Abstract
Background and purpose The effects of patient-related and technical factors on the risk of revision due to dislocation after primary total hip arthroplasty (THA) are only partly understood. We hypothesized that increasing the femoral head size can reduce this risk, that the lateral surgical approach is associated with a lower risk than the posterior and minimally invasive approaches, and that gender and diagnosis influence the risk of revision due to dislocation.
Patients and methods Data on 78,098 THAs in 61,743 patients performed between 2005 and 2010 were extracted from the Swedish Hip Arthroplasty Register. Inclusion criteria were a head size of 22, 28, 32, or 36 mm, or the use of a dual-mobility cup. The covariates age, sex, primary diagnosis, type of surgical approach, and head size were entered into Cox proportional hazards models in order to calculate the adjusted relative risk (RR) of revision due to dislocation, with 95% confidence intervals (CI).
Results After a mean follow-up of 2.7 (0–6) years, 399 hips (0.5%) had been revised due to dislocation. The use of 22-mm femoral heads resulted in a higher risk of revision than the use of 28-mm heads (RR = 2.0, CI: 1.2–3.3). Only 1 of 287 dual-mobility cups had been revised due to dislocation. Compared with the direct lateral approach, minimally invasive approaches were associated with a higher risk of revision due to dislocation (RR = 4.2, CI: 2.3–7.7), as were posterior approaches (RR = 1.3, CI: 1.1–1.7). An increased risk of revision due to dislocation was found for the diagnoses femoral neck fracture (RR = 3.9, CI: 3.1–5.0) and osteonecrosis of the femoral head (RR = 3.7, CI: 2.5–5.5), whereas women were at lower risk than men (RR = 0.8, CI: 0.7–1.0). Restriction of the analysis to the first 6 months after the index procedure gave similar risk estimates.
Interpretation Patients with femoral neck fracture or osteonecrosis of the femoral head are at higher risk of dislocation. Use of the minimally invasive and posterior approaches also increases this risk, and we raise the question of whether patients belonging to risk groups should be operated using lateral approaches. The use of femoral head diameters above 28 mm or of dual-mobility cups reduced this risk in a clinically relevant manner, but this observation was not statistically significant.
Dislocation remains a major problem after primary total hip arthroplasty (THA), and has a considerably negative effect on the quality of life after THA, especially if it is recurrent (Enocson et al. Citation2009b). Revision due to dislocation accounts for 9% of all revisions of primary THAs in the Swedish Hip Arthroplasty Register (SHAR), and it is therefore the second most common reason for revision after aseptic loosening (CitationSHAR Annual Report 2010). An even higher proportion of revisions due to dislocation—of 26%—has been reported by the Australian National Joint Replacement Registry (2011). Most dislocations occur during the first postoperative year, and up to 50% take place within the first 3 months (Woo and Morrey Citation1982, Phillips et al. Citation2003, Meek et al. Citation2006). The Norwegian Joint Register reported that the number of revisions performed due to dislocation has increased over time, possibly related to changes in head sizes and surgical approaches during the study period (Fevang et al. Citation2010).
Several factors have been proposed to influence the risk of dislocation, but many questions still remain unsolved (Meek et al. Citation2006). Various diagnoses such as femoral neck fracture (Conroy et al. Citation2008), the posterior approach to the joint, and small femoral head size of the prosthesis are parameters that have been identified as risk factors for dislocation (Furnes et al. Citation2001, Bystrom et al. Citation2003, Berry et al. Citation2005, Lachiewicz and Soileau Citation2006, Enocson et al. Citation2009b, Sariali et al. Citation2009, Ji et al. Citation2012).
The use of dual-mobility cups, synonymously termed tripolar cups in primary THA, leads to a low risk of dislocation (Farizon et al. Citation1998, Philippot et al. Citation2009b, Bouchet et al. Citation2011, Boyer et al. Citation2012). Revision surgery of patients with recurrent dislocations by the use of dual-mobility cups has also shown promising results (Langlais et al. Citation2008, Philippot et al. Citation2009a).
