Abstract
Background and purpose There have been few prospective reports on quality of life in patients treated surgically for scoliosis. We compared patients with idiopathic, congenital, and neuromuscular scoliosis.
Methods Data on 9- to 20-year-old patients were collected from the SweSpine registry. EQ-5D and (for a subset) SRS-22r were assessed preoperatively and after 1 and 2 years.
Results 211 patients had preoperative data: 168 with idiopathic, 11 with congenital, and 32 with neuromuscular scoliosis. Of the total, 158 patients responded to the 1-year follow-up and 149 responded to the 2-year follow-up. Preoperatively, the mean (SE) EQ-5D index was 0.76 (0.02) in the idiopathic group, 0.74 (0.07) in the congenital group, and 0.10 (0.06) in the neuromuscular group, and the SRS-22r index was 3.8 (0.1) in the idiopathic group, 4.0 (0.3) in the congenital group, and 3.3 (0.2) in the neuromuscular group. The mean EQ-5D increased by 0.06 points at 2 years in the idiopathic group, by 0.16 points in the congenital group, and by 0.15 points in the neuromuscular group. The mean SRS-22r index increased by 0.4 points at 2 years in the idiopathic group, by 0.4 points in the congenital group, and by 0.5 points in the neuromuscular group. The changes were statistically significant, with the exception of the congenital group. The number of patients who sustained at least 1 complication was 13 in the idiopathic group, 2 in the congenital group, and 9 in the neuromuscular group (p = 0.003).
Interpretation The general quality of life in the idiopathic and neuromuscular group improved after surgery.
Scoliosis, a 3-dimensional structural deformity of the spine, is defined as a curve angle of more than 10° measured on a standard anterior-posterior radiographic projection using the Cobb technique (Cobb Citation1948, Willner and Uden Citation1982). Scoliosis is divided into different types depending on etiology. The main types are idiopathic scoliosis, congenital scoliosis, and neuromuscular scoliosis.
Idiopathic scoliosis is the most common type of structural scoliosis (Shands and Eisberg Citation1955, Willner and Uden Citation1982). The general belief is that idiopathic scoliosis is a multifactorial condition, with a hereditary component (Grauers et al. Citation2012). The prevalence of idiopathic scoliosis in Sweden is 3% and it is commonest in girls. Around 10% of the children with idiopathic scoliosis curves progress to the level at which treatment is suggested (Willner and Uden Citation1982).
Congenital scoliosis results from defects in the embryological vertebral development. The defects are classified as failure of formation, failure of segmentation, or a combination of these 2 types. Congenital scoliosis may occur together with other organ malformations (Hedequist and Emans Citation2007). The incidence of congenital scoliosis has been estimated to be 0.5 per 1,000 births (Shands and Eisberg Citation1955).
Neuromuscular scoliosis occurs in patients with neurological or muscular disorders, including cerebral palsy (CP), myelomeningocele, muscular dystrophies, and spinal atrophies. The curves are often long, extending into the sacrum and associated with pelvic obliquity (Madigan and Wallace Citation1981, Sarwark and Sarwahi Citation2007).
Large curves increase the risk of health problems such as respiratory issues, disability, and pain (Pehrsson et al. Citation1992, Danielsson et al. Citation2001, Sarwark and Sarwahi Citation2007). Patients with a Cobbs’ angle greater than 45–50° are generally recommended surgical treatment, but age, curve progression, symptoms, and underlying disorders are important factors to consider (Willner and Uden Citation1982, Hedequist and Emans Citation2007, Sarwark and Sarwahi Citation2007, Kim et al. Citation2009). The primary treatment goal is to prevent curve progression and the secondary goal is to achieve curve correction. The correction is provided by spinal instrumentation (e.g. pedicle screws, hooks, or wires attached to rods) and the fusion is done by bone grafting (Hedequist and Emans Citation2007, Sarwark and Sarwahi Citation2007, Kim et al. Citation2009).
Results after scoliosis surgery have mainly been reported as radiographic changes, such as magnitude and correction of the curve. However, these radiological changes have been shown to be weak predictors of patient satisfaction (Wilson et al. Citation2002). Measurement of quality of life has therefore become increasingly common in the evaluation of surgical treatment of scoliosis.
