Abstract
Fast-track hip and knee arthroplasty aims at giving the patients the best available treatment at all times, being a dynamic entity. Fast-track combines evidence-based, clinical features with organizational optimization including a revision of traditions resulting in a streamlined pathway from admission till discharge – and beyond. The goal is to reduce morbidity, mortality and functional convalescence with an earlier achievement of functional milestones including functional discharge criteria with subsequent reduced length of stay and high patient satisfaction. Outcomes are traditionally measured as length of stay; safety aspects in the form of morbidity/mortality; patient satisfaction; and – as a secondary parameter – economic savings.
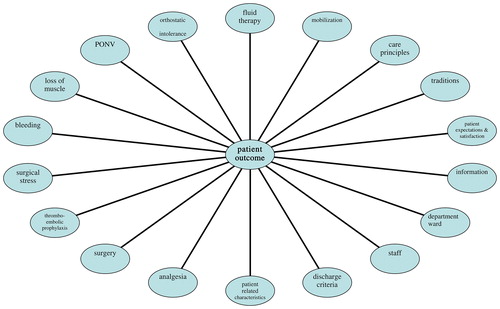
Optimization of the clinical aspects include focusing on analgesia; DVT-prophylaxis; mobilization; care principles including functional discharge criteria; patient-characteristics to predict outcome; and traditions which may be barriers in optimizing outcomes. Patients should be informed and motivated to be active participants and their expectations should be modulated in order to improve satisfaction.
Also, organizational aspects need to be analyzed and optimized. New logistical approaches should be implemented; the ward ideally (re)structured to only admit arthroplasties; the staff educated to have a uniform approach; extensive preoperative information given including discharge criteria and intended length of stay.
This thesis includes 9 papers on clinical and organizational aspects of fast-track hip and knee arthroplasty (I–IX). A detailed description of the fast-track set-up and its components is provided. Major results include identification of patient characteristics to predict length of stay and satisfaction with different aspects of the hospital stay (I); how to optimize analgesia by using a compression bandage in total knee arthroplasty (II); the clinical and organizational set-up facilitating or acting as barriers for early discharge (III); safety aspects following fast-track in the form of few readmissions in general (IV) and few thromboembolic complications in particular (V); feasibility studies showing excellent outcomes following fast-track bilateral simultaneous total knee arthroplasty (VI) and non-septic revision knee arthroplasty (VII); how acute pain relief in total hip arthroplasty is not enhanced by the use of local infiltration analgesia when multi-modal opioid-sparing analgesia is given (VIII); and a detailed description of which clinical and organizational factors detain patients in hospital following fast-track hip and knee arthroplasty (IX).
Economic savings following fast-track hip and knee arthroplasty is also documented in studies, reviews, metaanalyses and Cochrane reviews – including the present fast-track (ANORAK).
In conclusion, the published results (I–IX) provide substantial, important new knowledge on clinical and organizational aspects of fast-track hip and knee arthroplasty – with concomitant documented high degrees of safety (morbidity/mortality) and patient satisfaction.
Future research strategies are multiple and include both research strategies as efforts to implement the fast-track methodology on a wider basis. Research areas include improvements in pain treatment, blood saving strategies, fluid plans, reduction of complications, avoidance of tourniquet and concomitant blood loss, improved early functional recovery and muscle strengthening. Also, improvements in information and motivation of the patients, preoperative identification of patients needing special attention and detailed economic studies of fast- track are warranted.
Abstract in Danish - Resume på dansk
Formålet med fast-track hofte- og knæalloplastik er at give patienterne den til enhver tid bedste behandling, dvs. at være et dynamisk koncept. Fast-track kombinerer evidens-baserede kliniske tiltag med optimerede organisatoriske ditto, herunder en kritisk revision af traditioner, resulterende i et strømlinet forløb fra indlæggelse til udskrivelse – og også senere inkluderende hele det perioperative forløb. Formålet er at reducere morbiditet, mortalitet og funktionel rekonvalescens med tidligere opfyldelse af funktionelle mål inklusiv udskrivelseskriterier med deraf resulterende kortere indlæggelsesvarighed og høj patient tilfredshed. Resultater heraf opgøres traditionelt som måling af postoperativ indlæggelsesvarighed, forekomst af komplikationer/genindlæggelser og mortalitet, måling af patient tilfredshed og – som sekundær parameter – økonomisk besparelse.
Optimering af de kliniske aspekter inkluderer fokus på analgesi, tromboembolisk profylakse, mobilisation, pleje-principper inkluderende funktionelle udskrivelseskriterier, patient-karakteristika forbundet med indlæggelsesvarighed, og traditioner som kan påvirke udkommet negativt.
Patienter bør informeres og motiveres til aktiv deltagelse ligesom deres forventninger bør justeres til faktiske forhold for at bedre tilfredshed med forløb og udkomme.
Ligeledes bør organisatoriske aspekter analyseres og optimeres. Nye logistiske tiltag kan implementeres, sengeafdelingen (re-)struktureres til kun at modtage alloplastik-patienter, personalet undervises i fast-track principper til opnåelse af identisk patient-tilgang, grundig information om forløbet inklusiv udskrivelseskriterier gives samt oplysning om forventet hospitaliserings-varighed.
Denne disputats bygger på 9 studier omhandlende kliniske og organisatoriske forhold ved fast-track hofte- og knæalloplastik kirurgi (I–IX), ligesom en detaljeret beskrivelse af komponenterne i fast-track foretages. Vigtige resultater inkluderer identificering af patient-karakteristika, der påvirker indlæggelsesvarighed og tilfredshed med forskellige aspekter af forløbet (I); hvorledes anvendelse af en komprimerende bandage i forbindelse med lokal infiltrations analgesi kan optimere denne ved total knæalloplastik (II); identifikation af kliniske og organisatoriske faktorer, der faciliterer eller hæmmer tidlig udskrivelse (III); sikkerheds-aspekter efter fast-track i form af få genindlæggelser i almindelighed (IV) og få tromboemboliske komplikationer i særdeleshed (V); demonstration af gode resultater ved fast-track bilateral simultan knæalloplastik (VI) og fast-track non-septisk revisions-knæalloplastik (VII); hvorledes umiddelbar smerte-lindring efter total hoftealloplastik ikke bedres yderligere ved brug af lokal infiltrationsanalgesi, når der anvendes multimodal opioid-besparende analgesi (VIII); og en detaljeret beskrivelse af hvilke kliniske og organisatoriske faktorer, der forhindrer opfyldelse af funktionelle udskrivelses-kriterier og dermed udskrivelse efter fast-track hofte- og knæalloplastik (IX).
Økonomiske besparelser ved fast-track forløb sammenholdt med mere konventionelle forløb gennemgås med fokus på aktuelle fast-track forløb (ANORAK-HH). Oversigtsartikler, metaanalyser og Cochrane reviews har samstemmende fundet økonomisk gevinst ved fast-track.
Konklusivt giver de publicerede resultater (I–IX) betydelig vigtig ny viden om kliniske og organisatoriske aspekter af fast-track hofte- og knæalloplastik forløb med samtidig dokumentation af en høj grad af sikkerhed (morbiditet/mortalitet) og patient tilfredshed.
Fremtidige forskningsområder er multiple og inkluderer både klinisk forskning samt måder, hvorpå fast-track kan implementeres bedre og bredere. Klinisk forskning vil omhandle bedret smertebehandling, blødningsreducerende strategier, væskebehandling, reduktion af komplikationer, undladelse af tourniquet-anvendelse (med samtidig blødningsbesparelse), forbedringer af tidlig mobilisation og funktionel rekonvalescens, samt muskel styrkelse. Ligeledes vil der fokuseres på optimeret information og motivation af patienter i fast-track, præoperativ identifikation af patienter med særlige behov (smerte, tromboemboliske komplikationer) samt detaljerede økonomiske studier af moderne fast-track med 1–3 dages indlæggelse.
List of papers
This doctoral thesis is based on the following 9 papers, referred to in the text by Roman numerals (I–IX):
(I) Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 2008; 79: 168-73.
(II) Andersen LØ, Husted H, Otte KS, Kristensen BB, Kehlet H. A compression bandage prolongs duration of local infiltration analgesia in total knee arthroplasty. Acta Orthop 2008; 79: 800-5.
(III) Husted H, Hansen HC, Holm G, Bach-Dal C, Rud K, Andersen KL, Kehlet H. What determines length of stay after total hip and knee arthroplasty? A nationwide study in Denmark. Arch Orthop Trauma Surg 2010; 130: 263-8.
(IV) Husted H, Otte KS, Kristensen BB, Ørsnes T, Kehlet H. Readmissions after fast-track hip and knee arthroplasty. Arch Orthop Trauma Surg 2010; 130: 1185-91.
(V) Husted H, Kristensen BB, Otte KS, Ørsnes T, Wong C, Kehlet H. Low incidence of thromboembolic complications in a fast-track set-up with hip and knee arthroplasty. Acta Orthop 2010; 81: 599-605.
(VI) Husted H, Troelsen A, Otte KS, Kristensen BB, Holm G, Kehlet H. Fast-track surgery for bilateral total knee arthroplasty. J Bone Joint Surg (Br) 2011; 93: 351-6.
(VII) Husted H, Otte KS, Kristensen BB, Kehlet H. Fast-track revision knee arthroplasty. Acta Orthop 2011; 82(4): 438-40.
(VIII) Lunn TH, Husted H, Solgaard S, Kristensen BB, Otte KS, Kjersgaard AG, Gaarn-Larsen L, Kehlet H. Intraoperative Local Infiltration Analgesia for early analgesia after Total Hip Arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med 2011; 36(5): 424-9.
(IX) Husted H, Lunn TH, Troelsen A, Gaarn-Larsen L, Kristensen BB, Kehlet H. Why in hospital after fast- track hip and knee arthroplasty. Acta Orthop 2011; W
Acknowledgements
All studies that make the basis of this doctoral thesis have been performed during my ongoing employment as head of the arthroplasty section, Department of Orthopedic Surgery, Hvidovre Hospital.
I thank my co-authors: Lasse Ø Andersen, Kristoffer Lande Andersen, Charlotte Bach-Dal, Hans Christian Hansen, Gitte Holm, Steffen Jacobsen, Henrik Kehlet, Anne Grethe Kjersgaard, Billy B Kristensen, Lissi Gaarn-Larsen, Troels H Lunn, Kristian Stahl Otte, Kirsten Rud, Søren Solgaard, Anders Troelsen, Christian Wong, and Thue Ørsnes; you all made important practical and theoretical contributions to the studies and I thank you so much for sharing many fruitful, fun and inspiring hours in our research group.
I would like to acknowledge Billy B Kristensen, head of orthopedic anaesthesiology, for sharing my interest in optimization of patient care and for exquisite collaboration on so many levels. Also, a special thank you to Kristian Stahl Otte for all your help and support throughout the years. You both – as well as all my other colleagues – are setting such a high standard in patient treatment and it is a pleasure and a privilege to be working with you. Recently, Anders Troelsen has joined our team, and I thank him for his dedication with patients, insight, support and friendship – I am sure that many studies will emerge from our ongoing and future collaboration.
I want to thank my old friend Tim Toftgaard Jensen for many years of inspiration – which set the standard for doing it right: in the operating theater, in patient care and in research to strengthen decision-making. Also a very warm thank you to Stig Sonne-Holm, who apart from stimulating my research also has guided me in the statistical corners of research in my earlier days.
I thank Peter Gebuhr for being a great source of inspiration, for never-ending support and above all for facilitating research by granting me a weekly day to do so – and also for giving my time and space to pursue my interest in sharing our results with the rest of the world.
I thank my two secretaries, Mette Valbo Skovsen and Lene Lütken, for their support with data registration, databases and helping me through busy days.
I thank the “Lundbeck Centre for fast-track hip and knee arthroplasty” for generous support for funding of research assistants, the Danish Health Board for support for the nationwide audit study, and the Foundations “læge Fritz Karners og hustrus Fond” and “Edgar Schnohr og hustru Gilberte Schnohr`s Fond” for financial support to allow me to take time off to write this thesis.
I am truly grateful to the entire nursing staff in my department 310 for their dedication and support, both during daily activities and especially in helping with the many, many studies: thank you.
Also, I would like to thank Biomet (Lars Christiansen, Henrik Gamsgaard), NMS (Søren Rasmussen, Kim Hafstrøm), Protesekompagniet (Kim Jørgensen, Michael Kristensen) and Smith & Nephew (Mads Boris) for support, help, good discussions, excellent collaboration and friendship throughout the years.
Above all, I am very indebted to Professor Henrik Kehlet for his enormous support, always constructive criticism, and for a never-ending interest in trying to do better for the patients. It is highly contagious! Henrik has always encouraged me to ask the simple questions beginning with “why…” and I thank him from the bottom of my heart for his great support, help and friendship. One of these days I may have to let him win a few points on the tennis court…
Finally, a very special “thank you” to my wife Tina and my children Emma Louise and Christian Emil for your support; I love you and dedicate this thesis to you.
Summary of papers
(I) Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients
This prospective cohort study identifies patient characteristics associated with LOS and patient satisfaction after total hip and knee arthroplasty in a self-designed fast-track set-up, which is outlined. 712 consecutive, unselected patients operated with primary, unilateral arthroplasty had epidemiological, physical, and perioperative parameters registered and correlated to LOS and patient satisfaction. 92% of the patients were discharged to their homes within 5 days, and 41% were discharged within 3 days. A number of patient characteristics were found to influence postoperative outcome regarding LOS (among these especially age, sex, ASA-score, the need for blood transfusion, and time till first mobilization) and patient satisfaction (positive association with short LOS and advanced age) or and also logistical barriers for early discharge were identified (operation at the end of the week).This fast-track had short LOS (3.8 days) with high patient satisfaction and few readmissions within 3 months (5–6%).
(II) A compression bandage prolongs duration of local infiltration analgesia in total knee arthroplasty
This prospective, randomized study on one of the components of the high-volume local infiltration analgesia technique (LIA, 0.2% Ropivacaine, 170 mL) after total knee arthroplasty studied the role of bandaging to prolong analgesia. 48 patients undergoing fast-track TKA were randomized to receive a compression or a non-compression bandage with the assessment of pain for 24 h postoperatively. Pain at rest, during flexion, or during straight leg lift was lower for the first 8 h in patients with compression bandage than in those with non-compression bandage and with a similar low use of oxycodone and mean LOS (3.0 days). Thus, a compression bandage is recommended to improve analgesia after LIA in total knee arthroplasty.
(III) What determines length of stay after total hip and knee arthroplasty? A nationwide study in Denmark
This prospective nationwide study identified logistical and clinical areas of importance for LOS by identifying departments with short and long LOS and evaluating their set-up. The three departments with the shortest and the three with the longest LOS were identified based on the National Register on Patients in 2004 on LOS following THA and TKA. The logistical and clinical set-up was examined to identify factors acting as facilitators or barriers for early rehabilitation and discharge. Also, patients from these departments answered a questionnaire regarding satisfaction with components of their stay, co-morbidity, sex and age. Mean LOS was 7.4 and 8.0 days after THA and TKA, respectively, with patients staying from 4.5 to 12 days. Departments with short LOS were characterized by both logistical (homogenous entities, regular staff, high continuity, using more time on and up to date information including expectations on a short stay, functional discharge criteria) and clinical features (multimodal opioid sparing analgesia, early mobilisation and discharge when criteria were met) facilitating quick rehabilitation and discharge. Patient demographics from departments with the shortest stay were similar regarding age, sex and co-morbidities compared to patients from departments with longer stays, but the former patients were either as satisfied – or more satisfied – with all parts of their stay. There was no difference in staffing (nurses/physiotherapists) between the two types of departments.
(IV) Readmissions after fast-track hip and knee arthroplasty
This prospective cohort study of 1,731 consecutive, unselected patients operated with primary THA or TKA in a fast-track set-up studied safety aspects in the form of deaths and readmissions following the fast-track set-up in general and the risk of dislocation after THA and manipulation after TKA in specific. Mean LOS decreased from 6.3 to 3.1 days in the study period of 5 years and within 90 days, 15.6% of patients following TKA were readmitted as opposed to 10.9% after THA (p = 0.005). 3 deaths (0.17%) were associated with clotting episodes. Suspicion of DVT (not found) and suspicion of infection made up half of the readmissions. Readmissions in general and for thromboembolic events, dislocations and manipulations in specific did not increase with decreasing
LOS. It is concluded, that fast-track does not increase death or readmission rate following THA and TKA compared to other studies on more conventional stays and fast-track is thus considered safe regarding mortality and morbidity.
(V) Low incidence of thromboembolic complications in a fast-track set-up with hip and knee arthroplasty
This prospective cohort study evaluates the impact of short-duration pharmacological thromboprophylaxis combined with early mobilization and short hospitalization on the incidence of death, PE and DVT. 1,977 consecutive, unselected patients were operated with primary THA, TKA, or BSTKA in a well-described standardized fast-track set-up during 5 years. Patients received DVT prophylaxis with low-molecular-weight heparin starting 6–8 h after surgery until discharge only. All re-admissions and deaths within 30 and 90 days were analyzed using the national health register, concentrating especially on clinical DVT (confirmed by ultrasound and elevated D-dimer), PE, or sudden death. Numbers were correlated to days of prophylaxis (LOS). Mean LOS decreased from 7.3 days to 3.1 days. 3 deaths (0.15%) were associated with clotting episodes and overall, 11 clinical DVTs (0.56%) and 6 PEs (0.30%) were found. The vast majority of events took place within 30 days; only 1 death and 2 DVTs occurred between 30 and 90 days. During the last 2 years (854 patients), when patients were mobi-lized within 4 h postoperatively and the duration of DVT pro-phylaxis was shortest (1–4 days), the mortality was 0% and no DVT or PE were found following BSTKA. These figures compare favorably with published regimens with extended prophylaxis (up to 36 days) and hospitalization up to 11 days and question the need of extended thromboprophylaxis, when patients are mobilized early.
(VI) Fast-track bilateral total knee arthroplasty
This prospective cohort study analyzes the outcome of 150 consecutive, but selected, bilateral simultaneous total knee arthroplasties compared to 271 unilateral total knee arthroplasties in a standardized fast-track setting. Apart from staying longer (mean 4.7 days vs. 3.3 days) and using more blood transfusions; the outcome at 3 months and 2 years follow-up was identical or better in the bilateral group regarding morbidity, mortality, satisfaction, range of motion, pain, use of walking aids, ability to return to work and ability to perform activities of daily living. Bilateral simultaneous total knee arthroplasty can be performed in a fast-track set-up with satisfactory results.
(VII) Fast-track revision knee arthroplasty
This prospective cohort study on 29 consecutive, unselected patients operated with 30 revision total knee arthroplasties for non-septic indications in a fast-track setting evaluated whether patients undergoing revision TKA could follow a standardized fast-track set-up designed for primary TKA – with a similar outcome as primary TKA. LOS was median 2 (1–4) days for all but 1 patient who was transferred to another hospital for logistical reasons. No patient died within 3 months and 3 patients were readmitted (2 for suspicion of DVT but not found and one for manipulation). Patient satisfaction was high. It is concluded, that patients undergoing revision TKA for non-septic reasons can follow a fast-track set-up with an outcome comparable to primary TKA regarding LOS, morbidity, and satisfaction.
