Abstract
Background and purpose — The pathomechanics of the Essex-Lopresti lesion are not fully understood. We used human cadavers and documented the genesis of the injury with high-speed cameras.
Methods — 4 formalin-fixed cadaveric specimens of human upper extremities were tested in a prototype, custom-made, drop-weight test bench. An axial high-energy impulse was applied and the development of the lesion was documented with 3 high-speed cameras.
Results — The high-speed images showed a transversal movement of the radius and ulna, which moved away from each other in the transversal plane during the impact. This resulted into a transversal rupture of the interosseous membrane, starting in its central portion, and only then did the radius migrate proximally and fracture. The lesion proceeded to the dislocation of the distal radio-ulnar joint and then to a full-blown Essex-Lopresti lesion.
Interpretation — Our findings indicate that fracture of the radial head may be preceded by at least partial lesions of the interosseous membrane in the course of high-energy axial trauma.
The Essex-Lopresti lesion is a rare but severe injury of the human forearm. It is defined as a fracture of the radial head, a rupture of the interosseous membrane, and a disruption of the distal radio-ulnar joint () (Essex-Lopresti Citation1951). While the fracture of the radial head can easily be seen on plain radiographs, lesions of the interosseous membrane and the distal radio-ulnar joint may be missed (Jungbluth et al. Citation2006, Götz and Schulz Citation2013), leading to longitudinal forearm instability (Green and Zelouf Citation2009, Wegmann et al. Citation2012).
Figure 1. An Essex-Lopresti lesion: comminuted fracture of the radial head, resulting in proximalization of the radius and dislocation of the unstable distal radio-ulnar joint.

The pathobiomechanics of the lesion are not fully understood. It is not known which structure yields first. The radial head is known to be the primary longitudinal stabilizer of the forearm (Green and Zelouf Citation2009), which together with the interosseous membrane transfers load from the hand to the elbow, while the load transfer shifts towards the membrane when the radial head is deficient (Markolf et al. Citation2000, Shepard et al. Citation2001).
We created an artificial Essex-Lopresti lesion in human cadaveric upper extremities by the use of a custom-made test bench, and documented the chronological order of the development of the 3 lesions with high-speed video cameras.
Materials and methods
Specimen preparation
We used 4 formalin-fixed arms. The specimens came from 2 female and 2 male volunteer body donors with an average age of 84 (74–91) years. The specimens were disarticulated at the shoulder joint and screened for adequate range of motion and for preexisting bony pathologies by fluoroscopy in anteroposterior and lateral view. The humerus was cut at midlevel. The phalanges were resected to allow easier potting. The skin and the complete soft tissue envelope including the muscles were removed to view the radial head, the interosseous membrane, and the distal radio-ulnar joint. The joint capsules and ligaments at the elbow and at the wrist joint were preserved. Care was taken to spare the central band of the interosseous membrane as well as the distal and proximal oblique cord (Noda et al. Citation2009).
Test bench and custom-fit specimen fixation
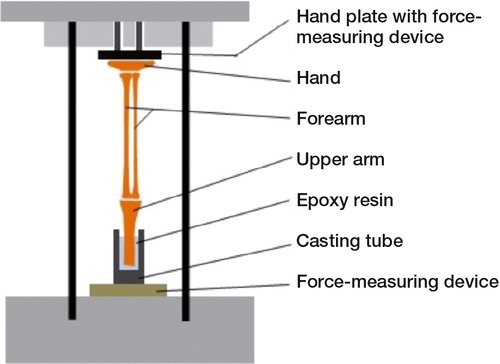
The test bench was designed and constructed for the sole purpose of trauma simulation in the upper extremities. McGinley et al. (2009) reported that energies in the range 73.5–294 J induced Essex-Lopresti lesions. To generate a high-speed impact with impact velocities higher than 4 m/s, we constructed a drop-weight test bench that allows generation of impact energy up to 400 J and potential peak forces of up 4.5 kN. The impulse is generated by a crosshead, which is held and can be released by an electromagnet. The crosshead hits against an impact stamp to transmit the impulse almost without friction onto the wrist of each specimen. The proximal end of the specimen, the cut humerus, was potted to a shiftable socket at the ground plate ().
In the constructed test bench, the amount of energy created can be altered by the drop height (0.5–1.3 m) and by adding weight to the crosshead (11.7 kg if unloaded, up to 26.8 kg). We chose a weight of 21.6 kg to be added to the crosshead and a falling height of 1 m, to create a calculated impact speed of crosshead of about 4 m/s. With these parameters, we aimed to create kinetic energy of about 210 J hitting the specimen.
