Abstract
Background and purpose During the past 40 years, several attempts have been made with total wrist arthroplasty to avoid fusion in severely destroyed wrists. The results have often been disappointing. There is only modest clinical documentation due to the small number of patients (especially non-rheumatoid cases) and short follow-up times. Here we report a multicenter series using a third-generation implant with a minimum follow-up time of 5 years.
Methods In 2012, data were retrieved from a registry of consecutive wrist operations at 7 centers with units specialized in hand surgery, between 2003 and 2007. The wrists had been reviewed annually and analysis was done on the latest follow-up data.
Results 60 patients had been operated (5 bilaterally), 5 wrists had been revised, and 52 were available for follow-up (with the revised cases excluded). The pain scores, QuickDASH scores, ulnar flexion, and supination for the whole group were statistically significantly better at follow-up. There were no statistically significant differences between the rheumatoid and the non-rheumatoid patients except for motion, which was better in the non-rheumatoid group. The motion obtained depended on the preoperative motion. Implant survival was 0.9 at 5–9 years.
Interpretation The clinical results in terms of pain, motion, strength, and function were similar to those in previous reports. The implant survival was 0.9 at 9 years, both in rheumatoid and non-rheumatoid cases, which is an important improvement compared to the earlier generations of total wrist arthroplasty.
During the last 40 years, several attempts have been made to avoid fusion in severely destroyed wrists, to preserve motion. The flexible silicone spacers used in the 1970s were mainly used for rheumatoid wrists and, although early reports indicated favorable results, later reports indicated that the procedure should be reserved for low-demand patients with good bone stock and restricted motion, because of frequent implant breakage and subsidence or osteolysis (Jolly et al. Citation1992, Lundkvist and Barfred Citation1992, Schill et al. Citation2001, Kistler et al. Citation2005). The next generations of total wrist arthroplasty (TWA) combined metal and polyethylene and they were distally fixated with pegs, pins, or screws in the metacarpals (Dennis et al. Citation1986, CitationMeuli and Fernandez 1995, Rahimtoola and Hubach Citation2004, van Harlingen et al. Citation2011). The results were disappointing. The third generation of wrist replacements requires less bone resection and avoids metacarpal fixation (Menon Citation1998, Herzberg Citation2011). However, clinical documentation has been modest due to the limited numbers of patients (especially non-rheumatoid cases) or short follow-up time (Divelbiss et al. Citation2002, van Winterswijk and Bakx Citation2010, Ferreres et al. Citation2011, Herzberg Citation2011, Ward et al. Citation2011). The main issues that still have to be answered are: what can be expected in terms of the longevity and what should the indications be—rheumatoid arthritis, degenerative arthritis, posttraumatic arthritis, low-demand patients, or high-demand patients? We report on a multicenter series using a third-generation implant, the Re-motion Total Wrist, with a follow-up time of at least 5 years.
Methods
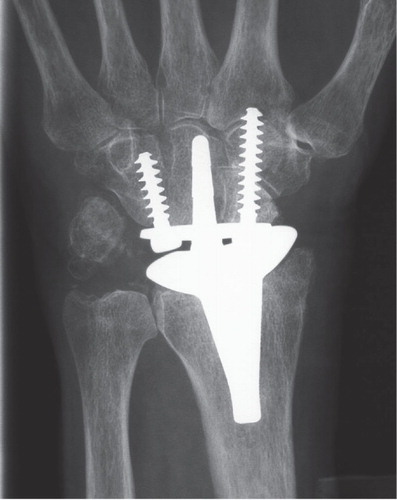
The Re-motion TWA is an elliptic ball and socket design consisting of radial and carpal Cr-Co components that are titanium-coated, and an intercalated polyethylene component that mainly articulates with the radial component but also permits a rotational articulation of 20 degrees with the carpal plate (). The carpal plate is fixated to the carpus by its stem and 2 screws, of which only the most radial may penetrate the metacarpal for a very short distance even though many advocate not doing so (Herzberg Citation2011). Thus, fixation is mainly aimed to be to the carpus and minimally in the metacarpals. The fixation is often done without cement ().
Figure 1. The Re-motion TWA with the metallic radial and carpal components and the intercalated polyethylene ball.

Figure 2. Frontal radiograph of the Re-motion TWA in a 75-year old woman with primary osteoarthrosis.
