Abstract
Background and purpose Failed closed treatment of carpal tunnel syndrome (CTS) is often followed by surgery. We investigated whether preoperative steroid injections could have a negative effect on the long-term outcome of the operation.
Patients and methods 174 hands (164 patients) were operated on by a single surgeon at Tartu University Hospital in 2005. The patients were interviewed by telephone 5–6 years after the operation. Self-reported data were gathered retrospectively concerning the number of steroid injections received before the surgery and the perceived regression of symptoms (on a 100-point numeric rating scale) at the time of interview. The patients were also asked about the presence of specific symptoms of CTS if regression of their symptoms had not been complete.
Results 93 of the 174 hands had complete regression of symptoms. Each additional injection was associated with an increased risk of occurrence of pain (RR = 1.1, 95% CI: 1.02–1-2), paresthesiae (RR = 1.1, CI: 1.1–1.2), and nocturnal awakenings (RR = 1.2, CI: 1.1–1.3). There was a weak association between the number of injections and the score given to regression of symptoms.
Interpretation This is the first study to indicate that patients who received a greater number of local steroid injections preoperatively were more likely to have postoperative complaints associated with CTS.
The prevalence of CTS in the general population has been estimated to be 1–5% (Atroshi et al. Citation1999, Stephens et al. Citation2008, Shiri et al. Citation2009). Non-steroidal anti-inflammatory drugs, diuretics, vitamin B6 injections, ultrasound therapy, laser therapy, acupuncture, magnetic therapy, bracing and local steroid injections have been used for closed treatment (Armstrong et al. Citation2004, Huisstede et al. Citation2010a). Effective results in the short-term treatment of CTS have been demonstrated clearly only for bracing and local steroid injections (Carlson et al. Citation2010, Huisstede et al. Citation2010a). For surgery, both open and endoscopic methods are used, although no benefit in long-term results has been demonstrated with endoscopic operation (Huisstede et al. Citation2010b). Since there is no consensus on the superiority of conservative treatment or immediate surgical treatment, therapy that first relies on steroid injections has been recommended (Verdugo et al. Citation2008, Shi et al. Citation2011). Although some patients may achieve long-lasting relief of symptoms after injection(s), many often fail to respond to subsequent injections and are operated on (Armstrong et al. Citation2004, Verdugo et al. Citation2008). Assessments of the outcome of surgical treatment in the literature have mostly concentrated on the differences between endoscopic and open methods, and less attention has been paid to the effects of pre- and postoperative treatment.
We have not found any studies that investigated the effect of preoperatively performed local steroid injections on the long-term outcome of surgical carpal tunnel release. Although not directly comparable, a recent systematic review of the treatment of tendinopathy with corticosteroids highlighted their harmful medium and long-term effects in lateral epicondylitis (Coombes et al. Citation2010). Thus, based on clinical suspicion and on inconsistencies in the published results on the long-term effectiveness of local steroid injections, we hypothesized that preoperative steroid injections might worsen long-term postoperative outcome in patients with CTS.
Patients and methods
This study was approved by the Ethics Review Committee on Human Research of the University of Tartu. Informed consent was obtained from all participants.
In January and February of 2011, we interviewed by telephone all patients with a diagnosis of CTS who had undergone surgical treatment during 2005 at the Neurology Clinic of Tartu University Hospital (Department of Neurosurgery). The patients were diagnosed based on well-defined clinical findings, including the results of nerve conduction studies in a few cases where the diagnosis was in doubt. The surgeries were performed by the same neurosurgeon using the same technique of open carpal tunnel release. Local anesthesia with bupivacaine hydrochloride (5 mg/mL) and epinephrine (5 µg/mL) was used for anesthesia in all cases. The maximum dose never exceeded 5 mL. The length of the skin incision in the wrist area was 3–4 cm. Bipolar diathermy was used for hemostasis. The flexor retinaculum was incised with scissors and epineural neurolysis was performed when deemed appropriate. Skin was closed using single sutures. A tourniquet was not used for regional hemostasis. A neutral-position wrist splint was used for postoperative immobilization for 2 weeks.