(VIII) Intraoperative local infiltration analgesia for early analgesia after total hip arthroplasty: a randomized, double-blind, placebo-controlled trial
This prospective randomized, double-blind, placebo-controlled study evaluated if intraoperative high-volume LIA, in addition to a multimodal oral analgesic regime, would further reduce acute postoperative pain after THA. 120 patients operated with unilateral primary THA were randomized to receive LIA or saline 0.9%. A multimodal oral analgesic regime consisting of slow release acetaminophen 2 g, celecoxib 400 mg and gabapentin 600 mg was instituted preoperatively. Rescue analgesic consisted of oral oxycodone. Pain scores were low for all pain assessments (walking, rest, and upon flexion of the hip) and did not differ between the LIA and the placebo group (p > 0.05). Consumption of rescue oxycodone did not differ between groups (p = 0.45). Intraoperative high-volume LIA with ropivacaine 0.2% provided no additional reduction in acute pain after THA when combined with a multimodal oral analgesic regime consisting of acetaminophen, celecoxib and gabapentin, and is therefore not recommended.
(IX) Why in hospital after fast-track hip and knee arthroplasty?
This prospective cohort study evaluated 207 consecutive, unselected patients (109 TKA and 98 THA) operated in a fast-track set-up where median LOS was 2 days for both groups and of which 95 % fulfilled functional discharge criteria ≤ 3 days. The clinical and logistical factors responsible for postoperative hospitalization showed that pain, dizziness and general weakness were the main reasons for being hospitalized at 24 and 48 hours postoperatively. Nausea, vomiting, confusion and sedation had minimal influence to delay discharge. Logistical challenges are mainly early upstart of physiotherapy (day of surgery) aiming at establishing ambulation and strengthening of muscles, and early transfusion of blood for patients needing this. It is concluded that future efforts to enhance recovery and reduce LOS after THA and TKA should focus on analgesia, orthostatic and muscle function.
| Abbreviations | ||
| ACCP | = | American College of Chest Physicians |
| ANORAK | = | Accelerated New Optimized Rationalized Arthroplasty Koncept (Concept) |
| AAOS | = | American Association of Orthopedic Surgeons |
| ASA-score | = | American Society of Anesthesiologists score |
| BSTKA | = | bilateral simultaneous total knee arthroplasty |
| BSTHA | = | bilateral simultaneous total hip arthroplasty |
| COX-2 inhibitor | = | cyclooxygenase inhibitor |
| CP | = | clinical pathway |
| DVT | = | deep venous thrombosis |
| LIA | = | local infiltration analgesia |
| LOS | = | length of stay |
| LMWH | = | low molecular weight heparin |
| NICE | = | National Institute for Health and Clinical Excellence (UK) |
| NSAID | = | non-steroidal anti-inflammatory drug |
| PACU | = | postoperative anaesthesia care unit |
| PE | = | pulmonal embolus |
| ROM | = | range of motion |
| RSA | = | roentgen stereophotogrammetric analysis |
| RTKA | = | revision total knee arthroplasty |
| THA | = | total hip arthroplasty |
| TKA | = | total knee arthroplasty |
| VTE | = | venous thromboembolic episodes |
1. Introduction
In 1983, clinical pathways (CP) were introduced in total hip and knee arthroplasty (THA and TKA) in the United States. CPs are algorithms or flowcharts containing all important factors regarding patient care from diagnosis over operation until the desired goals are achieved. The purpose of a CP is to standardize and optimize procedures to ensure an optimal and reproducible outcome regarding quality, efficiency and economic savings.
The reason for introducing CPs in USA was an economic incentive as a Diagnosis Related Grouping (DRG) system was introducedCitation1. This led to a decrease in the reimbursements for hospitals when performing THA and TKA and some even had budget deficits as the reimbursement covered less than the actual expenseCitation2, Citation3. These changes encouraged the development of CPs to lower costs and ensure a high, standardized quality of treatment and care. Focus would initially be primarily on the ability to save money to balance income and expenses.
Various orthopedic departments developed different variations of CPs focusing on both economic profitability and patient satisfaction; common features were a desire to: a) reduce costs by negotiating a reduced price with the manufacturers of prosthesesCitation4, Citation5; b) differentiate the activity-level of the patients resulting in choosing a cheaper prostheses for the low-activity old patient and a more expensive prosthesis aimed at the needs of the more active younger patientCitation4-8; c) reduce length of stay (LOS) by streamlining and rationalizing patient-flow from diagnosis till discharge – without compromising the clinical outcome or patient satisfactionCitation2, Citation5-7, Citation9. Some reduced LOS in hospital, but transferred patients to rehabilitation facilities outside hospital insteadCitation6.
In contrast to the more economic orientated and -driven approach, Professor Henrik Kehlet developed a fast-track conceptCitation10-12; a methodology focusing on optimization of clinical features in synergy with improved logistics allowing the patient to recover faster – and then secondarily resulting in a reduction of LOS as convalescence was shortened. Henrik Kehlet, having a background in surgical gastroenterology, focused initially on optimizing the hospital stays for patients undergoing abdominal surgery and hernia-repairs, but soon “fathered” fast-tracks across different surgical specialties but also anesthesiology and medical specialties. Research areas included surgical pathophysiology and many aspects of anesthesia and surgery in the broadest term in order to mediate and reduce the surgical stress response associated with all types of surgery. In 1992, a pilot study from Hvidovre Hospital on Danish THA patients was published and later followed by a cohort-study – indicating that a revision of pain treatment towards balanced multimodal analgesia, intensive mobilization and a critical revision of traditions could reduce convalescence and hospital stayCitation13, Citation14. This pioneering work led to many publications on different modalities to reduce the surgical stress response, reduce convalescence and improve patient outcome – and as early as 1994 the idea of “the pain- and risk-free operation” was bornCitation15.
While we still have not achieved a pain- and risk-free operation for all patients receiving THA or TKA, we are approaching step by step. Outcome measurements after fast-track surgery may include – apart from the above-mentioned LOS, patient satisfaction and economy – safety aspects in the form of morbidity/mortality, blood loss, and efficacy of pain treatment, time till first mobilization, swelling and strength of the operated limb among others. LOS should never be the key parameter – unless looked upon as an indicator of the clinical and logistical features making up the fast-track and following fixed, unaltered, functional discharge criteria (= the fulfilling the same functional milestones earlier). However, many questions remain unanswered and debated. What should an ideal fast-track set-up include? Can we predict LOS for certain patient characteristics? Which patients/operations should enter the fast-track? Is it safe – what kind and number of complications should be expected? How do we treat early post-operative pain best – allowing patients to mobilize early? And ultimately: why is the patient in hospital following THA or TKA – what is it we cannot control?
Attempting to answer these questions – by in-depth analyses of the clinical, organizational, and safety aspects of fast-track THA and TKA – has remained the driving force behind the studies making up this doctoral thesis. Many clinical features in the form of combinations of anesthesia, pain-reducing drugs and techniques, mobilization regimens and up-to-date care principles are being evaluated along with optimized logistics, patient education and – motivation, improved surgical techniques and prosthetic outcome. All efforts produce a synergistic result allowing us to replace potentially harmful traditions with evidence-based superior clinical features to give the patients the best possible treatment at any given time. This is what fast-track is aiming at: first doing it better, then doing it quicker – by improving all parts of the perioperative hospital stay and thereby addressing all parts of the convalescence: being the right track.
2. Clinical aspects
Fast-track surgery combines optimized clinical features with improved logistics. A variety of clinical aspects could and should be part of a fast-track set-up, including analgesia; DVT-prophylaxis; mobilization regimens and physiotherapy; and care principles (nursing). Selection of proper discharge criteria is imperative as these play a vital role as gate-keepers for discharge – which may also include traditions associated with all aspects of staying in hospital. Patient demographics and –related characteristics may influence LOS as some may predispose subgroups to staying longer for various reasons having difficulty fulfilling the discharge criteria within the expected time frame. Apart from clinical outcome and safety aspects following fast-track, patient satisfaction is a key parameter – although the patient may not fully understand the underlying principles for choosing the appropriate and best treatment modalities – the resulting satisfaction following discharge with the various parameters associated with the hospital stay is important and may influence the rehabilitation.
2.1 Analgesia
One of the key parameters of fast-track surgery is the implementation of an efficient and well-documented pain treatment regimen – as pain is detaining the patient in bed making early mobilization difficult. Updated information on evidence-based, procedure-specific pain treatment is found on www.postoppain.org, where the PROSPECT working group publishes its evidence-based recommendations. The recommended multimodal opioid-sparing pain treatment regimen is based on a synergistic effect of different pain treatment modalities including paracetamol, a COX-2 inhibitor, and opioids only as rescue medicine – weak or strong depending on pain intensity.
The multimodal opioid-sparing pain treatment used in most of the studies that comprise this thesis (I, II, IV–IX) consists of paracetamol (slow-release 2 g × 2), a COX-2 inhibitor (Celebra 200 mg x 2), gabapentin (300 mg + 600 mg) and opioid upon request (oxycodone (fast-acting) 5–10 mg/morphine 10 mg).
Whereas the use of paracetamol and COX-2 inhibitors – and the avoidance/minimal use of opioids – is well-documented, gabapentinoids are not recommended at the moment as insufficient data exist on its potential benefits in pain treatment following arthroplasty. Even though the most recent review concluded that gabapentin reduces pain and opioid requirements compared to placebo, the evidence compared with other post-operative regimens is not sufficientCitation16. A recent study on THA and gabapentin found no additional effect on pain or opioid consumption, but used only a single dose (600 mg) in conjunction with a multimodal regimen of acetaminophen, a COX-2 inhibitor and steroidsCitation17. The most recent study found an effect of combining gabapentin, dexamethasone and ketamine on pain (but not on opioid use), but this effect may be due to either the combination or a single drugCitation18. Nevertheless, the addition of gabapentin makes theoretical sense as a pain-reducing effect and an opioid-sparing effect may benefit multimodal pain treatment and thus facilitate mobilization – and also a sedative effect has been demonstrated which may be utilized by giving a dose before bed-time to facilitate sleepCitation19. Sleep disturbances are common following arthroplasty surgery and may lead to postoperative cognitive dysfunctionCitation20.
No randomized studies exist on pain reduction following multiple doses of gabapentin added to a multimodal opioid-sparing pain treatment regimen and the dose-response effect of gabapentin as part of a multimodal regimen in arthroplasty remains to be established.
Other modalities than oral analgesics for post-operative pain treatment include the local infiltration technique (LIA) with bandaging techniques and cooling, peripheral nerve blocks and the use of glucocorticoids.
The LIA technique, originally developed by Kerr and KohanCitation21 is also not (yet) recommended by the PROSPECT group. However, again, it makes good theoretical sense to block the nerve impulses at their origin and limit the pain stimuli from reaching the central nervous system. Dennis Kerr, being an Australian anesthetist, made a “recipe” on which ingredients to add in a cocktail attempting to keep the active drug localized, thus treating the wound like a snake-bite (ropivacaine 0.2%; adrenaline; ketorolac). Reporting on a cohort of 86 TKA, 54 THA and 185 hip resurfacings, excellent immediate pain relief was reported allowing early pain-free mobilization; no opioid use in > 65%; no side-effects regarding mobilization or potential (cardiac) toxicity nor infection – and allowing 71% of patients to reduce LOS to an overnight stayCitation21. No attempt was made by Kerr and Kohan to break down the technique in order to identify which component(s) contributed to the outcome. A number of studies have randomized the LIA technique versus placebo or other pain treatment modalities (PCA, femoral nerve block, epidural) but few have focused on evaluating the components/ingredients of the LIA technique ( and ) – which is in sheer contrast to its widespread use. Making comparisons and drawing conclusions from the few studies is made even more difficult as different “cocktails” are used (ingredients; concentration and volume hereof; addition of NSAID or not). One controversy is on the addition of NSAID to the mixture, most often as ketorolac (30 mg), as there is an ongoing debate as to whether local anti-inflammatory effects for NSAIDs are dominant in the periarticular tissues – or if it is better to give it systemicallyCitation22. The latter approach was chosen for our studies as it ensures an effect – and not potentially skewing outcomes for comparison between LIA (with local NSAID) and placebo (without local NSAID). Although cooling in conjunction with the LIA technique has not been specifically evaluated, a metaanalyses found no convincing effect of cryotherapy including no reduction of pain or swellingCitation23.
Table 1. RCT TKA with LIA. LIA+ = ropivacaine, adrenaline and ketorolac; LIA- = ropivacaine and adrenaline
Table 2. RCT THA with LIA. LIA+ = ropivacaine, adrenaline and ketorolac; LIA- = ropivacaine and adrenaline
LIA in TKA has been shown to be effective in the studies comparing it to placeboCitation24-27 with a reduction in pain for up to 48 hours, reduced opioid consumption for 24 hours, increased patient satisfaction, and better ROM (). However, one has to be careful regarding interpretation of what is causing these improvements in early convalescence as 3 of the 4 studies include NSAID in the mixture used for infiltration – as in the originally described “cocktail” by Kerr and Kohan. Only the study by Andersen et alCitation27 is evaluating the ropivacaine plus adrenaline mixture versus saline in a bilateral triple-blinded set-up, thus using the patient as his own control. One may argue that the LIA is “overflowing” to the other knee or has a systemic effect or the patient is unable to differentiate between the two painful knees, but this does not alter the highly significant difference in pain perception in favor of the LIA-side and – if anything – would minimize the difference between the knees. Also, infiltration into the subcutaneous tissues makes a differenceCitation28, whereas later injection through a catheter – multi-holed or epidural – in the subcutaneous tissues makes no difference as changing the volume/concentration is of no added benefit regarding pain reductionCitation28-30. Injection through a catheter has been found to reduce painCitation26, but in all the studies by Andersen et al. no clinically significant reduction in pain was seen regardless of placement of the catheter intraarticular, intracapsular or subcutaneouslyCitation27-33 and supported by other resultsCitation34.
Only a few randomized studies have compared the LIA technique against other modalities: 2 against continuous femoral nerve blockCitation35, Citation36 and 3 against epiduralCitation37-39. The studies are, however, of methodological limitations as the LIA technique remains to be more thoroughly investigated before comparing it to other modalities including what – despite an associated caveat on motor blockade leading to fall episodesCitation40 – remains the gold standard: the femoral nerve block.
The final element of the LIA technique is the application of a bandage (II). Bandaging techniques following TKA have not been investigated very much; actually there are only two studies – one on the effect on haemostasis (without LIA)Citation41 and one on the effect on pain in conjunction with LIA (II). The pressure necessary to produce tamponade of the knee joint is 52-62 mmHg, while the pressure on the skin from a properly placed compression bandage is around 30 mmHg – depending on the experience of the person applying it, the radius of the leg, the stiffness of the structures etc. Patients treated with the compression bandage had better ROM at discharge and fewer complications related to bleeding into the soft tissues compared to patients having a soft crepe bandageCitation41. A prospective, randomized study on the role of bandaging to prolong analgesia was performed in 48 patients undergoing fast-track TKA including LIA (II). The assumption was that the bandage would improve analgesia by reducing absorption of the local analgesics and also by reducing joint and limb swelling. Patients were randomized to receive a compression or a non-compression bandage with the assessment of pain for 24 h postoperatively. Pain at rest, during flexion, and during straight leg lift was lower for the first 8 h in patients with compression bandage than in those with non-compression bandage and with a similar low use of opioids (around 11 mg/24 hours) and mean LOS (3.0 days). Thus, a compression bandage is recommended to improve analgesia after LIA in total knee arthroplasty – but it is not deductible from the study which assumed mechanism resulted in less pain. Less swelling of the limb and less haemarthrosis was also noted in the study by Charalambides et al.Citation41 and this may reduce pain but also favor early mobilization as an association between swelling of the knee and the periarticular tissues exist.
LIA in THA has in the published studies different outcomes – spanning from a reduction in painCitation42-44, opioid consumptionCitation42-44 and LOSCitation42 to no additional effect when used in conjunction with a multimodal opioid-sparing pain treatment regimen (). Two studies from our group both found no effect on pain reduction of LIA in THA (VIII, Andersen et al., in press 2011). The reason is not a lack of analgesic effect when used in the periarticular tissues surrounding the hip, but rather a result of one of the following or a combination hereof: a) relatively low pain scores associated with THA, where median pain scores are at all times <3 and <5 upon rest and mobilization, respectivelyCitation32; b) good and sufficient effect on pain by an oral multimodal pain treatment regimen; c) different structures/perfusion around the hip compared to the knee; and/or d) less effect of cooling due to more tissue interposed.
The studies showing an effect of LIA in THA have not used as potent an oral multi-modal regimen as the one used in our negative studies (VIII, Andersen et al., in press 2011) or are potentially flawed by the addition of NSAIDs or glucocorticoids to the mixture given to the LIA-group but not to the control-group as explained above; thus – instead of measuring the effect of the local analgesic only – potentially measuring the well-known effect of NSAID or glucocorticoid on both pain and opioid consumptionCitation45-48.
In a two-center study, the largest published study on the potential effect of LIA on pain following THA, no additional effect was found (VIII). In this prospective randomized, double-blind, placebo-controlled study, it was evaluated whether high-volume LIA – in addition to a multimodal oral analgesic regime – would further reduce acute postoperative pain after THA. 120 patients were operated with unilateral primary THA and were randomized to receive LIA or saline 0.9%. The above described multimodal oral analgesic regimen consisting of paracetamol, celecoxib and gabapentin was instituted preoperatively. Pain scores were low (< 20, VAS 0–100) for all pain assessments (walking, rest, and upon flexion of the hip) and did not differ between the LIA and the placebo group (p > 0.05). Consumption of rescue oxycodone also did not differ between groups (p = 0.45). Intraoperative high-volume LIA with ropivacaine 0.2% provided no additional reduction in acute pain after THA when combined with a multimodal oral analgesic regimen consisting of paracetamol, celecoxib and gabapentin, and is therefore not recommended. The potential pain-reducing effect of an intra-articular catheter topped up with ropivacaine has not been evaluated in this study, but is highly unlikely to have any effect on reducing pain – as a) no effect was seen with a much higher dose at infiltration; b) no effect has been shown in most studies on intra-articular infusion of opioids or local analgesics in total knee arthroplastyCitation49; and c) a randomized study found no effect on pain, opioid consumption or LOS of injections of ropivacaine into a catheter versus placebo following 60 consecutive THAsCitation34. Thus, in conclusion, LIA does not seem to produce any additional effect on pain, opioid consumption or LOS – when a multimodal opioid-sparing analgesia regimen is used consisting of paracetamol, a COX-2 inhibitor and gabapentin.
Another potential modality to include in a multimodal regimen is glucocorticoids. These inhibitors of the inflammatory response may be applied locally or systemically and their effect on pain – among other positive effects – has been documented in other specialtiesCitation46, but also in orthopaedicsCitation50. In THA, a study found a reduction in pain upon mobilisation from a single dose of glucocorticoidCitation45 without any adverse effects at follow-up after 6 weeks and 1 yearCitation51. In TKA, a randomized double-blind placebo-controlled study on 48 patients receiving a single dose of glucocorticoid or saline found the first group of patients to have less pain for 48 hours and less opioid consumption – among other beneficiary outcomesCitation47. Further dose-response studies as well as safety studies are needed before general recommendations can be made.
Even with multimodal opioid-sparing pain treatment in combination with LIA, pain may still be a problem upon discharge and on short-term follow-up. A study on subacute pain following fast-track THA and TKA found pain to be a minor problem at rest and upon mobilization in THA patients 30 days after surgery, whereas 52% of TKA patients suffered from moderate pain and 16% had severe painCitation32.
