohost version). Additionally, the websites of the following medical journal publishers were searched: Elsevier ScienceDirect, Wiley Blackwell, Lippincott-Williams & Wilkins, Highwire, Informaworld/Informahealth, and Springer. To reduce the effect of any publication bias, the “gray literature” was searched up to and including March 2011: WHO International Clinical Trials Registry Platform and the proceedings of major conferences (NOF, AAOS, EFORT, ESSKA, ISTA). Furthermore, the bibliographies of included studies were hand-searched for relevant publications. Also, various lesser-known databases were searched, e.g. ScienceGov and OAIster. Finally, Google Scholar was searched.
The search involved all fields and full-text options to screen if the following component was mentioned anywhere in a manuscript (see Supplementary data for further details): “Interax” and relevant abbreviations and extensions. Since “Interax” is a registered brand name for a particular TKA model, it was assumed to be spelled out in the same way in the text of a manuscript irrespective of the language used. We did not use any language restrictions.
Study selection
All studies were subjected to the following inclusion criteria: (1) the study comprises an original patient cohort treated with the Interax TKA (Howmedica, Rutherford, NJ); (2) the cruciate retaining Interax prosthesis with half bearings is used (posterior stabilised Interax and Interax ISA versions are excluded); (3) the type of fixation of the tibial component and the number of knees receiving this type of fixation is adequately reported; (4) the number of revisions or recommended revisions for aseptic loosening of the tibial component is reported for each fixation separately; and (5) at least 2 fixation types are compared.
2 reviewers, BGP and MJN, independently judged all studies according to these 5 inclusion criteria. In cases where the title and abstract were inconclusive, the full-text article was obtained. Any disagreement between the reviewers was resolved by re-examination and subsequent discussion to reach a consensus. Both randomized controlled trials (RCTs) and observational studies were considered for inclusion.
Quality assessment and data extraction
The quality of each study included was independently appraised by 2 reviewers, BGP and MJN, using the Jadad scale (Jadad et al. Citation1996). The same reviewers independently extracted relevant data from each of the studies that were included. Any disagreement between the reviewers was resolved by re-examination and subsequent discussion to reach a consensus.
Statistics
Before considering a meta-analysis (pooling of data), we investigated whether it was appropriate to pool the data. Studies should be similar in design and in patient population. In addition, the variability in effect size between studies should not exceed those expected from sampling error: low heterogeneity is desirable. Heterogeneity was assessed by calculating the I2 statistic, which is appropriate for a small number of studies (Higgins et al. Citation2002). Publication bias was assessed with a funnel plot (Sterne et al. Citation2000). Meta-analysis was performed with Peto odds ratio (OR) fixed-effect pooling and Mantel-Haenszel random-effects pooling for the risk difference (RD) and number needed to treat (NNT). The NNT was defined as the number of cemented tibial components that would have to be implanted in order to prevent 1 revision as compared to when uncoated components were implanted. We used RevMan software.
Results
Study selection and study characteristics
The search strategy resulted in 268 unique hits, and 4 of these studies could be included (Gicquel et al. Citation2000, Stukenborg-Colsman and Wirth Citation2000, Wirth 2004, Petersen et al. Citation2005, Pijls et al. Citation2012) (). 2 papers were published in English (Petersen et al. Citation2005, Pijls et al. Citation2012), 1 in German (Stukenborg-Colsman et al. Citation2000), and 1 in French (Gicquel et al. Citation2000) (). 3 studies compared the cemented component to the uncoated one (Gicquel et al. Citation2000, Stukenborg-Colsman and Wirth Citation2000, Pijls et al. Citation2012). 1 of these studies (Stukenborg-Colsman and Wirth Citation2000) was part of a thesis (Barisic and Wirth Citation2004), which we used for more details. 1 of these studies (Pijls Citation2012) was the long-term follow-up of the RSA trial (Nelissen Citation1998) and reported 3 revisions (2 uncoated and 1 cemented) for aseptic loosening of the tibial component. Since only 1 study with 18 TKAs (Petersen et al. Citation2005) compared the HA-coated tibial component to the uncoated one, no pooling was done for this comparison. The funnel plot did not show any publication bias.
Figure 2. Flow diagram showing details of study selection. In cases where the title and abstract were insufficiently conclusive, the full text article was obtained.
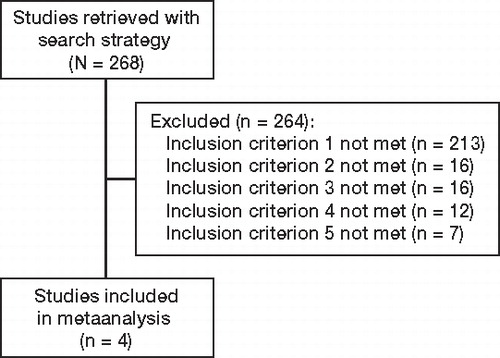
Table 2. Characteristics of the studies included
Uncoated vs. cemented tibial component
349 TKAs were included in the meta-analysis of uncoated and cemented components. There were 30 revisions of the tibial component for aseptic loosening, of which 27 were for the uncoated components and 3 were for the cemented component.
