Acknowledgements
First of all I am grateful to the children and the parents who have made this research possible by participating in my projects. I am greatly indebted to my omnipresent supervisor Dr. Asbjørn Årøen for guiding me through my PhD project. He seems to answer my emails before I send them, even at 2 am, and the responses are always constructive and very inspiring. I thank my two co-supervisors professor Pål Gulbrandsen and Einar A Sivertsen. Pål’s invaluable help made my projects much more important than if he had left it for the orthopods to sort things out on our own. Dr. Sivertsen is thorough, patient, methodological and highly intelligent, all features that I was sorely missing. Without any of these stellar instructors my thesis would simply not have been possible.
I also wish to thank my colleagues and co-authors who have helped me collect my data: Inge Skråmm, Stein Erik Utvåg, Hendrik Fuglesang, Ståle Clementsen, Mads Oksum, Filip Dolatowski, Ola-Lars Hammer and Jan-Harald Røtterud. I hope we all get to work together for years to come. I also thank my boss Dr. Odd Granlund, for making room for my research during the complicated reorganisation of the hospital.
A special thank to the brilliant statistician Jûrate Šaltyte Benth for invaluable help. I would also like to express my gratitude to professor Roald Bahr at the Oslo Sport Trauma Research Center who generously invited me repeatedly to the annual spring seminars at Kleivstua. These uniqe seminars improved my projects, and I am grateful for the hospitality I have been shown by everyone at OSTRC.
I have received financial support from the Sophie’s Minde Foundation, Ahus’ Strategic research fund and Aase Bye & Trygve J. B. Hoffs fund. To all, I am grateful.
Finally I thank my wife Marit for keeping up with me, and my children for making me keep up with them…. Stay out of trouble now (inclusion has stopped…).
Per-Henrik Randsborg
London, December 4th, 2012
Included papers with brief summaries
Paper I
Randsborg P H, Sivertsen E A. Distal radius fractures in children: substantial difference in stability between buckle and greenstick fractures. Acta Orthop 2009; 80(5): 585-9
The medical records of 305 paediatric distal radius fractures were reviewed. Only 1 of 311 follow-ups led to an active intervention. The greenstick fractures had more complications than the buckle fractures. The stability of greenstick and buckle fractures of the distal radius was assessed by comparing the lateral angulation radiographically. The lateral angulation of the buckle fractures did not change importantly throughout the treatment. The greenstick fractures displaced 5 degrees on average, and continued to displace after the first 2 weeks. On average, the complete fractures displaced 9 degrees. We conclude that buckle fractures are stable and do not require follow-up. Greenstick fractures are unstable and continue to displace after 2 weeks. Complete fractures of the distal radius are uncommon in children, and highly unstable. A precise classification of fracture type at the time of diagnosis would identify a smaller subset of patients that require follow-up.
Paper 2
Randsborg P H, Sivertsen E A, Skråmm I, Šaltyte Benth J, Gulbrandsen P. The need for better analysis of observational studies in orthopaedics. A retrospective study of elbow fractures in children. Acta Orthop 2010; 81(3): 377-81
In a cohort of 112 patients with single supracondylar humerus fractures, 78 patients were examined clinically on average 4 years after surgery. There were no cases of permanent neurovascular injury, deep infection, or compartment syndrome. We found 21 postoperative complications (19%). Gartland 3 fractures were operated earlier and more often by consultants, and had more complications than Gartland 2 fractures. 11 of the 78 elbows had a cubitus varus malunion. The mean VAS score was lower in patients who developed cubitus varus (7.7 vs. 9.6) than in patients who had a positive carrying angle (p < 0.001).
The results were used to compare traditional least-squares regression analysis with a two-level model with interactions. The conventional statistical methods employed in observational studies in orthopaedics require the fundamental assumption that the outcomes are independent. However, fractures treated by the same surgeon cannot be regarded as being independent of each other and should be nested in the statistical analysis. We found that 25% of the variance in outcome could be attributed to between-surgeon variance. We also identified an interaction between the surgeons’ experience and the severity of the fractures that influenced the conclusions. We conclude that researchers should consider the need for a 2-level model and the presence of interactions. Standard statistical methods might lead to wrong conclusions.
Paper 3
Randsborg P H, Sivertsen E A. Classification of distal radius fractures in children: good inter- and intraobserver reliability, which improves with clinical experience. BMC Musculoskeletal Disorders 2012; 13(1): 6
12 doctors rated 105 consecutive fractures of the distal radius in children on two occasions three months apart. The doctors were placed in 3 groups according to the level of formal experience; 4 junior registrars, 4 senior registrars and 4 orthopaedic consultants. Each fracture was placed in one of four possible categories; buckle, greenstick, complete or physeal. The kappa value for interobserver agreement at the first reading was 0.59 for the junior registrars, 0.63 for the senior registrars and 0.66 for the consultants. The mean kappa value for intraobserver reliability was 0.79 for the senior registrars, 0.74 for the consultants and 0.66 for the junior registrars. We conclude that the classification tested in this study is reliable and reproducible when applied by raters experienced in fracture management. The reliability varies according to the experience of the raters. More focus on the different fracture categories and better supervision of our younger colleges by experienced raters will reduce the number of unnecessary clinical and radiological follow-up appointments.
Paper 4
Randsborg PH, Gulbrandsen P, Šaltyte Benth J, Sivertsen E A, Hammer O L, Fuglesang H F, Årøen A. Fractures in children. Epidemiology and activity-specific fracture rates. J Bone Joint Surg [Am] 2013; 95: e42(1-7), DOI:10.2106/JBJS.L.00369
1403 paediatric fractures were registered prospectively over 12 months. Exposure time to the most common childhood activities was measured by parental interview. The overall annual incidence was 180.1 fractures per 10,000 children younger than 16 years. The distal radius was most often fractured (436 fractures, 31.1%). Snowboarding had the highest activity-specific fracture rate, estimated to 1.9 (95% confidence interval [CI] 1.16–2.60) fractures per 10,000 hours of exposure. In comparison, the fracture rate per 10,000 hours of exposure was 0.79 (CI, 0.42–1.09) for handball, 0.44 (CI, 0.35–0.52) for soccer, and 0.35 (CI, 0.23–0.47) for trampolining. We conclude that the fracture rates differ between various physical activities. Specific preventive measures should be implemented to target this subpopulation of children at risk of fractures.
Introduction
Fractures in childhood are common and are often considered a consequence of normal active upbringing. The fracture incidence seems to be rising Citation(67) and children with previous fractures are of particular risk to sustain a new fracture Citation(45). Evidence suggests that the majority of childhood fractures occur in children who will experience two or more fractures Citation(44). Still half of all children remain fracture free until adulthood Citation(63), suggesting that some children are more prone to fractures than others. When treating a paediatric fracture, the aim is to restore full function, as well as to obtain a best possible cosmetic result. The paediatric long bones have a great potential for remodelling Citation(113;129), helping the patient (and the orthopaedic surgeon) to achieve these goals. Although most fractures in children heal without loss of function, there are considerable costs for the child in form of pain, hospitalisation, time away from school and reduction of activity for weeks to months Citation(71). Although paediatric fractures normally are closely followed in the outpatient clinic Citation(46), it is a common clinical observation that secondary intervention after primary treatment is rare. However, serious complications do occur. Childhood fracture can affect health and development due to complications such as malalignment of the bone, length overgrowth, physeal arrest Citation(11), compartment syndrome or neurovascular complications, either iatrogenic or caused by the fracture itself Citation(47). Osteoarthritis can develop as a consequence of intraarticular fractures Citation(42) or secondary to malalignment. It is desirable to be able to identify the small subset of patients that actually needs follow up to implement effective follow-up routines. The prevention or reduction of fracture risk in addition to adequate follow-up would imply huge benefits both for the child and the society.
Epidemiology
During the last half century, children in the western world have enjoyed increasing prosperity, leisure time and access to recreational and organized sport. Despite this increase in welfare, the number of fractures in children has increased enormously. In his classic study of 8,682 paediatric fractures, Lennart Landin reported a two-fold increase in fracture rate between 1950 and 1979 in a Swedish population Citation(75). Though some of the increase might be attributed to better access to healthcare and better detection of small fractures, there is general agreement that there has been a true increase in the incidence of paediatric fractures Citation(48;52;67).
Age and gender
The properties of growing bone together with the natural physical development and increased ability to ambulate as children grow older explains why the incidence of childhood fractures increase linearly from birth to a peak incidence between ages 12 and 15 years Citation(9;14;75). The universally observed peak in fracture incidence at the start of puberty coincides with the growth-spurt that involves increased demand of new bone, a high turn-over of bone metabolism and reshaping of the metaphysis prior to the closing of the physis Citation(5;43;106). The onset of puberty is earlier in girls and boys, explaining why the fracture incidence peaks earlier in girls than in boys ().
Figure 1. Distribution of fractures by age and sex (from Paper 4). Copyright Journal of Bone and Joint Surgery [Am], reprinted with permission.
![Figure 1. Distribution of fractures by age and sex (from Paper 4). Copyright Journal of Bone and Joint Surgery [Am], reprinted with permission.](/cms/asset/77fa4aae-9f6d-4749-bb85-4eea8bae0744/iort_a_789731_f0001_b.jpg)
Landin observed a double risk of sport-related fractures in boys than in girls, and boys were 50% more likely than girls to sustain a fracture before age 16 Citation(75). As girl’s participation in sport and recreational activity increases, the difference between the sexes have decreased, but boys are still at a higher risk of sustaining a fracture. The level of physical activity in Norwegian 9-year-old children increased in the five year period from 2000 to 2005 Citation(70). The change was greater for girls than boys in children from families with high socioeconomic status, indicating that girls are catching up with boys in terms of participating in sports and recreational activities.
Seasonal distribution
Several large epidemiological studies from the northern hemisphere have found a seasonal variation of paediatric fractures, with most fractures occurring during summer and autumn Citation(14;89;126;150). Most paediatric fractures occur during physical activities such as sport and play. Physical activity depends on space and light, and explains why more fractures occur outdoors during summer and autumn when there are more hours of sunshine and easier to spend time outdoors.
Location of fracture
Most paediatric fractures occur outdoors. Younger children are at particular risk of sustaining fractures on playgrounds Citation(147), while older children tend to sustain fractures during recreational and organized sports Citation(9;14;144). In a large epidemiological study of more than 58 million emergency visits in the United States, 16.5% of all injuries in school-aged children (5–19 years) occurred at school. Sports injuries were significantly more common in school (53% of injuries) than outside schools (33%, p < 0.001). In a prospective registration of 1735 childhood fractures from Bergen, Norway, 20% of fractures in schoolchildren occurred outdoors at school, and 10% indoors at school Citation(9). Most fractures in schoolchildren occurred outdoors near the home (28%).
Paediatric fractures and physical activity
Regular physical activity is necessary for children to ensure healthy mental and physical development Citation(54). There is a global increase in the prevalence of childhood obesity Citation(103;148), and Norwegian children are no exception Citation(65). International physical activity guidelines for children recommend that children participate in at least 60 minutes of moderate or vigorous physical activity every day Citation(141). In the United States, less than one third of 15 year olds meet these guidelines Citation(98). Efforts are therefore necessary to increase the physical activity in children. However, physical activities expose children to an unwanted and in some cases unacceptable risk of injury, such as permanent complications or even death Citation(10;17;125;154). The increase in paediatric fractures observed by Landin Citation(75) have been attributed to a general increase in sports and physical activity Citation(9;52;84). Sport and recreational activities are reported to cause up to 39% of paediatric fractures Citation(9;52). To be able to identify measures that can reduce the risk of injury while maintaining the recommended level of physical activity, it is important to quantify the risk of injury associated with childhood activities.