The data collected at the interview included the efficiency of surgical treatment at the time of interview, any complaints related to CTS in the operated hand, and the number of preoperative steroid injections received. To evaluate the efficacy of treatment, we asked the patients to assess any alleviation of their preoperative symptoms on a numeric rating scale (NRS) from 0 to 100 points where 100 points corresponded to absolute regression of symptoms and 0 points corresponded to a lack of any effect of surgical treatment, including worsening of symptoms. Patients who were not free from symptoms were also asked about the presence of persistent or new complaints associated with CTS without any further assessment of severity of complaints. Concerning persistent or new complaints, we addressed disease-associated symptoms such as nocturnal awakening, paresthesiae, pain, muscular weakness, and numbness. The injections had been administered by neurologists who had referred the patients to a surgeon from a catchment area corresponding to around 500,000 people. The period over which the injections had been received was not limited to a specific interval before the surgery. The patients were not specifically aware of the study hypothesis, and the question regarding the number or corticosteroid injections was the last one to be asked.
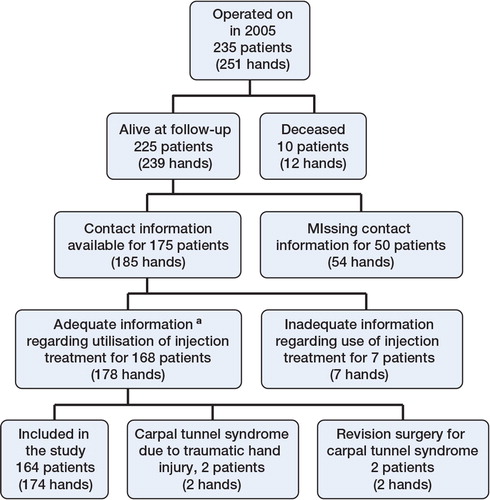
Of the 251 hands (235 patients) operated on in 2005, 174 hands (164 patients) were included in the study (). 10 patients had already died at the time of interview; 2 of them had had bilateral operations in 2005. For 50 patients the contact information was incomplete, which meant that 54 hands had to be excluded. 7 patients could not recall whether or not they had received local steroid injections and they were also excluded. In 2 patients CTS was caused by a traumatic hand injury and in 2 patients the carpal tunnel release was a revision operation.
Figure 1. Inclusion of patients. a Information about steroid injections was considered to be adequate if the patients remembered being injected. Due to the limitations in study design, the patient-reported numbers were not objectively verified by medical source data, although none of the patients specifically expressed difficulty in recalling the number of injections.
The mean age of the patients in the study at the time of interview was 60 years (range 32–93, SD 11.5). 25 patients were male (25 hands, 14%) and 138 were female (149 hands, 86%).
Statistics
The relationship between the presence of specific complaints and the number of injections received was analyzed using a random-effects logistic regression model adjusted for age and sex. A log-binomial model for binary outcomes was used to estimate relative risks (RRs). The relationship between the number of injections and regression of symptoms was examined with Poisson test. Results were considered to be statistically significant when the p-value was less than or equal to 0.05. Data were analyzed using the software packages R (version 2.15.2) and PASW Statistics 18.