Few studies including both preoperative and postoperative data on quality of life in patients operated for idiopathic scoliosis have been published (Merola et al. Citation2002). In addition, there have been very few data published on quality of life postoperatively in patients with neuromuscular and congenital scoliosis (Bridwell et al. Citation1999, Jones et al. Citation2003, Larsson et al. Citation2005, Citation2009, Tsirikos et al. Citation2008, Jalanko et al. Citation2011).
Here we describe the quality of life—as assessed by the EQ-5D and the SRS-22r questionnaires—preoperatively and 1 and 2 years postoperatively in children and young adults who were treated surgically for idiopathic, congenital, and neuromuscular scoliosis in Sweden.
Patients and methods
This was a registry-based study with data collected from the SweSpine registry. The SweSpine registry began in 1993 with registration of surgery in the lumbar spine (Stromqvist et al. Citation2013). The deformity part of the SweSpine registry, which was used in this study, was started in 2006. Participating clinics register data on a voluntary basis.
Patients
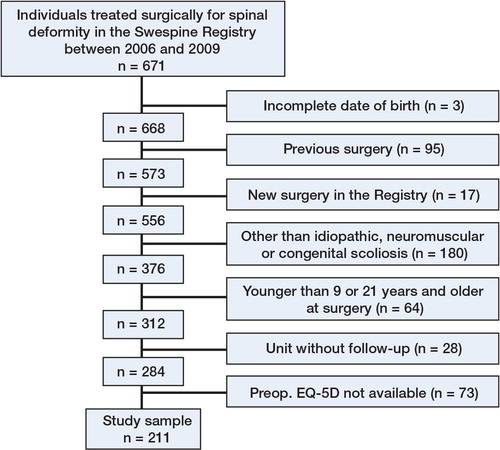
A flow chart of extraction of the cohort data from the SweSpine registry for this specific study is presented in . To enable a 2-year follow-up, patients who underwent surgery later than December 31, 2009 were excluded. Only patients with no previous spinal surgery were included. Patients who had subsequent surgical procedures for scoliosis, other than reoperations, were excluded.
Only surgeries on patients with idiopathic, congenital, and neuromuscular scoliosis were included, since these 3 groups were estimated to be large enough for analysis. The diagnosis was the one indicated by the surgeon in the registry at the time of surgery. The diagnoses included in the neuromuscular scoliosis group were: muscular dystrophy, upper motor neuron disease (e.g. cerebral paresis, tumors, or spinocerebellar degeneration), and lower motor neuron disease (e.g. post-polio syndrome or spinal muscle atrophy).
We excluded surgeries on patients registered without diagnosis, or with more than 1 diagnosis. Patients younger than 9 years, or 21 years or older at the time of surgery were excluded.
Of the participating hospitals, 1 did not have follow-up data for any of the patients and was therefore excluded. We only included patients for which EQ-5D data were available preoperatively. The final study sample consisted of 211 patients.
Surgeon-reported variables
The preoperative Cobb angle of the primary curve—and if important for the surgical decision, the Cobb angle of any kyphosis—was reported. Operating time, blood loss, type of surgery, hospital stay, operated vertebrae, and complications were reported at the time of discharge. A subjective preoperative estimate of the cognitive function of the patient was made by the surgeon and graded as normal, mild, or severe cognitive disability. Reoperations were registered in the SweSpine registry by the surgeon.
Mortality data
Data on mortality were obtained through the population registry.
Patient-reported variables
A questionnaire was answered by the patient preoperatively. An identical questionnaire was mailed to the patient 1 and 2 years postoperatively. The questionnaire contained the EuroQol (EQ-5D) instrument and after February, 2008, the Scoliosis Research Society 22r instrument (SRS-22r). In addition, at the 1-year follow-up patients were asked whether they had had complications within 3 months after the surgery. Specific complications asked for were: thrombosis, pulmonary embolism, superficial infection treated with antibiotics, deep infection treated with antibiotics for more than 6 weeks, weakness or paralysis in the lower extremities, and urinary or fecal incontinence.