The injury risk describes the cumulative number of injuries that occur in a given population over a given time, while the injury rate considers the length of person-time exposure to the risk. The terms risk and rate are often used interchangeably in sport injury epidemiology Citation(68). Although there are numerous reports of injury risk on various childhood activities, the exposure to risk is rarely quantified Citation(136). Further sport injury research and surveillance data is needed to help identify specific risk factors in young athletes. As we will discuss in this thesis, it is important that such studies include an estimate of the exposure time for the various activities. Exposure time is essential to be able to compare sports and to quantify their associated injury rates Citation(22). For example, some activities such as motor sports might have a low injury risk (incidence) because it is performed by few children, but have a high injury rate when the exposure to the activity is accounted for. Most reports on injury rates have focused on isolated sports, such as soccer, handball or ice-hockey Citation(29;97;153). Reported injury rates for soccer have varied from 0.04 injuries per 1000 hours Citation(23) to 75.8 injuries per 1000 hours Citation(55). This variation by a factor of 1000 is attributed to methodological differences Citation(136), mostly selection bias. This bias is introduced because the definition of injury varies greatly between publications. In some studies, parental reported injuries are included Citation(137), other studies include injuries that prevented the athlete from participating in the next training Citation(29;112). Other studies have included injuries that were evaluated by a doctor Citation(153). However, the threshold to avoid training or to seek medical advice varies greatly among children and families, as does the perception of what constitutes an injury worth reporting in a study setting. Hence, the injuries included in one study are different from the injuries included in another study. These differences in injury definition lead to a large variation in reported injury rates for the same sport, making comparison between studies impossible. It is therefore necessary to standardize the inclusion criteria so that studies can be reproduced and comparable. This is why we have elected to study fracture rates instead of injury rates. A fracture is normally a definite diagnosis based on radiological findings, and treatment is channelled through the fracture clinics, avoiding overestimation. Moreover, fractures are rarely left untreated, making underestimation less likely.
Furthermore, the exposure to different sports in the same population is rarely presented in published data, making comparison between sports impossible. In Paper 4 we estimate the fracture rates for various childhood activities in the same population during the same period of time, making comparison between sports possible. Our precise injury definition (fractures) and complete record of all fractures in a population will make it possible to reproduce our results elsewhere.
Health service perspectives
It is an ongoing challenge for decision makers to adopt the healthcare institution to the health challenges in the population. The incidence of diseases in a given population varies over time. The progress of medical science brings both new conditions and new treatments, while the dynamics of society remove and add risk factors, changing the panorama of diseases. It is therefore essential that proper population based studies are performed regularly to monitor the health of the population. This will enable policymakers to adapt to changes and prepare the healthcare organisations accordingly.
Any healthcare provider must evaluate the quality of the service rendered to the public by investigating the clinical outcome of the patients. The effectiveness of the infrastructure and treatment algorithms should be constantly scrutinized, so that the best practice is ensured. Resources are not limitless, and it is the responsibility for the institutions to ensure that expenses are acceptable. Unnecessary clinical controls and lengthy hospital stays are a burden both to society and patients. To be able to avoid unnecessary healthcare visits without compromising the safety of the patients, clinical data must be collected in a methodological and scientific matter. These data must then be analyzed using appropriate statistical methods. Statistical models can always be improved to better fit reality, and it is possible to lend statistical designs developed in other scientific fields to improve the accuracy of the conclusions drawn. This is especially crucial when the results from observational studies lead to a change in clinical management.
Purpose of the present dissertation
The overall purpose of the present thesis is to improve and increase our knowledge of the incidence, causes and management strategies of paediatric fractures. Four studies have been performed with the following aims:
| I | to compare the stability of greenstick and buckle fractures of the distal radius in children, | ||||
| II | to investigate the inter- and intrareliability of the most commonly used classification of distal radius fractures in children, | ||||
| III | to investigate the clinical outcome after displaced supracondylar humerus fractures in children managed by closed reduction and percutaneous pinning, | ||||
| IV | to evaluate the statistical methods employed in observational studies in orthopaedics, | ||||
| V | to describe the epidemiology of paediatric fractures in our region of Norway, | ||||
| VI | to estimate the fracture rate by hours of exposure of the most common childhood sport and recreational activities. | ||||
Methodological considerations
Ethics
To obtain informed consent from a participant in a research program means that the person willingly chooses to partake in the research after being informed in a manner that is understandable for her or him, without any external coercion, pressure or inducement. This means that the information has to be presented in a manner understandable for the children as well as the parents. Babies and toddlers cannot possibly be expected to understand a research protocol, but as the children grow older, more level of understanding is expected. But it is difficult to determine at what age a child is mature enough to make an independent choice. There has been an increasing focus on the right for children to participate in the discussion regarding their own health. In Norway, the ethical committees suggest that the parents or legal guardian make decisions for children younger than 12 years, children aged 12 to 16 have the right to be heard and children older than 16 years can make their own decision Citation(7). In practice, this means that children older than 12 years should have a say in the decision, and parental consent might not be sufficient to include the child in the study Citation(20). Reversely, in children older than 16 years old, parental dissent might be ignored if the patient gives informed consent. We have adhered strictly to these guidelines when including children in our research projects. To give children aged 12–16 years a better understanding of the research projects, specific information letters aimed at this age group were written. These letters were approved by the regional ethics committee. For children aged 12–16 both the children and their parents gave written consent.
Included materials and subjects
The papers included in this dissertation are based on data collected from a total of 2,673 children younger than 16 years from Akershus, Norway. Papers I to III reflects materials from three different retrospective cohorts. In Paper I, the radiographs and clinical data from all 306 paediatric distal radius fractures managed at our institution in 2006 was examined. There were 172 boys (56%) and the average age was 9.9 (range 1.3–16) years. The material investigated in Paper II derives from the radiographs and clinical data of 112 supracondylar humerus fractures that were treated operatively with percutaneous pinning at our institution between 1999 and 2006. There were 62 boys (55%) and the average age was 6.1 (range 1.6–12.4) years at the time of injury. 78 of these children attended a follow-up clinic on average 4.3 years after the injury. To examine the reliability of the classification of distal radius fractures in children (Paper III), we collected data from the first 105 consecutive paediatric distal radius fractures that were managed at our fracture clinic in 2007. These fractures occurred in January, February and March 2007. There were 72 boys (69%) and the average age at the time of fracture was 11.4 (range 1.6–15.8) years.
In the fourth and final paper we included all paediatric fractures that were managed at our institution between March 16, 2010 to March 15, 2011. 1,357 patients who had sustained 1403 fractures were finally included. 866 (61.7%) of the fractures occurred in boys. The average age at the time of fracture was 10.0 (range 0.7–16) years. To estimate the exposure time for various child activities, the parents of 794 random children in our area were interviewed, of which 395 (49.7%) were boys. The mean age of the children at the time of the interview was 9.3 (range 3–16) years. The patients from the fracture register are considered cases, and the children from the interviews are considered controls. An unmatched case-control study was then designed to estimate fracture rates of various childhood activities.
Study design and data collection
The choice of study design is of paramount importance in any research project. The type of design will affect both the results and how these should be analyzed and interpreted. Two main types of errors can affect the study design, namely systematic error and random error. Systematic errors are any circumstance that leads to the situation where the measured means of the outcome measurements differ significantly from the actual values of the population. A properly designed study will minimize the systematic error. The effect of the systematic error remains unchanged regardless of the sample size, while the effect of random error will decrease as the sample size increases. The random error is basically the variation in the data that we cannot readily explain. This type of error cannot be removed from the dataset, but the employment of the appropriate statistical model will reveal the inaccuracy of the data caused by the random error. Improper statistics might yield misleading results, although the study is well designed. This is certainly the case for observational studies in orthopaedics, as demonstrated in Paper 2 and discussed later in this dissertation.
Two broad types of clinical study designs exist: interventional studies and observational studies. Interventional studies are controlled experiments that compare the effect of different treatments by allocating different treatments to two or more groups of similar patients. In evidence-based medicine, randomized-controlled trials are considered the gold-standard that render the highest level of evidence. However, there are situations where it is impractical or even unethical to conduct a randomized controlled trial, especially in the field of surgery Citation(56). In these cases, observational studies may be more appropriate.
All of the four papers in this dissertation are observational studies. Differences between groups are observed and compared without the intervention of the investigator. The main concern regarding observational study is the potential threat to the internal validity caused by the potential introduction of confounders Citation(94). This occurs because there is no randomization or blinding to avoid (or at least limit) differences between groups, introducing known or unknown confounders that may generate biased results. Paper 2 demonstrates that the existence of interactions also can generate biased results, and should be considered as well as confounders.
There are several types of observational studies, such as cohort studies and case-control studies. A cohort is a group of people that have shared an experience over the same period of time. In research it is used to describe a group of individuals that are observed or followed over a period of time Citation(124). Case-control studies are epidemiological observational studies that endeavours to identify risk factors for any given condition by investigating patients with the disease (cases) with individuals without the disease (controls), but who are otherwise similar. Case-control studies are quicker and cheaper than prospective cohort studies, and the statistical power is higher because cohort studies have to continue until sufficient number of disease events have occurred. However, it is difficult to gather reliable exposure data for both cases and controls, risking the introduction of systematic errors.
The cohort studies
A cohort study can be both prospective (Paper 4) and retrospective (Paper 1, 2 and 3). The main problem with a cohort study is selection bias. Selection bias occurs when the patients who participate in the study differ from those who don’t. Another systematic error is information bias. In a retrospective cohort study, the information is based on previously collected data, and might not be detailed enough or even accurate. In a prospective cohort study, the type of data collected is standardised, thus reducing the risk of information bias.
Although prospective studies have several obvious benefits, such as controlling the data collection and standardizing measurements, retrospective studies describes the results from treatment conducted in the institution based on standard routines, outside the controlled settings of a study design. This gives important information regarding the effect of the health service and the current treatment algorithm in the institution where the study was conducted. Patients who know they are studied have improved results compared to those who don’t Citation(31;90). This is known as the Hawthorne effect, and is avoided in retrospective studies.
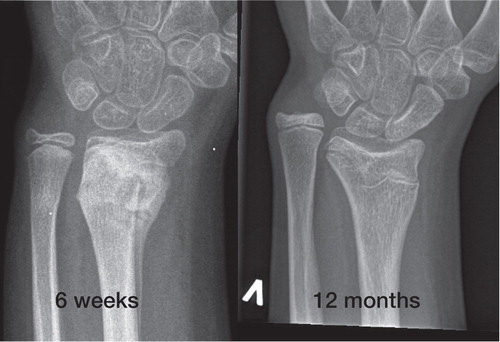
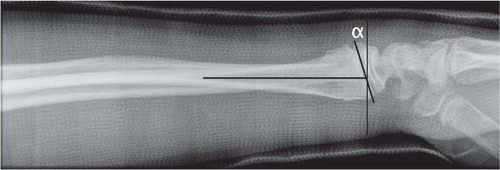
In Paper 1, we wanted to compare the stability of distal radius fractures in children. The study design is a retrospective cohort. The patients were easily identified through our computerized files, but some selection bias might have occurred. Patients who were given the wrong ICD-10 code (International Statistical Classification of Diseases and Related Health Problems, tenth revision) would be missed. Further, it is possible that some patients elected to attend neighbouring hospitals, and would not be included in our retrospective cohort. However, during the data collection leading to Paper 4 we controlled for leakage to neighbouring hospitals, which was found to be very small. We therefore believe that this is likely to be a very small number of patients and should not affect conclusions. Another reason to chose a retrospective design is that the data we collected were available in its original form (radiographs). To assess the stability of the fractures, we measured the lateral angulation on the radiographs at presentation and at all other subsequent radiographs retrospectively. The angle of the distal radial physis on the radial axis (the epiphyseal axis angle) is normally 90° Citation(77). Any deviation from this normality represents the true displacement caused by the fracture, as represented by α in . If we had designed a prospective study, we could have standardized the radiographs, possibly improving the accuracy of the measurements. However, we believe our results are valid , since this is a reliable and recommended method to asses distal radial deformities in children Citation(77). In our opinion the benefit of a retrospective design in this case outweighs the burden of conducting this study as a prospective cohort study.