Whether the amount and intensity of early pain may predispose to the development of chronic pain is debated – and currently unanswered for THA and TKA. In a nationwide study, chronic pain (12-18 months postoperatively) following THA was found in 28.1% of patients with moderate to severe intensity in 12.1%Citation52 but incidences may be even higher, i.e. 37.5%Citation53. Even though the transition from acute pain to chronic pain has been predicted by the intensity of early pain in several other studies, conflicting data exist following arthroplasty. In a study on pain following TKA, it was found that the degree of pain experienced in the days following surgery was unrelated to the type of knee arthroplasty (primary, bilateral, revision – indicating that pain treatment should not differ between these groups) but was associated with the development of chronic pain – as patients experiencing moderate to intolerable pain had 3-10 times greater risk of developing persistent pain compared to patients sensing only mild painCitation54. A study on pain following THA found no association between early postoperative pain intensity and pain after 6 monthsCitation53 – but as acute pain upon mobilization was found to be mild to moderate (< 4/VAS10) – as it was also found in a study on subacute painCitation32, this may explain the lack of association and be contributed to the multi-modal pain treatment regimen. The theory of increased pain responsiveness and central sensitization following major surgery is questionable. A study evaluating subjective pain and brain responses before and after TKA found responses in primary and secondary somatosensory cortex for stimulation of the operated leg to be significantly smaller after surgery – arguing against the development of an overall increased pain responsiveness after a major surgical traumaCitation55. However, preoperative function of the nociceptive system may be important to predict the risk of acute and persistent pain – as shown in inguinal herniatomyCitation56, Citation57.
In conclusion, a multimodal opioid-sparing analgesia regimen consisting of paracetamol, a COX-2 inhibitor and gabapentin with opioids as rescue medication only is supported by several studies. Whereas LIA has been demonstrated to be highly effective in TKA no additional effect was seen in THA. No clinical relevant effect of supplementary injections in a catheter has been demonstrated whereas a compression bandage augments the LIA in TKA. Glucocorticoids may be added to the regimen but dose-response and safety studies are needed before general recommendations can be made.
2.2 DVT prophylaxis
Fast-track surgery aims at shortening convalescence by optimizing the clinical features as to facilitate the complication-free recovery of the patients, i.e. reduce incidences of DVT and PE. Patients operated with THA or TKA are at risk of thromboembolic complications – regardless of application of fast-track or more conventional care. Whether that risk is high, intermediate or low is multi-factorial and may depend on genetic predispositionCitation58, presence of varicose veinsCitation59, type of anaesthesiaCitation60, fluid therapy during surgeryCitation61, duration of immobilizationCitation62, etc. Incidences hereof vary as does the studied population, prophylaxis, logistical and clinical set-up and also follow-up – making comparisons and even metaanalyses difficult and debatableCitation63, Citation64. Some surgeons estimate patients to be at high risk following THA and TKACitation65 while – with modern surgical treatment – THA and TKA are found to be low-risk procedures by othersCitation66.
The guidelines from ACCP outline which prophylactic agents (both pharmacological and mechanical) – and the duration hereof – are recommended for prophylaxis. For TKA at least 10 days of prophylaxis is recommended (preferably longer and up to 35 days) and for THA at least 35 days – using either LMWH, fondaparinux or a vitamin K antagonist (and mechanical prophylaxis for patients at high risk of bleeding)Citation67. These guidelines are at least partly based on older studies where LOS was 7–12 days, where a large fraction of patients were transferred to rehabilitation facilities and where (asymptomatic) DVT was accepted as a (surrogate) endpoint – and thus they are also debatableCitation65, Citation68-70. Especially the assumption that the occurrence of DVT will reflect the proportion of patients suffering from PE has led some orthopedic surgeons to abandon the more rigoristic ACCP guidelines in favor of more differentiated prophylaxis based on risk stratification. Fuelling this argument, a recent study on the potential association between DVT and PE demonstrated only 1.7% of patients to have both and not more frequent than having either and concluded that “the high association between DVT and PE that is assumed to exist does not seem to hold true for orthopedic surgery patients”Citation71. This has led to a recent development of other guidelines (AAOS and NICE) – and an ongoing debate on which pharmacological agents to use for which patients and for how longCitation65, Citation68-70, Citation72. Two interesting studies to be included in this debate are the studies by Kim et al. on Korean patients operated with THA (n=300) and TKA (n=343): no prophylaxis was given, more than 1/3 developed DVT, no treatment was given and all patients were followed with venograms and perfusion scans for 6 months: all DVT resolved, no PE developed and no deaths occurredCitation73, Citation74. Although this natural course may not turn out as favorably for all patients with different genes, different treatment algorithms etc., it does show one end of the spectrumCitation73, Citation74 – compared to the other where 40-85% of patients develop DVTCitation72.
One factor believed to be strongly associated with the development of DVT is immobilization, as it represents one of the cornerstones of the pathophysiology behind DVT (injury-induced hypercoagulability, endothelial injury, reduced blood flow, and immobilization)Citation75. Although no randomized controlled studies comparing timing (and amount) of mobilization with bed rest exist, suggestions of the beneficent effect of early mobilization on reducing DVT do existCitation60, Citation62, Citation76.
Based on this, a study (V) was undertaken to evaluate the impact of early mobilization combined with only short-duration pharmacological thromboprophylaxis and short hospitalization on the incidence of death, PE and DVT. 1,977 consecutive, unselected patients were operated with primary THA, TKA, or BSTKA in a well-described standardized fast-track set-up during 5 years. Patients received DVT prophylaxis with low-molecular-weight heparin (enoxaparin 40 mg) starting 6–8 h after surgery until discharge only. All re-admissions and deaths within 30 and 90 days were analyzed using the national health register, concentrating especially on clinical DVT (confirmed by ultrasound and elevated D-dimer), PE, or sudden death. Numbers were correlated to days of prophylaxis (LOS). Mean LOS decreased from 7.3 days to 3.1 days. 3 deaths (0.15%) were associated with clotting episodes and overall, 11 clinical DVTs (0.56%) and 6 PEs (0.30%) were found. The vast majority of events took place within 30 days; only 1 death and 2 DVTs occurred between 30 and 90 days. During the last 2 years (854 patients), when patients were mobilized within 4 h postoperatively and the duration of DVT prophylaxis was shortest (1–4 days), the mortality was 0% and no DVT or PE were found following BSTKA. These figures compare favorably with published regimens with extended prophylaxis (up to 36 days) and hospitalization up to 11 daysCitation64, Citation66, Citation77-85 and question the need of extended thromboprophylaxis, when patients are mobilized early. The majority of studies on extended prophylaxis with newer drugs are at least partly sponsored by the pharmaceutical companies producing these agents; LOS is long or not accounted for; timing and amount of mobilization is not registered; multiple departments with varying procedures are included etc. which may make interpretation difficult. Also, adding power to the findings of (V) is the inclusion of unselected, consecutive patients as opposed to the majority of the studies on extended prophylaxis where patients were highly selected excluding up to 25% of patients at high risk of developing thromboembolic episodes. Explanations for these favorable results may – apart from the early mobilization – also include other factors such as choice of fluid therapy during surgery as an earlier studyCitation61 on our patients found a liberal amount of fluid during surgery (median 4250 mL) to result in improved pulmonary function 6 h postoperatively, a reduced incidence of vomiting but also hypercoagulability 24–48 h postoperatively compared to a restrictive fluid plan (median 1740 mL).
For that reason, a standardized intraoperative fluid plan consisting of an intermediate volume has been chosen ever since, consisting of 0.9% saline (5 ml/kg/h) and colloid (Voluven; 7.5 ml/kg/h).
All patients in (V) received 1 g of tranexamic acid intraoperatively for hemostatic purposes as it has been shown to reduce blood lossCitation86, Citation87 and although some may fear an increased risk of DVT following such a regime – on top of the short time of prophylaxis – the results from this study on unselected, consecutive patients with 100% follow-up do not sustain this fear. Also, as none of the patients in (V) with a DVT developed PE within 90 days and also only 6/50 patients with PE had confirmed DVT in another studyCitation88, the findings do not support DVT as a valid surrogate parameter for development of PE (as supposed by ACCP) but rather to evaluate only the number of PE and death (as supposed by AAOS). As rebound hypercoagulabilityCitation89 (around 2% of patients discontinuing pharmacological prophylaxis are at risk of getting a DVT) seems to play only a minor – if any – role with short-term prophylaxis as in (V), a relevant question would be if the outcome regarding incident cases would be different if no prophylaxis was given with the early mobilization? The study (V) did not register bleeding episodes and although the newer studies report no increase in these episodes, some surgeons believe these to be underreported and are thus afraid to trade-off (unnecessary) DVT-prophylaxis for patients at low risk instead of an increased number of potentially devastating bleeding episodesCitation69, Citation90. Early mobilization may be one way to reduce the risk of DVT – regardless of type or length of prophylaxis. Large randomized studies or large prospective cohort studies are warranted.
Thus, in conclusion, patients operated with THA and TKA are at risk of thromboembolic complications but the size of this risk and the subsequent needed prophylaxis is debatable – and may depend on a number of factors including timing and amount of postoperative mobilization. Different guidelines have been developed but are based on older studies with treatment algorithms different from the fast-track methodology, where a prospective cohort study found low incidences of DVT, PE and death. Differentiated prophylaxis based on individual risk assessment including timing of mobilization and balancing the risk of bleeding may be optimal.
2.3 Mobilization
Another key prerequisite in fast-track is early mobilization. This requires the pain treatment to be effective, the patient to be motivated and the staff to be available – apart of course from surgery allowing immediate mobilization. The latter is well-investigated also in uncemented THA, where bone mineral density and serial RSA up to 5 years found full-weight bearing to be safeCitation91 – although also caution during stair climbing due to torsional forces for the first few weeks following surgery has been recommendedCitation92.
A nationwide survey in Denmark found a multitude of different physiotherapy regimens instituted after operations with THA and TKACitation93, all focusing on strengthening of the muscles, reduction of swelling, gaining ROM and restoration of a normalized gait pattern. Physiotherapy is thus heterogeneous and varies between studies, but meta-analyses evaluating the effect hereof have been disappointing as it is concluded that” insufficient evidence exists to establish the effectiveness of physiotherapy exercise following THA for osteoarthritis”Citation94 and also that “interventions … after discharge result in short term benefit after TKA”Citation95. Effect sizes were small to moderate regarding ROM and quality of life at 3–4 months, with no long term benefitCitation95. Also, doubling the amount of physiotherapy during hospitalization following TKA made no difference regarding (lack of) outcome on ROMCitation96.
Is it possible to pre-rehabilitate patients prior to operations with THA or TKA in order to facilitate their recovery? According to a review and a randomized study the answer is negativeCitation97, Citation98.
However, early mobilization has been associated with a reduction in complications – as bed rest has been shown to promote complicationsCitation99, Citation100. Patients lying in bed have a reduced oxygen saturation compared to sitting and standing thus potentially leading to prolonged tissue healing and pneumonia; patients are losing muscle and are at increased risk of thromboembolic episodesCitation60, Citation62, Citation76, pressure ulcers, etc.
For that reason, CPM – keeping the patients in bed for prolonged periods of time instead of mobilizing out of bed – has limited place in modern postoperative treatment of TKA patients. Although shown to produce a significant increase in both active and passive ROM of 3 and 2 degrees, respectively, this is of no clinical relevance and the difference has disappeared at 6 weeks and 3 months follow-upCitation101, Citation102. However, as there is weak evidence for a reduction in the number of manipulations, a small subgroup (unknown) of patients may benefit from its useCitation102.
Regaining muscle strength early is imperative to obtain a normal gait pattern. The quadriceps muscles often are weakened due to less use following progression of arthritis prior to the operation and are subsequently even more impaired due to the surgery. Muscle weakness may be due to decreased voluntary muscle function, muscle atrophy and pain from the jointCitation103. Progressive resistive strengthening exercises and neuromuscular electrical stimulation, possibly along with “pre-habilitation,” may improve quadriceps volitional force outputCitation103. It has been demonstrated that the decreased quadriceps muscle function is in the area of about 60-80 % after TKA and about 30-40 % after THACitation104, which may call for early physiotherapy including strengthening exercises and/or reduction of inhibitory neural reflexes (by electrical stimulation)Citation105-107. Also, other muscles may play a role in normalizing the gait pattern. Some focus has been on the hip abductors as studies have shown these muscles to be involved in walking, rising from a chair and stair climbing, and to be weakened to a degree where they impair the gait patternCitation108, Citation109.
Provided patients are receiving multimodal opioid-sparing analgesia, pain per se has a limited influence on early functional recovery beyond the first postoperative day after TKA. A study found 90% of patients were able to walk independently on the first postoperative day with pain ≤VAS 5 and on day 2 with pain ≤ VAS 4Citation106. Also, in THA, a study found no relation between pain intensity and independence level in functional activities on the second and sixth postoperative daysCitation110.
The lack of negative influence of pain on early functional recovery combined with the finding of impaired muscle function allows and warrants physiotherapy to be initiated very early – with protocols focusing on muscle strengthening exercises.
An analysis of reasons for staying in hospital up to 72 hours after surgery found that more than 40% of patients could fulfill all 6 functional discharge criteria in the afternoon on the day of the operation (IX). The main problems were taking care of personal care and walking 70 meters with crutches, the latter indicating the need for instant access to physiotherapy in order to regain a more normal gait pattern, but also to address pain and muscle weakness as main reasons for not fulfilling the discharge criteria (IX).
Thus, even though physiotherapy so far has failed to show a significant beneficent influence on functional outcome, it is part of most fast-track protocols. An improved understanding of which muscles to address and the best way to do it is emerging and specified physiotherapy may soon be part of an evidence-based regimen. For the moment being, it represents a valued effort to mobilize the patients correctly, teaching them an appropriate way to ambulate either with or without gait aids, ensuring progress in ROM - and a helpful tool in achieving functional discharge criteria.
In conclusion, conventional physiotherapy following THA and TKA is heterogeneous and has limited effect on outcome. Future studies should focus on early postoperative strengthening therapy and to define indications for physiotherapy in specific patient groups.
2.4 Discharge criteria
The goal for patients and staff alike is the fulfillment of discharge criteria allowing the patient a safe discharge. Many different discharge criteria are used for THA and TKA patients, some may be due to traditions or more practical circumstances rooted in the local community (i.e. the possibility for additional help at home and home-based nurses if needed). Either way, it is necessary to have fixed discharge criteria – known to both patients and staff – in order for both parties to know when discharge should take place and also to allow for comparison within the department, within the region or within the country.
Fast-track surgery should have functional discharge criteria. These functional discharge criteria should reflect the situations the patient has to master at home in order to avoid readmissions for not being able to cope at home. Fast-track surgery can be either value-based or time-based. In value-based fast-track set-ups, daily goals have to be fulfilled in order for the patient to progress to the next step, i.e. a specific ROM, time out of bed or distance to ambulate. In time-based fast-tracks, an intended LOS is set without any daily goals. The advantage to have a value-based fast-track is in the successive progression ensured by the daily goals, whereas the strength of the time-based set-up lies in the possibility to plan the bed occupancy in advance and to allow for differences between patients as some get off to a good start whereas others start off slowly and then speed up. Ideally, these could be combined as LOS is down to a few days for the majority of patients, which the patient and staff should be informed of. The inclusion of functional discharge criteria as the only goal to fulfill makes good sense – as some patients will do so within 24 hours.
The discharge criteria used in the studies (I, II, IV, V, VI, VII, VIII, IX) are strictly functional – with the addition of patients need having pain controlled by oral medication only, a VAS<5 and accept discharge. The functionality is: ability to take care of personal care, get in and out of bed, into and up from a chair, on and off a toilet and to walk with proper walking aids 70 m (the length of our hall way)Citation111(I). Minor variations of functional discharge criteria exist without profound impact on LOSCitation112, Citation113, and it has been found in a nationwide study that functional discharge criteria were present in the 3 departments with the shortest LOS (III). Other departments also have added flexion criteria for TKA (>90 degrees to allow discharge). The latter is not evidence-based as no study exists finding a minimum flexion of 90 degrees to ensure a good outcome. One study has, however, found that flexion of at least 60 degrees results in no extra health service useCitation114 whereas another study found patients with a ROM of 69 degrees to need more manipulations than patients with a ROM of 81 degreesCitation115 at discharge.
Fulfillment of discharge criteria is traditionally evaluated at surgeon rounds in the morning. With the fast-track methodology, progress in the form of earlier fulfillment of the functional milestones (i.e. the functional discharge criteria) may warrant some form of evaluation sooner than the following morning – as patients may not fulfill discharge criteria in the morning but do so following physiotherapy later that day. As discharge criteria are known by both patients and nursing staff, the latter could evaluate fulfillment and discharge the patient in the afternoon or early evening. Such an approach has been used in (IX), where fulfillment of every functional discharge criteria was evaluated twice daily by the nursing staff: at 9 a.m. and at 2 p.m. Also, reasons for not fulfilling the discharge criteria – whether clinical or organizational – were registered. This approach resulted in many patients being discharged earlier than they would have been if only discharge were to take place in the morning – thus reducing unnecessary lengthy stay after fulfillment of the discharge criteria (IX). This prospective cohort study evaluated 207 consecutive, unselected patients (109 TKA and 98 THA) operated in a fast-track set-up where median LOS was 2 days for both groups and of which 95 % fulfilled functional discharge criteria ≤ 3 days. The clinical and logistical factors responsible for postoperative hospitalization showed that pain, dizziness and general weakness were the main reasons for being hospitalized at 24 and 48 hours postoperatively. Nausea, vomiting, confusion and sedation had minimal influence to delay discharge. Logistical challenges are mainly early upstart of physiotherapy (day of surgery) aiming at establishing ambulation and strengthening of muscles, and early transfusion of blood for patients needing this. It is concluded that future efforts to enhance recovery and reduce LOS after THA and TKA should focus on analgesia, orthostatic and muscle function.
This is the first study to go into detail as to why the patient is hospitalized following THA or TKA (IX), although a few other studies have touched upon the subject finding “medical reasons, surgical reasons and social reasons” responsible for delaying discharge after the intended 5 daysCitation116. These findings re-emphasize the importance of looking at fast-track as a dynamic process constantly focusing at improving both clinical and organizational features. Fast-track is not a fixed entity of processes, but should include the newest evidence-based clinical enhancements; ANORAK-HH is an example of such a dynamic, evolving fast-track.
In conclusion, fulfillment of functional discharge criteria is a prerequisite for discharge ensuring the patients capability to cope at home. Underlying reasons for not fulfilling these include both clinical and organizational factors to be addressed with a focus on analgesia, orthostatic and muscle function and early physiotherapy and blood transfusion (if needed).
2.5 Care principles
A fast-track was developed and implemented in September 2003, based on previous studies showing improved outcomes following revisions in pain treatment, mobilization and traditionsCitation13, Citation14. It was called ANORAK-HH (Accelerated New Optimized Rationalized Arthroplasty Koncept (concept) – Hvidovre Hospital) and was designed to include all patients admitted for surgery with THA or TKA including bilaterals and revisions (I). The intentions included a continued high quality of treatment, nursing and training; patients should experience as little pain as possible after operation; gain quick ambulation and recovery; a high patient-satisfaction and no (few) complications/readmissions. Treatment, care and mobilization should consist of evidence-based interventions combined in a multi-disciplinary set-up including an optimized multi-modal pain treatment, efficient and focused nursing and early mobilization. The basic idea was to first do it better, then quicker and a reduction in LOS would only be relevant provided the patient`s outcome was unaltered or increased regarding the surgery performed and satisfaction with the stay, without increasing complications or readmissions and unaltered discharge criteria were met (sooner).
From the beginning, ANORAK was a more time-based fast-track with an intended maximum LOS of 5 days and later it shifted towards a combination of time-based and value-based fast-track; i.e. both an intended maximum LOS (lowered to 3 days and now 1-2 days) and the only value being fulfillment of the functional discharge criteria. The philosophy has remained simple: information on intended max. LOS; information provided at a multi-disciplinary pre-admission patient-clinic; the patient motivated to be an active participant; establishing a specialized ward with a dedicated specialized staff; and finally standardization and rationalization of all procedures. The tasks performed by the nurses have shifted from more traditional nursing towards more interactive participation with the patient and tasks now include information and motivation of the patients, first mobilization of the patients following surgery, evaluation of fulfillment of discharge criteria and subsequent discharging the patient, etc.