In 2009, we created a web-based registry in which surgeons using the Re-motion Total Wrist could enter prospectively collected data. Data were recorded on the etiology of wrist destruction, pre- and postoperative pain (0–100 on a visual analog scale, VAS), function (0–100 according to the QuickDASH questionnaire), active wrist motion, forearm rotation, and grip strength (measured with the JAMAR dynamometer). Surgical details and data concerning complications were also recorded. Clinical follow-up examinations were performed at 6 weeks, 6 months, and 1 year after the operation and annually thereafter without any upper limit. In real time, users can generate a detailed and updated statistics report online at no charge.
Radiographic examinations were performed on each of these occasions and the evaluation of the surgeons regarding the position of the implants and the presence of osteolysis with or without loosening (change in position of the implants) was noted.
In 2012, we retrieved data on consecutive wrists operated between 2003 and 2007 at 7 centers with units specialized in hand surgery: Gentofte Hospital, Denmark; Lyon University Hospital, France; Rigshospitalet, Denmark; Sahlgrenska Sjukhuset, Sweden; Aarhus University Hospital, Denmark; Strasbourg University Hospital, France; and Besançon University Hospital, France. Revisions were excluded.
Statistics
A Kaplan-Meier survival analysis was used to estimate the cumulative probability of remaining free of revision (i.e. reoperation with total or partial removal of the implants). A non-parametric Wilcoxon signed-rank test was used for data that were not normally distributed (Quick DASH scores) and the parametric Student t-test was used for normally distributed data (range of motion, grip strength, and VAS scores) when comparing rheumatoid patients and non-rheumatoid patients. For comparison of data collected at follow-up with preoperative data, the paired t-test was used. Bilaterally operated patients were included in the calculations with the first-operated wrist only to avoid possible statistical dependency problems. When comparing postoperative values with preoperative values, the tests were used for paired data. Significance was set at a p-value of less than 0.05.
Results
65 consecutive wrists had been operated in the period considered; 5 were bilateral (). In 49, one or several simultaneous procedures had been performed: 38 ulnar head resections, 19 tendon procedures, 3 ulnar head replacements (2 SBI, 1 Eclypse), 1 fusion of the first metacarpophalangeal joint, and 1 Nalebuff procedure on the thumb. Perioperative complications occurred in 5 cases: 2 crack fractures of the radius that healed uneventfully, 1 carpal fracture, 1 partial tendon laceration, and 1 total tendon laceration. 2 patients developed carpal tunnel syndrome during the early postoperative period. Carpal tunnel release was successful. There were no infections, dislocations, or reflex sympathetic dystrophy.
Table 1. Patient demographics
5 cases were revised: 3 were fused, in 1 a total exchange of implant components was done, and in 1 the carpal plate and polyethylene ball were revised. The causes of revision were loosening in 4 patients, 3 of whom (aged 56, 58, and 62 years) suffered from rheumatoid arthritis and the other (aged 55) having a posttraumatic condition. In the fifth patient (aged 55 years) who also had rheumatoid arthritis and almost no motion preoperatively, the TWA was not loose but had stiffened in an awkward position. Thus, no specific demographic cause could be identified as a confounding factor for failure.
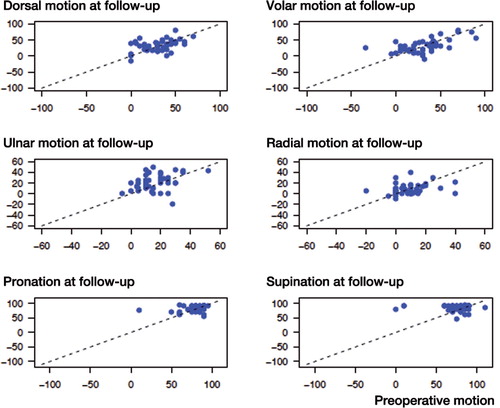
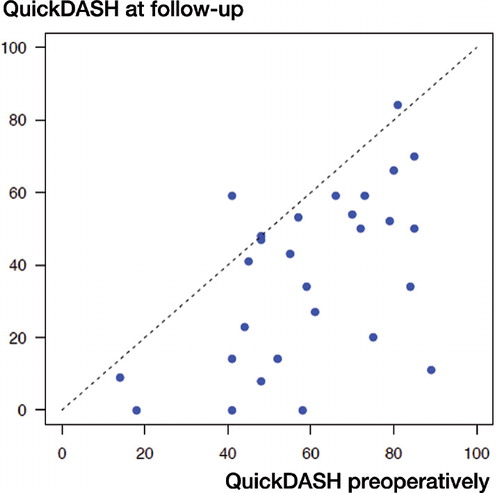
7 patients (8 wrists) did not join the late follow-up: 2 had died, 3 were untraceable, and 2 could not participate for personal reasons. The late follow-up examination of the remaining 52 wrists (with revised patients excluded) was performed at an average of 6.5 (5–9) years after operation. None of the wrists operated between 2003 and 2007 were missed in the registration, but the QuickDASH was not available in Danish before 2005. Thus, the preoperative QuickDASH was missing in 24 cases. The pain scores on VAS, QuickDASH scores, ulnar flexion, and supination for the whole group were statistically significantly better at follow-up. There were no statistically significant differences between the rheumatoid patients and the non-rheumatoid patients except for motion: supination and flexion were better in the non-rheumatoid group (). Almost all patients had a statistically significantly lower pain score and QuickDASH score at follow-up ( and ). There was a positive correlation between motion before operation and motion at follow-up ().