Figure 2. Measuring the sagittal displacement of distal radial fractures in children. α represents the angular displacement caused by the fracture.
The classification of the fractures in Paper 1 could have introduced an information bias known as misclassification, since we were two different raters who classified the fractures into one of the four categories (buckle, greenstick, complete and physeal). We know now from Paper 3 that this classification is reliable, but depends on the experience of the rater Citation(117). The two raters of Paper 1 have similar experience in treating wrist fractures in children, and we have therefore reason to believe that the information bias is limited.
Paper 2 consists of a retrospective review of the medical records of 112 supracondylar humerus fractures in children operated between 1999 and 2006. Some selection bias is likely to have been introduced during the sampling. Patients who were given the wrong diagnostic- or operative code would have been missed in our electronic search. 78 of 112 patients attended the follow up, probably introducing a selection bias known as self-selection. The 34 patients who did not attend the follow-up clinic might have had a different clinical outcome than those who attended.
In Paper 4 we wanted to collect data regarding the mechanism of injury in paediatric fractures. A retrospective study would not be appropriate, because the type of data needed are not normally recorded in the medical files. A prospective design let us standardize the data collection, which consisted of a questionnaire regarding the location and mechanism of injury, previous medical history including previous fractures etc. We collected data for 12 months. Very few parents (or children) refused participation, but selection bias could still have been introduced.
When calculating the annual incidence of paediatric fractures, the major challenge is to control both the nominator (All children younger than 16 years with a new fracture) and denominator (all children younger than 16 years living in our region). The denominator could be identified by national registers. The National Population Register is a public register with details of all registered residents living in Norway. By October 1, 2010 (halfway through the inclusion period) 77,683 persons younger than 16 years (63,986 aged 3–16) were registered habitants of the catchment are of Akershus University Hospital Citation(138). Virtually all paediatric fractures are treated at our institution, and all radiographs and medical journals are digitalized and viewable via the same system. This system allows for a comprehensive fracture registration of all paediatric fractures. The neighbouring hospitals were contacted during the study period, to identify children with new fractures living in our area who contacted these hospitals. These patients constituted less than 1% of our total number, and most of these patients were included in the study when they were transferred to our institution for follow-up. We therefore believe that the nominator in our incidence is complete and reliable. The only exemption could be patients who were fully treated outside of our region or neighbouring hospitals, and thus not referred to our institution for follow up. We believe this to be a miniscule number of patients, representing a small selection bias that would not affect conclusions.
The case-control study
To estimate fracture rates for various childhood activities, we designed a case-control study. The major drawback of a cohort study is the need to gather information of a large population to measure the rate of a disease. Only 1–2% of children sustain a fracture every year Citation(43). We could not possibly measure the exposure time for all activities for all children living in our area in a prospective cohort. We therefore designed a case-control study, where the cases are the patients from the prospective cohort of children with fractures. We assume this to be a complete record of children with fractures in our region. The controls however, had to be selected from the population. This introduces selection bias, which is the major weakness of any case-control study. The source population in our case-control study is all children living in our region (at risk of fracture). We randomly invited the parents of children in our region to answer questions regarding their child(ren)s exposure time for various activities in summer and winter. 24% (600 of 2502) of the households agreed to participate in the survey. This is the major limitation of our study, and represents a self-selection bias. The parents (and children) who accepted could be different from those who didn’t. Therefore the estimated exposure time in our calculation might not be representative for the entire population. An information bias known as memory bias could also have been introduced. The parents answered questions on their child activity level, and had to rely on their memory. Even though the collection of the exposure data might introduce selection bias and therefore limit the ability to generalize study findings to the whole population, it represents the underlying strength of the study, making it possible to compare the fracture rates between different sports and activities.
Statistics
Just as we strive to improve surgical technique, we should also try to improve our statistical design. The statistical models we employ on our data might influence results, and even lead to change in clinical management. No statistical method can fully describe reality, but we should constantly look for the best fitted model. Standard statistical methods, such as ordinary least-squares regression analysis might not be appropriate. In this thesis, we have looked at several statistical issues. In Paper II we compared the use of a more sophisticated multilevel modelling with and without interactions to the standard OLS regression model. The kappa statistics used to measure reliability of fracture classification have been scrutinized in Paper III. In the last paper we discussed the difference and importance of injury rates compared to injury risk, and the necessity of exposure data to be able to compare risk.
Multilevel modelling
Multilevel modelling was initially developed in social sciences, such as education and sociology Citation(24), but the implementation of this statistical method has not yet been adopted by medical researchers, despite repeated encouragements Citation(15;130). In standard regression analysis, there is a fundamental assumption that every outcome event is independent of each other. However, patients operated by the same surgeon are likely to have a more similar outcome than patients operated by another surgeon. This dependency should be controlled for in the statistical design. Multilevel analysis allows clustering of individual units (patients) within units of a higher level (patients operated by the same surgeon). It is a common misunderstanding that multilevel analysis is controlling for the experience of the surgeon, or to put it simply; to see who the best (or worst) surgeon is. This misconception might partly explain why this model is rarely used in orthopaedic research. But the results for fractures treated by the same hands are likely to be more similar than if they were not, regardless of the ability of the surgeon. Ignoring such correlations may lead to underestimation of standard errors, increasing the risk of committing a type-I error with the conclusion that a variable is statistically significant when it is not. The intraclass correlation coefficient (ICC) expresses the amount of dependency among observation and is calculated to decide whether a multilevel analysis is appropriate. The ICC can take values from 0 to 1. A non-zero value of ICC implies that the observations are not uncorrelated and that there is a need for multilevel modelling.
In Paper II we show that the clinical outcome after pinning of displaced supracondylar humerus fractures in children is good or excellent in most cases. We have used our clinical data to compare two different statistical approaches; regression analysis and multilevel modelling. We demonstrate that the simple statistical methods that are commonly used in observational studies might in fact lead to wrong conclusions. We have considered the most commonly used explanatory variables for inferior outcome; still 84% of the variance in outcome is unexplained by our data. The level of explainable variance should be stated in published papers, so that readers can consider the clinical relevance of statistically significant results. Furthermore, we have demonstrated that even in a case with low level of explained variance, the use of models that more accurately reflect reality (effect modifiers, two levels) affects conclusions. This is even more likely to occur in observational studies with more frequent adverse outcomes.
Our two-level model demonstrates that 24% of the explainable variance is attributed to the surgeon level. It seems that the surgeon has more influence on outcome than any of the predictors. It is noteworthy that the variable “number of pins” becomes non-significant in this model (p=0.07). Without a two-level model we would report this as a significant finding (p=0.01), committing a Type I error.
Interactions
In Paper II we also tested the effect of the inclusion of interaction variables in the model. An interaction is defined as a factor that modifies the independent factor under study Citation(95). Interactions reflect that the effect of one variable depends on the values of one or more other variables. For example, the influence of the surgeon’s experience on outcome could be stronger for severe fractures than for less complicated ones. In such cases, a statistical model with interactions should be tested. One should not try out all possible interactions since this increases the risk of spurious results. Thus, when building the statistical model, variables that might produce an interaction must be considered apriori to the analysis, based on existing knowledge and clinical experience. In our study, we decided that the surgeon’s level of experience (consultant or resident) and time to surgery might have different effects on outcome depending on the severity of the fracture. We therefore included these two interaction terms in the model. The interaction had a significant effect on outcome (p=0.046) and was therefore included in the final model.
Measuring reliability
In Paper III we measured the reliability of the most commonly used classification system for paediatric distal radius fractures. The study was designed to comply with the guidelines for reliability studies of fracture classification systems outlined by Audigé, Bhandari and Kellam Citation(4). We selected to measure the reliability of the classification by means of the kappa coefficient. A kappa score of 1 indicates perfect agreement and a score of zero indicates that the variation in agreement can be explained purely by chance. Kappa is generally considered the best way to measure agreement between categorical assessments Citation(16;33), although there are certain limitations that should be acknowledged. Several aspects influence the kappa value, such as the number of categories, the prevalence of the different categories in the population and – as we demonstrated in Paper III – the experience of the raters. It is also evident that when a dataset is reduced to a single kappa value, information is lost underway. It is therefore difficult to interpret a kappa value, and even harder to agree on which kappa value should be considered acceptable. Most authors agree that a value inferior to 0.5 represents poor agreement Citation(33;76;142), but what constitutes an acceptable agreement will depend on circumstances. Statistical outcome measures can never replace clinical judgement.
Discussion
Distal radius fractures in children
Distal radius fractures is the most common fracture in childhood, representing 23–36% of all childhood fractures Citation(9;18;52;71;75;83;144). These fractures occur at any age, but they are most common during the adolescent growth spurt Citation(5;62). They are more common in boys, and the non-dominant arm is more often affected Citation(9;14;67). Two of the papers in this thesis focus on distal radius fractures in children (Papers 1 and 3), and Paper 4 provides estimates of the annual fracture incidence in our region of Norway.
Classification
In the scientific literature, fractures of the distal radius in children are commonly grouped into four categories Citation(12;21;79;91;92;100;111;118;135) (): Buckle (torus) fractures are characterized by a compression failure of bone without disruption of the cortex on the tension side of the bone Citation(79). The greenstick fractures differ from the buckle fracture as the cortex is disrupted on the tension side, but intact on the compression side of the fracture Citation(21). Complete fractures (adult type) have disruption of both cortices in one plane. Physeal injuries occur frequently during the preadolescent growth spurt, when there is a transient cortical porosity caused by the increase in calcium requirement and bone turn-over Citation(106). Fractures involving the growth plate are often subdivided according to the classification of Salter and Harris () Citation(127). The follow-up algorithm of these different categories varies, thus the classification will provide guidelines for management and prognosis.
Figure 3. Examples of fractures from each category. A: Buckle fracture B: Greenstick fracture C: Complete fracture D: Physeal fracture (From Paper 3). Published by BioMedCentral Musculoskeletal Disorders.
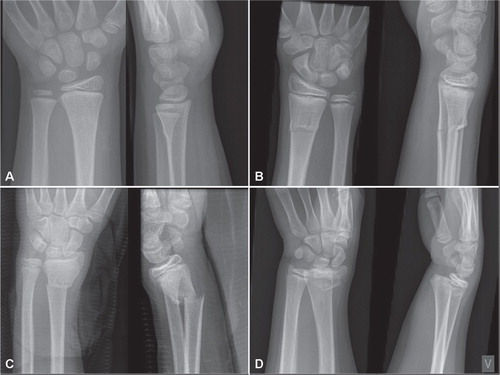
Figure 4. The Salter-Harris classification of growth plate injuries. Type I is a plain fracture through the physis. Type II includes a metaphyseal fragment. Type III is an intraarticular physeal fracture without affection of the metaphysis. Type IV has both intraarticular affection and a metaphyseal component. Type V is a compression injury of the physis. There is some controversy regarding the existence of type V.