To ensure standardization and rationalization, a detailed description of all procedures performed by nurses and assistants, physiotherapists, surgeons etc. has been completed in a set of care principles, which are updated regularly to include changes in the clinical (evidence-based) and logistical (practical) set-up. The fast-track protocol described in (I) has thus changed from then till now regarding: information on intended maximum LOS (from 5 to now 1-2 days); use of regional anaesthesia in the form of spinal only to all patients regardless of procedure (earlier combined with epidural to TKA); pain treatment (a broader multimodal pain-treatment protocol is now in use including LIA); use of bladder catheter is now abandoned. Optimization of logistical features include preoperative training with crutches, short stays in the PACU, radiographs to be taken when leaving the PACU before arriving in the ward, and evaluation of discharge criteria twice daily. Along with the changes in care-principles, LOS has been reduced in increments (I, II, IV, V, VIII, IX) from 3.8 days to now about 2 daysCitation28, Citation29, Citation31-33, Citation47, Citation104, Citation106, Citation107, Citation111, Citation112, Citation117-126. The most recent used care principles from ANORAK-HH are summarized in .
Table 3. Care principles, patient-realted characteristics and satisfaction parameters of ANORAK-HH
Parameters, which have been continuously monitored from the beginning, include LOS, readmissions, patient satisfaction and as a secondary parameter: the economy – these are coherent with the ones most frequently assessed in previous studiesCitation127 (apart from number of patients being discharged to home, which in Denmark approaches 100%). The first 3 parameters are easy to measure and ensure a patient-based assurance of quality and allows for prompt interception should one of the parameters indicate a negative change. One example hereof was the detection of an increase in readmissions due to suspicion of infection and DVT, which was not found. However, as this cause for readmission turned out to be the number 1 reason for readmission – and made up for half of the total number of readmissions following THA and TKA (IV) – the decision was made to establish an additional out-patient clinic manned by nursing staff offering the patients removal of clamps/sutures and the opportunity to have an expert opinion on the wound/affected leg – if necessary by a surgeon as well.
Another aspect of ANORAK is the high degree of continuity – both from a patient point of view as from a staff point of view. The majority of tasks are placed at the arthroplasty ward, where out-patient clinics are situated (surgeon and nurse: both referrals and postoperative), all paperwork is completed here, and the multidisciplinary patient-clinic takes place here – all involving the same surgical and nursing staff. This is believed to result in a high degree of satisfaction from both patients and staff – and to reduce anxiety by the first.
Other fast-track set-ups exist, but detailed description of the contents is relatively rareCitation112, Citation116, Citation128-130. As the most recent Cochrane review on “Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy” (2008)Citation131 could only identify 5 randomized controlled studies on fast-track versus traditional care, it seems paramount to describe the fast-track set-up in detail in order to allow for comparison.
ANORAK is the formalized attempt to describe the combined, standardized optimization of organizational aspects applicable, available and possible at Hvidovre Hospital with evidence-based optimized clinical features (). The registration of outcome parameters allows for evaluation of which of the registered variables make a difference, including patient-related characteristics.
Thus, in conclusion, care principles detailing procedures are essential to ensure continuation, standardization and rationalization of both clinical and organizational aspects and are fundamental for the outcomes regarding LOS, satisfaction, readmissions and economy.
2.6 Patient-related characteristics
Many factors may influence LOS: some are clinical, some organizational, with traditions potentially affecting both – and then there are patient characteristics: traits and factors associated with each individual. The set-up of the individual fast-track will of course determine whether or not these characteristics come into play – if the fast-track was to plan with a LOS of, say, 10 days, virtually every single patient would be able to achieve this, and looking at patient characteristics would be obsolete.
In the ANORAK-HH fast-track set-up (I), 712 consecutive, unselected patients operated with primary, unilateral THA and TKA had patient characteristics and perioperative parameters registered and correlated to LOS and patient satisfaction. 92% of the patients were discharged to their homes within 5 days, and 41% were discharged within 3 days. A number of patient characteristics were found to influence postoperative outcome regarding LOS by multivariate backwards logistic regression analyses: Age: for each year of age, the probability of staying longer than 3 days increased by 2.4%; Sex: women had around 40% greater probability of staying more than 3 days compared to men; Living situation: patients living alone had 25% greater probability of staying more than 3 days than those who lived with a spouse; Preoperative use of walking aids: patients with had 40% greater probability of staying longer than 3 days; Weekday of surgery: patients operated at the end of the week had greater risk of staying longer than 3 days; ASA-score: patients with a score of 1 and 2 had 60% and 20%, respectively, probability of staying less than 3 days compared to ASA 3; Blood transfusion: patients requiring blood transfusions had 340% probability of staying longer than 3 days compared to those without. Bivariate (but not multivariate) analyses also found pre- and postoperative hemoglobin levels (Spearman) and time from surgery till first mobilization (Mann-Whitney) to be associated with LOS. Other studies have also found associations between ageCitation116, Citation132-135; female sexCitation134-136; living situationCitation134, Citation137; co-morbiditiesCitation133-135, Citation138 and LOS, whereas it was a tie regarding ASA-scoreCitation116, Citation138 and LOS, as in (I). Living situation may reflect a more complex underlying mechanism as a study found patients living alone to be older, with greater co-morbidity and more joint pain and dysfunction before surgery and at 3 months and 1 year after surgery – predicting a poorer outcomeCitation139. Differences in muscular strength and gait-pattern between patients with and without walking aids may explain the association with longer LOS for the first group of patientsCitation133, Citation138.
The implications of identifying patient characteristics influencing LOS in a fast-track set up with a mean LOS of 3.8 days are obvious and triple: a) it allows for identifying subgroups of patients who need special attention in order to achieve equally well as the majority of patients; b) it allows for addressing and improving clinical situations to alleviate the impact of the characteristic (i.e. weekday of surgery, blood transfusions, and early mobilization); and c) it allows for optimized planning of bed occupancy/patient flow.
These findings demonstrate the importance of registering data in order to be able to act (Plan-Do-Study-Act, the Deming circle)Citation140. As age, sex, living situation and preoperative use of walking aids are all given, they cannot be addressed. However, co-morbidities (which may influence ASA) can be optimized preoperatively; weekday of surgery can be placed at the beginning of the week (especially for the older patients, whose advanced age may increase LOS); blood loss leading to blood transfusions can be minimized (Tranexamic acidCitation86, Citation87, fibrin sealants, bipolar sealers, etc. etc.); and patients can be motivated for early mobilization (facilitated by clinical enhancements in pain treatment).
Patient-related characteristics may also on a larger scale – and not within the fast-track methodology – influence outcome. A study on 222,684 patients operated with TKA found predictors for complications to include (among others) age, gender, race/ethnicity, a co-morbidity index, and insurance type and could predict morbidity and mortality rates depending on the combination of these factorsCitation141. Correspondingly, a similar study on 138,399 THA patients identified a co-morbidity score, diabetes, rheumatoid arthritis, advanced age, male gender, and black race to increase risk of complicationsCitation142. A study on preoperative pain, co-morbidities and late postoperative pain following TKA demonstrated the number of co-morbidities to predict the presence of pain at 2 years follow-upCitation143. Also, the study found (catastrophic) preoperative pain scores to predict chronic postoperative pain. These findings highlight the importance of identifying subgroups of patients needing special attention. A review, nevertheless, concluded that despite identification of patient-related characteristics influencing outcome negatively, all subgroups benefitted from total joint arthroplasty and no restrictions as to accessing operations should be based on these patient characteristicsCitation144.
It is thus evident, that a specific LOS predisposes specific patient-related characteristics to influence outcomes (and vice versa) and that longer LOS may diminish/remove this influence – and for that reason patient-characteristics are more or less specific for the various fast-tracks, depending on the clinical and logistical set-up including traditions.
In conclusion, patient-related characteristics may affect both LOS and satisfaction but also morbidity and mortality, thus calling for identification of and addressing subgroups of patients needing special attention in order to improve their outcome.
2.7 Traditions
Undocumented traditions in perioperative care after THA and TKA are often passed on as gold standard. Traditions may have a powerful influence on outcome as they may be good, neutral and harmful; influencing pain, infection, blood loss, mobilization, LOS, thromboembolic prophylaxis, and cost. However, evidence-based medicine in the form of fast-track, offering the best available documented treatment, may interfere with (harmful) traditions. It is therefore essential to re-visit traditions or routines once in a while and re-evaluate current practice according to existing evidenceCitation145. An example of a potentially good tradition (because evidence, however scarce, supports it) is the use of a separate skin knife as a study found a 90% potential reduction in contamination of the deeper layers by changing the bladeCitation146.
Some of the more common traditions include the following, which all have limited or no evidence or may even be deleterious: a) preoperative hair removal to reduce postoperative infection rate is found to have no effect and hair removal with a razor to produce more infections than clipping or depilatory creamCitation147; b) plastic adhesive drapes (with or without Iodine) does not reduce infection rates, on the contrary, as more patients in the adhesive drape group developed a surgical site infectionCitation148; c) drains increase the blood loss and transfusions with no impact on infection, hematoma or reoperationsCitation149; d) bladder catheter routinely is not recommended as it could cause unnecessary problems in 68% of patientsCitation150; e) compression stockings do not give supplementary prophylaxis regarding PE or death when pharmacological prophylaxis is already instituted but may reduce DVTCitation67; f) CPM only improves ROM with 3 degrees which is clinically irreleventCitation102; g) discharge criteria following TKA do not need to include flexion > 90 degrees as 6o degrees has been demonstrated not to cause extra health service useCitation114; h) minimally invasive surgery (MIS) – although barely a tradition yet – is demonstrated to give better early ROM and functional recovery after TKA initially and no effect on THA with more wound healing problems and infections for the first and more lesions to the lateral femoral cutaneous nerve for the lastCitation151-153; and i) tourniquet in TKA does not reduce total blood loss and may cause swelling and impair early functional recoveryCitation154, Citation155 and does not reduce the number of lateral releases if applied with the knee flexedCitation156. As tourniquet pain is realized as pain different from knee pain, especially following introduction of the LIA technique most often resulting in very little or no pain from the knee itself, great interest is in reducing this sometimes excruciating pain. One simple method is to reduce the cuff pressure as 100 mm Hg above the systolic pressure is sufficient for a blood less surgical field and has been demonstrated to result in less pain for 3 days compared to a cuff pressure of 350 mm HgCitation157. Another method is to give an NSAID prior to inflation of the tourniquet as a study has shown this to reduce the prostaglandin production locally resulting in less pain and less opioid consumption for 4 hoursCitation158. Administration of a COX2-inhibitor prior to operation has been demonstrated not to interfere with prosthetic ingrowth as measured with RSA at 2 years follow-upCitation159 and has also shown a 30% reduction in pain scores for 4 weeks, lower opioid consumption, better ROM at day 1–3 and at 1 month, and identical blood loss and functional outcomeCitation160. These findings support the use of a multimodal pain treatment regimen including a COX2-inhibitor initiated before surgery. This regimen is not to be confused with pre-emptive analgesia, in which one attempts to modulate the postoperative response to pain by a preoperative administration of drugs intended to affect the central nervous system. Unfortunately, pre-emptive analgesia has not been documented to take place, regardless of drug usedCitation161. Other methods to reduce/remove tourniquet pain include inflation for short periods of time only (during cementation) and not using a tourniquet at all; the latter possibly resulting in a substantial blood loss of 1.5 L and a 12.6% blood transfusion rateCitation162. Wanting to avoid the corresponding longer LOS (I), fibrin sealants and bipolar sealers could be explored as both have shown promising results although in very few and small studies with a reduction in blood loss and equal clinical outcomeCitation163, Citation164. However, only the bipolar sealer has the ability to keep the surgical field dry and avoiding tourniquet application.
In conclusion, fast-track surgery should exclude traditions supported by limited or no evidence but request randomized controlled studies comparing modalities to clarify their potential value. Fast-track is more like a philosophy attempting to incorporate evidence-based clinical enhancements dynamically by constantly evaluating and replacing features with more efficient ones. Patients should always count on and expect to receive the best available treatment resulting in a high degree of satisfaction with the outcome.
2.8 Patient expectations and satisfaction
A review regarding the outcomes of THA and TKA as evaluated by health-related quality-of-life instruments found the procedures to be quite effective and THA appears to return patients to function to a greater extent than TKACitation165. However, patients have different expectations as to outcome following THA and TKA and these may influence satisfaction. A study found expectation of complete pain relief after surgery to be an independent predictor of better physical function and improvement in level of pain at 6 months post-surgery; and expectation of low risk of complications was an independent predictor of greater satisfactionCitation166. Another study found 18.6% of patients not satisfied with their arthroplasty at one year and predictors hereof was the pre-operative SF-12 mental component score, depression and pain in other joints, the six-month SF-12 score and poorer improvement in the pain element of the Oxford Knee Score. Patient expectations were highly correlated with satisfactionCitation167. Supporting these data are other studies finding lower preoperative SF-36 mental health score to independently predict patient dissatisfaction – regardless of Western Ontario McMaster University Osteoarthritis IndexCitation168.
Achieving satisfied patients during hospitalization is essential: apart from being an indicator of the quality of care delivered, it may inflict positively on the overall outcome as shown in a recent study on satisfaction with care after THA and TKA as this predicts self-perceived health status 1 year after surgery with higher scores on the SF-36Citation169.
Thus, measuring patient satisfaction in the perioperative phase is in itself an important outcome but also predictive of the intermediate and long-term outcome. Perioperative satisfaction is found to be associated with a number of factors (I); most importantly: the shorter the LOS, the more the patients were satisfied with information, nursing, pain treatment, doctors rounds, LOS and the entire stay (I). The older patients were more satisfied – and 2 subgroups of patients needing special attention were identified: patients with co-morbidities were less satisfied with both pain treatment and LOS, and patients using opioids prior to the operation were less satisfied with the entire stay. Although these outcomes were obtained prior to the inclusion of LIA and the more extensive multimodal pain treatment, data show a need to focus on pain treatment for these 2 subgroups. A study on patients with co-morbidities (3 or more) following THA and TKA revealed a lack in continuity of care of co-morbidities resulting in reduced well-being and delayed recoveryCitation170.
Overall, a patient satisfaction of 9.4 of 10 was achieved with median values for all satisfaction measurements of 10, indicating a high degree of satisfaction in unselected consecutive primary THA and TKA patients with this fast-track set-up. Similar results regarding satisfaction have been found in patients following ANORAK in bilateral simultaneous TKA (VI) and non-septic revision TKA (VII) and in other studiesCitation116. Again, the logistical set-up may influence outcome – as an earlier study on satisfaction found patients to be more satisfied when doctors rounds was performed by the operating surgeon ensuring continuityCitation117. In a nationwide study, patients from departments with short LOS were equally or more satisfied on all parameters compared to patients from hospitals with longer stays (III) – reassuring staff and administrators alike that it is not LOS per se but rather the contents of the track making a difference.
Other factors than early perioperative satisfaction may affect later outcome as a study demonstrated an association between good satisfaction at 2 years and absence of complications, absence of depression, body mass index less than 27kg/mCitation2, severe joint space narrowing before operation, and age greater or equal to 70 yearsCitation171. Three of these factors can be assessed before surgery (age greater than 70 years, absence of obesity, and severe joint space narrowing) and although not in themselves usable to pinpoint right candidates for operation, they may together with other criteria such as mental status (depression) be indicative of subsequent patient satisfaction with the outcome. Apart from manifest depression, a variety of psychological factors could be predictive of a poor outcome; low self-efficacy, poor pain coping strategies, somatization, and low social support etc.Citation172. Educational level has also been found to be associated with a good outcome 1 year after THACitation173
Expectations, mental state (depression), patient-characteristics, and pain thus seem to predict and influence satisfaction the most. As surgeons we have to modulate and manage patient expectations as to what to expect from surgery in order not to have a mismatch between expectations and outcome leading to potential dissatisfaction. High, possibly unrealistic expectations of TKA have been found common and rooted in both patient-related factors as different scoring systemsCitation174. As expectations may differ between patients from different countries as well, the problem of managing expectations is indeed multi-factorialCitation175. Information on what to expect should be part of the preparation of the patients before surgery and has been demonstrated to result in more realistic expectations regarding outcome and increased satisfaction at 3 monthsCitation176.
Subsequent, patient satisfaction may depend on a variety of factors – including uncertainty versus thorough information on what to expect. The latter demonstrated by the occurrence of noise, numbness and kneeling difficulties in 69–82% of TKA patients, which patients were not informed on and leading to dissatisfactionCitation177.
In conclusion, modulating patient expectations may inflict on satisfaction, which again may result in higher satisfaction a year after surgery. Short LOS following fast-track surgery has not been found to impair satisfaction; on the contrary and patient satisfaction should be measured to give a patient-based assurance of quality.
3. Organizational aspects
Fast-track surgery combines optimized organizational and clinical aspects from patients being admitted till discharge. This perioperative period may be stretched in both directions to include the pre-hospital and post-discharge periods as well but the evidence on team and service outcome is lackingCitation178. Ideally, the patient with co-morbidities has these accompanying diseases optimized before referral, is well-medicated, has a proper diagnosis with standing fully weight-bearing radiographs, etc. Following discharge, the patients should experience a smooth transition from hospital to general practioners, the latter being fully informed on the postoperative course, multimodal pain treatment, when to react (infection, DVT, indication for manipulation) etc. These factors in the healthcare system surrounding the hospital will vary and it is up to the hospital to inform its colleagues on how to improve this collaboration if needed. However, the following section on organizational aspects of fast-track THA and TKA will focus on the perioperative course in hospital only as this environment can be standardized for the benefit of the patients to ensure optimal outcome.
3.1. Implementation
A prerequisite for successful implementation of a fast-track set-up is preparation. Focus needs to be on the current path (or lack thereof) regarding outcome and identification of which factors one desires optimized. Again, the Deming circle of Plan-Do-Study-ActCitation140 is useful starting with a planning phase in which one reads, listen to talks and visits departments with a fast-track set-up up and running. Then one decides on which clinical and organizational aspects to include; the clinical features should be evidence-based and are thus “universal” whereas the organizational set-up may depend on local factors. Physical environment, economy, presence of other specialties and collaboration, quick access to radiographic documentation, traditions etc. may present challenges or barriers to overcome. Organizing some form of outcome measurement to study is important in order to document the changes and for reassurance: LOS, complications/readmission and patient satisfaction are easily accessed and provide the basic for quality controlling of the fast-track. Next is the evaluation phase (Act) to evaluate if the goal was achieved and then set a new one. The discharge criteria are key: they should be functional and unaltered. The current LOS should dictate which organizational or clinical features to focus on. If LOS is in excess of around 7 days, focus should be on organization; if LOS is between 4 and 7 days also clinical features should be optimized (anaesthesia, pain treatment, blood loss, etc.) and only when LOS is below 3-4 days fine-tuning of the organizational and clinical (primarily pain treatment and mobilization) features makes sense.
As experiences were gathered from ANORAK-HH (I), LOS was reduced locally in our departmentCitation117, Citation118 to around 4 days. In Denmark in the same period, LOS was 8–9 days following THA and TKA (2003)Citation179. In this context, a prospective nationwide study (III) identified logistical and clinical areas of importance for LOS by identifying departments with short and long LOS and evaluating their set-up. The three departments with the shortest (around 4 days) and the three with the longest (around 12 days) LOS were identified based on the National Register on Patients in 2004 on LOS following THA and TKA. The logistical and clinical set-up was examined to identify factors acting as facilitators or barriers for early rehabilitation and discharge. Also, patients from these departments answered a questionnaire regarding satisfaction with components of their stay, co-morbidity, sex and age. Departments with short LOS were characterized by both logistical (homogenous entities, regular staff, high continuity, using more time on and up to date information including expectations on a short stay, functional discharge criteria) and clinical features (multimodal opioid sparing analgesia, early mobilisation and discharge when criteria were met) facilitating quick rehabilitation and discharge. Patient demographics from departments with the shortest stay were similar regarding age, sex and co-morbidities compared to patients from departments with longer stays. There was no difference in staffing (nurses/physiotherapists) between the two types of departments.