Table 2. Clinical results at the latest follow-up (“Post”) compared to preoperative values (“Pre”). Mean values (SD), but median (range) for QuickDASH
Figure 3. Pain on Visual analogue scale before operation and at follow-up. The dotted line represents equivalency.
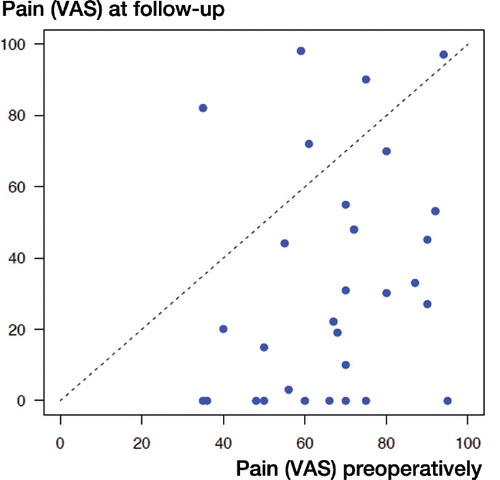
Figure 4. QuickDASH-score before operation and at follow-up. The dotted line represents equivalency.
In 6 cases, there were radiographic signs of implant loosening (subsidence or tilting): 5 carpal plates and 1 radial component (5 rheumatoid, 1 idiopathic osteoarthrosis (OA)). In 11 other cases, osteolysis without any loosening of implant components was reported: 3 carpal alone, 7 radial alone, and 1 radial and carpal (8 rheumatoid, 3 posttraumatic).
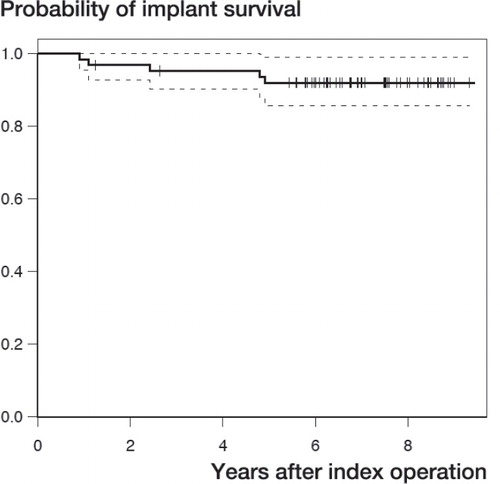
Implant survival (no implant removal) based on all 65 wrists was 0.9 at 9 years (). According to the principles of Kaplan-Meier survival calculations, the cases lost to follow-up were censored, assuming that the survivorship in the group lost to follow-up was the same as in the remaining group. The survival curves were identical in the rheumatoid group and in the non-rheumatoid group.
Discussion
The role of TWA is debated: efficient pain relief can be obtained with total fusion and patients may accommodate well for the loss of motion (Murphy et al. Citation2003). A recent systematic review of the literature, covering 503 TWAs and 860 wrist fusions, concluded that there were insufficient data to support the preference of TWA over wrist fusion in the severely destroyed rheumatoid wrist (Cavaliere and Chung Citation2008). These data were mainly based on older-generation metal-polyethylene implants with metacarpal fixation of the distal component (Biaxial-, Trispherical, CVF, and RWS prostheses).