Fracture classifications are important tools in the reporting of clinical research, leading to clinical consequences such as the development and implementation of treatment strategies. Although the classification of distal radius fractures in children described above has been used in several publications Citation(12;21;79;91;92;100), its reliability has to the best of our knowledge never been examined. If the reliability of a fracture classification is unacceptably poor, any research based on this system should be interpreted with caution, especially if the results changes clinical management. In Paper 3, we therefore investigated the inter- and intrareliability of the most commonly used classification system of paediatric distal radius fractures. Our results indicates that this classification system is indeed more reliable than other commonly used classification systems, such as the AO classification of distal radius fractures in adults Citation(74). The overall interobserver reliability of 0.61 in our study would be classified as excellent according to Fleiss Citation(33) and Svanholm Citation(142), and substantial according to Landis and Koch Citation(76). We therefore recommend this simple four category fracture classification for future research on the treatment and prognosis of distal radius fractures in children. However, we noted that inexperienced doctors had lower inter- and intraobserver reliability and placed more fractures in categories that merit a follow up (greenstick fractures and complete fractures) than more experienced doctors. We demonstrate that this lead to an increase in unnecessary radiological and clinical follow-ups, which can be avoided by better supervision and more focus on the fracture categories.
Stability, management and remodelling potential
We demonstrated in Paper I that buckle fractures are stable Citation(118). In this study most fractures (254 of 305) were minimally displaced and managed conservatively (without reduction). The majority of fractures were stable and did not need follow-up. Since this was a retrospective study, the results represent the actual management and effectiveness of the health service in our institution during 2006. No complications in the buckle or greenstick group led to surgical intervention. Of more than 300 clinical follow-ups, only 1 led to change in management. This was a complete fracture. Complete fractures are highly unstable, and will often need fixation with Kirschner pins Citation(91;92). Our results are similar to previous publications Citation(3;46;58;62;140). Like others, we see no need to follow-up buckle fractures Citation(30;110;135;151).
Greenstick fractures are, however, unstable. Moreover, they continue to displace also after the first 2 weeks (). Our study shows that it is difficult to identify which fractures will displace beyond 20º. None of the greenstick fractures in Paper 1 that displaced during the immobilisation period were subsequently manipulated. Two greenstick fractures with dorsal angulation > 20° at plaster removal were followed up after 6 months (at the discretion of the physician). In both cases the angulation had remodelled considerably. These are examples of the amazing potential for sagittal remodelling of the distal radius (). In children under 5 years, sagittal plane angulation up to 35° can remodel completely, and in patients younger than 10 years up to 25° of lateral angulation might remodel fully Citation(37;39;61;115;152). Excellent long-term functional and anatomical results have been reported Citation(58). Because of this wonderful ability to remodel, it is difficult to agree on limits for acceptable angulations and consequently on follow-up routines. If displaced greenstick factures of the distal radius remodel over time, and the clinical and radiological follow-ups never lead to a change in management (as seen in our study), it can be argued that immobilization alone is sufficient Citation(3;25). Immobilization alone has also been shown to be less costly than manipulation Citation(25). However, little is known about the consequences of a bent wrist on the physical activity of children, even if it’s transient. The degree of acceptable angulation diminishes as the child approaches puberty. Since girls reach puberty before boys, the acceptable lateral displacement is greater for boys than for girls ().
Figure 5. Lateral angulation during the immobilization period in plaster of unreduced greenstick fractures. Note the tendency of the lateral angulation to increase throughout the period. (Data from Paper I).
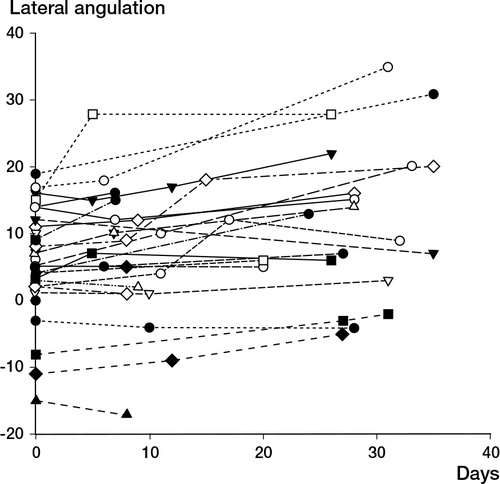
Table 1. Limits of angulation of distal radial metaphyseal fractures that will remodel anatomically. Based on references Citation(3;25;37;39;58;61;152)
Fractures involving the physis might lead to growth disturbances. The risk of distal radial growth arrest is estimated to 4–5% for displaced radial physeal fractures Citation(12;78). The risk of growth disturbances increase, however, if the fracture is reduced more than 3 days after the fracture, or if repeat attempts of reduction is attempted Citation(12). Salter-Harris Type 2 is the most common physeal fracture. Salter-Harris Type 3 and 4 are intraarticular fractures. These rare fractures often need surgery because the joint surface must always be reduced anatomically. When a physeal fracture needs reduction, the manipulation should be done carefully without the use of excessive force to avoid iatrogenic injury to the growth plate. It’s acceptable to place a smooth K-wire through the physis to stabilize the reduction, but repeat drilling through the growth plate should be avoided. There is some evidence to suggest that pinning reduces the risk of growth disturbance (), possibly because it stabilizes the physis and prevents harmful movement of the fragments Citation(131). Pinning through the physis may on the other hand also cause growth disturbance Citation(57).
Supracondylar humerus fractures in children
Supracondylar humerus fractures (SCHF) in children is the most common fracture around the elbow in children, and the most common fracture in children younger than 7 years (14;105). It is the most common cause of surgery to the elbow in children. The mechanism of injury is frequently a fall from a height, i.e. higher than body height (). The results after pinning of displaced SCHFs in children were examined in Paper 2.
Table 2. Mechanism of injury for 114 Gartland 2 and 3 supracondylar humerus fractures treated with closed reduction and percutaneous pining at Akershus University Hospital between 1999 and 2005
Classification
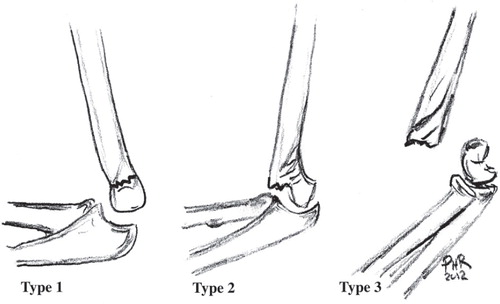
SCHF in children are classified according to the Gartland classification Citation(41). This fracture classification is based on the lateral radiological view. Undisplaced fractures are classified as type 1, displaced fractures with an intact posterior pereosteal hinge are classified as Type 2 fractures, while Type 3 fractures are completely displaced with no bony contact between the fragments (). This classification system has excellent intra- and interobserver reliability (overall kappa value of 0.74 for interobserver reliability) Citation(6). Most fractures (97–99%) are extension type fractures where the distal fragment is tilted posteriorly Citation(86) .
Management
Undisplaced SCHFs are treated conservatively in an above elbow plaster in 3 to 4 weeks, and complications are very rare Citation(81). Traditionally displaced fractures have been managed with closed reduction and immobilization in plaster. However, to maintain reduction, the elbow must be immobilized in more than 90° of flexion. This increases the risk of ischemia of the anterior cubital fossa (Volkmann’s ischemia) Citation(96) and malunion in cubitus varus Citation(53). Open surgery is generally not recommended for SCHFs Citation(34;41).
Management by traction was introduced by John Dunlop in the 1930s, with good functional results Citation(27). Traction can be done laterally Citation(27;108) or overhead Citation(1;73;122;157). The method avoids the risk of deep infections or iatrogenic neurovascular injury Citation(26), but still up to a third of the fractures malunite in varus Citation(114). Traction reduces the rate of ischemic injury compared to immobilization in plaster alone Citation(1;81).
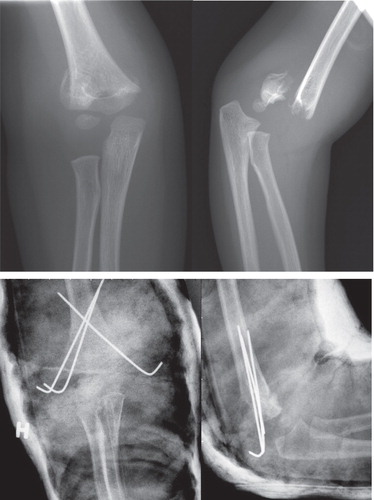
Percutaneous pinning of SCHFs was first described by Judet in 1947 Citation(64) (). It is now considered the gold standard for management of SCHFs in children Citation(34;35;114;145). The method allows for better control of the bone fragments. The arm does not have to be immobilized in acute flexion, reducing the risk of compartment syndrome with subsequent development of Volkmann’s ischemic contracture Citation(36). The plaster and the pins are removed after three to four weeks.
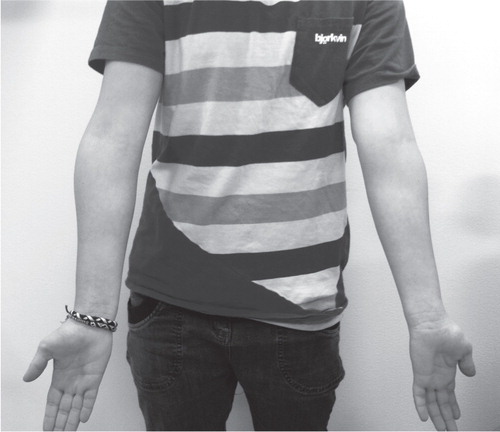
Cubitus varus
The physiological carrying angle of the elbow (cubitus angle) varies from 3° to 29° Citation(139). Girls usually have a more pronounced carrying angle than boys. After SCHF the valgus angle tend to decrease. If the valgus angle is lost altogether, the deformity is referred to as cubitus varus, also known as the gunstock deformity (). Cubitus varus is caused by insufficient reduction of the fracture and not a growth disturbance of the medial physis as previously thought Citation(133). The incidence of cubitus varus after conservative management of displaced fractures (Gartland type 2 and 3) was historically relatively high Citation(88), and it has been reported to be lower after CRPP than after management in traction Citation(114). It is still the most common permanent complication after displaced SCHFs, but it is mainly a cosmetic concern. Little dysfunction as a result of cubitus varus has been reported in the literature Citation(69;132;156;157), although some authors have reported an increased risk of lateral condyl fractures and posterolateral instability after severe cubitus varus deformities Citation(2;102). In Paper 2 we found that 14% (11 of 78) had developed the cubitus varus malunion. This might be seen as an unacceptable high percentage. A study from England of 291 SCHFs reported that only 3% of patients developed the cubitus varus malunion Citation(87). However, in this study the patients were not re-examined, only children who contacted the institution because of concerns regarding the malunion were identified. This introduces a significant risk of selection bias, especially when we know that this condition is well tolerated with little physical complaints. In our study, several of the eleven patients with cubitus varus of the elbow as measured with a goniometer were not aware of the condition before the follow-up examination.
Figure 10. Cubitus varus after a supracondylar humerus fracture of the right elbow. The patient had no functional complaints, normal neurovascular status and had a Quick-DASH score of 0 four years after injury.
When measuring the outcome after SCHFs, the Flynn’s criteria is commonly used Citation(34). It is divided in two parts or factors; the cosmetic factor and the functional factor (). This simple scoring system makes comparison between studies possible, but the outcome measure has some limitation. It does not take into consideration any pain, neurovascular complications or ability to perform daily activities or partake in sports. In addition, the cosmetic factor defines cubitus varus as a poor result by definition. However, the natural carrying angle varies greatly between individuals Citation(139). Some patients in our study had a natural carrying angle of less than 5 degrees. A loss of five degrees would place the results in the category for poor results, while other subjects with the same loss of angle would be classified as having an excellent result. In our study, All 11 patients with a cubitus varus malunion was by definition classified as a poor result according to the cosmetic factor of Flynn’s criteria, but only 4 has a poor result according to the functional factor.