With regards to the implementation procedure of ANORAK-HH (I), this was headed by a few dedicated staff members (surgeons, nurses) (III). Thorough information was shared with all members of the team to ensure a uniform approach and areas of special interest were given to individuals upon request (teaching at multidisciplinary patient clinics; optimization, documentation and updating of care principles; pain; assisting in consultant out-patient clinic and preoperative assessment clinics; manning of the nurse outpatient clinic; etc.) – in order to strengthen ownership to the concept and motivate team spirit. The uniform approach includes principles of mobilization, pain treatment, motivation and information of patients. A special ward was established admitting only arthroplasty patients; only regular staff was used securing a high degree of continuity; the functional discharge criteria and intended LOS made known to both staff and patients. Multiple and repeated meetings with all involved specialties (surgeons, nursing staff, physiotherapists, porters, occupational therapists, anesthesiologists, radiologists, theater nurses, and nurses from PACU) were and are being held in order to constantly improve the organization around the patient to optimize flow and minimize waiting time.
A database was established registering 22 patient characteristics and 11 parameters on satisfaction: patient clinic, information (booklets), operating room stay, recovery ward stay, nursing, pain-treatment, physiotherapy, surgeon rounds, physical conditions, LOS and the entire stay (VAS 0–10 on all parameters, 10 being the best), .
In addition, all procedures – clinical and logistical – were evaluated: the former for evidence, the latter for practicality. When optimized, all procedures were rationalized and standardized.
Thus, the cornerstones of the fast-track set-up are the: information on intended max. LOS, multi-disciplinary pre-admission patient-clinic, motivation of the patient to be an active participant, dedicated specialized staff, and rationalization and standardization.
In conclusion, implementation of fast-track includes evaluation of the existing set-up and depending on this, various actions may apply. Studies have identified both clinical and organizational factors associated with departments with short LOS.
3.2. Department
A specialized ward with a fast-track set-up (I, III) may result in shorter LOS compared to departments with more conventional pathways and a case-mix including acute patients or with conventional pathways with only elective orthopedic surgeryCitation126. Other benefits include patients being among only similar patients sharing experiences and not being disturbed by the more noisy acute setting with admittance of patients around the clock. Also, the specialization of the nursing staff is beneficiary in this regard as they accumulate knowledge and experience. Although a regular satisfaction survey has not been performed among the nursing staff, the very low morbidity among staff may be indicative of a high degree of satisfaction (III). Continuation in the form of daily doctors rounds by the operating surgeon is also facilitated by this set-up and does increase patient satisfactionCitation117.
All patients are admitted in the morning on the day of surgery as there is no need for the patients to be hospitalized before the operation. DVT prophylaxis is best initiated 6-8 hours after the operationCitation67 and preoperative blood sampling is reduced to the necessary and does not include matching of blood for the routine primary THA or TKACitation180, Citation181. Patients pausing anticoagulants are not operated as number 1 on the program, which leaves plenty of time to draw a fresh blood sample to secure the International Normalized Ratio (INR) to be within the appropriate range.
As a study demonstrated patients who were operated in the end of the week to stay longer than patients operated on at the beginning of the week (I) due to organizational factors (less staffing in weekends), it was decided to only operate on arthroplasty patients Monday to Wednesday. Other benefits included higher satisfaction as patients were seen only by their surgeonCitation117 and also the ward was reduced to being open only Monday through Friday. Apart from economic savings, this was allowing the nursing staff not to work weekends and is believed to be appreciated by the staff.
The volume of patients per year passing through the department and the volume of the individual surgeons affiliated with the department may influence LOS as well. A very large study looking at patient- and provider-characteristics demonstrated an association between individual surgical volume (<67 TKA and <50 THA per year) or hospital volume (<101 TKA and <65 THA) and LOS with cutting-off limits in brackets for poorer performance regarding LOSCitation135 – the latter association was also found in other studiesCitation182 including a Danish nationwide studyCitation121.
In conclusion, a ward specialized in and admitting only arthroplasty patients may facilitate fast-track; organizational aspects including day of surgery and also volume may affect LOS.
3.3. Staff
The staff involved in fast-track surgery should have a uniform approach towards giving the patients the evidence-based care-principles. Dedicated leaders should be front-runners. As fast-track is a multidisciplinary team-effort, dedicated representatives from each involved group of staff and specialty should form a team of decision-makers. In reorganizing the perioperative care process the team members can improve logistics by gaining insight into each other’s fields and thus plan the best possible flow for the patients through the organization and process. A study on the relation between the organization of care processes and patient outcomes in THA and TKA measured by the validated Care Process Self Evaluation Tool (five subscales: (i) patient-focused organization; (ii) coordination of the care process; (iii) communication with patients and family; (iv) collaboration with primary care; and (v) follow-up of the care process) found an effect on LOS by use of fast-track, coordination hereof, and communication with patients and familyCitation183. Also, the impact of the concept of relational coordination between team members on the quality of care, postoperative pain and functioning, and LOS was studiedCitation184. It was found that relational coordination between staff members improved quality of care (judged by the patients), postoperative pain, reduced LOS and that postoperative functioning was improved by the frequency of communication, the strength of shared goals, and the degree of mutual respect among team membersCitation184. The interpersonal manner of medical practitioners and nurses were found to be associated with patient satisfaction in another studyCitation185. Thus, optimization of organizational issues by dedicated staff working together in relational coordination and informing the patients in a kind, clear way will influence the functional recovery and satisfaction of the patients. It is worth noting that the surgeon’s attitude and interpersonal manner was judged more important by the patients than the nurse’s interpersonal mannerCitation185.
In conclusion, the combined multi-disciplinary staff efforts of fast-track may inflict positively on LOS, satisfaction and pain perception, especially if reflecting relational coordination.
3.4. Information
Preoperative information on the upcoming perioperative track and expected outcome is essential and serves multiple purposes. Apart from the basic information on the intended operation, the associated benefits and risks (which is also mandatory by law), more detailed information should be available. First, patients will need to know the intended maximum LOS and the discharge criteria in order to be motivated to participate actively and get an understanding of the contents of the fast-track facilitating adherence. Second, expectations should be modulated preoperatively as this may produce more satisfied patients. Third, preoperative information may reduce anxiety.
In order to inform unbiased, the surgeon should give evidence-based information including on what to expect during early recovery. A study on patient abilities at 4–5 weeks postoperatively following a mean LOS of 2 days demonstrated that 80% of patients walked without a cane, 54% drove a car, and around 90% already found the operated knee wellfunctioningCitation186. Less pain was experienced, which was confirmed in a fast-track study on sub acute painCitation32. Another study found the patients’ preoperative expectation to be higher than their postoperative abilityCitation187. 93% of the patients were generally satisfied 5 years postoperatively, while 87% were satisfied with the relief of pain and 80% with their improvement in physical function at that time – indicating that satisfaction is not equivalent to fulfilled expectations. It is concluded that: ”preoperative counseling should include realistic information on outcomes concerning physical function and pain relief”Citation187.
Information in fast-track settings are often provided during group sessions apart from individual counselingCitation112. A nationwide study found fast-track departments to use 2–3 times the amount of time on preparing/informing the patients on the upcoming hospitalization compared to departments with more conventional stays (III). This resulted in higher satisfaction among THA patients (III). However, it was also found that no difference regarding satisfaction existed within the fast-track setting between patients attending the preoperative patient seminar and those who did not (I). This is probably due to the fact that it is not the seminar in itself but rather the sum of information given during the (short) stay resulting in increased satisfaction. This finding is in accordance with a Cochrane review stating that there is no evidence to support the use of pre-operative education over and above standard care to improve postoperative outcomes (pain, function or LOS) in THA and TKA patients, but a modest beneficial effect on preoperative anxiety and none on postoperative anxietyCitation188. This is not to say that preoperative information does not make a difference and if nothing else it may modulate patients’ expectations, educate the accompanying relatives and constitute an efficient way to inform patients in plenary sessions and also strengthen the relational coordination between staff members and finally show good interpersonal manners of all participating staff members. Also, written information in an easy read language on each day and activity may be part of a fast-track and may also address the support of family and friendsCitation130.
Thus, in conclusion, information should be extensive on the upcoming track and outcome and can be given in plenum at a multidisciplinary preoperative patient seminar, but should not be expected to reduce LOS, pain or satisfaction.
3.5. Discharge criteria and traditions
Achievement of functional discharge criteria should result in subsequent discharge – without organizational issues causing a delay. Thus, waiting for radiographs to be taken, blood transfusions to be given, establishment of home-based help or care to be effective, etc. should be avoided by securing these logistical features in due time. A detailed study on why patients are hospitalized following fast-track with LOS median 2 days and optimized logistics revealed such organizational factors to remain a challenge from operation till discharge for at least 18% of patients (IX). Also, waiting for the surgeon to arrive to discharge the patient the traditional way by next morning’s surgical rounds makes no sense when the discharge criteria are known beforehand by both nursing staff and patient and fulfilled in the afternoon. These organizational issues illuminate the interaction between clinical and organizational factors influencing LOS. If functional discharge criteria are fulfilled, organizational lackings may delay actual discharge high-lighting the importance of a well organized expeditious flow regarding fulfillment of logistical “milestones”.
Traditions may influence this process tremendously – both locally as well as nationwide. Local traditions may come into play regarding when to start mobilization out of bed, when to allow full weight-bearing when to begin physiotherapy, when to change walking aids to crutches, when to take radiographs, when to have the occupational therapist to deliver aids to ease the home-based situation etc. etc. Nationwide or cultural traditions may dictate a certain LOS regardless of faster functional recovery and fulfillment of discharge criteria (if any). A nationwide study from Japan around 2007 found a mean LOS following TKA of 35 daysCitation182 as opposed to about 6-12 days in Germany and the UK and 3-4 days in the USACitation135 and Denmark (unpublished data). LOS from some of these studies may not include transferral to rehabilitation facilities, potentially influencing outcome negatively as more readmissions have been found from skilled nursing facilities than from homeCitation189.
In conclusion, organizational issues should be resolved before fulfillment of functional discharge criteria to avoid these or traditions to cause a delay in subsequent discharge.
4. Safety aspects
Safety aspects following fast-track include morbidity and mortality, the first in the form of complications and readmissions. LOS, safety and satisfaction are key outcomes and may affect each other. Upon changing a perioperative course, it is mandatory to have evaluation of safety aspects as top priority along with patient satisfaction.
As fast-track surgery includes optimization of clinical features in the form of application of evidence-based enhancements, no negative influence on morbidity or mortality is expected. Receiving the best available treatment leads to achievement of functional milestones including discharge criteria more rapidly than following conventional treatment (based in greater extent on non-evidence based treatment and traditions). However, the subsequent reduction in LOS would turn a complication immediately following discharge into a potential readmission whereas the same procedure-specific complication occurring at the same time following conventional treatment with longer LOS would not be registered as a readmission but handled during the index hospitalizationCitation190. Such a readmission is not due to fast-track surgery in itself and does not justify longer hospitalization.
4.1 Morbidity/readmissions
A detailed study on readmissions following fast-track surgery (ANORAK-HH) in a consecutive, unselected cohort study of 1,731 patients operated with primary THA or TKA found mean LOS to decrease from 6.3 to 3.1 days in the study period of 5 years from 2003 to 2008 (IV). Within 90 days, 15.6% of patients following TKA were readmitted as opposed to 10.9% after THA (p = 0.005). Suspicion of DVT (not found) and suspicion of infection made up half of the readmissions. Readmissions in general and for thromboembolic events, dislocations and manipulations in specific did not increase with decreasing LOS. It is concluded, that fast-track does not increase readmission rate following THA and TKA compared to other studies on more conventional stays and fast-track is thus considered safe regarding morbidity (IV). Readmission rates of 15.6% and 10.9% may at first glance appear high, especially when compared to the rates of 7.9% and 6.8% registered earlier (September 2003–December 2005) (I), but the definition of a readmission was broadened in (IV) to include other diagnoses including medical.
Comparison of readmission rates between studies is difficult as readmissions are defined differently and include varying diagnoses in the published studies and also depends on the thresholds for readmission by patients and physicians, presence of co-morbidities, access to diagnostic tools, beds, the completion of follow-up, etc. Also, the same complication may be treated in an outpatient setting in one institution and during readmission in another (i.e. suspicion of DVT or wound infection). Half the readmissions in (IV) were due to suspicion of DVT or infection and removing those diagnoses, produces readmission rates of 8.0% for TKA and 7.3% for THA, which are comparable to or lower than other studies both on fast-track and following conventional staysCitation5, Citation144, Citation191-197. In order to reduce these unnecessary readmissions by the general practioners, a nurse-manned out-patient clinic was established 3 weeks postoperatively offering all patients the opportunity to have their wound clamps removed, the wound inspected and to ask questions. However, a recent meta-analysis concluded that no study comparing a clinical pathway with standard care has shown an increased rate of readmission in general with hospitalization ranging from about 3.2 to 12.8 daysCitation127.
Concerns regarding specific readmissions in the form of dislocation in THA and manipulation in TKA have been aired. Dislocation rates around 3.9–4.5% have been found with the posterior approachCitation190, Citation198. A study found in increase in dislocation rate from 0.5% to 3.9% when LOS was reduced from 6.3 to 3.9 daysCitation199 and concern was expressed and shared with another studyCitation190 on more readmissions as LOS is decreasing. Too short a period of practicing restrictions was estimated to be the cause. Contrasting this, the study (IV) demonstrated a decrease in dislocation with a similar reduction in LOS from 6.3 to 3.9 days and could thus not support an increased rate of dislocation when LOS is reduced. In support of this, a study on 2612 THAs followed for a mean of 14 months found a dislocation rate of 0.15% - without any restrictions at allCitation200. As large-diameter heads are introduced more frequently in THA, the dislocation rate may decrease to an even lower level as a study found 1/2020 THAs to dislocate using heads >36 mm for a rate of 0.05%Citation201. Also, 2 studies found the rate of manipulation after TKA to increase: from 6 to 14% while reducing LOS from 7.2 to 4.2 daysCitation9 and from 6 to 12% while reducing LOS from 6.4 to 4.4 daysCitation115. The indication for manipulation was similar to ours (< 90 degrees of flexion around 6 weeks). However, no cause was identified for this increase and it was concluded that from an economical point of view, an increase in LOS in order to avoid manipulations could not be justified. Since we found no increase in manipulations when LOS was reduced from 4.6 to 3.1 days and, as the rate of manipulation was 1% for the period, it is concluded that fast-track TKA does not increase the risk of manipulation. With the focus on early multi-modal pain treatment including the LIA technique and techniques for reducing intra-articular bleeding, rates of manipulation due to arthrofibrosis may be further reducedCitation202.
Thus, in conclusion, fast-track does not produce more complications – nor in general nor in specific (dislocation, manipulation, thromboembolic episodes) – and does not result in an increased number of readmissions.
4.2 Mortality
Mortality following fast-track THA and TKA has been studied (IV, V). From 2004 to 2008, 14 patients died within 90 days of surgery: 3 in 2004 [mesenterial thrombosis (89 days), myocardial infarction (2 days), sepsis/pneumonia (27 days)]; 3 in 2005 [hepatic cirrhosis and coma (28 days), perforated colonic cancer (51 days), sudden death (1 day, no autopsy)]; 3 in 2006 [metastatic lung cancer (77 days), dysregulated warfarin treatment (resulting in massive bleeding) for atrial fluttering (50 days), perforated gastric ulcer (22 days)]; 4 in 2007 [cardiomyopathy and failure (89 days), lung cancer (10 days), mechanical bowel obstruction (76 days), hepatic cirrhosis with esophageal bleeding (83 days)] and 1 in 2008 [aortic stenosis, pulmonary insufficiency and cardiac failure (19 days)]. Deaths possibly related to postoperative complications following the index arthroplasty operation were: 1 in 2004, 1 in 2005, 1 in 2006, 0 in 2007 and 1 in 2008, giving an overall potential surgery-related mortality rate of 0.35% (IV). Thus, 3 deaths of 1,977 (0.15%) THA, TKA and BSTKA were found to be associated with clotting episodes (V) (0.17% of 1,731 THA and TKA (IV), same material). These incidences of death following fast-track surgery are lower or comparable to other studies on more conventional tracksCitation64, Citation66, Citation77-79, Citation81-85.
In conclusion, fast-track does not increase mortality following THA and TKA compared to more conventional set-ups. This is essential and warrants further detailed studies of mortality in specified sub-groups of patients (i.e. patients with co-morbidities) as high-risk patients may actually benefit also regarding reduced mortality from fast-track.
4.3 Bilateral arthroplasty and revision arthroplasty
Fast-track surgery represents the best available treatment including both clinical and organizational aspects and has shown superior results compared to more conventional stays regarding outcome, patient satisfaction, and safety for primary, unselected TKA and THA (I, II, III, IV, V). Can it also be applied to other patient-groups operated on with bilateral and revision arthroplasty? These operations are more complex and may cause surgical stress to a greater extent including blood loss.
Bilateral simultaneous total knee arthroplasty (BSTKA) is often associated with higher mortality and morbidity rates compared to unilateral total knee arthroplasty (UTKA)Citation203-205. However, as fast-track has shown superior outcomes in unilateral, primary THA and TKA and as no previous study has investigated the outcome of BSTKA in a fast-track setting, a study was undertaken. A prospective cohort study on patients operated with BSTKA analyzed the outcome of 150 consecutive, but selected, BSTKA compared to 271 unilateral total knee arthroplasties in a standardized fast-track setting (VI). Apart from staying longer (mean 4.7 days vs. 3.3 days) and using more blood transfusions; the outcome at 3 months and 2 years follow-up was identical or better in the bilateral group regarding morbidity, mortality, satisfaction, range of motion, pain, use of walking aids, ability to return to work and ability to perform activities of daily living. Bilateral simultaneous total knee arthroplasty can be performed in a fast-track set-up with satisfactory results (VI). Also, safety issues have been studied: in 123 patients operated with BSTKA (246 TKAs) no patient died, no patient developed PE or DVT (V). This is in accordance with another study also finding BSTKA to be safe, with few complications, low mortality, and few VTEsCitation206.
Bilateral simultaneous total hip arthroplasty (BSTHA) is as debated as BSTKACitation82, Citation207, Citation208. In the first and only study on BSTHA in a fast-track setting on 50 consecutive patients with median LOS of 4 days, mortality was 4% and 8% needed a reoperation within 90 daysCitation209. The overall complication rate was 22% with around half considered to be caused by the surgical technique per se and half not being related to the surgery. It is concluded that BSTHA may have a high complication rate despite a fast-track setting and that further safety studies in larger series are neededCitation209.
Revision surgery is performed because of varying underlying reasons and often with a less predictable outcome compared to primary arthroplasties. Studies have found LOS following all revisions to be around 5-6 days (however including all revisions and only 35% with all components exchange)Citation205, Citation210. In non-septic revisions of TKA, the final revision-prosthesis is in place and functioning immediately after surgery and theoretically these patients would benefit from fast-track as well as they can be mobilized right away – but no studies are available except a feasibility study (VII). This prospective cohort study on 29 consecutive, unselected patients operated with 30 revision total knee arthroplasties for non-septic indications in a fast-track setting evaluated whether patients undergoing revision TKA could follow a standardized fast-track set-up designed for primary TKA (ANORAK-HH) with a similar outcome as primary TKA. LOS was median 2 (1-4) days for all but 1 patient who was transferred to another hospital for logistical reasons. No patient died within 3 months and 3 patients were readmitted (2 for suspicion of DVT but not found and one for manipulation). Patient satisfaction was high. It is concluded, that patients undergoing revision TKA for non-septic reasons can follow a fast-track set-up with an outcome comparable to primary TKA regarding LOS, morbidity, and satisfaction.