Some reports on the latest generation of TWA have described favorable results using the Re-motion Total Wrist (Herzberg Citation2011, 20 cases) or the Universal Total Wrist (van Winterswijk and Bakx Citation2010, 17 cases; Ferreres et al. Citation2011, 22 cases). On the other hand, the series published by Ward et al. (Citation2011) with 24 Universal wrist implants had a survival rate of only 0.4 at 10 years. These small series include rheumatoid patients almost exclusively. An analysis performed on cases with a shorter observation period (2–8 years) from the same registry as in our series had a more substantial number of non-rheumatoid cases (Herzberg et al. Citation2012) and showed similar clinical results in rheumatoid and non-rheumatoid cases.
The clinical results in terms of pain, motion, strength, and function in our series are similar to those in previous reports. Moreover, we found that the motion that could be obtained depended on the preoperative motion and it did not change significantly, either clinically or statistically, except for supination and ulnar flexion. The improvement in supination is probably due to additional procedures performed on the ulnar head. As in other series, most of our patients had rheumatoid arthritis; such patients were mainly operated in the early years.
The strength of our series was the longer observation time, minimum 5 years. The implant survival was 0.9 after 9 years, in both rheumatoid and non-rheumatoid cases, which is an important improvement over the earlier generations of metal-polyethylene TWA (Cobb and Beckenbaugh Citation1996, van Harlingen et al. Citation2011). The most probable explanation for this improvement in implant survival is that fixation of the carpal component does not rely on stems inserted in the metacarpals. Indeed, loosening of the carpal component was a major problem in the earlier implants. Of the 52 “surviving” implants in our series, 6 showed signs of loosening on radiographs. The treating surgeons had not considered that revision was indicated, mainly because the patients did not suffer severe pain—or any pain at all. Even so, implant survival would be expected to decrease in the years to come. Even if the implant survival curve would decline after 9 years, the implant survival in our series is still comparable to the implant survival after total elbow arthroplasty and total ankle arthroplasty, which are more commonly used and less debatable procedures (Fevang et al. Citation2007, Citation2009, Skytta et al. Citation2009, Citation2010).
As in other registry reports, the details of analysis depend on the data included in the registry. Thus, a reliable analysis of periprosthetic osteolysis, as seen in routine plain radiographs, was not possible since no precise guidelines for evaluation of osteolysis were given to the surgeons. In the literature, osteolysis or radiolucency with or without prosthetic loosening has often been reported. In a series of 40 Biaxial TWAs, 32 of which joined a follow-up examination, 22 showed possible radiographic signs of loosening. In 12 of these, a periprosthetic radiolucent zone of at least 2 mm was present in frontal plain radiographs (mean follow-up time 6 years) (van Harlingen et al. Citation2011). Rizzo and Beckenbaugh (Citation2003) analyzed a series of 17 Biaxial TWAs with a modified (long) metacarpal stem. There were radiolucent zones in 4 of 17 cases with a mean follow-up time of 6 years, without other signs of implant loosening. Takwale et al. (Citation2002) re-examined 76 Biaxial TWAs with a mean follow-up time of 4 years. Implant survival was 0.86 and 14 more cases showed radiographic signs of prosthetic loosening, but it was not reported whether osteolysis was associated with subsidence or angulation of the implant components. Ferreres et al. (Citation2011) reported 2 cases of osteolysis or prosthetic loosening in a series of 21 Universal TWAs 3–8 years after operation. Ward et al. (Citation2011) published a series of 24 cemented Universal I TWAs in rheumatoid patients. Of the 19 patients with a follow-up time of more than 5 years, 9 had been revised because of loosening of the carpal component. Polyethylene wear has been mentioned as a possible cause of osteolysis, but in our opinion no definite proof has been given for this assumption.
MB: planning of the study, interpretation of data analysis, and writing. SM: planning of the study, computation of data, and constructive comments. GH: planning of study and constructive comments.
We thank the following surgeons for contributing data: Dr. Allan Ibsen Sørensen and Dr. Peter Axelsson, Gothenburg; Prof. Laurent Obert, Besançon; Prof. Philippe Liverneaux, Strasbourg; and Dr. Karsten Krøner, Aarhus.
No competing interests declared.
- Cavaliere CM, Chung KC. A systematic review of total wrist arthroplasty compared with total wrist arthrodesis for rheumatoid arthritis. Plast Reconstr Surg (Comparative Study Review). 2008; 122 (3): 813-25.
- Cobb TK, Beckenbaugh RD. Biaxial total-wrist arthroplasty. J Hand Surg 1996; 21 (6): 1011-21.
- Dennis DA, Ferlic DC, Clayton ML. Volz total wrist arthroplasty in rheumatoid arthritis: a long-term review. J Hand Surg 1986; 11 (4): 483-90.