The odds of revision due to aseptic loosening of the uncoated tibial component was 3.1 times higher than for the cemented tibial component: pooled OR = 3.1 (95% CI: 1.4–7.2) (). The pooled risk difference was 7% (CI: 3–12) in favor of the cemented component. The number needed to treat (NNT) was 14 in favor of the cemented component (CI: 8–33). This means that for every 14 patients treated with a cemented Interax tibial component, 1 revision for aseptic loosening is prevented compared to the uncoated component.
Risk of bias within studies
The sequence of randomization and concealment of allocation were described and appropriate in 2 studies (Gicquel et al. Citation2000, Pijls et al. Citation2012). In 1 study (Petersen et al. Citation2005), randomization was performed but the method and concealment was inadequately described and in another study (Stukenborg-Colsman and Wirth Citation2000) no randomization was performed. In the non-randomized study, the decision for implanting either a cemented or an uncoated uncemented tibial component was made by the surgeon during the operation, leading to confounding—because cemented components were used for cases with reduced bone quality (Stukenborg-Colsman and Wirth Citation2000). This confounding would lead to a possible underestimation of the revision rate of the uncoated uncemented tibial component. Thus, the higher revision rate for the uncoated components than for the cemented ones may have been an underestimation of the true revision rate.
In all studies blinding, was a potential source of bias. Since evaluation of radiographs is essential for the indication for a revision and the presence or absence of cement cannot be masked on the radiograph, blinding—if possible at all—was not performed in any of the studies.
The number of withdrawals and dropouts was adequately described in all studies. The number of patients who were lost to follow-up (corresponding to 8 cemented and 12 uncoated components) was high in the study by Gicquel et al. Citation2000 (see ).
All 3 studies that compared cemented and uncoated components included all patients consecutively during the inclusion period, and thus reduced the possibility of selection bias (Stukenborg-Colsman and Wirth Citation2000, Gicquel et al. Citation2000, Pijls et al. Citation2012).
Discussion
Uncoated vs. cemented components
Our aim was to investigate whether the predictions of a previous trial using radiostereometric analysis (RSA) were correct. Since the uncoated Interax components had shown the highest migration, it was predicted that this type of fixation would have a high failure rate (Nelissen et al. Citation1998). The results of the meta-analysis showed a statistically significant 3 times higher revision rate for the uncoated uncemented component than for the cemented tibial component. Thus, the prediction from the previous RSA trial was correct: the uncoated tibial components showed the highest migration and had the highest revision rate for aseptic loosening. The uncoated tibicomponents also continued to migrate after 1 year, whereas the HA-coated components stabilized after 1 year. This is in accordance with a recent report by Wilson et al. (Citation2012), which showed that tibial components can give solid fixation despite high levels of initial migration.
In the RSA trial, the high degree of migration of the uncoated uncemented tibial components was identified within 2 years in a small group of 44 patients (24 in the cemented group and 20 in the non-coated group) compared to the 349 in the meta-analysis. This emphasizes the value of RSA for the early detection of inferior TKA designs in a small series of patients (Grewal et al. Citation1992, Karrholm et al. Citation1994, Ryd et al. Citation1995).
It is noteworthy that none of the individual traditional clinical studies with large numbers of patients and medium-term or long-term follow-up showed a statistically significant difference in revision rates between the uncoated uncemented and cemented Interax tibial components (Gicquel et al. Citation2000, Stukenborg-Colsman and Wirth Citation2000). Only when the results of these studies were combined in a meta-analysis setting did the high revision rate in the uncoated components become clearly visible.
Uncoated vs. HA-coated components
One of the selected studies compared the uncoated tibial component with the HA-coated component (Petersen et al. Citation2005). This study involved only 18 patients who were followed for 2 years. Because of the short follow-up and small patient cohort, it was not appropriate to perform a meta-analysis for the comparison of uncoated and HA-coated components. The uncoated Interax tibial component has been withdrawn from the market after the results of the RSA trial were published. Since the HA-coated component migrates less than the uncoated tibial component, a beneficial effect of the HA coating would be expected. Less migration of an HA-coated component than of a non-coated component has also been demonstrated for the Interax CR by Østgaard et al. (Citation1999). Their migration results were similar to those of our RSA trial (Nelissen et al. Citation1998), despite differences in patient characteristics: all their patients were suffering from osteoarthritis, as compared to one third with osteoarthritis and two thirds with rheumatoid arthritis in our RSA trial.