Thus, in conclusion, fast-track may produce excellent outcomes for other arthroplasty procedures than primary THA and TKA, including bilateral simultaneous total knee arthroplasty and non-septic revision total knee arthroplasty whereas bilateral simultaneous total hip arthroplasty may be associated with complications despite a fast-track set-up.
5. Economic aspects
The change in the reimbursement with DRG-grouping in the USA in the 1980`ies put focus on the economy regarding hospital stays associated with THA and TKA – as net losses were noted in some instancesCitation2, Citation3. Mabrey et al. (1997) were among the first to describe how a reduction in LOS from 10.9 to 4.7 days (57%) including careful monitoring of different steps (rationalization of radiographs and blood testing) would lead to a reduction in total costCitation2. A correlation was found between LOS and total cost in the control group (generating a net-loss of 863 USD per patient) whereas the CP-group generated a win of 2.334 USD per patient. Early planning of discharge was concluded to be essential allowing the patients to aim at achieving this realizing the biggest savings by reducing LOS from 7 to 5 days. This study was followed by others to document economic savings by reducing LOSCitation1, Citation4, Citation5, Citation211, Citation212.
Healy et al. (1997) documented that in patients operated with TKA staying 6 days in hospital, 49% of cost were related to the operating room; 9% to the PACU; 9% to the pharmacy; and only 12% to the ward stay and 4% to cover the physiotherapyCitation4. The most expensive day was the day of operation which accounted for 72% of the total costs followed by 8%, 7%, 5%, 3%, and 2%, respectively, for the following days. Also, in another study, 56% of total costs were associated with the operating room and PACU stays; whereas 17% were prosthesis-related costs and 23% associated with the stay in the wardCitation1. This study argues for focusing on a reduction of the 56% cost generated the first day as reducing LOS only affects the final less-costly days in hospital. One way of doing so is to reduce the cost associated with the prosthesis and several studies have demonstrated savings by matching implant to patient and negotiations with the manufacturers regarding price reductionsCitation1, Citation4, Citation8, Citation213. A reduction of operating time has also been demonstrated to affect total costs in a system where the minutes spent in the operating room are priced – a reduction of 54% in cost were achieved as opposed to savings of 16% from a reduction in LOSCitation212. The rationalization of medication, blood products, radiographs, anaesthesia and physiotherapy combined to savings of 30% when reducing LOS from 6.7 to 5.7 daysCitation212.
These studies from USA illustrate the reduction in cost associated with a reduction in LOS to around 5–6 days where focus primarily has been on economy. In 1998, an international survey among 110 orthopedic surgeons from 30 countries found that 80% stated to be under pressure to reduce cost and 68% to reduce LOSCitation213. However, from a patient point of view, economic savings come second to improving the outcome. Combining the patient and economic point of views, patients should stay as short as necessary combined with the highest patient satisfaction and the fewest complications and readmissions.
A Danish study compared the outcomes and costs associated with fast-track compared to more conventional stays in departments doing only elective surgery and departments with a case-mix of both arthroplasty and acute surgeryCitation126. Fast-track surgery had shorter LOS; similar or better outcome regarding readmissions and contacts to the general practioners and physiotherapists – and reduced costs. Although varying costs were associated with different parts of the perioperative stay, the majority of savings (33-39%) were related to the reduction in LOSCitation126 – a finding also found by someCitation3, Citation214, but not allCitation1, Citation4, Citation212, Citation215. Nevertheless, small or large, economic savings from a reduction in LOS may have a huge impact on total savings. A recent study found that each additional day in a patient’s LOS was associated with an 8% increase in hospital charges – and that a reduction of just one day may have a significant impact on the 11.9 billion USD spent on TKAs in USA in 2003Citation135. However, although savings may be huge on a national scale, concern has been aired as to the sustainability of the current DRG-system. One study concludes: “During the last 25 years, our economic experience with TKA is concerning. Hospital revenues have lagged behind inflation, hospital expenses have been reduced, and our institution is earning a profit. However, the margin for TKA is decreasing and Managed Medicare patients do not generate a profit. The erosion of hospital revenue for TKA will become a critical issue if it leads to economic losses for hospitals or reduced access to TKA”Citation3. In some countries, including the USA and Germany, reimbursement is reduced if patients are staying shorter than a fixed LOS. This lack of economic incentive could be a serious barrier for further improvement of the fast-track concept and halt further research on clinical enhancement. Two Danish studies have documented that a) more time (2-3 times the amount used in conventional tracks (III)) and b) more money was used on preoperative preparation of the patients in the fast-track set-up compared to one of the more conventional staysCitation126 indicating the need for further studies on economic aspects – before conclusions are reached regarding the size of reimbursements relying solely on LOS. As no studies have looked at the economics following modern fast-track THA and TKA with LOS around 1-3 days, detailed studies hereof are warranted.
In conclusion, reviews; meta-analyses; and Cochrane reviews on outcomes following fast-track THA and TKA all have found economic savings compared to more conventional set-upsCitation127, Citation131, Citation178.
6. Conclusions
Fast-track surgery is a dynamic entity evolving with clinical enhancements and concomitant organizational optimization constantly interacting (). Outcome measurements in the form of LOS, morbidity/mortality, safety aspects, patient satisfaction and economy among others are essential to monitor outcomes regarding all parameters. The studies included in this thesis use these outcome measurements to ensure a satisfactory clinical outcome for the patients combined with a rationalized patient-friendly organizational flow. Underlying care principles detailing procedures are essential fundamentals for continuation, standardization and rationalization of both clinical and organizational aspects.
A fast-track set-up is described in detail with resulting LOS in primary unselected consecutive THA and TKA and identifying patient-related characteristics associated with LOS and satisfaction (I). LOS was influenced by age, sex, ASA-score, the need for blood transfusion, and the time till first mobilization whereas patient satisfaction was positively associated with short LOS. Also organizational barriers for early discharge were identified (operation at the end of the week). The results of this study allow for identification of subgroups needing special attention and also potentially facilitating planning of bed occupancy. Other patients than primary THA and TKA may enter the fast-track as studies have demonstrated both bilateral simultaneous TKA (VI) and non-septic revision TKA (VII) to have satisfactory outcomes comparable to primary outcomes regarding most parameters. Patients operated with bilateral simultaneous TKA were staying a little longer and using more blood transfusions than a control group of primary unilateral TKA; the outcome at 3 months and 2 years follow-up was identical or better in the bilateral group regarding morbidity, mortality, satisfaction, range of motion, pain, use of walking aids, ability to return to work and ability to perform activities of daily living. Fast-track revision TKA for non-septic reasons resulted in LOS of median 2 days with no mortality, low morbidity and high patient satisfaction.
Organizational issues acting as facilitators of or barriers for early discharge have been identified as part of a nationwide study on both clinical and organizational features characterizing departments with short LOS (III). Departments with short LOS were characterized by having homogenous entities, regular staff, high continuity, using more time on and up to date information including expectations on a short stay, and functional discharge criteria. Optimized clinical features included multimodal opioid sparing analgesia, early mobilisation and discharge when criteria were met facilitating quick rehabilitation and discharge. Fulfillment of functional discharge criteria is a prerequisite for discharge ensuring the patients capability to cope at home.
Organizational factors such as implementation of fast-track; teaching a dedicated staff to have relational coordination and a uniform approach focusing on information and motivation; and establishment of a ward specialized in and admitting only arthroplasty patients may facilitate fast-track. Other organizational aspects including day of surgery and volume may also affect LOS.
Traditions not supported by evidence may be a challenge to change as these may act as barriers for establishing new evidence-based features subsequently delaying early discharge.
Patient expectation may influence on outcome and modulating patient expectations may inflict on satisfaction, which again may result in higher satisfaction a year after surgery. Short LOS following fast-track surgery has not been found to impair satisfaction – on the contrary and patient satisfaction should be measured to give a patient-based assurance of quality.
Sufficient pain treatment is a key factor in facilitating early functional recovery and enhanced by the use of multimodal opioid-sparing analgesia in addition with blockade of the pain originating at the surgical site. Gold standard is a peripheral nerve block following TKA, but LIA may someday be replacing peripheral nerve blocks as the preferred modality as it is safe, efficient and easy to apply. The addition of a compression bandage is improving the analgesia for the first 8 hours in TKA (II). LIA on the other hand was not found to give additional analgesia in THA with the concomitant use of multimodal opioid-sparing analgesia and pain scores were low at all times and during all activities (VIII). Glucocorticoids may be added to the multimodal regimen preceded by dose-response and safety studies.
Safety aspects have been studied in detail following fast-track surgery (IV) and (V). As mean LOS decreased in the study period of 5 years, mortality and morbidity remained low demonstrating that dislocations and manipulations in specific did not increase with decreasing LOS. Thromboembolic complications were few with 0.15% mortality from clotting episodes and overall 0.56% clinical DVT and 0.30% PE. In specific, no DVT or PE was found following bilateral simultaneous TKA. These favorable figures were achieved with early mobilization and short prophylaxis till discharge only. The need of extended thromboprophylaxis – if any – is questioned, when patients are mobilized early. Differentiated prophylaxis based on individual risk assessment including timing of mobilization and balancing the risk of bleeding may be optimal. Fast-track does not increase mortality or morbidity following THA and TKA compared to more conventional set-ups.
Although early mobilization reduces LOS and may reduce complications, physiotherapy following THA and TKA is heterogeneous, has limited effect on outcome and may be impaired by muscle weakness partly due to swelling. Efforts to indentify which muscles to stimulate and the best way to do so in combination with counteractions aimed at reducing bleeding and swelling are imperative.
The ultimate question as to why the patient is in hospital following THA or TKA was studied (IX). In order to study and evaluate, fulfillment of functional discharge criteria is a prerequisite for discharge ensuring the patients capability to cope at home. Underlying reasons for not fulfilling these include both clinical and organizational factors to be addressed with a focus on analgesia, orthostatic and muscle function and early physiotherapy and blood transfusion (if needed).
The clinical and logistical factors responsible for postoperative hospitalization showed that pain, dizziness and general weakness were the main reasons for being hospitalized at 24 and 48 hours postoperatively. Nausea, vomiting, confusion and sedation had minimal influence to delay discharge. Logistical challenges were mainly early upstart of physiotherapy (day of surgery) and early transfusion of blood for patients needing this. Future efforts to enhance recovery and reduce LOS after THA and TKA should focus on analgesia, orthostatic and muscle function.
Economic point of views also favor fast-track surgery as reviews, meta-analyses, and Cochrane reviews on outcomes following fast-track THA and TKA all have found economic savings compared to more conventional set-ups.
Thus, many clinical features in the form of combinations of anesthesia, pain-reducing drugs and techniques, mobilization regimens and up-to-date care principles along with optimized logistics, patient education and -motivation, improved surgical techniques etc. combined produce a synergistic result benefitting both patients and economy. Improvements are still possible and warranted and studies hereof needed.
7. Future strategiess
Future strategies are multiple and include both research strategies as efforts to implement the fast-track methodology on a wider basis. It may be difficult, even impossible or unethical, to perform randomized studies on some or all aspects of fast-track, but “well-designed and executed prospective cohort studies can provide high-quality evidence in the evaluation of the effectiveness of surgical interventionsCitation216”.
Research strategies should include a focusing on further optimization of pain treatment (especially after discharge), blood saving strategies, fluid plans and muscle strengthening – as (IX) demonstrated future efforts to enhance recovery and reduce LOS after THA and TKA should focus on analgesia, orthostatic and muscle function.
Focusing on optimizing pain treatment has a dual aim: both to make it more efficient by adding other synergistic analgesic agents to the existing platform of multi-modal opioid-sparing analgesia and to reduce side effects (dizziness, sedation, PONV). Also, and in particular, longer lasting effects are warranted to supplement the 6-8 hours of effective pain treatment offered by the LIA technique in TKA – as catheters do not seem to work. Again, other agents may come into play such as capsaicin (the active ingredient in chili pepper) or repeated (small) doses of glucocorticoids. Dose-response and safety studies are needed for glucocorticoids as well as for gabapentin. Prediction of high-pain responders is another interesting area of researchCitation57, Citation217 as the ability to foresee which patients will need extra attention regarding effective pain treatment is essential; gene testing may be a prerequisite.
Gene testing may also predict which patients are at high risk of developing thromboembolic complications. Identification of high-risk patients may allow for differentiation of prophylaxis and target longer and more extensive prophylaxis at patients in specific need hereof – allowing patients at low risk a less extensive (if any) prophylaxis not exposing unnecessary bleeding risks to this subgroup.
As early mobilization may be prophylactic towards thromboembolic complications (V) and muscle weakness was one of the barriers for early discharge (IX), research efforts should also be directed at improving mobilization. A reduction of perioperative swelling may improve muscle strength and clinical factors aiming at this should be studied (fibrin sealants, bipolar sealers) – as they may also facilitate not using a tourniquet. The tourniquet often produces pain far more severe than from the operated knee and operating without a tourniquet with accompanying low blood loss is desirable. Questions to be answered in doing so include studying the quality of cementation when not using a tourniquet (RSA studies on randomized patients with/without tourniquet). Also, different approaches including MIS with muscle-sparing may prove of value as some muscle-groups are more active during gait. Timing of early mobilization – and amount hereof – depends on both clinical and organizational factors: dosage of analgesics in the spinal, when has the spinal worn off, pain treatment ensuring a smooth transition from central to more peripheral blockade (LIA – has epinephrine any added value?), physiotherapists available at return from PACU etc. and efforts should focus on strategies to allow patients to take full advantage of the potential to begin their early functional recovery. Efforts should also address the contents of physiotherapy as regular strength training – ideally addressing identified specific muscles – may prove to be more beneficent than the previous used regimens.
Orthostatic intolerance has been demonstrated to make early mobilization difficult by impairment of the postoperative postural cardiovascular response by a pathogenic reduction of total peripheral resistance and cardiac outputCitation218 and investigating ways to strengthen the normal response would be of value in improving early functional recovery. Also, avoidance of postoperative cognitive dysfunction is a step towards improving postoperative care and research is ongoingCitation20.
Other areas to explore include optimization of ways to inform and motivate the patients – potentially involving a feedback to ensure coverage of areas of importance to the patients. Preoperative evaluation of the psychological profile of patients – and appropriate action if subclinical depression is detected – may improve the outcome regarding the proportion of satisfied patients.
Strategies to improve the organizational flow may be warranted, even mandatory, for further improvement as waiting for physiotherapy, radiographs to be taken, crutches to be handed out, a surgeon to appear for discharge etc. may be barriers for early discharge when the functional discharge criteria are fulfilled.
Monitoring of safety aspects and patient satisfaction should be mandatory when changing fast-track set-ups – the first gives a clinical assurance of quality and the latter a patient- based assurance of quality. Also, expanding fast-track to include other subgroups of patients, i.e. revision THA and septic revision THA and TKA, would potentially improve outcome.
Finally, detailed economic studies are needed to illuminate the costs of fast-track including the perioperative set-up with extensive preoperative information. The current reimbursement system in Denmark does not (as in some other countries) rely (solely) on LOS, and other factors may contribute to give a fair reimbursement system for both state and hospital.
In conclusion and looking back, much progress has been achieved in many areas in the last decade and hopefully we will achieve “the pain and risk-free THA and TKA” within a few years.
- Stern SH, Singer LB, Weissman SE. Analysis of hospital cost in total knee arthroplasty. Does length of stay matter?. Clin Orthop Relat Res 1995:36-44.
- Mabrey JD, Toohey JS, Armstrong DA, Lavery L, Wammack LA. Clinical pathway management of total knee arthroplasty. Clin Orthop Relat Res 1997:125-33.
- Healy WL, Rana AJ, Iorio R. Hospital economics of primary total knee arthroplasty at a teaching hospital. Clin Orthop Relat Res 2011:87-94.
- Healy WL, Iorio R, Richards JA. Opportunities for control of hospital cost for total knee arthroplasty. Clin Orthop Relat Res 1997:140-7.
- Scranton PE. Jr. The cost effectiveness of streamlined care pathways and product standardization in total knee arthroplasty. J Arthroplasty 1999;14:182-6.
- Healy WL, Iorio R, Ko J, Appleby D, Lemos DW. Impact of cost reduction programs on short-term patient outcome and hospital cost of total knee arthroplasty. J Bone Joint Surg Am 2002; 84-A: 348-353.
- Healy WL, Ayers ME, Iorio R, Patch DA, Appleby D, Pfeifer BA. Impact of a clinical pathway and implant standardization on total hip arthroplasty: a clinical and economic study of short-term patient outcome. J Arthroplasty 1998;13:266-76.
- Iorio R, Healy WL, Kirven FM, Patch DA, Pfeifer BA. Knee implant standardization: an implant selection and cost reduction program. Am J Knee Surg 1998;11:73-9.
- Fisher DA, Trimble S, Clapp B, Dorsett K. Effect of a patient management system on outcomes of total hip and knee arthroplasty. Clin Orthop Relat Res 1997:155-60.
- Kehlet H, Wilmore DW. Fast-track surgery. Br J Surg 2005;92:3-4.
- Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg 2002;183:630-41.
- Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 2008;248:189-98.
- Moiniche S, Hansen BL, Christensen SE, Dahl JB. Kehlet H. [Patients’ activity and length of stay after hip arthroplasty with balanced analgesia and early mobilization]. Ugeskr Laeger 1992;154:1495-9.
- Rasmussen S, Kramhoft MU, Sperling KP, Pedersen JH, Falck IB, Pedersen EM. Kehlet H. [Accelerated course in hip arthroplasty]. Ugeskr Laeger 2001;163:6912-16.
- Kehlet H. [Painless and risk-free surgery--a vision of the future?]. Ugeskr Laeger 1994;156:3468-9.
- Dauri M, Faria S, Gatti A, Celidonio L, Carpenedo R, Sabato AF. Gabapentin and pregabalin for the acute post-operative pain management. A systematic-narrative review of the recent clinical evidences. Curr Drug Targets 2009;10:716-33.
- Clarke H, Pereira S, Kennedy D, Andrion J, Mitsakakis N, Gollish J, . Adding gabapentin to a multimodal regimen does not reduce acute pain, opioid consumption or chronic pain after total hip arthroplasty. Acta Anaesthesiol Scand 2009;53:1073-83.
- Rasmussen ML, Mathiesen O, Dierking G, Christensen BV, Hilsted KL, Larsen TK, . Multimodal analgesia with gabapentin, ketamine and dexamethasone in combination with paracetamol and ketorolac after hip arthroplasty: a preliminary study. Eur J Anaesthesiol 2010;27:324-30.
- Tiippana EM, Hamunen K, Kontinen VK, Kalso E. Do surgical patients benefit from perioperative gabapentin/pregabalin? A systematic review of efficacy and safety. Anesth Analg 2007;104:1545-56, table.
- Krenk L, Rasmussen LS, Kehlet H. New insights into the pathophysiology of postoperative cognitive dysfunction. Acta Anaesthesiol Scand 2010;54:951-6.
- Kerr DR, Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. Acta Orthop 2008;79:174-83.
- Romsing J, Moiniche S, Ostergaard D, Dahl JB. Local infiltration with NSAIDs for postoperative analgesia: evidence for a peripheral analgesic action. Acta Anaesthesiol Scand 2000;44:672-83.
- Adie S, Naylor JM, Harris IA. Cryotherapy after total knee arthroplasty a systematic review and meta-analysis of randomized controlled trials. J Arthroplasty 2010;25:709-15.