EQ-5D is available in a validated Swedish version, which is being increasingly used (Burstrom et al. Citation2001). The EQ-5D consists of 5 questions (domains) regarding mobility, usual activities, self care, pain, and anxiety, which are translated to an index. The index reflects the societal view of health. There are no Swedish index data, so the UK EQ-5D index tariff was used (Dolan et al. Citation1996, Dolan Citation1997). An index of 1 corresponds to perfect health and 0 to death. The construction of the index also allows negative values, i.e. a quality of life worse than death.
The SRS instrument was constructed to evaluate quality of life after surgical treatment in adolescent idiopathic scoliosis (Asher et al. Citation2006). The current revised version of SRS22, the SRS-22r, has been translated into Swedish and validated (A. Danielsson, personal communication). The SRS22r consists of 22 questions divided into 5 different domains: function, pain, self image, mental health, and satisfaction. For each question, domain, and total index, a score between 1 (worst possible) and 5 (best possible) can be obtained. In contrast to the EQ-5D index, which reflects the societal view of health, the SRS22r index represents the individual’s subjective experience of health. The satisfaction domain is a measure of treatment satisfaction and in this study it is only presented for 2-year postoperative data.
Statistics
Since group sizes and many variances were unequal, the Welch-Satterthwaite t-test or the Welch F-test was used to assess group differences. The Wilcoxon signed ranks test was performed to analyze dependent variables. The chi-square test or Fisher’s exact test was used when dichotomous variables were compared. Descriptive data are presented as mean (SD), except for the EQ-5D and the SRS-22r index in which mean (SE) is presented, since these have been commonest in most previous reports. When comparing the different domains in the EQ-5D, patients with problems were compared with patients without problems. Any p-value less than 0.05 was considered significant. The statistical analyses were performed using IBM SPSS version 20.0.
Ethical approval
The study was performed in accordance with the Helsinki Declaration and approved by the Ethical review board in Stockholm (number 2012/172-31/4).
Results
Surgeon-reported variables
Of the 211 patients who were finally included, 168 had an idiopathic scoliosis, 11 had a congenital scoliosis, and 32 had a neuromuscular scoliosis (). In the idiopathic group, 148 had been treated with posterior surgery, 16 with anterior surgery, and 4 with anterior and posterior surgery. The corresponding figures for the patients in the congenital group were 9, 1, and 1 and in the neuromuscular group they were 29, 0, and 3.
Table 1. Data at the time of surgery (mean (SD) or number (n)) for the 211 patients in the study. In cases of missing data, the number of patients who were available is given in the table. The p-values were obtained from the chi-square test or the Welch F-test
The proportion of women in the idiopathic scoliosis group was considerably larger than in the congenital and neuromuscular scoliosis groups. In the neuromuscular group, the mean number of operated vertebra and the intraoperative blood loss were greater than in the idiopathic and congenital group, and the duration of surgery and the hospital stay were longer (). 15 of the 32 patients in the neuromuscular group had a severe cognitive disability, while no patients in the other 2 groups had a severe cognitive disability.
Mortality data
1 patient in the idiopathic group died before the 2-year follow-up.
Patient-reported variables
The number of patients who responded to the EQ-5D and/or the SRS-22r instruments was 158 (75%) at the 1-year follow-up and 149 (71%) at the 2-year follow-up. Of the 149 patients who responded at the 2-year follow-up, 126 had also responded at the 1-year follow-up.
When we compared all patients who responded, the EQ-5D index was lower at all time points for the group of patients with neuromuscular scoliosis. When comparing those who responded preoperatively and at the 2-year follow-up, the EQ-5D index increased by 0.06 (0.02) points in the idiopathic group (p = 0.001), by 0.16 (0.08) points in the congenital group (p = 0.07), and 0.15 (0.06) points in the neuromuscular group (p = 0.02) (, and and )
Table 2. Preoperative, 1-year, and 2-year postoperative EQ-5D-index in the 3 groups of scoliosis patients. Data are mean (SE). The p-values given are from the Welch F-test for comparison between groups at the different time points
Figure 2. Distribution of the EQ-5D index. The data shown are for the 211 patients who answered the EQ-5D preoperatively.