Results
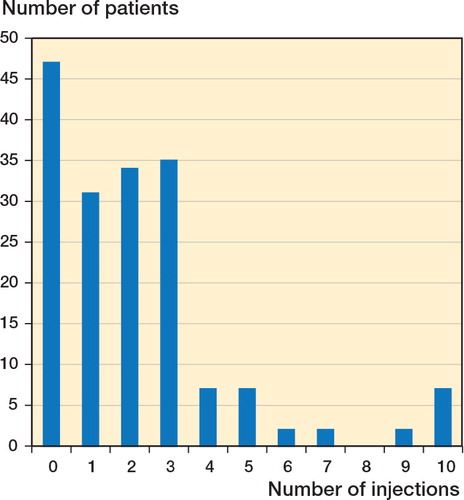
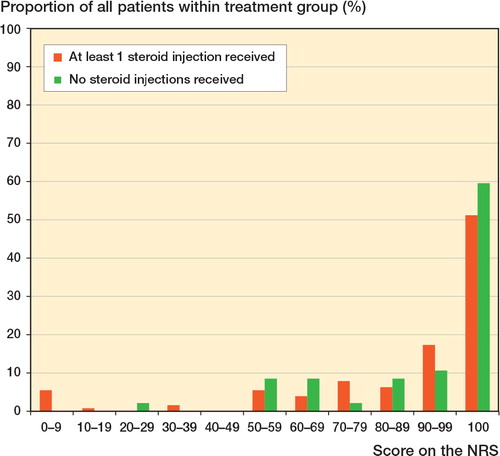
127 hands (73%) had received local steroid injections. On average, each hand had received 2.2 injections (range 0–10, SD 2.4). 27 patients had received more than 3 injections (). For 120 hands (69%), the patients judged their regression of symptoms to be equal to or greater than 90 points on the NRS (). The mean NRS score given by the patients for their regression of symptoms was 85 points (0–100, 95% CI: 81–89). The mean NRS score did not differ significantly in patients who had received steroid injections and those who had not, with the mean score in the former being 88 points (20–100, CI: 83–94) and that in the latter being 84 points (0–100, CI: 79–88). 93 hands (53%) were completely free from symptoms at the time of interview. 40 patients still complained about the occurrence of paresthesiae, 40 of pain, 36 of numbness, 30 of muscle weakness, and 18 of nocturnal awakening.
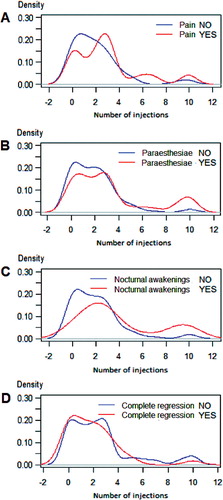
The risk of occurrence of all complaints was higher in patients who had received local steroid injections before surgery than in those who had not, although the increased risk was statistically significantly higher for pain, paresthesiae, and nocturnal awakenings. Each subsequent injection increased the risk of occurrence of pain (RR = 1.1, 95% CI: 1.02–1.2. p = 0.04), paresthesiae (RR = 1.1, CI: 1.1–1.2, p = 0.007), and nocturnal awakening (RR = 1.2, CI: 1.2–1.4, p = 0.003). Patients who had specific complaints had received more injections on average than those with no complaints ( and ). The same was true for patients who had incomplete regression of symptoms. There was a statistically insignificant weak association between the number of injections and the score given to the regression of symptoms.
Distribution of injections among patients with and without specific complaints and complete regression of symptoms
Discussion
The effect of local injection treatment before the operation on the long-term outcome of carpal tunnel release has not been described in the literature. The results of our findings indicate that those surgically treated patients who had received a greater number of steroid injections preoperatively are at an increased risk of suffering from pain, paresthesiae, and nocturnal awakening.
Treatment with local steroid injections improves the clinical symptoms of CTS in the short term, and it has been considered to be safe (Armstrong et al. Citation2004, Milo et al. Citation2009). Patients with CTS have a higher tissue pressure (32–110 mmHg) within the carpal tunnel than patients with normal hands (2–31 mmHg) (Gelberman et al. Citation1981). The potential mechanism of action of local steroid injection has been thought to involve reduction of swelling in the flexor tendon synovials (Carlson et al. Citation2010). However, as the Schwann cells of peripheral nerves express glucocorticoid receptors and because glucocorticoids promote the formation of myelin in vitro, it is possible that the clinical effect of steroid injections in CTS is at least in part based on the modulation of myelin synthesis (Morisaki et al. Citation2010). Improvement in electrophysiological parameters as opposed to clinical symptoms after local steroid injections is moderate—and even minimal in moderate and severe forms of the disease (Prick et al. Citation2003, Lee et al. Citation2009, Milo et al. Citation2009).
The main complication of local steroid injections is intraneural injection of steroid, which can cause degeneration of myelin and axons (Haase Citation2007). However, the incidence of median nerve injury from intraneural injection has been estimated to be less than 0.1% when performed by an experienced physician. It has not been established how many times an injection should be repeated and how long the period between successive injections should be. It has been suggested that a positive response to a steroid injection might predict the efficacy of surgical treatment (Carlson et al. Citation2010). The patients in our study who had received more steroid injections had a greater risk of occurrence of pain, paresthesiae, and nocturnal awakenings, which might support the notion of favoring a smaller number of injections.