Table 3. Flynn’s criteria for grading functional and cosmetic outcome of supracondylar humerus fractures in children Citation(34). Values are degrees
We also used the validated Quick DASH outcome score Citation(32) to measure the outcome in our patients. Unlike Flynn’s criteria, this outcome measure considers pain, discomfort and the ability to perform daily activity and partake in sports or play musical instruments. Only twenty patients (25%) had a positive Quick-DASH score, with a median value of 0 and a mean value of 0.51. We conclude that this commonly used outcome measure is inappropriate to measure the outcome after pinning of supracondylar humerus fractures in children in a modern clinical setting, because the Quick-DASH is not sensitive enough to measure the small variability in the otherwise excellent outcome.
Although the cubitus varus seems to be a benign complication, it is not without concern for the patients. The mean VAS score was significantly lower among patients who developed cubitus varus (7.7 vs. 9.6) compared with patients who ended up with a positive carrying angle (p < 0.001). The VAS score we used was a subjective global satisfaction score, asking the question: How satisfied are you with the results of your elbow today? A score of 0 indicated that the patient felt that the result after surgery was “the worst imaginable” and a score of 10 indicated a perfect result, “as good as the uninjured arm”. However, there was no difference in range of motion as measured by a goniometer between the group of patients with a cubitus varus malunion and the rest.
Volkmann’s ischemia
Displaced SCHFs have historically been associated with a relatively high incidence of severe complications, such as the Volkmann’s Ischemia with subsequent flexion deformity of the forearm known as Volkmann’s ischemic contracture Citation(96). It occurs after compartment syndrome of the cubital fossa due to injury to the brachial artery or as a consequent of post ischemic oedema. The subsequent contracture results from necrosis of the flexor muscles of the forearm. In our study (Paper 2) there were no cases of permanent neurovascular injury or compartment syndrome. There were ten cases of transient neurological deficit, but only one postoperative nerve injury was considered severe. This was a patient with loss of both sensory and motoric ulnar nerve function which was explored three months later. The nerve was found intact, and the pin holes indicated that the pins had not injured the ulnar nerve. The function returned spontaneously two months after the exploration. Our results support the notion that severe neurovascular complications after CRPP of displaced SCHFs are rare. Between 2001 and 2007 the Rikshospitalet University Hospital in Oslo received only five children with compromised distal vascular status after CRPP of displaced SCHFs operated at other hospitals. The elbows were explored, and the brachial artery was found entrapped in the fracture in all five patients. At follow-up over a year later all had excellent function, normal range of motion and intact neurovascular status Citation(121). Another study identified 11 patients who had developed compartment syndrome after a displaced SCHF Citation(116). The average time from injury to surgery was 22 hours. To find the patients, the authors had to search the medical files of eight hospitals in three countries for the period 1995-2005, illustrating how rare such complications have become.
A preoperatively neurovascular compromised arm is a sign of a potential vascular injury, but angiography is not indicated initially, as this is time consuming and does not alter management Citation(47). In the presence of a pulseless limb, closed reduction and percutaneous pinning should be performed as quickly as possible Citation(13). The absent pulse might be caused by vascular injury, thrombosis, aneurism or the entrapment of brachial artery in the fracture Citation(19;82;99;121), but the most common cause of a pulseless limb after a SCHF is vascular spasm Citation(49). In most cases the pulse returns after the fracture is reduced. Some authors recommend exploration of the artery if the extremity remains pulseless after CRPP Citation(19). The artery might simply be stuck in the fracture, and it is therefore worth redoing the CRPP to see if the pulse returns, before exploring the artery Citation(121). But if the extremity is pulseless, cold and white after CRPP, the artery should be explored quickly. The management of a pulseless, but warm and pink arm is more controversial Citation(72). A review of the literature conclude that a pink, pulseless hand following CRPP of a SCHF can be treated expectantly, unless other symptoms of neurovascular compromise develop, in which case urgent exploration of the artery should be undertaken Citation(47). The introduction of CRPP as standard management has greatly reduced the risk of Volkmann’s ischemia following a SCHF Citation(34;109;143).
We could not find any convincing prognostic factors for an inferior outcome in our study. We tried four different outcome variables, and the effect of timing of the surgery (night-time or daytime), was the only significant finding (p = 0.01). Our main outcome, the VAS score, is a subjective measurement of global satisfaction, and could be influenced by other factors than the surgical treatment. Perhaps patients (or parents) who were operated at night were more satisfied simply because they did not have to wait until the next morning. Apart from that, we did not find any associated risk of inferior outcome associated with time to surgery, hence delayed surgical treatment of these fractures to the next day seems safe. However, since the majority of the variance in outcome is unexplained, and almost a quarter of the explainable variance can be attributed to the surgeon, the level of evidence remains rather weak. We therefore agree with the authors who still recommend considering Gartland 3 supracondylar fractures an orthopaedic emergency Citation(80;104;116;146), especially in cases with symptoms of neurovascular compromise.
Epidemiology and fracture risk
Epidemiology of childhood fractures
The last study of the thesis found an overall fracture incidence of 180.1 fractures per 10,000 children younger than 16 years (Paper 4). This is comparable with other reports from Scandinavia and Great Britain Citation(9;18;52;84;144).
As children grow older and are able to spend more time outdoors, they try new and various activities and the number of fractures increase. The mechanism of injury varies accordingly. For example, older children tend to fracture during more complex activities, such as alpine skiing and soccer, while young children sustain fractures from simple falls at the playground. The difference in preferred activities increases also between girls and boys as they grow older. For example, in our material, only girls sustained fractures from horseback riding, which is much more popular among girls than boys.
In the 1990s, a decrease in paediatric fracture incidence was described in Sweden Citation(144). This decrease came after the monumental increase in fracture incidence between 1950 and 1979 described by Landin, attributed to an increased participation in sport. It is difficult to decide whether the incidence of paediatric fractures has decreased or increased in our region, as there are no previous reports to compare with. The results indicate however that the fracture incidence have stabilized during the last decade. The annual incidence in our material is lower than the report from Brudvik and Hove, who reported an annual incidence of 245 fractures per 10,000 children younger than 16 years in Bergen, Norway in 1998 Citation(9). Methodological differences are unlikely to explain this difference fully, as these studies were very similar in design. Brudvik and Hove reported that most fractures occurred in children aged 12–16 years, while we found that most fractures occurred in children aged 6–12 years. An increase in sport activity has been reported for 9-year old Norwegian children between 1999 and 2005 Citation(70). It is possible that in the decade that has passed since Brudvik and Hove conducted their study, children are exposing themselves to fracture risk at an increasingly younger age. Climate has been reported to influence fracture incidence, and could also in part explain the difference Citation(89;107). Bergen is on the west coast of Norway, enjoying a wet and rainy climate, compared to the dry inland climate of Akershus. The seasonal variation we observed, with peaks in May-June and August-September, is similar to the variation registered in Umeå, Sweden, by Hedström et al. Citation(52). In our study a variation in the distribution of fractures by time of day between winter and summer was demonstrated. In summer, when the afternoons are long and bright, most fractures occurred after school, while during winter, most fractures occurred during school hours. These findings might seem obvious, but are nevertheless important to consider when preparing healthcare services and preventive measures.
Fracture rates of various childhood activities
Most preventable childhood fractures occur during sports and recreational activities. To be able to implement effective preventive measures, it is important to identify high-risk activities. In our study soccer was the activity that caused most fractures (). However, soccer is also the most popular sport among children. It is therefore crucial to estimate the fracture rate for various activities, as this takes into account the exposure time to the activity. We found that the fracture rates per exposure-time differ between various sport and recreational activities (). Our results correspond well with the injury rate of 1.7 per10,000 hours of exposure reported by Spinks et al. Citation(137). In this study, the authors included all injuries that received treatment, either from a local doctor, an emergency department, a dentist or a physiotherapist. The injuries are not described in further detail, but we must assume that sprains and soft tissue injuries were included as well as fractures.
Table 4. Most common fractures by most common sport activity. Values are number (%). (From Paper 4) Copyright The Journal of Bone and Joint Surgery [Am]. Reprinted with permission
Table 5. Fracture rate estimates for common children activities. Estimates number of fractures per 104 hours of activity. Confidence interval assuming Poisson distribution of fractures (From Paper 4) Copyright The Journal of Bone and Joint Surgery [Am], reprinted with permission
About one third of injuries associated with childhood activities are fractures Citation(8), explaining the 3 times higher injury rate reported by Spinks et al compared to the fracture rates in our study. Snowboarding had the highest fracture rate, five times higher than the fracture rate for trampolining and four times higher than the fracture rate for soccer. Snowboarding has become an increasingly popular sport, and the snowboard-related trauma incidence has increased accordingly Citation(51). Furthermore, 77% of fractures sustained on snowboards are fractures of the distal radius, and 58% of snowboard related fractures occurred in boys aged 12–16 years (). Our results are in accordance with the literature Citation(50;85). This information should propel an increased effort to implement the use of wrist-protectors towards this subgroup of children where preventive measures are likely to be effective Citation(123).
The increase in trampoline injuries seen in emergency departments has caused some authors to recommend that trampolines should be banned Citation(28;40;59). However, reports on trampoline injuries have not considered exposure time, or the possible positive effects of trampolining. Our results indicate that the trampoline-associated fracture rate is lower than that of handball or soccer. Trampolines have become increasingly common, and it would be logical to expect an increase in trampoline related injuries over time. In Paper IV we found that the most common cause of distal humerus fractures in children during 2010–2011 was a fall from playground equipment, followed by trampolining. 25% of all trampoline related fractures was a fracture of the distal humerus, while 17% of all distal humerus fractures was caused by a fall on or off a trampoline. This is in line with the results from the retrospective study of supracondylar humerus fractures treated between 1999 and 2006 (Paper II), where the most common cause of injury was a fall on or off a trampoline (19%) (). There is no clear evidence to say that trampoline related fractures have increased during the last decade. Perhaps effective measures have been successful, such as the use of safety nets and avoiding multiple users, all of which have proven effective Citation(101;120;155). We therefore believe there is currently not enough evidence to support a ban of the use of recreational trampolines.
Paediatric fractures in a socioeconomic perspective
Prevention of injury is obviously always preferable, both from the point of view of the children and parents and in a socioeconomic perspective. We believe there is great potential to reduce the number of paediatric fractures by implementing preventive strategies. But the management of childhood fractures will always be a major task for fracture clinics, as long as there are playgrounds, ski slopes, soccer fields and trees to climb in. In addition to effective preventive strategies, we must therefore also look for the most effective way to handle paediatric fractures in the clinic, without risking adverse outcomes.
In Paper 1 we investigate the stability, remodelling and follow-up routine of the most common paediatric fracture (distal radius) Citation(118), another study measures the reliability of the most commonly used classification for distal radius fractures in children (Paper III) Citation(117). A third study examines the outcome after operative management of elbow fractures in children (Paper 2) Citation(119). The results of these studies provide useful knowledge to improve the treatment for these patients and to reduce expenses in the health care system. The last study in this thesis investigates the epidemiology and fracture rates for various popular childhood activities (Paper 4), and provides healthcare managers, politicians, trainers, teachers, parents and clinicians with important information that help identify and facilitate the implementation of effective preventive measures to reduce paediatric fractures.