We studied the influence of both patient-related and surgical factors on the risk of revision due to dislocation in the Swedish Hip Arthroplasty Register. We hypothesized that age, sex, primary diagnosis underlying THA surgery, femoral head size, and surgical approach can affect the risk of revision due to dislocation. Furthermore, we specifically investigated the effects of dual-mobility cups on the risk of dislocation.
Patients and methods
Data selection
Our data were derived from the Swedish Hip Arthroplasty Register (CitationSHAR Annual Report 2010), initiated in 1979. All public and private orthopedic units report demographic data, laterality, surgical approach, and detailed information on implants and fixation to the Register. The SHAR has been validated, and the completeness has been found to be about 99% for primary THA (CitationSHAR Annual Report 2010) and 94% for revision hip arthroplasties (Söderman Citation2000).
Femoral head sizes above 28 mm and dual-mobility cups have only been in frequent use in Sweden since 2005. Thus, only primary THA procedures registered in the SHAR from January 1, 2005 to December 31, 2010 were extracted. An extension of the selection criteria to earlier time periods would only have resulted in the addition of more head sizes below 28 mm and of more historical cup designs that are no longer in clinical use.
To reduce the influence of cup designs used in small numbers, we included only cups that had been inserted in at least 1,000 hips—with the exception of the dual-mobility design, which had only been used in 287 THAs. In Sweden, this type of cup has only recently been introduced, and, with few exceptions, only one design has been inserted (Avantage; Biomet, Warsaw, IN). Hip resurfacings and implants with rarely used head diameters (24, 26, 30, and 40 mm; n = 140), 20 hips with missing data on head diameter, and 487 hips with uncertain information on the type of surgical approach were excluded. Thus, we identified and analyzed 78,098 procedures in 61,743 patients.
Terminology
The term “revision” was defined as an intervention where 1 or more components of the prosthesis were exchanged, where an augmentation device was added, or where the whole prosthesis was removed. Thus, other types of reoperations in which the implant was left in situ, e.g. closed reductions or incision and drainage, were disregarded.
The covariate “diagnosis” was divided into primary osteoarthritis (pOA), inflammatory joint disease, femoral neck fracture, osteonecrosis of the femoral head (FHN), previous pediatric hip diseases such as developmental dysplasia of the hip, Perthes’ disease and slipped femoral epiphysis, and other diagnoses. The category “other diagnoses” included secondary osteoarthritis due to previous trauma or malignancy. The covariate “surgical approaches” was divided into lateral, posterior, and minimally invasive. The category “lateral approaches” included the approaches described by Hardinge, Gammer, or Bauer, with or without trochanteric osteotomy. “Posterior approaches” included approaches based on the description by Moore, with or without trochanteric osteotomy. “Minimally invasive approaches” included lateral (n = 604), posterior (n = 100), and 2-incision approaches (n =30).
Statistics
Continuous descriptive statistics used means, median values, ranges, and 95% confidence intervals (CIs) where appropriate. Cox proportional hazards models were used to analyze the influence of various covariates on the relative risk (RR) of revision due to dislocation. Follow-up started on the day of primary THA and ended on the day of revision, death, emigration, or December 31, 2010, whichever came first. The covariates age (< 50, 50–59, 60–75, > 75), sex, primary diagnosis, head size (22, 28, 32, 36, dual-mobility) and surgical approach were initially investigated as singular covariates resulting in a crude RR with 95% CI. All covariates mentioned above were subsequently entered into the model, and adjusted RRs were calculated using the Breslow method for handling ties. A separate analysis was performed for the first 6 months after the index procedure. The assumption of proportional hazards was investigated by calculating the correlation coefficient between transformed survival time and the scaled Schoenfeld residuals. The level of significance was set at p < 0.05 in all analyses, and we used the R software package (version 2.14.1).