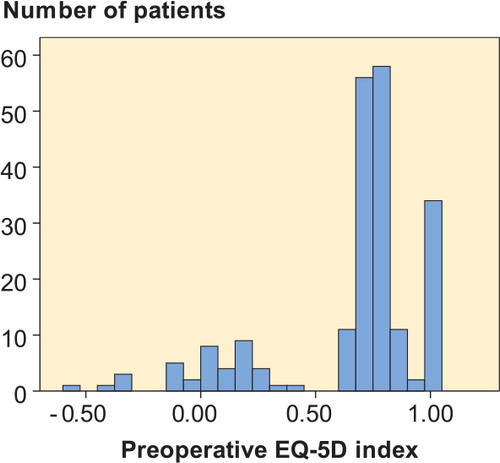
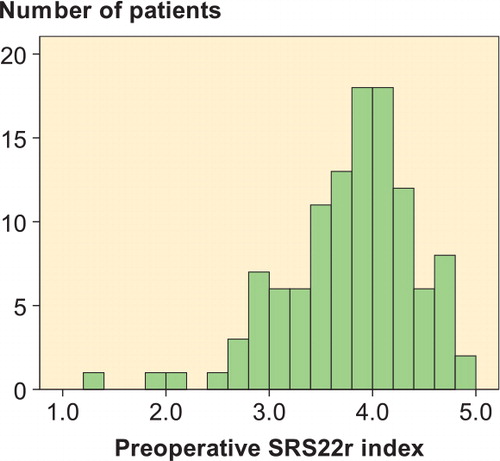
Figure 3. Distribution of the SRS22r index. The data shown are for the 114 patients who answered the SRS22r preoperatively.
When we examined the specific domains of EQ-5D, and compared individuals with and without problems in each domain (mobility, usual activities, self care, pain, and anxiety), any amount of pain was experienced by 93 of 122 (76%) in the idiopathic group preoperatively and by 70 of 122 (57%) 2 years postoperatively (p < 0.001). In the group of neuromuscular patients, 12 of 14 patients experienced pain preoperatively and 6 of 14 experienced pain 2 years postoperatively (p = 0.01). The patients in the idiopathic scoliosis group experienced less problems with mobility (p = 0.02) and anxiety 2 years postoperatively (p = 0.008). No other significant changes were observed (all p > 0.08; data not shown).
The SRS-22r was not available for all patients since it was introduced in the registry at a later time point than the EQ-5D. When we compared the different groups of responding patients preoperatively and 1 and 2 years postoperatively, the SRS-22r index was similar (). When comparing those who responded preoperatively and at the 2-year follow-up, the SRS-22r index improved by 0.4 (0.1) points at 2 years in the idiopathic group (p < 0.001), by 0.4 (0.1) points in the congenital group (p = 0.07), and by 0.5 (0.2) points in the neuromuscular group (p = 0.024).
Table 3. Preoperative, 1-year, and 2-year postoperative SRS-22r-index, excluding the satisfaction domain, in the 3 groups of scoliosis patients. The SRS-22r was introduced later than the EQ-5D in the registry, and was therefore not available for all patients. Data are mean (SE). The p-values given are from the Welch F-test for comparison between groups at the different time points
When we compared the different domains in the SRS-22r preoperatively and 2 years postoperatively, the neuromuscular group experienced improved function (p = 0.008) and the idiopathic group experienced less pain (p = 0.007). Both the idiopathic group and the neuromuscular group experienced a better self image (p < 0.001 and p = 0.011, respectively). Mental health was unchanged in all 3 groups (data not shown).
The mean score for the satisfaction domain in the SRS-22r was similar between the 3 groups 2 years postoperatively: 4.1 (0.1) in the idiopathic group, 4.1 (0.4) in the congenital group, and 4.2 (0.2) in the neuromuscular group. Of those patients who answered question 21 regarding treatment satisfaction in SRS-22r, 108 of 141 (77%) were satisfied or very satisfied, 23 of 141 (16%) were neither satisfied nor dissatisfied, and 10 of 141 (7%) were dissatisfied or very dissatisfied.
Complications
The number of patients who sustained at least 1 complication (patient- or surgeon-reported) was 13 (8%) in the idiopathic group, 2 in the congenital group, and 9 in the neuromuscular group (p = 0.003). The number of patients who were reoperated during the 2-year follow-up was 10 (6%) in the idiopathic group, 1 in the congenital group, and 4 in the neuromuscular group (p = 0.3).