Every clinic should have proper written protocols for the managements of common fractures. Such protocols have been demonstrated to reduce the need for fracture clinic attendance Citation(66). Our results support the notion that wrist fractures in childhood are benign.. In Paper 1, 68% (208) of the 305 distal radius fractures were classified as buckle fractures, which we have demonstrated are stable fractures without need for further follow up. However, stable distal radius fractures in children are extensively monitored with both clinical and radiological follow ups Citation(46;118). In our study of 105 consecutive fractures (Paper 3), 65 fractures were by consensus defined as buckle fractures. These stable fractures were given a total of 72 clinical follow-up examinations and 34 further radiological examinations. These unnecessary follow-ups could have been avoided with more focus on the fracture classification and better supervision. It has been demonstrated that proper treatment algorithms managed by experienced orthopaedic surgeons will reduce the costs of managing paediatric fractures Citation(128;134). We demonstrated that junior registrars had statistically significant lower kappa value for interobserver reliability than the more experienced raters. They placed fewer fractures in the buckle group, and rated more fractures as greenstick or physeal injuries. There is much to be gained if treating physicians distinguish between buckle and greenstick fractures. Between March 2010 and March 2011 436 paediatric distal radius fractures were treated at our institution (Paper 4). Around 300 of these would be buckle fractures. Our institution alone can therefore potentially avoid over 330 unnecessary clinical follow-ups and around 150 radiological follow-ups every year. The costs for unnecessary fracture clinic appointments are both direct and indirect. The direct costs are the hospitals expenses, everything from salary, equipment, electricity, maintenance, infrastructure etc. This was estimated in 2006 to 1300 NOK (173 Euros) for a consultation and 500 NOK per radiological examination Citation(38). However, in Norway the Consumer Price Index has increased with over 10% between 2006 and 2011 Citation(138), indicating that our institution could save over 550,000 NOK in direct costs annually. In addition there will be a tremendous reduction in indirect costs, such as the cost of parents taking time off work to accompany the child to the clinic, transportation, time away from school and activities for the child etc. These costs are more difficult to estimate. In a report of the epidemiology of childhood fractures in Stavanger, Norway, the authors found an average restriction from activities of 26 days for fractures in the lower extremities Citation(71). A study from Sheffield, England, estimated the indirect cost of attending a paediatric fracture clinic to 0.25 work days, 0.18 days wages, and 0.54 days schooling Citation(93). This represents tremendous costs for society, especially when considering the high incidence of childhood fractures, estimated to be 180.1 / 10,000 children in our study (Paper 4).
Percutaneous pinning of displaced supracondylar humerus fractures in children is now gold standard, but treatment by traction has been common until relatively recently. CRPP for SCHF is also a preferred method from a socioeconomic point of view. The median stay in hospital in our material (Paper 2) was 1 day. A study from Bergen, Norway, reported a median stay in hospital of 11 days for children treated with overhead traction Citation(157). The cost of an overnight stay in our institution is estimated to 9,000 NOK Citation(60). The difference of 10 overnight stays implies that it is 90,000 NOK cheaper to manage these fractures by CRPP rather than traction. Additional costs would include the time away from work for the parents (children don’t stay in hospital alone anymore) and time away from school for the child. This difference in costs between CRPP and traction for SCHF in children has also been found by others Citation(114). The small risk of iatrogenic neurovascular injury and pin infection is clearly outweighed by this difference in expenses.
Furthermore, our results support the notion that there is no need for a clinical follow-up between hospital discharge and plaster and pin removal. Nor is it necessary for a follow-up some weeks after pin removal. The elbow is often quite stiff on the day the pins and the plaster are removed, but physiotherapy is not necessary. 90% of the normal range of motion is regained after five weeks without physical therapy Citation(149), and further improvement can be expected for another 12 months after injury Citation(158). This is consistent with John Gartland’s clinical experience. In his classic paper published in 1959 he writes: ”Formal physical therapy is not required (…) Children possess their own special brand of magic and will regain full function if left to their own devices” Citation(41).
Although there is potential to reduce the expenses of paediatric fracture management without compromising the safety of patient follow-up, the optimal goal would still be prevention of injury. In paper 4 we estimate fracture rates for various childhood activities in the same population based on exposure time. To the best of our knowledge this has not previously been done. This information identifies high risk sports, most notably snowboarding with a fourfold increase in fracture rate compared to other activities. As discussed previously, preventive measures should be developed to reduce the risk of wrist fractures in children on snowboards. But our results should also be used to debate whether activities with low fracture rates should be targeted for preventive measures. Prevention in sports with lower fracture rate might outweigh the benefits of physical activity, especially if the preventive measures are decreasing the level of physical activity.
Conclusions
The distal radius is the most common fracture in childhood.
Buckle fractures of the distal radial metaphysis in children are stable, and don’t need follow-up. Management consists of immobilization for comfort, in a splint that is removable by the parents after three weeks.
Greenstick fractures of the distal radius are unstable, and continue to displace also after the first two weeks in plaster.
The classification of fractures of the distal radius in children tested in this study is reliable and reproducible, but varies according to the experience of the raters. More focus on the different fracture categories and better supervision of our younger colleges by experienced raters will reduce the number of unnecessary clinical and radiological follow-up appointments.
Closed reduction and percutaneous pinning (CRPP) of displaced supracondylar humerus fractures (SCHFs) in children is a safe method with excellent results for the vast majority of patients.
Cubitus varus is the most common permanent complication after CRPP of displaced SCHFs in children. Cubitus varus is mainly a cosmetic concern.
We found that 25% of the variance in outcome after CRPP of SCHFs in children could be attributed to between-surgeon variance.
In observational studies in orthopaedics, standard statistical methods, such as an Ordinary Leasts-Squares regression model, might lead to wrong conclusions. We have demonstrated that even in a case with low level of explained variance, the use of models that more accurately reflect reality (effect modifiers, two levels) affects conclusions.
The fracture rates differ between various physical activities. The fracture rate for snowboarding is four times higher compared to other common childhood sport and recreational activities.
The fracture rate for trampoline is comparable or lower than that of handball, soccer and skiing.
Perspectives for the future
An increased focus on the simple fracture classification of paediatric distal radius fractures is recommendable. Buckle fractures do not need follow up, and a great amount of unnecessary clinical and radiological follow-up appointments can be avoided every year by making supervision by senior colleagues available to help classify these simple fractures.
Future observational studies in orthopaedics must consider inclusion of interaction terms before performing the analyses. Further, since surgery is two-level in nature, the need for a two-level model should always be explored by calculating the intraclass correlation coefficient (ICC). This is possible even in relatively small materials. Statistically significant findings in previous studies where an OLS model without effect modifiers has been used, and where the conclusions have had impact on clinical practice, should be reviewed using more sophisticated methods.
A considerable amount of paediatric fractures occurs during sport and recreational activities. The fracture incidence in the paediatric population remains unacceptable high, and preventive measures should be implemented through national campaigns. The epidemiology of paediatric fractures is well described, but there are still few reports on fracture rates that take exposure time into consideration. More detailed studies of the high risk sports such as snowboard, soccer, handball, playground and alpine skiing are needed to describe the injury situation to be able to intervene with meaningful effective preventive measures.
This PhD has focused on the fracture risk of various childhood activities. More studies are needed to identify the individual children at risk for fracture. Studies on bone mineral density, hormonal status, environment, behavioural (psychological) and motor skills should be undertaken to help identify children at risk for fractures.
References
- Aamodt A, Gronmark T. Suprakondylære humerusfrakturer hos barn. Tidsskr Nor Laegeforen 1991; 111(10): 1240-2.
- Abe M, Ishizu T, Shirai H, Okamoto M, Onomura T. Tardy ulnar nerve palsy caused by cubitus varus deformity. J Hand Surg Am 1995; 20(1): 5-9.
- Al-Ansari K, Howard A, Seeto B, Yoo S, Zaki S, Boutis K. Minimally angulated pediatric wrist fractures: is immobilization without manipulation enough? CJEM 2007; 9(1): 9-15.
- Audige L, Bhandari M, Kellam J. How reliable are reliability studies of fracture classifications? A systematic review of their methodologies. Acta Orthop Scand 2004; 75(2): 184-94.
- Bailey DA, Wedge JH, McCulloch RG, Martin AD, Bernhardson SC. Epidemiology of fractures of the distal end of the radius in children as associated with growth. J Bone Joint Surg Am 1989; 71(8): 1225-31.
- Barton KL, Kaminsky CK, Green DW, Shean CJ, Kautz SM, Skaggs DL. Reliability of a modified Gartland classification of supracondylar humerus fractures. J Pediatr Orthop 2001; 21(1): 27-30.
- Bratlid D. [Children as research subjects--have we exceeded one or two principles?]. Tidsskr Nor Laegeforen 2004 19; 124(4): 510-2.
- Brudvik C. Child injuries in Bergen, Norway. Injury 2000; 31(10): 761-7.
- Brudvik C, Hove LM. Childhood fractures in Bergen, Norway: identifying high-risk groups and activities. J Pediatr Orthop 2003; 23(5): 629-34.
- Byard RW, James RA, Gilbert JD. Childhood sporting deaths. Am J Forensic Med Pathol 2002; 23(4): 364-7.
- Caine D, DiFiori J, Maffulli N. Physeal injuries in children's and youth sports: reasons for concern? Br J Sports Med 2006; 40(9): 749-60.
- Cannata G, De MF, Mancini F, Ippolito E. Physeal fractures of the distal radius and ulna: long-term prognosis. J Orthop Trauma 2003; 17(3): 172-9.
- Cheng JC, Lam TP, Shen WY. Closed reduction and percutaneous pinning for type III displaced supracondylar fractures of the humerus in children. J Orthop Trauma 1995; 9(6): 511-5.
- Cheng JC, Shen WY. Limb fracture pattern in different pediatric age groups: a study of 3,350 children. J Orthop Trauma 1993; 7(1): 15-22.
- Cho SH. Using multilevel analysis in patient and organizational outcomes research. Nurs Res 2003 Jan; 52(1): 61-5.
- Cohen J. A coefficient of agreement for nominal scales. Educ Psychol meas 1960; 20: 37-46.
- Conn JM, Annest JL, Gilchrist J. Sports and recreation related injury episodes in the US population, 1997-99. Inj Prev 2003; 9(2): 117-23.
- Cooper C, Dennison EM, Leufkens HG, Bishop N, van Staa TP. Epidemiology of childhood fractures in Britain: a study using the general practice research database. J Bone Miner Res 2004; 19(12): 1976-81.
- Copley LA, Dormans JP, Davidson RS. Vascular injuries and their sequelae in pediatric supracondylar humeral fractures: toward a goal of prevention. J Pediatr Orthop 1996; 16(1): 99-103.
- Davidson AJ, O'Brien M. Ethics and medical research in children. Paediatr Anaesth 2009; 19(10): 994-1004.
- Davidson JS, Brown DJ, Barnes SN, Bruce CE. Simple treatment for torus fractures of the distal radius. J Bone Joint Surg Br 2001; 83(8): 1173-5.
- de Loës M. Exposure data. Why are they needed? Sports Med 1997; 24(3): 172-5.
- de Loës M, Goldie I. Incidence rate of injuries during sport activity and physical exercise in a rural Swedish municipality: incidence rates in 17 sports. Int J Sports Med 1988; 9(6): 461-7.
- Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health 2000; 21: 171-92.
- Do TT, Strub WM, Foad SL, Mehlman CT, Crawford AH. Reduction versus remodeling in pediatric distal forearm fractures: a preliminary cost analysis. J Pediatr Orthop B 2003; 12(2): 109-15.