The inclusion of both joints in bilaterally operated patients does not appear to lead to dependency issues in registry studies of this size, and both joints in bilaterally operated patients were thus included in the analysis (Hailer et al. Citation2010). To confirm these previous observations, separate analyses excluding the second THA in bilaterally operated patients were performed without affecting parameter estimates.
Characteristics of the study population
The population studied consisted of 36,968 females (60%) and 24,775 males. The distribution of age and diagnosis groups is given in and . 35,460 THAs (45%) had been performed using a lateral approach, 41,904 (54%) using a posterior approach, and 734 THAs (1%) had been inserted using minimally invasive approaches. 28 mm was by far the most widely used head diameter (). 71,094 cups (91%) were cemented and 7,004 (9%) were uncemented. 2 different types of Avantage cups had been used: the cemented, polished version (n = 275) and the uncemented, hydroxyapatite-coated version (n = 12). Cross-tabulations for diagnosis or surgical approach by femoral head size are summarized in . The Lubinus cup was the most commonly used acetabular implant (). Cups had been combined with a wide variety of stems, both cemented (n = 64,808; 83%) and uncemented (n = 13,251; 17%, with missing data for 39 stems), creating both cemented, hybrid, and uncemented systems. Mean follow-up time was 2.7 (0–6) years.
Table 1. Age at index THA
Table 2. Diagnosis at index THA
Table 3. Head diameters inserted at index THA
Table 4. Head size by diagnosis or by surgical approach
Table 5. Cup types inserted during index THA
Table 6. Cox regression analysis of risk factors for revision due to dislocation a
Results
Reasons for revision of THA
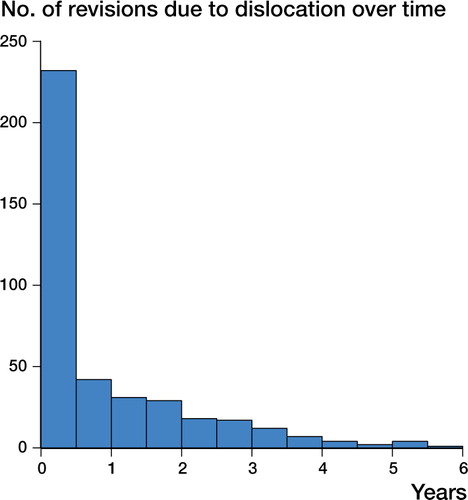
At follow-up 1,302 hips (1.7%) had been revised, 406 (0.5%) due to infection, 399 (0.5%) due to dislocation, 213 (0.3%) due to aseptic loosening, 146 (0.2%) due to periprosthetic fracture, and the remaining 138 (0.2%) for various reasons. Most revisions due to dislocation (n = 274, 69%) were performed during the first postoperative year, and another 60 (15%) occurred during the second postoperative year (). Of all revisions performed during the first postoperative year, revision due to dislocation was the second most common reason after revision due to infection (n = 295).
Risk of revision due to dislocation
In the unadjusted Cox regression analysis, a head diameter of 22 mm was associated with a higher risk of revision due to dislocation than the reference diameter of 28 mm. The diagnoses of femoral neck fracture and femoral head necrosis, and the group of other diagnoses, were associated with an increased risk of revision due to dislocation when compared with the reference category of primary osteoarthritis. Finally, the minimally invasive approaches resulted in a significantly higher risk of revision due to dislocation than the direct lateral approaches ().
All covariates mentioned above were subsequently entered into a multiple regression model and adjusted RRs were calculated (). The use of the smallest head diameter of 22 mm resulted in an increased risk of revision when compared with 28-mm heads (RR = 2.0, 95% CI: 1.2–3.3). We found a reduced risk of revision due to dislocation with increasing head diameter, with the lowest RR being observed for dual-mobility cups (RR = 0.4, CI: 0.1–2.9). This observation was not statistically significant, however. In an exploratory analysis, we found no evidence that the type of cup fixation (cemented or uncemented) influenced the risk of dislocation (data not shown). Moreover, we performed a separate analysis investigating the risk of revision due to dislocation within the first 6 months, but the adjusted risk estimates remained similar to those described for the entire study period (data not shown).