Furthermore, there is a lack of consensus on the long-term effectiveness of steroid injections (Bland Citation2007). Some authors have found that 18 months on average after an injection, 22% of patients are completely free from complaints (Gelberman et al. Citation1980). Shorter duration of symptoms before the initiation of injection therapy appears to be a positive predictor of outcome of treatment (Kaplan et al. Citation1990). A study conducted by Padua et al. in 2001 on the natural history of CTS found that after a period of 10–15 months, roughly a quarter of all patients improved spontaneously without any therapy, a quarter worsened, and about one half remained the same. There tended to be clinical worsening in those who had been diagnosed with a mild form of CTS at presentation, and there tended to be improvement in those who initially presented with more severe disease (Padua et al. Citation2001). Thus, it cannot be excluded that an apparently good long-term response to steroid injections might be caused by the natural course of the disease.
Our results also indicated that 5 years after the operation, two-thirds of all patients considered the regression of symptoms to be excellent (90–100 points). These results are in accordance with previously published reports (Prick et al. Citation2003, Milo et al. Citation2009).
Our study had several limitations. As it was retrospective, we lacked data on the reasons why some patients had received more injections than others. Therefore, a more frequent occurrence of symptoms may have been the result of a more severe disease at presentation, which had progressed to a stage where surgical treatment failed to provide sufficient relief. Since not all steroid injections were performed at Tartu University Hospital, it is also possible that the patients who had received more injections were later referred for surgical treatment, which could have had a negative effect on the long-term outcome. Also, the number of injections received was based on the information provided by patients themselves, leaving the possibility of recall bias.
As the groups were not randomized, we are unable to assess the causality of relationships observed. We can only assume that patients referred to surgical treatment had moderate or severe disease. Also, we lack data concerning the outcome of patients who never proceeded to surgery after a local steroid injection.
The lack of assessment of complaint severity could also be considered to be a limitation. There were patients in the study who complained of pain but rated their regression of symptoms to be equal to or greater than 90 points. On the other hand, there were patients with pain who judged the effect of treatment to be non-existent. Although the assessment of pain is also to some extent reflected in the assessment of regression of symptoms, it would have been interesting to see if there was an association between treatment received and the intensity of pain. It has been demonstrated that many CTS patients who have undergone surgical release consider the operation to have been unsuccessful if pain still persists in the wrist region (Prick et al. Citation2003). Since we had no information about the occurrence of preoperative pain, it is possible that patients with pain rated the regression of their symptoms more pessimistically than those in whom pain was not a feature of the clinical presentation of CTS. This, in turn, could have had an influence on the results.
As we did not perform electroneuromyography on our patients 5 years after the operation, we were unable to assess the effect of preoperative steroid injections on the electrophysiological parameters. Studies have shown that immediate surgical treatment for electrodiagnostically established CTS is more cost effective than conservative treatment with steroid injections and bracing (Korthals-de Bos et al. Citation2006, Pomerance et al. Citation2009). The optimization of pre- and postoperative treatment in carpal tunnel release should be a topic for further research—considering the prevalence of CTS, the economic loss caused by such disability, and its burden on the healthcare system.
The work presented here was carried out through collaboration by all the authors. PSV collected and interpreted the data, performed statistical analysis, and drafted the manuscript. MK performed statistical analysis, interpreted the data, and revised the manuscript. LK made significant revisions to the manuscript and contributed to the literature overview. MB defined the hypothesis, designed the study, interpreted the data, and made major revisions to the manuscript.
No competing interests declared.
- Armstrong T, Devor W, Borschel L, Contreras R. Intracarpal steroid injection is safe and effective for short-term management of carpal tunnel syndrome. Muscle Nerve 2004; 29 (1): 82-8.
- Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosén I. Prevalence of carpal tunnel syndrome in a general population. JAMA 1999; 282 (2): 153-8.
- Bland JD. Carpal tunnel syndrome. BMJ 2007; 335 (7615): 343-6.