- Divelbiss BJ, Sollerman C, Adams BD. Early results of the Universal total wrist arthroplasty in rheumatoid arthritis. J Hand Surg 2002; 27 (2): 195-204.
- Ferreres A, Lluch A, Del Valle M. Universal total wrist arthroplasty: midterm follow-up study. J Hand Surg 2011; 36 (6): 967-73.
- Fevang BT, Lie SA, Havelin LI, Brun JG, Skredderstuen A, Furnes O. 257 ankle arthroplasties performed in Norway between 1994 and 2005. Acta Orthop 2007; 78 (5): 575-83.
- Fevang BT, Lie SA, Havelin LI, Skredderstuen A, Furnes O. Results after 562 total elbow replacements: a report from the Norwegian Arthroplasty Register. J Shoulder Elbow Surg 2009; 18 (3): 449-56.
- Herzberg G. Prospective study of a new total wrist arthroplasty: short term results. Chir Main 2011; 30 (1): 20-5.
- Herzberg G, Boeckstyns M, Ibsen Sørensen A, Axelsson P, Kroener K, Liverneaux P, Obert L, Merser S.“Remotion” total wrist qrthroplasty: Preliminary results of a prospective international multicenter study of 215 cases. J Wrist Surg 2012; 01 (01): 17-22.
- Jolly SL, Ferlic DC, Clayton ML, Dennis DA, Stringer EA. Swanson silicone arthroplasty of the wrist in rheumatoid arthritis: a long-term follow-up. J Hand Surg (review) 1992; 17 (1): 142-9.
- Kistler U, Weiss AP, Simmen BR, Herren DB. Long-term results of silicone wrist arthroplasty in patients with rheumatoid arthritis. J Hand Surg 2005; 30 (6): 1282-7.
- Lundkvist L, Barfred T. Total wrist arthroplasty. Experience with Swanson flexible silicone implants. 1982-1988. Scand J Plast Reconstr Surg Hand Surg 1992; 26 (1): 97-100.
- Menon J. Universal total wrist implant: experience with a carpal component fixed with three screws. J Arthroplasty 1998; 13 (5): 515-23.
- Meuli HC, Fernandez DL. Uncemented total wrist arthroplasty. J Hand Surg (comparative study) 1995; 20(1): 115-22.
- Murphy DM, Khoury JG, Imbriglia JE, Adams BD. Comparison of arthroplasty and arthrodesis for the rheumatoid wrist. J Hand Surg 2003; 28 (4): 570-6.
- Rahimtoola ZO, Hubach P. Total modular wrist prosthesis: a new design. Scand J Plast Reconstr Surg Hand Surg 2004; 38 (3): 160-5.
- Rizzo M, Beckenbaugh RD. Results of biaxial total wrist arthroplasty with a modified (long) metacarpal stem. J Hand Surg 2003; 28 (4): 577-84.
- Schill S, Thabe H, Mohr W. Long-term outcome of Swanson prosthesis management of the rheumatic wrist joint. Handchir Mikrochir Plast Chir 2001; 33 (3): 198-206.
- Skytta ET, Eskelinen A, Paavolainen P, Ikavalko M, Remes V. Total elbow arthroplasty in rheumatoid arthritis: a population-based study from the Finnish Arthroplasty Register. Acta Orthop 2009; 80 (4): 472-7.
- Skytta ET, Koivu H, Eskelinen A, Ikavalko M, Paavolainen P, Remes V. Total ankle replacement: a population-based study of 515 cases from the Finnish Arthroplasty Register. Acta Orthop 2010; 81 (1): 114-8.
- Takwale VJ, Nuttall D, Trail IA, Stanley JK. Biaxial total wrist replacement in patients with rheumatoid arthritis. Clinical review, survivorship and radiological analysis. J Bone Joint Surg (Br) 2002; 84 (5): 692-9.
- Van Harlingen D, Heesterbeek PJ, de Vos MJ. High rate of complications and radiographic loosening of the biaxial total wrist arthroplasty in rheumatoid arthritis: 32 wrists followed for 6 (5-8) years. Acta Orthop 2011; 82 (6): 721-6.
- van Winterswijk PJ, Bakx PA. Promising clinical results of the universal total wrist prosthesis in rheumatoid arthritis. Open Orthop J 2010; 4: 67-70.
- Ward CM, Kuhl T, Adams BD. Five to ten-year outcomes of the Universal total wrist arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg (Am) 2011; 93 (10): 914-9.