Femoral neck fracture, femoral head necrosis, and the group of other diagnoses were associated with an increased risk of revision due to dislocation. THA performed because of femoral neck fracture had an RR of 3.9 (CI: 3.1–5.0) when compared with hips operated due to primary osteoarthritis. We found an RR of 3.7 (CI: 2.5–5.5) for hips with femoral head necrosis. Hips with inflammatory diseases showed almost the same risk as the group with primary osteoarthritis. In patients with sequelae after pediatric hip diseases, the adjusted RR was higher, but this was not statistically significantly different from the reference group.
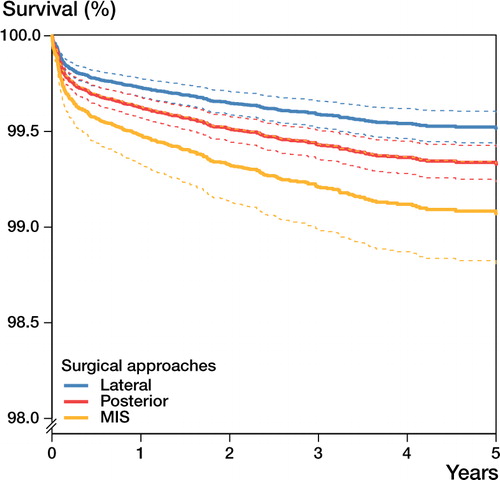
Minimally invasive surgical approaches showed a higher risk of revision due to dislocation than the direct lateral approach after adjustment for covariates (RR = 4.2, CI: 2.3–7.7) (). In the adjusted model, the posterior approaches showed a higher risk of revision due to dislocation than the direct lateral approaches, with an RR of 1.3 (CI: 1.1–1.7).
Figure 2. Survival functions with the endpoint “revision due to dislocation” by surgical approach. A Cox proportional hazards model was used in order to calculate adjusted survival functions with 95% CI (dotted lines) for the 3 surgical approaches lateral (n = 35,460), posterior (n = 41,904), and minimally invasive (n = 734). The endpoint was revision due to dislocation. Survival functions were adjusted for the mean of the covariates gender, age, primary diagnosis, and femoral head size. The lateral approach was associated with the lowest risk of revision due to dislocation.
The demographic covariates age and sex were also entered into the regression model. Age at the time of index THA had no influence on the risk of revision due to dislocation, whereas females had a lower risk than males (RR = 0.8, CI: 0.7–1.0).
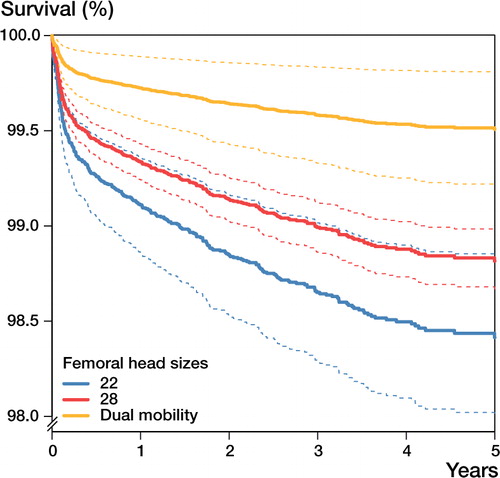
The risk of revision due to dislocation in subgroups of THA found to have a higher than average risk was studied separately. In the group operated because of fracture, for femoral head necrosis, or for other reasons (n = 10,370), 137 (1.3%) had been revised because of dislocation. A dual-mobility cup had been used in 206 of the hips belonging to these risk groups, and, notably, none of these had been revised because of dislocation. The covariates age at index operation, sex, type of surgical approach, and head size were then entered into the regression model with the endpoint “revision due to dislocation”. Factors that influenced the risk of revision due to dislocation in these risk groups were a femoral head size of 22 mm (RR = 2.5, CI: 1.1–5.7; p = 0.03), female sex (RR = 0.5, CI: 0.4–0.7; p < 0.001), the posterior approach (RR = 1.6, CI: 1.2–2.3; p = 0.01) and a minimally invasive approach (RR = 5.0, CI: 1.2–21.1; p = 0.03). The risk of revision due to dislocation was dependent on femoral head size for patients with a femoral neck fracture, and the use of dual-mobility cups was associated with the lowest risk of dislocation ().