When we compared patients with and without complications in the idiopathic group, there were no statistically significant differences at the 2-year follow-up for the EQ-5D index, the SRS22r index (excluding the satisfaction domain), and the SRS22r satisfaction domain (all p > 0.25). The congenital group was too small for analysis. No difference was found in the neuromuscular group (all p > 0.08).
Discussion
This study has been the first to use data from the SweSpine registry to evaluate quality of life before and after surgery in patients in Sweden who were treated surgically for scoliosis. The results suggested that quality of life remained unchanged or was slightly improved 2 years after surgery.
Few studies have used the EQ-5D as a measurement of quality of life in scoliosis patients. 2 years postoperatively, patients in the idiopathic and congenital groups of the present study had only slightly lower indices than the Swedish reference value (0.89) for ages 20–29 (Burstrom et al. Citation2001), indicating fairly good health in these patients. A Norwegian study involving 86 patients with idiopathic scoliosis 10 years after spinal fusion found a mean EQ-5D index of 0.83 (Bjerkreim et al. Citation2007), which is comparable to the mean of 0.82 in the idiopathic group in our study. In the same study, it was found that about half of the surgically treated individuals with idiopathic scoliosis experienced pain, according to the EQ-5D. The present 2-year follow-up showed a significant decrease in pain after surgery, but 57% of the idiopathic scoliosis patients still experienced pain—which is considerably higher than the prevalence of 28% found in the part of the normal Swedish population aged 20–29 years (Burstrom et al. Citation2001).
We have not found any published prospective pre- and postoperative data regarding the SRS-22r instrument. The positive effects using the SRS-22r instrument found in patients with idiopathic scoliosis are consistent with a previous report using the SRS-24 instrument, in which the preoperative mean index of 3.7 improved to 4.6 at the 2-year follow-up (Merola et al. Citation2002).
The magnitude and direction of change for the EQ-5D and the SRS22r indices in the small congenital group were similar to those of the other 2 groups. We have found 1 study that measured quality of life in patients who were surgically treated for congenital scoliosis. However, the authors only presented postoperative data for the SRS-24, up to 1–7 years after surgery (Jalanko et al. Citation2011). These results appear to be comparable to the results for the congenital group in the present study.
It is not surprising that patients in the neuromuscular group had lower general health scores than the normal population, considering the severity of their underlying diseases. Studies on outcome after surgery in patients with neuromuscular scoliosis have not used any of the EQ-5D or SRS instruments, so direct comparisons cannot be made. Using other questionnaires, these studies have shown a similar positive effect of surgery on overall quality of life (Bridwell et al. Citation1999, Jones et al. Citation2003, Larsson et al. Citation2005, Citation2009, Tsirikos et al. Citation2008).
The SRS instrument was constructed to evaluate idiopathic scoliosis in an active ambulatory population and has not been validated for patients with congenital and neuromuscular scoliosis (Asher et al. Citation2006). As a consequence, the importance of the results of the SRS-22r in the congenital and neuromuscular groups is uncertain. However, no instruments that have been sufficiently validated are available for evaluation of treatment of non-idiopathic scoliosis. Interestingly, the EQ-5D and the SRS22r indices behaved similarly in the idiopathic, congenital, and neuromuscular groups, but the changes were not statistically significant in the small congenital group. This indicates that even though general health and the etiologies of the spinal deformities are different, it is possible that all groups appreciate the surgical procedure in the same way.
Even though the mean improvement for the SRS22r did not exceed the minimal clinically important difference of 0.6 as suggested by Bago et al. (Citation2009), most patients were satisfied with the treatment. Whether or not the minimal clinically important difference was reached for the EQ-5D index cannot be determined, since estimates for the surgical treatment of scoliosis are lacking.
The treatment goal with surgery is to prevent curve progression, since large curves increase the risk of health problems (Pehrsson et al. Citation1992, Danielsson et al. Citation2001, Sarwark and Sarwahi Citation2007). Better knowledge of the long-term outcome of surgery for scoliosis would be beneficial for both surgeons and patients regarding the decision for or against surgical treatment. There have been long-term follow-ups after surgery on patients with idiopathic scoliosis, but these have lacked preoperative data and they involved patients treated with surgical techniques that are seldom used today. These studies have indicated that surgically treated individuals with idiopathic scoliosis have a slightly lower quality of life than the general population (Danielsson et al. Citation2001, Andersen et al. Citation2006, Bjerkreim et al. Citation2007). The future prospective data collection of the SweSpine registry, at 5 and 10 years after surgery, will be useful and can provide prospective data on a large-scale, nationwide basis.