Strengths and limitations
Our search strategy was thorough and complete. This is underscored by the fact that we found 2 studies that were published in the non-English literature. Although our research question was highly specialized, i.e. fixation of a single type of TKA, we were still able to include 3 studies. This is not uncommon for orthopedic meta-analysis, even in Cochrane reviews (Jacobs et al. Citation2004).
The studies included were of moderate quality, mostly due to issues with blinding for the fixation method—which is a general problem in any study comparing cemented and uncemented components and was not specific to the present meta-analysis.
Publication bias generally favors the newly introduced treatment (Gotzsche Citation1987), the uncoated uncemented fixation in this case. Since the studies included in this meta-analysis did not find a positive effect for the uncoated components, publication bias was probably not a major factor here. Thus, we are confident that our conclusion is correct: the uncoated tibial component of the Interax has a higher revision rate for aseptic loosening.
The I-statistic was 0%, so there was no indication of statistical heterogeneity. Despite differences in patient demographics, surgical technique, or study design, all ORs were on the same side, i.e. showed higher—although not individually significantly higher—revision rates for the uncoated component, and this confirms the predictions of the RSA trial.
Future perspectives
More than a decade ago, Liow and Murray (Citation1997) and Muirhead-Allwood (Citation1998) called for a more evidence-based evaluation and clinical introduction of (new) prosthetic designs and fixations. CitationMalchau (2000) proposed a phased evidence-based introduction of new designs. Recently, a renewed call for concrete steps has been made towards such an evidence-based clinical introduction (McCulloch et al. Citation2009, Schemitsch et al. Citation2010). A disastrous design can be detected early postoperatively in a small group of patients by RSA, which therefore has the potential to play an important role in the clinical introduction of new models and fixation methods in total knee arthroplasty. For example, in vitro testing-machine studies should be followed by 2-year RSA studies in small cohorts in different institutions worldwide, followed by larger comparative studies, after which introduction to the market can be started (CitationMalchau 2000)—with the latter also involving follow-up in national registries. In this way, a more phased prosthesis introduction to the market is guaranteed, as is currently the standard for pharmacological agents.
Supplementary Material
Download PDF (83.4 KB)The following authors designed the study (SM, BGP, RGN, ERV), designed the search strategy for the literature search (JWS), performed the study selection (BGP, MJN), appraised the quality of the literature (BGP, MJN), analyzed the data (BGP, SM), wrote the draft manuscript (ERV, BGP, JWS, MJN), and ensured the accuracy of the data and the analysis (SM, RGN). Critical revision of the manuscript was performed by all authors.
The authors thank the Atlantic Innovation Fund (Atlantic Canada Opportunities Agency) and the Dutch Arthritis Association (LRR 13) for providing funding for this study. The Atlantic Innovation Fund and the Dutch Arthritis Association (LRR 13) did not take part in the design and conduction of the study; in the collection, management, analysis, and interpretation of the data; or in the preparation, review, and approval of the manuscript.
- Barisic M, Wirth CJ. 5-7-Jahres-Ergebnisse des Interax-Knieendoprothesensystems. Dissertation Hannover Medizinischen Hochschule. 2004.
- Carlsson A, Bjorkman A, Besjakov J, Onsten I. Cemented tibial component fixation performs better than cementless fixation: a randomized radiostereometric study comparing porous-coated, hydroxyapatite-coated and cemented tibial components over 5 years. Acta Orthop 2005; 76 (3): 362-9.
- Cloke DJ, Khatri M, Pinder IM, McCaskie AW, Lingard EA. 284 press-fit Kinemax total knee arthroplasties followed for 10 years: poor survival of uncemented prostheses. Acta Orthop 2008; 79 (1): 28-33.
- Dunbar MJ, Wilson DA, Hennigar AW, Amirault JD, Gross M, Reardon GP. Fixation of a trabecular metal knee arthroplasty component. A prospective randomized study. J Bone Joint Surg (Am) 2009; 91 (7): 1578-86.
- Gicquel P, Kempf JF, Gastaud F, Schlemmer B, Bonnomet F. Comparative study of fixation mode in total knee arthroplasty with preservation of the posterior cruciate ligament. Rev Chir Orthop Reparatrice Appar Mot 2000; 86 (3): 240-9.
- Gotzsche PC. Reference bias in reports of drug trials. Br Med J (Clin Res Ed) 1987; 295 (6599): 654-6.
- Grewal R, Rimmer MG, Freeman MA. Early migration of prostheses related to long-term survivorship. Comparison of tibial components in knee replacement. J Bone Joint Surg (Br) 1992; 74 (2): 239-42.
- Hauptfleisch J, Glyn-Jones S, Beard DJ, Gill HS, Murray DW. The premature failure of the Charnley Elite-Plus stem: a confirmation of RSA predictions. J Bone Joint Surg (Br) 2006; 88 (2): 179-83.