Figure 3. Survival functions for patients with a femoral neck fracture with the endpoint “revision due to dislocation” by femoral head size. A Cox proportional hazards model was used to calculate adjusted survival functions with 95% CI (dotted lines) for patients with a femoral head fracture, for the femoral head sizes 22 mm (n = 1,394) and 28 mm (n = 57,194), and dual-mobility cups (n = 287). The endpoint was revision due to dislocation. Survival functions were adjusted for the mean of the covariates gender, age, and surgical approach but fixed for the diagnosis femoral neck fracture. Dual-mobility cups were associated with the lowest risk of revision due to dislocation.
Discussion
Femoral head size
Our findings are largely in accordance with those of previously reported medium-sized cohort studies and registry studies. Data derived from the Norwegian Arthroplasty Register indicated that dislocation rates were lower after the use of 32-mm femoral heads than after the use of 28-mm femoral heads (Bystrom et al. Citation2003). The Charnley stem with a 22-mm head did, however, perform just as well as the group with 28-mm heads, which contradicts our findings. In a cohort study of 2,572 hips that received either 28- or 32-mm femoral heads, a 6-fold increased risk of dislocation was associated with the use of 28-mm heads, but this analysis also included cases treated with closed reduction (Amlie et al. Citation2010). An analysis of almost 248,000 THA procedures from the National Joint Registry for England and Wales suggested that the increasing use of femoral head sizes of 36 mm or larger during the period 2005–2009 was associated with a decrease in the number of dislocations (Jameson et al. Citation2011). In that study, however, no direct link between patients and specific head sizes was investigated. A comparison of 198 consecutive hips operated with 28-mm femoral heads with 259 hips that had received 36-mm femoral heads showed that the risk of dislocation was almost 8-fold in the group with the smaller head size (Bistolfi et al. Citation2011).
Dual-mobility cups have a femoral head component of either 22 mm or 28 mm diameter that moves inside a larger-sized polyethylene liner. The liner moves freely in a metal shell with an inner diameter that corresponds to the outer diameter of the polyethylene liner. The metal shell can be fixed to the acetabular bone by cement or press-fit. Only 1 out of 287 dual-mobility cups investigated in our study was revised due to dislocation, although this implant was mostly used for THA inserted because of femoral neck fracture. It should be kept in mind that the subgroup of dual-mobility cups was small compared to the entire cohort in this study, and a high degree of uncertainty remains. However, taking these limitations into account, we suggest that dual-mobility cups reduce the risk of dislocation in patients with femoral neck fracture and other risk groups to a clinically relevant degree. This is in accordance with other studies. In a case-control study of 213 hips, no dislocations were found in primary THA inserted using a posterior approach, whereas 5 dislocations occurred in patients operated with a conventional 28-mm metal head (Bouchet et al. Citation2011). No dislocations were observed in a series of 150 patients operated with a dual-mobility cup due to primary osteoarthritis, at a mean follow-up of 7 years (Bauchu et al. Citation2008). This cup design can also reduce the risk of dislocation in patients who receive a THA due to femoral neck fracture (Tarasevicius et al. Citation2010).