- Dodge HS. Displaced supracondylar fractures of the humerus in children--treatment by Dunlop's traction. J Bone Joint Surg Am 1972; 54(7): 1408-18.
- Dunlop J. Transconcylar fractures of the humerus in childhood. J Bone Joint Surg Am 1939; 21(1): 59-73.
- Eberl R, Schalamon J, Singer G, Huber SS, Spitzer P, Hollwarth ME. Trampoline-related injuries in childhood. Eur J Pediatr 2009; 168(10): 1171-4.
- Emery CA, Meeuwisse WH. Risk factors for injury in indoor compared with outdoor adolescent soccer. Am J Sports Med 2006; 34(10): 1636-42.
- Farbman KS, Vinci RJ, Cranley WR, Creevy WR, Bauchner H. The role of serial radiographs in the management of pediatric torus fractures. Arch Pediatr Adolesc Med 1999; 153(9): 923-5.
- Fernald DH, Coombs L, DeAlleaume L, West D, Parnes B. An assessment of the Hawthorne Effect in practice-based research. J Am Board Fam Med 2012; 25(1): 83-6.
- Finsen V. [Norwegian version of the DASH questionnaire for examination of the arm shoulders and hand]. Tidsskr Nor Laegeforen 2008; 128(9): 1070.
- Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull 1971; 86: 378-82.
- Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years' experience with long-term follow-up. J Bone Joint Surg Am 1974; 56(2): 263-72.
- Foead A, Penafort R, Saw A, Sengupta S. Comparison of two methods of percutaneous pin fixation in displaced supracondylar fractures of the humerus in children. J Orthop Surg (Hong Kong) 2004; 12(1): 76-82.
- France J, Strong M. Deformity and function in supracondylar fractures of the humerus in children variously treated by closed reduction and splinting, traction, and percutaneous pinning. J Pediatr Orthop 1992; 12(4): 494-8.
- Friberg KS. Remodelling after distal forearm fractures in children. II. The final orientation of the distal and proximal epiphyseal plates of the radius. Acta Orthop Scand 1979; 50(6 Pt 2): 731-9.
- Frihagen F, Waaler GM, Madsen JE, Nordsletten L, Aspaas S, Aas E. The cost of hemiarthroplasty compared to that of internal fixation for femoral neck fractures. 2-year results involving 222 patients based on a randomized controlled trial. Acta Orthop 2010; 81(4): 446-52.
- Fuller DJ, McCullough CJ. Malunited fractures of the forearm in children. J Bone Joint Surg Br 1982; 64(3): 364-7.
- Furnival RA, Street KA, Schunk JE. Too many pediatric trampoline injuries. Pediatrics 1999; 103(5): e57.
- Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet 1959; 109(2): 145-54.
- Gelber AC, Hochberg MC, Mead LA, Wang NY, Wigley FM, Klag MJ. Joint injury in young adults and risk for subsequent knee and hip osteoarthritis. Ann Intern Med 2000 5; 133(5): 321-8.
- Goulding A. Risk factors for fractures in normally active children and adolescents. Med Sport Sci 2007; 51: 102-20.
- Goulding A, Grant AM, Williams SM. Bone and body composition of children and adolescents with repeated forearm fractures. J Bone Miner Res 2005; 20(12): 2090-6.
- Goulding A, Jones IE, Taylor RW, Manning PJ, Williams SM. More broken bones: a 4-year double cohort study of young girls with and without distal forearm fractures. J Bone Miner Res 2000; 15(10): 2011-8.
- Green JS, Williams SC, Finlay D, Harper WM. Distal forearm fractures in children: the role of radiographs during follow up. Injury 1998; 29(4): 309-12.
- Griffin KJ, Walsh SR, Markar S, Tang TY, Boyle JR, Hayes PD. The pink pulseless hand: a review of the literature regarding management of vascular complications of supracondylar humeral fractures in children. Eur J Vasc Endovasc Surg 2008; 36(6): 697-702.
- Hagino H, Yamamoto K, Ohshiro H, Nose T. Increasing incidence of distal radius fractures in Japanese children and adolescents. J Orthop Sci 2000; 5(4): 356-60.
- Harris IE. Supracondylar fractures of the humerus in children. Orthopedics 1992; 15(7): 811-7.
- Hasler RM, Berov S, Benneker L, Dubler S, Spycher J, Heim D, et al. Are there risk factors for snowboard injuries? A case-control multicentre study of 559 snowboarders. Br J Sports Med 2010; 44(11): 816-21.
- Hayes JR, Groner JI. The increasing incidence of snowboard-related trauma. J Pediatr Surg 2008; 43(5): 928-30.
- Hedstrom EM, Svensson O, Bergstrom U, Michno P. Epidemiology of fractures in children and adolescents. Acta Orthop 2010; 81(1): 148-53.
- Henrikson B. Supracondylar fracture of the humerus in children. A late review of end-results with special reference to the cause of deformity, disability and complications. Acta Chir Scand Suppl 1966; 369: 1-72.
- Hills AP, King NA, Armstrong TP. The contribution of physical activity and sedentary behaviours to the growth and development of children and adolescents: implications for overweight and obesity. Sports Med 2007; 37(6): 533-45.
- Hoff GL, Martin TA. Outdoor and indoor soccer: injuries among youth players. Am J Sports Med 1986 May; 14(3): 231-3.
- Hoppe DJ, Schemitsch EH, Morshed S, Tornetta P, III, Bhandari M. Hierarchy of evidence: where observational studies fit in and why we need them. J Bone Joint Surg Am 2009 May; 91 Suppl 3: 2-9.
- Horn J, Kristiansen LP, Steen H. Partial physeal arrest after temporary transphyseal pinning – a case report. Acta Orthop 2008; 79(6): 867-9.
- Hove LM, Brudvik C. Displaced paediatric fractures of the distal radius. Arch Orthop Trauma Surg 2008; 128(1): 55-60.
- Hurson C, Browne K, Callender O, O'Donnell T, O'Neill A, Moore DP, et al. Pediatric trampoline injuries. J Pediatr Orthop 2007; 27(7): 729-32.
- Huseby BM (red). Samdata rapport spesialisthelsetjenesten 2010. Oslo: Helsedirektoratet; 2011 Nov 1.
- Johari AN, Sinha M. Remodeling of forearm fractures in children. J Pediatr Orthop B 1999; 8(2): 84-7.
- Jones IE, Cannan R, Goulding A. Distal forearm fractures in New Zealand children: annual rates in a geographically defined area. N Z Med J 2000; 113(1120): 443-5.
- Jones IE, Williams SM, Dow N, Goulding A. How many children remain fracture-free during growth? A longitudinal study of children and adolescents participating in the Dunedin Multidisciplinary Health and Development Study. Osteoporos Int 2002; 13(12): 990-5.
- Judet J. Traitement des fractures épiphysaires de l'enfant par broche transarticulaire. Mém Acad Chir 1947; 73: 562-6.
- Juliusson PB, Eide GE, Roelants M, Waaler PE, Hauspie R, Bjerknes R. Overweight and obesity in Norwegian children: prevalence and socio-demographic risk factors. Acta Paediatr 2010 Jun; 99(6): 900-5.
- Kakarlapudi TK, Santini A, Shahane SA, Douglas D. The cost of treatment of distal radial fractures. Injury 2000; 31(4): 229-32.
- Khosla S, Melton LJ, III, Dekutoski MB, Achenbach SJ, Oberg AL, Riggs BL. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA 2003 17; 290(11): 1479-85.
- Knowles SB, Marshall SW, Guskiewicz KM. Issues in estimating risks and rates in sports injury research. J Athl Train 2006; 41(2): 207-15.
- Kocher MS, Kasser JR, Waters PM, Bae D, Snyder BD, Hresko MT, et al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial. J Bone Joint Surg Am 2007; 89(4): 706-12.
- Kolle E, Steene-Johannessen J, Klasson-Heggebo L, Andersen LB, Anderssen SA. A 5-yr change in Norwegian 9-yr-olds' objectively assessed physical activity level. Med Sci Sports Exerc 2009; 41(7): 1368-73.
- Kopjar B, Wickizer TM. Fractures among children: incidence and impact on daily activities. Inj Prev 1998; 4(3): 194-7.
- Korompilias AV, Lykissas MG, Mitsionis GI, Kontogeorgakos VA, Manoudis G, Beris AE. Treatment of pink pulseless hand following supracondylar fractures of the humerus in children. Int Orthop 2009; 33(1): 237-41.
- Kramhoft M, Keller IL, Solgaard S. Displaced supracondylar fractures of the humerus in children. Clin Orthop 1987; (221): 215-20.
- Kreder HJ, Hanel DP, McKee M, Jupiter J, McGillivary G, Swiontkowski MF. Consistency of AO fracture classification for the distal radius. J Bone Joint Surg Br 1996; 78(5): 726-31.
- Landin LA. Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950-1979. Acta Orthop Scand Suppl 1983; (202): 1-109.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33(1): 159-74.
- Lautman S, Bergerault F, Saidani N, Bonnard C. Roentgenographic measurement of angle between shaft and distal epiphyseal growth plate of radius. J Pediatr Orthop 2002; 22(6): 751-3.
- Lee BS, Esterhai JL, Jr., Das M. Fracture of the distal radial epiphysis. Characteristics and surgical treatment of premature, post-traumatic epiphyseal closure. Clin Orthop 1984; (185): 90-6.
- Light TR, Ogden DA, Ogden JA. The anatomy of metaphyseal torus fractures. Clin Orthop 1984; (188): 103-11.
- Loizou CL, Simillis C, Hutchinson JR. A systematic review of early versus delayed treatment for type III supracondylar humeral fractures in children. Injury 2009; 40(3): 245-8.
- Lund-Kristensen J, Vibild O. Supracondylar fractures of the humerus in children. A follow-up with particular reference to late results after severely displaced fractures. Acta Orthop Scand 1976; 47(4): 375-80.
- Luria S, Sucar A, Eylon S, Pinchas-Mizrachi R, Berlatzky Y, Anner H, et al. Vascular complications of supracondylar humeral fractures in children. J Pediatr Orthop B 2007; 16(2): 133-43.
- Lyons RA, Delahunty AM, Kraus D, Heaven M, McCabe M, Allen H, et al. Children's fractures: a population based study. Inj Prev 1999 Jun; 5(2): 129-32.
- Lyons RA, Sellstrom E, Delahunty AM, Loeb M, Varilo S. Incidence and cause of fractures in European districts. Arch Dis Child 2000 Jun; 82(6): 452-5.
- Made C, Elmqvist LG. A 10-year study of snowboard injuries in Lapland Sweden. Scand J Med Sci Sports 2004 Apr; 14(2): 128-33.
- Mahan ST, May CD, Kocher MS. Operative management of displaced flexion supracondylar humerus fractures in children. J Pediatr Orthop 2007 Jul; 27(5): 551-6.
- Mangwani J, Nadarajah R, Paterson JM. Supracondylar humeral fractures in children: ten years' experience in a teaching hospital. J Bone Joint Surg Br 2006 Mar; 88(3): 362-5.
- Mann TS. Prognosis in supracondylar fractures. J Bone Joint Surg Br 1963; 45: 516-22.
- Masterson E, Borton D, O'Brien T. Victims of our climate. Injury 1993; 24(4): 247-8.
- McCarney R, Warner J, Iliffe S, van HR, Griffin M, Fisher P. The Hawthorne Effect: a randomised, controlled trial. BMC Med Res Methodol 2007; 7: 30.
- McLauchlan GJ, Cowan B, Annan IH, Robb JE. Management of completely displaced metaphyseal fractures of the distal radius in children. A prospective, randomised controlled trial. J Bone Joint Surg Br 2002; 84(3): 413-7.