The present study had some limitations. The response rate was rather low. Nevertheless, the response rate for the deformity part is comparable to other parts of the SweSpine registry (Stromqvist et al. Citation2013). The neuromuscular group had a large number of patients with cognitive impairment and functional disability, which could explain the low response rate in this group. This is further illustrated by the fact that the proportion of patients with neuromuscular scoliosis among those without preoperative EQ-5D data was greater than among the study participants (data not shown). The accuracy of the complication rate in the present study has not been assessed, but complication rates are similar to those in previous reports (Weiss and Goodall Citation2008).
The EQ-5D can be used to compare spinal deformity surgery with that for other diseases and to achieve a utility index in the evaluation of cost effectiveness, while SRS-22r generates more specific information that can be used to evaluate the patient’s back-related health over time (Adobor et al. Citation2010).
The EQ-5D was developed for use in adults. This must be taken into consideration when interpreting the results, since age at the time of surgery was 20 years or less in all 3 groups. A Swedish pilot version for children and adolescents, the EQ-5D-Y, has recently been presented (Burstrom et al. Citation2011). However, if we have different questionnaires for specific subgroups and ages we would run the risk of reducing the response rate even further, but the use of the EQ-5D-Y in the registry could be discussed.
In summary, data from the SweSpine registry indicates that quality of life, assessed by the EQ-5D and the SRS22r, improved after surgery in the idiopathic and neuromuscular groups, and was unchanged in the congenital group.
AE: data analysis, drafting of and commenting on manuscript. PG: study design, hypothesis, data analysis, finalizing of manuscript.
Paul Gerdhem is currently the unpaid elected president of the Swedish Society of Spine Surgeons, a non-profit organization that is responsible for the operation and development of the SweSpine registry.
This study was financially supported by funds from the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and the Karolinska Institute, and the Karolinska Institute research funds. We thank all the surgeons and patients who have contributed data to the spine deformity part of the SweSpine registry, and Carina Blom of the SweSpine Registry for assistance with data retrieval.
- Adobor RD, Rimeslatten S, Keller A, Brox JI. Repeatability, reliability, and concurrent validity of the scoliosis research society-22 questionnaire and euroqol in patients with adolescent idiopathic scoliosis. Spine 2010; 35 (2): 206-9.
- Andersen MO, Christensen SB, Thomsen K. Outcome at 10 years after treatment for adolescent idiopathic scoliosis. Spine 2006; 31 (3): 350-4.
- Asher MA, Lai SM, Glattes RC, Burton DC, Alanay A, Bago J. Refinement of the srs-22 health-related quality of life questionnaire function domain. Spine 2006; 31 (5): 593-7.
- Bago J, Perez-Grueso FJ, Les E, Hernandez P, Pellise F. Minimal important differences of the srs-22 patient questionnaire following surgical treatment of idiopathic scoliosis. Eur Spine J 2009; 18 (12): 1898-904.
- Bjerkreim I, Steen H, Brox JI. Idiopathic scoliosis treated with cotrel-dubousset instrumentation: Evaluation 10 years after surgery. Spine 2007; 32 (19): 2103-10.
- Bridwell KH, Baldus C, Iffrig TM, Lenke LG, Blanke K. Process measures and patient/parent evaluation of surgical management of spinal deformities in patients with progressive flaccid neuromuscular scoliosis (duchenne’s muscular dystrophy and spinal muscular atrophy). Spine 1999; 24 (13): 1300-9.
- Burstrom K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the eq-5d. Qual Life Res 2001; 10 (7): 621-35.
- Burstrom K, Svartengren M, Egmar AC. Testing a swedish child-friendly pilot version of the eq-5d instrument–initial results. Eur J Public Health 2011; 21 (2): 178-83.
- Cobb J. Outline for the study of scoliosis. Instructional course lectures, the american academy of orthopaedic surgeons (aaos): Ann arbor 1948: 261-75.