Surgical approach
The type of surgical approach influences the risk of dislocation after THA, but several points of controversy remain. A retrospective study of 713 hips indicated that patients with a THA inserted due to femoral neck fracture had a higher risk of dislocation after the use of a posterior approach, and a retrospective analysis of 21,047 THA—mostly inserted due to osteoarthritis—showed that the posterior approach was associated with a higher cumulative 10-year risk of dislocation (Berry et al. Citation2005, Enocson et al. Citation2009a). It was also found that the introduction of the anterolateral approach as a routine approach in the treatment of patients with femoral neck fracture reduced the risk of dislocation from 8% to 2% when compared to the previously used posterior approach (Sköldenberg et al. Citation2010). However, the proposed enhanced risk of dislocation associated with posterior approaches has been questioned. A randomized trial comparing a lateral approach and a posterior approach combined with repair of posterior capsule and external rotators found a higher dislocation rate in the group with THAs inserted using a lateral approach (Ji et al. Citation2012).
We found that minimally invasive approaches increase the risk of revision due to dislocation relative to the anterolateral approach. There have been numerous reports on intraoperative and postoperative complications associated with minimally invasive approaches, but we have not found any mention of a higher rate of dislocation in larger cohorts. A higher risk of dislocation following minimally invasive procedures could at least in part be explained by suboptimal cup positioning during minimally invasive surgery (Callanan et al. Citation2011). In that study, the use of minimally invasive approaches increased the risk of cup positioning outside the safe zone by a factor of 6.
It has been suggested that resuturing of the posterior capsule and/or external rotators can reduce the risk of THA dislocation after using a posterior approach. In a retrospective review of 945 THAs inserted using a posterior approach combined with a posterior soft tissue repair, only 8 hips dislocated. However, it is unclear how the authors ascertained completeness of follow-up (Weeden et al. Citation2003). Meticulous external rotator repair was also found to result in only 1 dislocation in 178 THAs, but without comparison with a control group (Browne and Pagnano Citation2012). In contrast, an analysis of 713 THAs indicated that a posterior approach gave a higher risk of dislocation than the lateral approach irrespective of whether or not a posterior soft tissue repair had been performed (Enocson et al. Citation2009a). Our findings support the notion that a posterior approach is indeed associated with a higher risk of dislocation than the lateral approach, but we cannot comment on the possible effects of posterior soft tissue repair since such detailed information is not recorded in the Register.
Diagnosis
Our results on the higher risk of dislocation of hips operated due to femoral neck fracture or idiopathic femoral head necrosis are in partial agreement with an Australian Registry study. In that study, the diagnoses femoral neck fracture and osteonecrosis were associated with increased risk of revision due to dislocation. In contrast to our findings, an approximately doubled risk of revision due to dislocation was observed in patients with rheumatoid arthritis (Conroy et al. Citation2008). Our finding that THAs inserted due to sequelae after pediatric diseases of the hip are not at higher risk of revision due to dislocation than THA inserted due to osteoarthritis are contradicted by a Danish registry study. In that study, patients with childhood disorders had an adjusted RR of revision due to dislocation of 3 compared to patients operated due to primary osteoarthritis (Thillemann et al. Citation2008). A reason for this discrepancy could be that we selected standard implants that had been used in at least 1,000 hips in order to specifically address the influence of head size, whereas custom-made implants and exotic implants were not included in our analysis, although such devices are probably over-represented in patients with sequelae after pediatric diseases of the hip. Another possible confounder is that most patients in Denmark are operated using the posterior approach.
Limitations of the study
We have only reported cases of revision due to dislocation, since closed reductions are not reported to the Register. The definition of the term “dislocation” varies between studies, and registry studies cannot be directly compared with cohort studies since the former usually do not include closed reductions, whereas the latter do. Factors such as age or medical comorbidity certainly influence the decision-making process for or against revision surgery after recurrent dislocations. We could not adjust for these confounders in our study. If present, one could speculate that cases believed to run an increased risk of dislocation are over-represented in the groups who received 36 mm heads and dual articular cups, in an effort by the surgeon to prevent dislocation. The observation that the majority of dual articular cups were inserted in cases with femoral neck fracture supports this presumption. Finally, due to the relatively short follow-up, we cannot comment on other relevant endpoints such as revision due to aseptic loosening, which is an interesting parameter when analyzing the outcome of large-diameter bearings.