- Carlson H, Colbert A, Frydl J, Arnall E, Elliot M, Carlson N. Current options for nonsurgical management of carpal tunnel syndrome. Int J Clin Rheumatol 2010; 5 (1): 129-42.
- Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet 2010; 376 (9754): 1751-67.
- Gelberman RH, Aronson D, Weisman MH. Carpal-tunnel syndrome. Results of a prospective trial of steroid injection and splinting. J Bone Joint Surg (Am) 1980; 62 (7): 1181-4.
- Gelberman RH, Hergenroeder PT, Hargens AR, Lundborg GN, Akeson WH. The carpal tunnel syndrome: a study of carpal canal pressures. J Bone Joint Surg (Am) 1981; 63 (3): 380-3.
- Haase J. Carpal tunnel syndrome—a comprehensive review. Adv Tech Stand Neurosurg 2007; 32: 175-249.
- Huisstede BM, Hoogvliet P, Randsdorp MS, Glerum S, van Middelkoop M, Koes BW. Carpal tunnel syndrome. Part I: Effectiveness of nonsurgical treatments—a systematic review. Arch Phys Med Rehabil 2010a; 91 (7): 981-1004.
- Huisstede BM, Randsdorp MS, Coert JH, Glerum S, van Middelkoop M, Koes BW. Carpal tunnel syndrome. Part II: Effectiveness of surgical treatments—a systematic review. Arch Phys Med Rehabil 2010b; 91 (7): 1005-1024.
- Kaplan SJ, Glickel SZ, Eaton RG. Predictive factors in the non-surgical treatment of carpal tunnel syndrome. J Hand Surg Br 1990; 15 (1): 106-8.
- Korthals-de Bos IB, Gerritsen AA, van Tulder MW, Rutten-van Mölken MP, Adèr HJ, de Vet HC, Bouter LM. Surgery is more cost-effective than splinting for carpal tunnel syndrome in the Netherlands: results of an economic evaluation alongside a randomized controlled trial. BMC Musculoskelet Disord 2006; 7: 86.
- Lee JH, An JH, Lee SH, Hwang EY. Effectiveness of steroid injection in treating patients with moderate and severe degree of carpal tunnel syndrome measured by clinical and electrodiagnostic assessment. Clin J Pain 2009; 25 (2): 111-5.
- Milo R, Kalichman L, Volchek L, Reitblat T. Local corticosteroid treatment for carpal tunnel syndrome: a 6-month clinical and electrophysiological follow-up study. J Back Musculoskelet Rehabil 2009; 22 (2): 59-64.
- Morisaki S, Nishi M, Fujiwara H, Oda R, Kawata M, Kubo T. Endogenous glucocorticoids improve myelination via Schwann cells after peripheral nerve injury: An in vivo study using a crush injury model. Glia 2010; 58 (8): 954-63.
- Padua L, Padua R, Aprile I, Pasqualetti P, Tonali P. Multiperspective follow-up of untreated carpal tunnel syndrome: a multicenter study. Neurology 2001; 56 (11): 1459-66.
- Pomerance J, Zurakowski D, Fine I. The cost-effectiveness of nonsurgical versus surgical treatment for carpal tunnel syndrome. J Hand Surg Am 2009; 344 (7): 1193-200.
- Prick JJ, Blaauw G, Vredeveld JW, Oosterloo SJ. Results of carpal tunnel release. Eur J Neurol 2003; 10 (6): 733-6.
- Shi Q, Macdermid JC. Is surgical intervention more effective than non-surgical treatment for carpal tunnel syndrome? A systematic review. J Orthop Surg Res 2011; 6 (1): 17.
- Shiri R, Miranda H, Heliövaara M, Viikari-Juntura E. Physical work load factors and carpal tunnel syndrome: a population-based study. Occup Environ Med 2009; 66 (6): 368-73.
- Stephens MB, Beutler AI, O’Connor FG. Musculoskeletal injections: a review of the evidence. Am Fam Physician 2008; 78 (8): 971-6.
- Verdugo RJ, Salinas RA, Castillo JL, Cea JG. Surgical versus non-surgical treatment for carpal tunnel syndrome. Cochrane Database Syst Rev 2008 Oct 8; (4): CD001552.