- Danielsson AJ, Wiklund I, Pehrsson K, Nachemson AL. Health-related quality of life in patients with adolescent idiopathic scoliosis: A matched follow-up at least 20 years after treatment with brace or surgery. Eur Spine J 2001; 10 (4): 278-88.
- Dolan P. Modeling valuations for euroqol health states. Med Care 1997; 35 (11): 1095-108.
- Dolan P, Gudex C, Kind P, Williams A. The time trade-off method: Results from a general population study. Health Econ 1996; 5 (2): 141-54.
- Grauers A, Rahman I, Gerdhem P. Heritability of scoliosis. Eur Spine J 2012; 21 (6): 1069-74.
- Hedequist D, Emans J. Congenital scoliosis: A review and update. J Pediatr Orthop 2007; 27 (1): 106-16.
- Jalanko T, Rintala R, Puisto V, Helenius I. Hemivertebra resection for congenital scoliosis in young children: Comparison of clinical, radiographic, and health-related quality of life outcomes between the anteroposterior and posterolateral approaches. Spine 2011; 36 (1): 41-9.
- Jones KB, Sponseller PD, Shindle MK, McCarthy ML. Longitudinal parental perceptions of spinal fusion for neuromuscular spine deformity in patients with totally involved cerebral palsy. J Pediatr Orthop 2003; 23 (2): 143-9.
- Kim HJ, Blanco JS, Widmann RF. Update on the management of idiopathic scoliosis. Curr Opin Pediatr 2009; 21 (1): 55-64.
- Larsson EL, Aaro SI, Normelli HC, Oberg BE. Long-term follow-up of functioning after spinal surgery in patients with neuromuscular scoliosis. Spine 2005; 30 (19): 2145-52.
- Larsson EL, Aaro S, Ahlinder P, Normelli H, Tropp H, Oberg B. Long-term follow-up of functioning after spinal surgery in patients with rett syndrome. Eur Spine J 2009; 18 (4): 506-11.
- Madigan RR, Wallace SL. Scoliosis in the institutionalized cerebral palsy population. Spine 1981; 6 (6): 583-90.
- Merola AA, Haher TR, Brkaric M, Panagopoulos G, Mathur S, Kohani O, Lowe TG, Lenke LG, Wenger DR, Newton PO, Clements DH, 3rd, Betz RR. A multicenter study of the outcomes of the surgical treatment of adolescent idiopathic scoliosis using the scoliosis research society (srs) outcome instrument. Spine 2002; 27 (18): 2046-51.
- Pehrsson K, Larsson S, Oden A, Nachemson A. Long-term follow-up of patients with untreated scoliosis. A study of mortality, causes of death, and symptoms. Spine 1992; 17 (9): 1091-6.
- Sarwark J, Sarwahi V. New strategies and decision making in the management of neuromuscular scoliosis. Orthop Clin North Am 2007; 38 (4): 485-96.
- Shands AR, Jr., Eisberg HB. The incidence of scoliosis in the state of delaware; a study of 50,000 minifilms of the chest made during a survey for tuberculosis. J Bone Joint Surg (Am) 1955; 37 (6): 1243-9.
- Stromqvist B, Fritzell P, Hagg O, Jonsson B, Sanden B. Swespine: The swedish spine register: The 2012 report. Eur Spine J 2013; 22 (4): 953-74.
- Tsirikos AI, Lipton G, Chang WN, Dabney KW, Miller F. Surgical correction of scoliosis in pediatric patients with cerebral palsy using the unit rod instrumentation. Spine 2008; 33 (10): 1133-40.
- Weiss HR, Goodall D. Rate of complications in scoliosis surgery–a systematic review of the pub med literature. Scoliosis 2008; 3: 9.
- Willner S, Uden A. A prospective prevalence study of scoliosis in southern sweden. Acta Orthop Scand 1982; 53 (2): 233-7.
- Wilson PL, Newton PO, Wenger DR, Haher T, Merola A, Lenke L, Lowe T, Clements D, Betz R. A multicenter study analyzing the relationship of a standardized radiographic scoring system of adolescent idiopathic scoliosis and the scoliosis research society outcomes instrument. Spine 2002; 27 (18): 2036-40.