In summary, patients receiving THA because of a femoral neck fracture or necrosis of the femoral head are at a higher risk of dislocation than patients with primary osteoarthritis, whereas patients with inflammatory joint diseases or sequelae after pediatric hip diseases are not. Posterior surgical approaches are associated with an increased risk of dislocation compared to lateral approaches, and minimally invasive approaches quite dramatically enhance the risk of this complication. Our study indicates that the overall risk of dislocation is reduced by increasing femoral head size. Even if the use of dual-mobility cups appeared to adequately address the problem of instability, this observation did not reach statistical significance. Our findings raise the question of whether patients with risk factors such as a diagnosis of femoral neck fracture or femoral head necrosis should be operated using lateral approaches with larger femoral head sizes or dual-mobility cups in order to minimize the risk of dislocation.
NPH: statistical analysis, and writing and revision of the manuscript. AS and RJW: revision of the manuscript. JK: database preparation, statistical analysis, and revision of the manuscript.
We thank all the Swedish orthopedic surgeons and secretaries who contributed data.
No competing interests declared.
- Amlie E, Hovik O, Reikeras O. Dislocation after total hip arthroplasty with 28 and 32-mm femoral head. J Orthop Traumatol 2010; 11 (2): 111-5.
- Australian Orthopaedic Association. National Joint Replacement Registry. Annual Report 2011.
- Bauchu P, Bonnard O, Cypres A, Fiquet A, Girardin P, Noyer D. The dual-mobility POLARCUP: first results from a multicenter study. Orthopedics (Suppl 2) 2008;31:(12).
- Berry DJ, von Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg (Am) 2005; 87 (11): 2456-63.
- Bistolfi A, Crova M, Rosso F, Titolo P, Ventura S, Massazza G. Dislocation rate after hip arthroplasty within the first postoperative year: 36 mm versus 28 mm femoral heads. Hip International 2011; 21 (5): 559-64.
- Bouchet R, Mercier N, Saragaglia D. Posterior approach and dislocation rate: a 213 total hip replacements case-control study comparing the dual mobility cup with a conventional 28-mm metal head/polyethylene prosthesis. Orthop Traumatol Surg Res 2011; 97 (1): 2-7.
- Boyer B, Philippot R, Geringer J, Farizon F. Primary total hip arthroplasty with dual mobility socket to prevent dislocation: a 22-year follow-up of 240 hips. Int Orthop 2012; 36 (3): 511-8.
- Browne JA, Pagnano MW. Surgical technique: A simple soft-tissue-only repair of the capsule and external rotators in posterior-approach THA. Clin Orthop 2012; (470) (2): 511-5.
- Bystrom S, Espehaug B, Furnes O, Havelin LI. Femoral head size is a risk factor for total hip luxation: a study of 42,987 primary hip arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop Scand 2003; 74 (5): 514-24.
- Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, Malchau H. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop 2011; (469) (2): 319-29.
- Conroy JL, Whitehouse SL, Graves SE, Pratt NL, Ryan P, Crawford RW. Risk factors for revision for early dislocation in total hip arthroplasty. J Arthroplasty 2008; 23 (6): 867-72.
- Enocson A, Hedbeck CJ, Tidermark J, Pettersson H, Ponzer S, Lapidus LJ. Dislocation of total hip replacement in patients with fractures of the femoral neck. Acta Orthop. 2009a; 80(2): 184-9.
- Enocson A, Pettersson H, Ponzer S, Tornkvist H, Dalen N, Tidermark J. Quality of life after dislocation of hip arthroplasty: a prospective cohort study on 319 patients with femoral neck fractures with a one-year follow-up. Qual Life Res 2009b; 18 (9): 1177-84.