- Henricson A, Linder L, Nilsson KG. A trabecular metal tibial component in total knee replacement in patients younger than 60 years: a two-year radiostereophotogrammetric analysis. J Bone Joint Surg (Br) 2008; 90 (12): 1585-93.
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21 (11): 1539-58.
- Jacobs W, Anderson P, Limbeek J, Wymenga A. Mobile bearing vs fixed bearing prostheses for total knee arthroplasty for post-operative functional status in patients with osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev 2004; (2): CD003130.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996; 17 (1): 1-12.
- Karrholm J, Borssen B, Lowenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg (Br) 1994; 76 (6): 912-7.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6 (7): e1000100.
- Liow RY, Murray DW. Which primary total knee replacement? A review of currently available TKR in the United Kingdom. Ann R Coll Surg Engl 1997; 79 (5): 335-40.
- Malchau H. Introducing new technology: a stepwise algorithm. Spine (Phila Pa 1976) 2000; 25 (3): 285.
- McCulloch P, Altman DG, Campbell WB, Flum DR, Glasziou P, Marshall JC, No surgical innovation without evaluation: the IDEAL recommendations. Lancet 2009; 374 (9695): 1105-12.
- Michelson JD, Riley LH, Jr. Considerations in the comparison of cemented and cementless total hip prostheses. J Arthroplasty 1989; 4 (4): 327-34.
- Muirhead-Allwood SK. Lessons of a hip failure. BMJ 1998; 316 (7132): 644.
- Nelissen RG, Valstar ER, Rozing PM. The effect of hydroxyapatite on the micromotion of total knee prostheses. A prospective, randomized, double-blind study. J Bone Joint Surg (Am) 1998; 80 (11): 1665-72.
- Nilsson KG, Karrholm J, Ekelund L, Magnusson P. Evaluation of micromotion in cemented vs uncemented knee arthroplasty in osteoarthrosis and rheumatoid arthritis. Randomized study using roentgen stereophotogrammetric analysis. J Arthroplasty 1991; 6 (3): 265-78.
- Nilsson KG, Henricson A, Norgren B, Dalen T. Uncemented HA-coated implant is the optimum fixation for TKA in the young patient. Clin Orthop 2006; (448): 129-39.
- Onsten I, Nordqvist A, Carlsson AS, Besjakov J, Shott S. Hydroxyapatite augmentation of the porous coating improves fixation of tibial components. A randomised RSA study in 116 patients. J Bone Joint Surg (Br) 1998; 80 (3): 417-25.
- Østgaard SE, Dirksen KL, Lund B. Hydroxyapatite coating in total knee arthroplasty - a randomised RSA study of tibial components. Acta Orthop (Suppl 289) 1999; 70: 4.
- Petersen MM, Gehrchen PM, Ostgaard SE, Nielsen PK, Lund B. Effect of hydroxyapatite-coated tibial components on changes in bone mineral density of the proximal tibia after uncemented total knee arthroplasty: a prospective randomized study using dual-energy x-ray absorptiometry. J Arthroplasty 2005; 20 (4): 516-20.
- Pijls BG, Valstar ER, Kaptein BL, Fiocco M, Nelissen RG. The beneficial effect of hydroxyapatite lasts: a randomized radiostereometric trial comparing hydroxyapatite coated, uncoated and cemented tibial components up to 16 years. Acta Orthop 2012; 83 (2): 135-41.
- RevMan (Review Manager) (Computer program). Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008.
- Ryd L, Albrektsson BE, Carlsson L, Dansgard F, Herberts P, Lindstrand A, Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg (Br) 1995; 77 (3): 377-83.
- Schemitsch EH, Bhandari M, Boden SD, Bourne RB, Bozic KJ, Jacobs JJ, The evidence-based approach in bringing new orthopaedic devices to market. J Bone Joint Surg (Am) 2010; 92 (4): 1030-7.
- Selvik G. Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. Acta Orthop Scand (Suppl 232) 1989; 232: 1-51.
- Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol 2000; 53 (11): 1119-29.
- Stukenborg-Colsman C, Wirth CJ. Knee endoprosthesis: clinical aspects. Orthopade 2000; 29 (8): 732-8.
- Swedish Knee Arthroplasty Registry Report 2010 V1.0. http://wwwkneenkose.accessed 06-06-2011.
- Vochteloo AJ, Pijls BG, van der Heide HJ. Sutures v staples. Let’s add three other studies. Bmj 2010; 340: c2627.
- Wilson DA, Richardson G, Hennigar AW, Dunbar MJ. Continued stabilization of trabecular metal tibial monoblock total knee arthroplasty components at 5 years—measured with radiostereometric analysis. Acta Orthop 2012: 83 (1): 36-40.
Appendix
Supplementary data are available at our website (www.actaorthop.org), identification number 4935.