- Vendittoli PA, Makinen P, Drolet P, Lavigne M, Fallaha M, Guertin MC, . A multimodal analgesia protocol for total knee arthroplasty. A randomized, controlled study. J Bone Joint Surg Am 2006;88:282-9.
- Busch CA, Shore BJ, Bhandari R, Ganapathy S, MacDonald SJ, Bourne RB, . Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am 2006;88:959-63.
- Essving P, Axelsson K, Kjellberg J, Wallgren O, Gupta A, Lundin A. Reduced morphine consumption and pain intensity with local infiltration analgesia (LIA) following total knee arthroplasty. Acta Orthop 2010;81:354-60.
- Andersen LO, Husted H, Otte KS, Kristensen BB, Kehlet H. High-volume infiltration analgesia in total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. Acta Anaesthesiol Scand 2008;52:1331-5.
- Andersen LO, Husted H, Kristensen BB, Otte KS, Gaarn-Larsen L, Kehlet H. Analgesic efficacy of subcutaneous local anaesthetic wound infiltration in bilateral knee arthroplasty: a randomised, placebo-controlled, double-blind trial. Acta Anaesthesiol Scand 2010;54:543-8.
- Andersen LO, Gaarn-Larsen L, Kristensen BB, Husted H, Otte KS, Kehlet H. Analgesic efficacy of local anaesthetic wound administration in knee arthroplasty: volume vs concentration. Anaesthesia 2010;65:984-90.
- Andersen LO, Kristensen BB, Madsen JL, Otte KS, Husted H, Kehlet H. Wound spread of radiolabeled saline with multi- versus few-hole catheters. Reg Anesth Pain Med 2010;35:200-2.
- Andersen LO, Husted H, Kristensen BB, Otte KS, Gaarn-Larsen L, Kehlet H. Analgesic efficacy of intracapsular and intra-articular local anaesthesia for knee arthroplasty. Anaesthesia 2010;65:904-12.
- Andersen LO, Gaarn-Larsen L, Kristensen BB, Husted H, Otte KS, Kehlet H. Subacute pain and function after fast-track hip and knee arthroplasty. Anaesthesia 2009;64:508-13.
- Andersen LO, Kristensen BB, Husted H, Otte KS, Kehlet H. Local anesthetics after total knee arthroplasty: intraarticular or extraarticular administration? A randomized, double-blind, placebo-controlled study. Acta Orthop 2008;79:800-5.
- Specht K, Leonhardt JS, Revald P, Mandoe H, Andresen EB, Brodersen J, . No evidence of a clinically important effect of adding local infusion analgesia administrated through a catheter in pain treatment after total hip arthroplasty. Acta Orthop 2011;82:315-20.
- Toftdahl K, Nikolajsen L, Haraldsted V, Madsen F, Tonnesen EK, Soballe K. Comparison of peri- and intraarticular analgesia with femoral nerve block after total knee arthroplasty: a randomized clinical trial. Acta Orthop 2007;78:172-9.
- Carli F, Clemente A, Asenjo JF, Kim DJ, Mistraletti G, Gomarasca M, . Analgesia and functional outcome after total knee arthroplasty: periarticular infiltration vs continuous femoral nerve block. Br J Anaesth 2010;105:185-95.
- Andersen KV, Bak M, Christensen BV, Harazuk J, Pedersen NA, Soballe K. A randomized, controlled trial comparing local infiltration analgesia with epidural infusion for total knee arthroplasty. Acta Orthop 2010;81:606-10.
- Spreng UJ, Dahl V, Hjall A, Fagerland MW, Raeder J. High-volume local infiltration analgesia combined with intravenous or local ketorolac+morphine compared with epidural analgesia after total knee arthroplasty. Br J Anaesth 2010;105:675-82.
- Thorsell M, Holst P, Hyldahl HC, Weidenhielm L. Pain control after total knee arthroplasty: a prospective study comparing local infiltration anesthesia and epidural anesthesia. Orthopedics 2010;33:75-80.
- Sharma S, Iorio R, Specht LM, Davies-Lepie S, Healy WL. Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res 2010:135-40.
- Charalambides C, Beer M, Melhuish J, Williams RJ, Cobb AG. Bandaging technique after knee replacement. Acta Orthop 2005;76:89-94.
- Andersen KV, Pfeiffer-Jensen M, Haraldsted V, Soballe K. Reduced hospital stay and narcotic consumption, and improved mobilization with local and intraarticular infiltration after hip arthroplasty: a randomized clinical trial of an intraarticular technique versus epidural infusion in 80 patients. Acta Orthop 2007;78:180-6.
- Andersen LJ, Poulsen T, Krogh B, Nielsen T. Postoperative analgesia in total hip arthroplasty: a randomized double-blinded, placebo-controlled study on peroperative and postoperative ropivacaine, ketorolac, and adrenaline wound infiltration. Acta Orthop 2007;78:187-92.
- Busch CA, Whitehouse MR, Shore BJ, MacDonald SJ, McCalden RW, Bourne RB. The efficacy of periarticular multimodal drug infiltration in total hip arthroplasty. Clin Orthop Relat Res 2010:2152-9.
- Kardash KJ, Sarrazin F, Tessler MJ, Velly AM. Single-dose dexamethasone reduces dynamic pain after total hip arthroplasty. Anesth Analg 2008;106:1253-7, table.
- Kehlet H. Glucocorticoids for peri-operative analgesia: how far are we from general recommendations?. Acta Anaesthesiol Scand 2007;51:1133-5.
- Lunn TH, Kristensen BB, Andersen LO, Husted H, Otte KS, Gaarn-Larsen L, . Effect of high-dose preoperative methylprednisolone on pain and recovery after total knee arthroplasty: a randomized, placebo-controlled trial. Br J Anaesth 2011;106:230-8.
- Meunier A, Lisander B, Good L. Effects of celecoxib on blood loss, pain, and recovery of function after total knee replacement: a randomized placebo-controlled trial. Acta Orthop 2007;78:661-7.
- Ritter MA, Koehler M, Keating EM, Faris PM, Meding JB. Intra-articular morphine and/or bupivacaine after total knee replacement. J Bone Joint Surg Br 1999;81:301-3.
- Romundstad L, Breivik H, Niemi G, Helle A, Stubhaug A. Methylprednisolone intravenously 1 day after surgery has sustained analgesic and opioid-sparing effects. Acta Anaesthesiol Scand 2004;48:1223-31.
- Bergeron SG, Kardash KJ, Huk OL, Zukor DJ, Antoniou J. Perioperative dexamethasone does not affect functional outcome in total hip arthroplasty. Clin Orthop Relat Res 2009;467:1463-7.
- Nikolajsen L, Brandsborg B, Lucht U, Jensen TS, Kehlet H. Chronic pain following total hip arthroplasty: a nationwide questionnaire study. Acta Anaesthesiol Scand 2006;50:495-500.
- Clarke H, Kay J, Mitsakakis N, Katz J. Acute pain after total hip arthroplasty does not predict the development of chronic postsurgical pain 6 months later. J Anesth 2010;24:537-43.
- Puolakka PA, Rorarius MG, Roviola M, Puolakka TJ, Nordhausen K, Lindgren L. Persistent pain following knee arthroplasty. Eur J Anaesthesiol 2010;27:455-60.
- Kupers R, Schneider FC, Christensen R, Naert A, Husted H, Paulson OB, . No evidence for generalized increased postoperative responsiveness to pain: a combined behavioral and serial functional magnetic resonance imaging study. Anesth Analg 2009;109:600-6.
- Aasvang EK, Gmaehle E, Hansen JB, Gmaehle B, Forman JL, Schwarz J, . Predictive risk factors for persistent postherniotomy pain. Anesthesiology 2010;112:957-69.
- Werner MU, Mjobo HN, Nielsen PR, Rudin A. Prediction of postoperative pain: a systematic review of predictive experimental pain studies. Anesthesiology 2010;112:1494-502.
- Kim YH, Kim JS. The 2007 John Charnley Award. Factors leading to low prevalence of DVT and pulmonary embolism after THA: analysis of genetic and prothrombotic factors. Clin Orthop Relat Res 2007; (33-9.
- Edmonds MJ, Crichton TJ, Runciman WB, Pradhan M. Evidence-based risk factors for postoperative deep vein thrombosis. ANZ J Surg 2004;74:1082-97.
- Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van ZA, Sage D, Futter M, Saville G, Clark T, MacMahon S. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ 2000;321:1493.
- Holte K, Kristensen BB, Valentiner L, Foss NB, Husted H, Kehlet H. Liberal versus restrictive fluid management in knee arthroplasty: a randomized, double-blind study. Anesth Analg 2007;105:465-74.
- Pearse EO, Caldwell BF, Lockwood RJ, Hollard J. Early mobilisation after conventional knee replacement may reduce the risk of postoperative venous thromboembolism. J Bone Joint Surg Br 2007;89:316-22.
- Sharrock NE, Gonzalez D.V, Go G, Lyman S, Salvati EA. Potent anticoagulants are associated with a higher all-cause mortality rate after hip and knee arthroplasty. Clin Orthop Relat Res 2008:714-21.
- Eriksson BI, Friedman RJ, Cushner FD, Lassen MR. Potent anticoagulants are associated with a higher all-cause mortality rate after hip and knee arthroplasty. Clin Orthop Relat Res 2008:2009-11.
- Sheth NP, Lieberman JR, Della Valle CJ. DVT prophylaxis in total joint reconstruction. Orthop Clin North Am 2010;41:273-80.
- Cusick LA, Beverland DE. The incidence of fatal pulmonary embolism after primary hip and knee replacement in a consecutive series of 4253 patients. J Bone Joint Surg Br 2009;91:645-8.
- Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, . Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008;133:381S-453S.
- Lachiewicz PF, Comparison of ACCP and AAOS guidelines for VTE prophylaxis after total hip and total knee arthroplasty. Orthopedics 2009;32:74-8.
- Weber KL, Zuckerman JD, Watters WC. III, Turkelson CM. Deep vein thrombosis prophylaxis. Chest 2009;136:1699-700.
- Eikelboom JW, Karthikeyan G, Fagel N, Hirsh J. American Association of Orthopedic Surgeons and American College of Chest Physicians guidelines for venous thromboembolism prevention in hip and knee arthroplasty differ: what are the implications for clinicians and patients? Chest 2009;135:513-20.
- Parvizi J, Jacovides CL, Bican O, Purtill JJ, Sharkey PF, Hozack WJ, . Is deep vein thrombosis a good proxy for pulmonary embolus?. J Arthroplasty 2010;25:138-44.
- Nikolaou VS, Desy NM, Bergeron SG, Antoniou J. Total knee replacement and chemical thromboprophylaxis: current evidence. Curr Vasc Pharmacol 2011;9:33-41.
- Kim YH, Oh SH, Kim JS. Incidence and natural history of deep-vein thrombosis after total hip arthroplasty. A prospective and randomised clinical study. J Bone Joint Surg Br 2003;85:661-5.
- Kim YH, Kim JS. Incidence and natural history of deep-vein thrombosis after total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br 2002;84:566-70.
- Salvati EA, Sharrock NE, Westrich G, Potter HG, Valle AG, Sculco TP. The 2007 ABJS Nicolas Andry Award: three decades of clinical, basic, and applied research on thromboembolic disease after THA: rationale and clinical results of a multimodal prophylaxis protocol. Clin Orthop Relat Res 2007; (246-54.
- Xing KH, Morrison G, Lim W, Douketis J, Odueyungbo A, Crowther M. Has the incidence of deep vein thrombosis in patients undergoing total hip/knee arthroplasty changed over time? A systematic review of randomized controlled trials. Thromb Res 2008;123:24-34.
- Mantilla CB, Horlocker TT, Schroeder DR, Berry DJ, Brown DL. Frequency of myocardial infarction, pulmonary embolism, deep venous thrombosis, and death following primary hip or knee arthroplasty. Anesthesiology 2002;96:1140-6.
- Lachiewicz PF, Soileau ES. Mechanical calf compression and aspirin prophylaxis for total knee arthroplasty. Clin Orthop Relat Res 2007:61-4.
- Lachiewicz PF, Soileau ES. Multimodal prophylaxis for THA with mechanical compression. Clin Orthop Relat Res 2006:225-30.
- Lassen MR, Ageno W, Borris LC, Lieberman JR, Rosencher N, Bandel TJ, . Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N Engl J Med 2008;358:2776-86.
- Blom A, Pattison G, Whitehouse S, Taylor A, Bannister G. Early death following primary total hip arthroplasty: 1,727 procedures with mechanical thrombo-prophylaxis. Acta Orthop 2006;77:347-50.
- Tarity TD, Herz AL, Parvizi J, Rothman RH. Ninety-day mortality after hip arthroplasty: a comparison between unilateral and simultaneous bilateral procedures. J Arthroplasty 2006;21:60-4.
- Samama CM, Ravaud P, Parent F, Barre J, Mertl P, Mismetti P. Epidemiology of venous thromboembolism after lower limb arthroplasty: the FOTO study. J Thromb Haemost 2007;5:2360-7.
- Aynardi M, Pulido L, Parvizi J, Sharkey PF, Rothman RH. Early mortality after modern total hip arthroplasty. Clin Orthop Relat Res 2009:213-18.
- Lassen MR, Raskob GE, Gallus A, Pineo G, Chen D, Portman RJ. Apixaban or enoxaparin for thromboprophylaxis after knee replacement. N Engl J Med 2009;361:594-604.
- Benoni G, Fredin H. Fibrinolytic inhibition with tranexamic acid reduces blood loss and blood transfusion after knee arthroplasty: a prospective, randomised, double-blind study of 86 patients. J Bone Joint Surg Br 1996;78:434-40.
- Husted H, Blond L, Sonne-Holm S, Holm G, Jacobsen TW, Gebuhr P. Tranexamic acid reduces blood loss and blood transfusions in primary total hip arthroplasty: a prospective randomized double-blind study in 40 patients. Acta Orthop Scand 2003;74:665-9.
- Dahl OE, Gudmundsen TE, Bjornara BT, Solheim DM. Risk of clinical pulmonary embolism after joint surgery in patients receiving low-molecular-weight heparin prophylaxis in hospital: a 10-year prospective register of 3,954 patients. Acta Orthop Scand 2003;74:299-304.
- Cundiff DK. Clinical evidence for rebound hypercoagulability after discontinuing oral anticoagulants for venous thromboembolism. Medscape J Med 2008;10:258.
- Eikelboom JW, Quinlan DJ, O’Donnell M. Major bleeding, mortality, and efficacy of fondaparinux in venous thromboembolism prevention trials. Circulation 2009;120:2006-11.
- Wolf O, Mattsson P, Milbrink J, Larsson S, Mallmin H, A randomized study using DXA and RSA in 38 patients followed for 5 years. Acta Orthop 2010;81:286-91.
- Hol AM, van GS, Lucas C, van Susante JL, van Loon CJ. Partial versus unrestricted weight bearing after an uncemented femoral stem in total hip arthroplasty: recommendation of a concise rehabilitation protocol from a systematic review of the literature. Arch Orthop Trauma Surg 2010;130:547-55.
- Holm B. Kehlet H. [Rehabilitation after total knee arthroplasty]. Ugeskr Laeger 2009;171:691-4.
- Minns Lowe CJ, Barker KL, Dewey ME, Sackley CM. Effectiveness of physiotherapy exercise following hip arthroplasty for osteoarthritis: a systematic review of clinical trials. BMC Musculoskelet Disord 2009;10:98.
- Minns Lowe CJ, Barker KL, Dewey M, Sackley CM. Effectiveness of physiotherapy exercise after knee arthroplasty for osteoarthritis: systematic review and meta-analysis of randomised controlled trials. BMJ 2007;335:812.
- Lenssen AF, Crijns YH, Waltje EM, van Steyn MJ, Geesink RJ, van den Brandt PA, . Efficiency of immediate postoperative inpatient physical therapy following total knee arthroplasty: an RCT. BMC Musculoskelet Disord 2006;7:71.
- Ackerman IN, Bennell KL. Does pre-operative physiotherapy improve outcomes from lower limb joint replacement surgery? A systematic review. Aust J Physiother 2004;50:25-30.
- Ferrara PE, Rabini A, Maggi L, Piazzini DB, Logroscino G, Magliocchetti G, . Effect of pre-operative physiotherapy in patients with end-stage osteoarthritis undergoing hip arthroplasty. Clin Rehabil 2008;22:977-86.
- Brower RG. Consequences of bed rest. Crit Care Med 2009;37:S422-8.
- Allen C, Glasziou P, Del MC. Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet 1999;354:1229-33.
- Lenssen TA, van Steyn MJ, Crijns YH, Waltje EM, Roox GM, Geesink RJ, . Effectiveness of prolonged use of continuous passive motion (CPM), as an adjunct to physiotherapy, after total knee arthroplasty. BMC Musculoskelet Disord 2008;9:60.
- Harvey LA, Brosseau L, Herbert RD. Continuous passive motion following total knee arthroplasty in people with arthritis. Cochrane Database Syst Rev 2010; CD004260.
- Saleh KJ, Lee LW, Gandhi R, Ingersoll CD, Mahomed NN, Sheibani-Rad S, . Quadriceps strength in relation to total knee arthroplasty outcomes. Instr Course Lect 2010;59:119-30.
- Holm B, Kristensen MT, Husted H, Kehlet H, Bandholm T. Thigh and knee circumference, knee extension strength, and functional performance following fast-track hip arthroplasty. PM R 2011;3:117-24; quiz 124.
- Mizner RL, Petterson SC, Stevens JE, Vandenborne K, Snyder-Mackler L. Early quadriceps strength loss after total knee arthroplasty. The contributions of muscle atrophy and failure of voluntary muscle activation. J Bone Joint Surg Am 2005;87:1047-53.
- Holm B, Kristensen MT, Myhrmann L, Husted H, Andersen LO, Kristensen B, . The role of pain for early rehabilitation in fast track total knee arthroplasty. Disabil Rehabil 2010;32:300-6.
- Holm B, Kristensen MT, Bencke J, Husted H, Kehlet H, Bandholm T. Loss of knee-extension strength is related to knee swelling after total knee arthroplasty. Arch Phys Med Rehabil 2010;91:1770-6.
- Piva SR, Teixeira PE, Almeida GJ, Gil AB, Digioia AM. III, Levison TJ, Fitzgerald GK. Contribution of hip abductor strength to physical function in patients with total knee arthroplasty. Phys Ther 2011;91:225-33.
- Sled EA, Khoja L, Deluzio KJ, Olney SJ, Culham EG. Effect of a home program of hip abductor exercises on knee joint loading, strength, function, and pain in people with knee osteoarthritis: a clinical trial. Phys Ther 2010;90:895-904.
- Tugay N, Akarcali I, Kaya D, Tugay BU, Atilla B, Tokgozoglu AM. High independence level in functional activities reduces hospital stay after total hip arthroplasty regardless of pain intensity. Saudi Med J 2004;25:1382-7.
- Husted H, Holm G. Fast track in total hip and knee arthroplasty--experiences from Hvidovre University Hospital, Denmark. Injury 2006;37:Suppl 5: S31-S35.
- Husted H, Solgaard S, Hansen TB, Soballe K, Kehlet H. Care principles at four fast-track arthroplasty departments in Denmark. Dan Med Bull 2010;57:A4166.
- Ilfeld BM, Mariano ER, Girard PJ, Loland VJ, Meyer RS, Donovan JF, . A multicenter, randomized, triple-masked, placebo-controlled trial of the effect of ambulatory continuous femoral nerve blocks on discharge-readiness following total knee arthroplasty in patients on general orthopaedic wards. Pain 2010;150:477-84.
- Davies DM, Johnston DW, Beaupre LA, Lier DA. Effect of adjunctive range-of-motion therapy after primary total knee arthroplasty on the use of health services after hospital discharge. Can J Surg 2003;46:30-6.