- Farizon F, de Lavison R, Azoulai JJ, Bousquet G. Results with a cementless alumina-coated cup with dual mobility. A twelve-year follow-up study. Int Orthop 1998; 22 (4): 219-24.
- Fevang BT, Lie SA, Havelin LI, Engesaeter LB, Furnes O. Improved results of primary total hip replacement. Acta Orthop 2010; 81 (6): 649-59.
- Furnes O, Lie SA, Espehaug B, Vollset SE, Engesaeter LB, Havelin LI. Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987-99 J Bone Joint Surg (Br) 2001;83(4): 579-86.
- Hailer NP, Garellick G, Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Evaluation of 170,413 operations. Acta Orthop 2010; 81 (1): 34-41.
- Jameson SS, Lees D, James P, Serrano-Pedraza I, Partington PF, Muller SD, Meek RM, Reed MR. Lower rates of dislocation with increased femoral head size after primary total hip replacement: a five-year analysis of NHS patients in England. J Bone Joint Surg (Br) 2011; 93 (7): 876-80.
- Ji HM, Kim KC, Lee YK, Ha YC, Koo KH. Dislocation after total hip arthroplasty: A randomized clinical trial of a posterior approach and a modified lateral approach. J Arthroplasty 2012; 27 (3): 378-85.
- Lachiewicz PF, Soileau ES. Dislocation of primary total hip arthroplasty with 36 and 40-mm femoral heads. Clin Orthop 2006; (453): 153-5.
- Langlais FL, Ropars M, Gaucher F, Musset T, Chaix O. Dual mobility cemented cups have low dislocation rates in THA revisions. Clin Orthop 2008; (466) (2): 389-95.
- Meek RM, Allan DB, McPhillips G, Kerr L, Howie CR. Epidemiology of dislocation after total hip arthroplasty. Clin Orthop 2006; (447): 9-18.
- Philippot R, Adam P, Reckhaus M, Delangle F, Verdot FX, Curvale G, Farizon F. Prevention of dislocation in total hip revision surgery using a dual mobility design. Orthop Traumatol Surg Res 2009a; 95 (6): 407-13.
- Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop 2009b; 33 (4): 927-32.
- Phillips CB, Barrett JA, Losina E, Mahomed NN, Lingard EA, Guadagnoli E, Baron JA, Harris WH, Poss R, Katz JN. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg (Am) 2003; 85 (1): 20-6.
- Sariali E, Lazennec JY, Khiami F, Catonne Y. Mathematical evaluation of jumping distance in total hip arthroplasty: influence of abduction angle, femoral head offset, and head diameter. Acta Orthop 2009; 80 (3): 277-82.
- Sköldenberg O, Ekman A, Salemyr M, Boden H. Reduced dislocation rate after hip arthroplasty for femoral neck fractures when changing from posterolateral to anterolateral approach. Acta Orthop 2010; 81 (5): 583-7.
- Söderman P. On the validity of the results from the Swedish National Total Hip Arthroplasty Register. Acta Orthop Scand (Suppl 296) 2000; 71: 1-33.
- Swedish Hip Arthropasty Register. Annual Report. 2010. http://www.shpr.se/en/Publications/DocumentsReports.aspx
- Tarasevicius S, Busevicius M, Robertsson O, Wingstrand H. Dual mobility cup reduces dislocation rate after arthroplasty for femoral neck fracture. BMC Musculoskelet Disord 2010; 11:175.
- Thillemann TM, Pedersen AB, Johnsen SP, Soballe K. Implant survival after primary total hip arthroplasty due to childhood hip disorders: results from the Danish Hip Arthroplasty Registry. Acta Orthop 2008; 79 (6): 769-76.
- Weeden SH, Paprosky WG, Bowling JW. The early dislocation rate in primary total hip arthroplasty following the posterior approach with posterior soft-tissue repair. J Arthroplasty. 2003; 18 (6): 709-13.
- Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg (Am) 1982; 64 (9): 1295-306.