- Miller BS, Taylor B, Widmann RF, Bae DS, Snyder BD, Waters PM. Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: a prospective, randomized study. J Pediatr Orthop 2005; 25(4): 490-4.
- Morris MW, Bell MJ. The socio-economical impact of paediatric fracture clinic appointments. Injury 2006; 37(5): 395-7.
- Morshed S, Tornetta P, III, Bhandari M. Analysis of observational studies: a guide to understanding statistical methods. J Bone Joint Surg Am 2009; 91 Suppl 3: 50-60.
- Moyé LA. Statistical reasoning in medicine. The intuitive p-value primer. 2nd edition ed. Springer; 2006.
- Mubarak SJ, Carroll NC. Volkmann's contracture in children: aetiology and prevention. J Bone Joint Surg Br 1979; 61-B(3): 285-93.
- Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med 2003; 13(2): 71-8.
- Nader PR, Bradley RH, Houts RM, McRitchie SL, O'Brien M. Moderate-to-vigorous physical activity from ages 9 to 15 years. JAMA 2008; 300(3): 295-305.
- Noaman HH. Microsurgical reconstruction of brachial artery injuries in displaced supracondylar fracture humerus in children. Microsurgery 2006; 26(7): 498-505.
- Noonan KJ, Price CT. Forearm and distal radius fractures in children. J Am Acad Orthop Surg 1998; 6(3): 146-56.
- Nysted M, Drogset JO. Trampoline injuries. Br J Sports Med 2006; 40(12): 984-7.
- O'Driscoll SW, Spinner RJ, McKee MD, Kibler WB, Hastings H, Morrey BF, et al. Tardy posterolateral rotatory instability of the elbow due to cubitus varus. J Bone Joint Surg Am 2001; 83-A(9): 1358-69.
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA 2006 5; 295(13): 1549-55.
- Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am 2008 May; 90(5): 1121-32.
- Otsuka NY, Kasser JR. Supracondylar Fractures of the Humerus in Children. J Am Acad Orthop Surg 1997 Jan; 5(1): 19-26.
- Parfitt AM. The two faces of growth: benefits and risks to bone integrity. Osteoporos Int 1994 Nov; 4(6): 382-98.
- Parsons N, Odumenya M, Edwards A, Lecky F, Pattison G. Modelling the effects of the weather on admissions to UK trauma units: a cross-sectional study. Emerg Med J 2011 Oct; 28(10): 851-5.
- Piggot J, Graham HK, McCoy GF. Supracondylar fractures of the humerus in children. Treatment by straight lateral traction. J Bone Joint Surg Br 1986; 68(4): 577-83.
- Pirone AM, Graham HK, Krajbich JI. Management of displaced extension-type supracondylar fractures of the humerus in children. J Bone Joint Surg Am 1988; 70(5): 641-50.
- Plint AC, Perry JJ, Correll R, Gaboury I, Lawton L. A randomized, controlled trial of removable splinting versus casting for wrist buckle fractures in children. Pediatrics 2006; 117(3): 691-7.
- Plint AC, Perry JJ, Tsang JL. Pediatric wrist buckle fractures. CJEM 2004 Nov; 6(6): 397-401.
- Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA 1999; 282(10): 958-63.
- Price CT, Scott DS, Kurzner ME, Flynn JC. Malunited forearm fractures in children. J Pediatr Orthop 1990; 10(6): 705-12.
- Prietto CA. Supracondylar fractures of the humerus. A comparative study of Dunlop's traction versus percutaneous pinning. J Bone Joint Surg Am 1979; 61(3): 425-8.
- Qairul IH, Kareem BA, Tan AB, Harwant S. Early remodeling in children's forearm fractures. Med J Malaysia 2001; 56 Suppl D: 34-7.
- Ramachandran M, Skaggs DL, Crawford HA, Eastwood DM, Lalonde FD, Vitale MG, et al. Delaying treatment of supracondylar fractures in children: has the pendulum swung too far? J Bone Joint Surg Br 2008; 90(9): 1228-33.
- Randsborg PH, Sivertsen EA. Classification of distal radius fractures in children: good inter- and intraobserver reliability, which improves with clinical experience. BMC Musculoskelet Disord 2012; 13(1): 6.
- Randsborg PH, Sivertsen EA. Distal radius fractures in children: substantial difference in stability between buckle and greenstick fractures. Acta Orthop 2009; 80(5): 585-9.
- Randsborg PH, Sivertsen EA, Skramm I, Saltyt BJ, Gulbrandsen P. The need for better analysis of observational studies in orthopedics. A retrospective study of elbow fractures in children. Acta Orthop 2010; 81(3): 377-81.
- Rattya J, Serlo W. Using a safety net and following the safety instructions could prevent half the paediatric trampoline injuries. Eur J Pediatr Surg 2008; 18(4): 261-5.
- Reigstad O, Thorkildsen R, Grimsgaard C, Reigstad A, Røkkum M. Supracondylar fractures with circulatory failure after reduction, pinning, and entrapment of the brachial artery: Excellent results more than 1 year after open exploration and revascularization. J Orthop Trauma 2011; In press.
- Rodriguez-Merchan EC. Supracondylar fractures of the humerus in children: treatment by overhead skeletal traction. Orthop Rev 1992; 21(4): 475-82.
- Ronning R, Ronning I, Gerner T, Engebretsen L. The efficacy of wrist protectors in preventing snowboarding injuries. Am J Sports Med 2001; 29(5): 581-5.
- Rothman KJ. Epidemiology An introduction. Oxford University Press; 2002.
- Ruedl G, Bilek H, Ebner H, Gabl K, Kopp M, Burtscher M. Fatalities on Austrian ski slopes during a 5-year period. Wilderness Environ Med 2011 Dec; 22(4): 326-8.
- Ryan LM, Teach SJ, Searcy K, Singer SA, Wood R, Wright JL, et al. Epidemiology of pediatric forearm fractures in Washington, DC. J Trauma 2010 Oct; 69(4 Suppl): S200-S205.
- Salter RB. Injuries of the epiphyseal plate. Instr Course Lect 1992; 41: 351-9.
- Sawyer JR, Ivie CB, Huff AL, Wheeler C, Kelly DM, Beaty JH, et al. Emergency room visits by pediatric fracture patients treated with cast immobilization. J Pediatr Orthop 2010 Apr; 30(3): 248-52.
- Schock CC. “The crooked straight”: distal radial remodeling. J Ark Med Soc 1987 Jul; 84(2): 97-100.
- Singer B, Ryff C. New Horizons in Health: An Integrative Approach. Wahington DC: National Academy Press; 2000.
- Sivertsen EA, Randsborg PH. Distale radiusfrakturer hos barn: Epidemiologi, behandling og resultater. Oslo: Norsk Ortopedisk Forenings Høstmøte; 2009.
- Skaggs DL, Cluck MW, Mostofi A, Flynn JM, Kay RM. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg Am 2004 Apr; 86-A(4): 702-7.
- Smith L. Deformity following supracondylar fractures of the humerus. Journal of Bone and Joint Surgery American Volume 1960; 42 A(Mar): 235-52.
- Smith JT, Price C, Stevens PM, Masters KS, Young M. Does pediatric orthopedic subspecialization affect hospital utilization and charges? J Pediatr Orthop 1999 Jul; 19(4): 553-5.
- Solan MC, Rees R, Daly K. Current management of torus fractures of the distal radius. Injury 2002; 33(6): 503-5.
- Spinks AB, McClure RJ. Quantifying the risk of sports injury: a systematic review of activity-specific rates for children under 16 years of age. Br J Sports Med 2007; 41(9): 548-57.
- Spinks AB, McClure RJ, Bain C, Macpherson AK. Quantifying the association between physical activity and injury in primary school-aged children. Pediatrics 2006; 118(1): e43-e50.
- Statistics Norway. www.ssb.no. 2011. 1-9-2011. Ref Type: Online Source
- Steel FL, Tomlinson JD. The carrying angle in man. J Anat 1958; 92(2): 315-7.
- Stoffelen D, Broos P. Minimally displaced distal radius fractures: do they need plaster treatment? J Trauma 1998; 44(3): 503-5.
- Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, et al. Evidence based physical activity for school-age youth. J Pediatr 2005; 146(6): 732-7.
- Svanholm H, Starklint H, Gundersen HJ, Fabricius J, Barlebo H, Olsen S. Reproducibility of histomorphologic diagnoses with special reference to the kappa statistic. APMIS 1989; 97(8): 689-98.
- Swenson AL. The treatment of supracondylar fractures of the humerus by Kirschner-wire transfixion. J Bone Joint Surg Am 1948; 30A(4): 993-7.
- Tiderius CJ, Landin L, Duppe H. Decreasing incidence of fractures in children: an epidemiological analysis of 1,673 fractures in Malmo, Sweden, 1993-1994. Acta Orthop Scand 1999; 70(6): 622-6.
- Topping RE, Blanco JS, Davis TJ. Clinical evaluation of crossed-pin versus lateral-pin fixation in displaced supracondylar humerus fractures. J Pediatr Orthop 1995; 15(4): 435-9.
- Walmsley PJ, Kelly MB, Robb JE, Annan IH, Porter DE. Delay increases the need for open reduction of type-III supracondylar fractures of the humerus. J Bone Joint Surg Br 2006; 88(4): 528-30.
- Waltzman ML, Shannon M, Bowen AP, Bailey MC. Monkeybar injuries: complications of play. Pediatrics 1999; 103(5): e58.
- Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes 2006; 1(1): 11-25.
- Wang YL, Chang WN, Hsu CJ, Sun SF, Wang JL, Wong CY. The recovery of elbow range of motion after treatment of supracondylar and lateral condylar fractures of the distal humerus in children. J Orthop Trauma 2009; 23(2): 120-5.
- Wareham K, Johansen A, Stone MD, Saunders J, Jones S, Lyons RA. Seasonal variation in the incidence of wrist and forearm fractures, and its consequences. Injury 2003; 34(3): 219-22.
- West S, Andrews J, Bebbington A, Ennis O, Alderman P. Buckle fractures of the distal radius are safely treated in a soft bandage: a randomized prospective trial of bandage versus plaster cast. J Pediatr Orthop 2005; 25(3): 322-5.
- Wilkins KE. Principles of fracture remodeling in children. Injury 2005; 36 Suppl 1: A3-11.
- Willer B, Kroetsch B, Darling S, Hutson A, Leddy J. Injury rates in house league, select, and representative youth ice hockey. Med Sci Sports Exerc 2005; 37(10): 1658-63.
- Williams JM, Wright P, Currie CE, Beattie TF. Sports related injuries in Scottish adolescents aged 11-15. Br J Sports Med 1998; 32(4): 291-6.
- Wootton M, Harris D. Trampolining injuries presenting to a children's emergency department. Emerg Med J 2009; 26(10): 728-31.
- Woratanarat P, Angsanuntsukh C, Rattanasiri S, Attia J, Woratanarat T, Thakkinstian A. Meta-analysis of pinning in supracondylar fracture of the humerus in children. J Orthop Trauma 2012; 26(1): 48-53.
- Young S, Fevang JM, Gullaksen G, Nilsen PT, Engesæter LB. Deformity and functional outcome after treatment for supracondylar humerus fractures in children: a 5- to 10-year follow up of 139 supracondylar humerus fractures treated by plaster cast, skeletal traction or corssed wire fixation. J Child Orthop 2010; 4(5): 445-53.
- Zionts LE, Woodson CJ, Manjra N, Zalavras C. Time of return of elbow motion after percutaneous pinning of pediatric supracondylar humerus fractures. Clin Orthop 2009; 467(8): 2007-10.