- Mauerhan DR, Mokris JG, Ly A, Kiebzak GM. Relationship between length of stay and manipulation rate after total knee arthroplasty. J Arthroplasty 1998;13:896-900.
- Schneider M, Kawahara I, Ballantyne G, McAuley C, Macgregor K, Garvie R, . Predictive factors influencing fast track rehabilitation following primary total hip and knee arthroplasty. Arch Orthop Trauma Surg 2009;129:1585-91.
- Husted H, Holm G. Sonne-Holm S. [Accelerated course: high patient satisfaction and four days’ hospitalisation in unselected patients with total hip and knee arthroplasty]. Ugeskr Laeger 2005;167:2043-8.
- Husted H, Holm G. Sonne-Holm S. [A small number of patient characteristics influence the length of hospital stay after total hip and knee arthroplasty]. Ugeskr Laeger 2004;166:3197-201.
- Husted H, Holm G. Sonne-Holm S. [Reduced length of hospital stay after total hip and knee arthroplasty without increased utilization of other resources]. Ugeskr Laeger 2004;166:3194-7.
- Husted H, Otte KS, Kristensen BB, Orsnes T, Kehlet H. Readmissions after fast-track hip and knee arthroplasty. Arch Orthop Trauma Surg 2010;130:1185-91.
- Husted H, Hansen HC, Holm G, Bach-Dal C, Rud K, Andersen KL. Kehlet H. [Length of stay in total hip and knee arthroplasty in Danmark I: volume, morbidity, mortality and resource utilization. A national survey in orthopaedic departments in Denmark]. Ugeskr Laeger 2006;168:2139-43.
- Husted H, Hansen HC, Holm G, Bach-Dal C, Rud K, Andersen KL. Kehlet H. [Accelerated versus conventional hospital stay in total hip and knee arthroplasty III: patient satisfaction]. Ugeskr Laeger 2006;168:2148-51.
- Husted H, Hansen HC, Holm G, Bach-Dal C, Rud K, Andersen KL, . What determines length of stay after total hip and knee arthroplasty? A nationwide study in Denmark. Arch Orthop Trauma Surg 2010;130:263-8.
- Husted H, Hansen HC, Holm G, Bach-Dal C, Rud K, Andersen KL. Kehlet H. [Accelerated versus conventional hospital stay in total hip and knee arthroplasty II: organizational and clinical differences]. Ugeskr Laeger 2006;168:2144-8.
- Husted H, Otte KS, Kristensen BB, Orsnes T, Wong C, Kehlet H. Low risk of thromboembolic complications after fast-track hip and knee arthroplasty. Acta Orthop 2010;81:599-605.
- Andersen SH, Husted H. Kehlet H. [Economic consequences of accelerated care pathways in total knee-arthroplasty]. Ugeskr Laeger 2009;171:3276-80.
- Barbieri A, Vanhaecht K, Van HP, Sermeus W, Faggiano F, Marchisio S, . Effects of clinical pathways in the joint replacement: a meta-analysis. BMC Med 2009;7:32.
- Wammack L, Mabrey JD. Outcomes assessment of total hip and total knee arthroplasty: critical pathways, variance analysis, and continuous quality improvement. Clin Nurse Spec 1998;12:122-9.
- Renkawitz T, Rieder T, Handel M, Koller M, Drescher J, Bonnlaender G, . Comparison of two accelerated clinical pathways--after total knee replacement how fast can we really go?. Clin Rehabil 2010;24:230-9.
- Saufl N, Owens A, Kelly I, Merrill B, Freyaldenhouen LL. A multidisciplinary approach to total joint replacement. J Perianesth Nurs 2007;22:195-206.
- Khan F, Ng L, Gonzalez S, Hale T, Turner-Stokes L. Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy. Cochrane Database Syst Rev 2008; CD004957.
- Kim DM, Brecher ME, Estes TJ, Morrey BF. Relationship of hemoglobin level and duration of hospitalization after total hip arthroplasty: implications for the transfusion target. Mayo Clin Proc 1993;68:37-41.
- Wang T, Ackland T, Hall S, Gilbey H, Parsons R. Functional recovery and timing of hospital discharge after primary total hip arthroplasty. Aust N Z J Surg 1998;68:580-3.
- Hayes JH, Cleary R, Gillespie WJ, Pinder IM, Sher JL. Are clinical and patient assessed outcomes affected by reducing length of hospital stay for total hip arthroplasty?. J Arthroplasty 2000;15:448-52.
- Styron JF, Koroukian SM, Klika AK, Barsoum WK. Patient vs Provider Characteristics Impacting Hospital Lengths of Stay After Total Knee or Hip Arthroplasty. J Arthroplasty 2011.
- Watkins JR, Bryan S, Muris NM, Buxton MJ. Examining the influence of picture archiving communication systems and other factors upon the length of stay for patients with total hip and total knee replacements. Int J Technol Assess Health Care 1999;15:497-505.
- Rissanen P, Aro S, Paavolainen P. Hospital- and patient-related characteristics determining length of hospital stay for hip and knee replacements. Int J Technol Assess Health Care 1996;12:325-35.
- Wasielewski RC, Weed H, Prezioso C, Nicholson C, Puri RD. Patient comorbidity: relationship to outcomes of total knee arthroplasty. Clin Orthop Relat Res 1998:85-92.
- Gandhi R, Razak F, Davey JR, Rampersaud YR, Mahomed NN. Effect of sex and living arrangement on the timing and outcome of joint replacement surgery. Can J Surg 2010;53:37-41.
- Berwick DM. Developing and testing changes in delivery of care. Ann Intern Med 1998;128:651-6.
- SooHoo NF, Lieberman JR, Ko CY, Zingmond DS. Factors predicting complication rates following total knee replacement. J Bone Joint Surg Am 2006;88:480-5.
- SooHoo NF, Farng E, Lieberman JR, Chambers L, Zingmond DS. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop Relat Res 2010:2363-71.
- Forsythe ME, Dunbar MJ, Hennigar AW, Sullivan MJ, Gross M. Prospective relation between catastrophizing and residual pain following knee arthroplasty: two-year follow-up. Pain Res Manag 2008;13:335-41.
- Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, . Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg 2008;51:428-36.
- Husted H, Troelsen A. Kehlet H. [Undocumented regimes after total hip and knee arthroplasty can deteriorate the results.]. Ugeskr Laeger 2011;173:1802-5.
- Schindler OS, Spencer RF, Smith MD. Should we use a separate knife for the skin?. J Bone Joint Surg Br 2006;88:382-5.
- Tanner J, Woodings D, Moncaster K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev 2006; 3: CD004122.
- Webster J, Alghamdi AA. Use of plastic adhesive drapes during surgery for preventing surgical site infection. Cochrane Database Syst Rev 2007; CD006353.
- Parker MJ, Roberts CP, Hay D. Closed suction drainage for hip and knee arthroplasty. A meta-analysis. J Bone Joint Surg Am 2004; 86-A: 1146-1152.
- Balderi T, Carli F. Urinary retention after total hip and knee arthroplasty. Minerva Anestesiol 2010;76:120-30.
- Smith TO, Blake V, Hing CB. Minimally invasive versus conventional exposure for total hip arthroplasty: a systematic review and meta-analysis of clinical and radiological outcomes. Int Orthop 2011;35:173-84.
- Smith TO, King JJ, Hing CB. A meta-analysis of randomised controlled trials comparing the clinical and radiological outcomes following minimally invasive to conventional exposure for total knee arthroplasty. Knee 2010.
- Cheng T, Liu T, Zhang G, Peng X, Zhang X. Does minimally invasive surgery improve short-term recovery in total knee arthroplasty?. Clin Orthop Relat Res 2010:1635-48.
- Smith TO, Hing CB. Is a tourniquet beneficial in total knee replacement surgery? A meta-analysis and systematic review. Knee 2010;17:141-7.
- Li B, Wen Y, Wu H, Qian Q, Lin X, Zhao H. The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop 2009;33:1263-8.
- Husted H, Toftgaard JT. Influence of the pneumatic tourniquet on patella tracking in total knee arthroplasty: a prospective randomized study in 100 patients. J Arthroplasty 2005;20:694-7.
- Worland RL, Arredondo J, Angles F, Lopez-Jimenez F, Jessup DE. Thigh pain following tourniquet application in simultaneous bilateral total knee replacement arthroplasty. J Arthroplasty 1997;12:848-52.
- Takada M, Fukusaki M, Terao Y, Yamashita K, Inadomi C, Takada M, . Preadministration of flurbiprofen suppresses prostaglandin production and postoperative pain in orthopedic patients undergoing tourniquet inflation. J Clin Anesth 2007;19:97-100.
- Meunier A, Aspenberg P, Good L. Celecoxib does not appear to affect prosthesis fixation in total knee replacement: A randomized study using radiostereometry in 50 patients. Acta Orthop 2009;80:46-50.
- Meunier A, Lisander B, Good L. Effects of celecoxib on blood loss, pain, and recovery of function after total knee replacement: a randomized placebo-controlled trial. Acta Orthop 2007;78:661-7.
- Moiniche S, Kehlet H, Dahl JB. A qualitative and quantitative systematic review of preemptive analgesia for postoperative pain relief: the role of timing of analgesia. Anesthesiology 2002;96:725-41.
- Matziolis D, Perka C, Hube R. Matziolis G. [Influence of tourniquet ischemia on perioperative blood loss after total knee arthroplasty.]. Orthopade 2011;40:178-82.
- Levy O, Martinowitz U, Oran A, Tauber C, Horoszowski H. The use of fibrin tissue adhesive to reduce blood loss and the need for blood transfusion after total knee arthroplasty. A prospective, randomized, multicenter study. J Bone Joint Surg Am 1999;81:1580-8.
- Marulanda GA, Krebs VE, Bierbaum BE, Goldberg VM, Ries M, Ulrich SD, . Hemostasis using a bipolar sealer in primary unilateral total knee arthroplasty. Am J Orthop (Belle Mead NJ) 2009;38:E179-83.
- Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 2004; 86-A: 963-974.
- Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, . The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol 2002;29:1273-9.
- Scott CE, Howie CR, Macdonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br 2010;92:1253-8.
- Gandhi R, Davey JR, Mahomed NN. Predicting patient dissatisfaction following joint replacement surgery. J Rheumatol 2008;35:2415-18.
- Baumann C, Rat AC, Osnowycz G, Mainard D, Cuny C, Guillemin F. Satisfaction with care after total hip or knee replacement predicts self-perceived health status after surgery. BMC Musculoskelet Disord 2009;10:150.
- Williams A, Dunning T, Manias E. Continuity of care and general wellbeing of patients with comorbidities requiring joint replacement. J Adv Nurs 2007;57:244-56.
- Merle-Vincent F, Couris CM, Schott AM, Conrozier T, Piperno M, Mathieu P, . Factors predicting patient satisfaction 2 years after total knee arthroplasty for osteoarthritis. Joint Bone Spine 2011;78:383-6.
- Wylde V, Dieppe P, Hewlett S, Learmonth ID. Total knee replacement: is it really an effective procedure for all?. Knee 2007;14:417-23.
- Judge A, Cooper C, Williams S, Dreinhoefer K, Dieppe P. Patient-reported outcomes one year after primary hip replacement in a European Collaborative Cohort. Arthritis Care Res (Hoboken ) 2010;62:480-8.
- Hepinstall MS, Rutledge JR, Bornstein LJ, Mazumdar M, Westrich GH. Factors that impact expectations before total knee arthroplasty. J Arthroplasty 2011;26:870-6.
- Lingard EA, Sledge CB, Learmonth ID. Patient expectations regarding total knee arthroplasty: differences among the United States, United kingdom, and Australia. J Bone Joint Surg Am 2006;88:1201-7.
- McGregor AH, Rylands H, Owen A, Dore CJ, Hughes SP. Does preoperative hip rehabilitation advice improve recovery and patient satisfaction?. J Arthroplasty 2004;19:464-8.
- Sharkey PF, Miller AJ. Noise, numbness, and kneeling difficulties after total knee arthroplasty: is the outcome affected?. J Arthroplasty 2011;26:1427-31.
- Van HP, Vanhaecht K, Deneckere S, Bellemans J, Panella M, Barbieri A, . Key interventions and outcomes in joint arthroplasty clinical pathways: a systematic review. J Eval Clin Pract 2010;16:39-49.
- Husted H, Holm G, Rud K, Bach-Dal C, Hansen HC, Andersen KL. Kehlet H. [Length of stay after primary total hip and knee arthroplasty in Denmark, 2001-2003]. Ugeskr Laeger 2006;168:276-9.
- Rogers BA, Johnstone DJ. Audit on the efficient use of cross-matched blood in elective total hip and total knee replacement. Ann R Coll Surg Engl 2006;88:199-201.
- Mundy GM, Hardiment K, Revill J, Birtwistle SJ, Power RA. Do we really need to routinely crossmatch blood before primary total knee or hip arthroplasty?. Acta Orthop Scand 2004;75:567-72.
- Yasunaga H, Tsuchiya K, Matsuyama Y, Ohe K. Analysis of factors affecting operating time, postoperative complications, and length of stay for total knee arthroplasty: nationwide web-based survey. J Orthop Sci 2009;14:10-16.
- Vanhaecht K, Bellemans J, De WK, Diya L, Lesaffre E, Sermeus W. Does the organization of care processes affect outcomes in patients undergoing total joint replacement?. J Eval Clin Pract 2010;16:121-8.
- Gittell JH, Fairfield KM, Bierbaum B, Head W, Jackson R, Kelly M, . Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine-hospital study of surgical patients. Med Care 2000;38:807-19.
- Schoenfelder T, Klewer J, Kugler J. Factors associated with patient satisfaction in surgery: the role of patients’ perceptions of received care, visit characteristics, and demographic variables. J Surg Res 2010;164:e53-9.
- Howell SM, Rogers SL. Method for quantifying patient expectations and early recovery after total knee arthroplasty. Orthopedics 2009;32:884-90.
- Nilsdotter AK, Toksvig-Larsen S, Roos EM. Knee arthroplasty: are patients’ expectations fulfilled? A prospective study of pain and function in 102 patients with 5-year follow-up. Acta Orthop 2009;80:55-61.
- McDonald S, Hetrick S, Green S. Pre-operative education for hip or knee replacement. Cochrane Database Syst Rev 2004; CD003526.
- Bini SA, Fithian DC, Paxton LW, Khatod MX, Inacio MC, Namba RS. Does discharge disposition after primary total joint arthroplasty affect readmission rates?. J Arthroplasty 2010;25:114-17.
- Phillips CB, Barrett JA, Losina E, Mahomed NN, Lingard EA, Guadagnoli E, . Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg Am 2003; 85-A: 20-26.
- Mauerhan DR, Mokris JG, Ly A, Kiebzak GM. Relationship between length of stay and manipulation rate after total knee arthroplasty. J Arthroplasty 1998;13:896-900.
- Dowsey MM, Kilgour ML, Santamaria NM, Choong PF. Clinical pathways in hip and knee arthroplasty: a prospective randomised controlled study. Med J Aust 1999;170:59-62.
- Pearson S, Moraw I, Maddern GJ. Clinical pathway management of total knee arthroplasty: a retrospective comparative study. Aust N Z J Surg 2000;70:351-4.
- Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am 2007;89:526-33.
- Berger RA, Kusuma SK, Sanders SA, Thill ES, Sporer SM. The feasibility and perioperative complications of outpatient knee arthroplasty. Clin Orthop Relat Res 2009:1443-9.
- Fehringer EV, Mikuls TR, Michaud KD, Henderson WG, O’Dell JR. Shoulder arthroplasties have fewer complications than hip or knee arthroplasties in US veterans. Clin Orthop Relat Res 2010:717-22.
- Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, . Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am 2003; 85-A: 27-32.
- Kwon MS, Kuskowski M, Mulhall KJ, Macaulay W, Brown TE, Saleh KJ. Does surgical approach affect total hip arthroplasty dislocation rates?. Clin Orthop Relat Res 2006:34-8.
- Mauerhan DR, Lonergan RP, Mokris JG, Kiebzak GM. Relationship between length of stay and dislocation rate after total hip arthroplasty. J Arthroplasty 2003;18:963-7.
- Restrepo C, Mortazavi SM, Brothers J, Parvizi J, Rothman RH. Hip dislocation: are hip precautions necessary in anterior approaches?. Clin Orthop Relat Res 2011:417-22.
- Lombardi AV Jr, Skeels MD, Berend KR, Adams JB, Franchi OJ. Do large heads enhance stability and restore native anatomy in primary total hip arthroplasty?. Clin Orthop Relat Res 2011:1547-53.
- Everts PA, Devilee RJ, Oosterbos CJ, Mahoney CB, Schattenkerk ME, Knape JT, van ZA. Autologous platelet gel and fibrin sealant enhance the efficacy of total knee arthroplasty: improved range of motion, decreased length of stay and a reduced incidence of arthrofibrosis. Knee Surg Sports Traumatol Arthrosc 2007;15:888-94.
- Restrepo C, Parvizi J, Dietrich T, Einhorn TA. Safety of simultaneous bilateral total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am 2007;89:1220-6.
- Stefansdottir A, Lidgren L, Robertsson O. Higher early mortality with simultaneous rather than staged bilateral TKAs: results from the Swedish Knee Arthroplasty Register. Clin Orthop Relat Res 2008:3066-70.
- Memtsoudis SG, Gonzalez D. V, Besculides MC, Gaber L, Sculco TP. In-hospital complications and mortality of unilateral, bilateral, and revision TKA: based on an estimate of 4,159,661 discharges. Clin Orthop Relat Res 2008:2617-27.
- Kim YH, Choi YW, Kim JS. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br 2009;91:64-8.
- Berend KR, Lombardi AV. Jr., Adams JB. Simultaneous vs staged cementless bilateral total hip arthroplasty: perioperative risk comparison. J Arthroplasty 2007;22:111-15.
- Kim YH, Kwon OR, Kim JS. Is one-stage bilateral sequential total hip replacement as safe as unilateral total hip replacement?. J Bone Joint Surg Br 2009;91:316-20.
- Otte KS, Husted H, Ørsnes T, Kehlet H. Bilateral simultaneous total hip arthroplasty in a fast-track setting. Hip Int 2011;21:336-9.
- Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, . The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 2010:45-51.
- Healy WL, Ayers ME, Iorio R, Patch DA, Appleby D, Pfeifer BA. Impact of a clinical pathway and implant standardization on total hip arthroplasty: a clinical and economic study of short-term patient outcome. J Arthroplasty 1998;13:266-76.
- Macario A, Horne M, Goodman S, Vitez T, Dexter F, Heinen R, . The effect of a perioperative clinical pathway for knee replacement surgery on hospital costs. Anesth Analg 1998;86:978-84.
- Metz CM, Freiberg AA. An international comparative study of total hip arthroplasty cost and practice patterns. J Arthroplasty 1998;13:296-8.
- Brunenberg DE, van Steyn MJ, Sluimer JC, Bekebrede LL, Bulstra SK, Joore MA. Joint recovery programme versus usual care: an economic evaluation of a clinical pathway for joint replacement surgery. Med Care 2005;43:1018-26.
- Taheri PA, Butz DA, Greenfield LJ. Length of stay has minimal impact on the cost of hospital admission. J Am Coll Surg 2000;191:123-30.
- Bryant DM, Willits K, Hanson BP. Principles of designing a cohort study in orthopaedics. J Bone Joint Surg Am 2009;91:Suppl 3: 10-14.
- Werner MU, Duun P, Kehlet H. Prediction of postoperative pain by preoperative nociceptive responses to heat stimulation. Anesthesiology 2004;100:115-19.
- Bundgaard-Nielsen M, Jorgensen CC, Jorgensen TB, Ruhnau B, Secher NH, Kehlet H. Orthostatic intolerance and the cardiovascular response to early postoperative mobilization. Br J Anaesth 2009;102:756-62.