An essential part of the experiments was the adequate positioning and fixation of the specimens in the test bench. To allow the radius and ulna to move independently after impact, the energy had to be applied to the proximal carpal row. This was achieved by acrylate-potting of the distal carpal row and the metacarpals in a hollow cylinder, which was clamped on a special hand-plate with an integrated coordinate system. The specimen was placed in such a way that the wrist was at 0° of extension/flexion, and the forearm in full pronation. This position has been suggested to lead to the Essex-Lopresti lesion in a trauma situation (McGinley et al. Citation2003). In addition, we chose to set the elbow in 15° of flexion, which made specimen fixation in the test bench easier.
The center of the impact stamp stood vertically in the center of the proximal force sensor. The cut humerus was also potted using acrylate cement and fixed with the hollow cylinder against the shiftable baseplate, which was centered over the distal force sensor. The shiftable baseplate allowed 2-dimensional adjustment of the position of the specimen. With this fixation method, almost any desirable alignment of the specimens could be achieved.
Force measurements and video documentation
For control reasons, 2 force sensors were mounted on the test bench. 1 sensor (piezo-electric measuring sensors, Kistler type 9011A; Kistler, Winterthur, Switzerland) with a frame rate of 45 kHz was placed proximally in the impact stamp, and a second one (Kistler type 9061A) with a frame rate of 100 kHz was placed between the slide unit and the hollow cylinder distally. The raw signal was transformed with an 8-channel charge amplifier (Kistler type 9865E). The force signals were scanned by an AD/DA module from National Instruments (USB-6259; National Instruments Corporation, Austin, TX).
3 high-speed cameras (type HCC 1000 (F) BGE, Vosskuehler; Allied Vision Technologies GmbH, Stadtroda, Germany) were used to record the impact at 1,825 frames per second, with an image resolution of 1024 × 256 pixels, and they were aligned at an angle of 120° each, to achieve a 360° view around the specimen. Every camera pointed either to the radial head, the interosseous membrane, or the distal radio-ulnar joint. The high-speed cameras, the force sensors, and the triggering of the magnetic clamp were synchronized and started simultaneously. Customized simulator software for synchronization and data recording was programmed using the LabVIEW development environment (ver. 2010; National Instruments Corporation).
Results
Full Essex-Lopresti lesions were created in the 4 specimens. The application of about 200 J to the wrist via crosshead 2 led to a fracture of the radial head, a disruption of the interosseous membrane, and a dislocation of the distal radio-ulnar joint. The high-speed video documentation revealed the sequence of the development of the lesions in the cadaver models ( and ).
Figure 3. Part 1 of the sequence of development of an Essex-Lopresti lesion. A. Unloaded specimen. B. Loading leads to slight impaction and bending of radius and ulna, and thereby to a transverse movement of the radial and ulnar shaft away from each other (see increasing distance between radial and ulnar shaft), leading to tension of the interosseous membrane (IOM). C. Due to the rising tension in the IOM, the IOM ruptures and ulna and radius separate further. D. A slight proximalization of the radius—and thereby of the radial head—is detectable (see movement of radial head in relation to the black line).
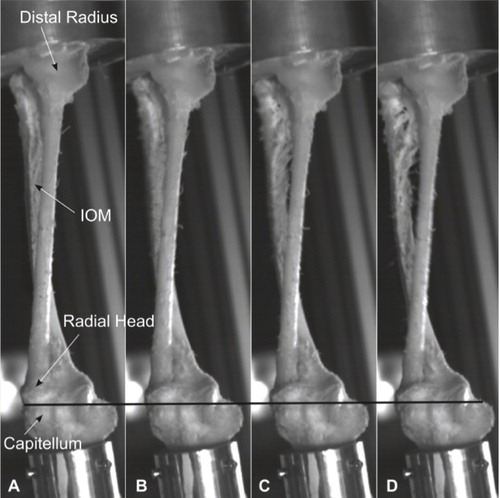
Figure 4. Part 2 of the sequence of development of an Essex-Lopresti lesion. A. The intraosseous membrane is completely ruptured. Radius moves downwards (proximal direction), leading to fracture of the radial head and increasing displacement (again in relation to the black line). B–D. The lesion progresses to a dislocation of the distal radio-ulnar joint, then to a full Essex-Lopresti lesion.
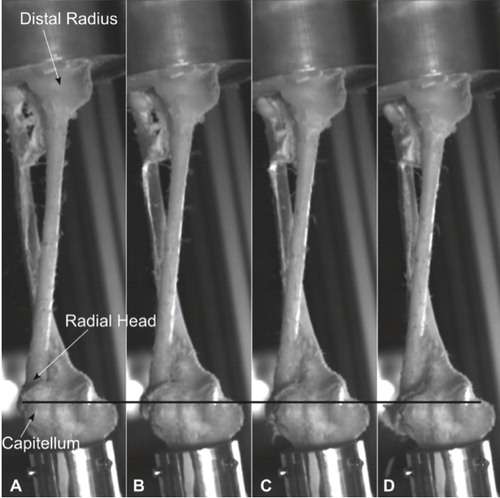
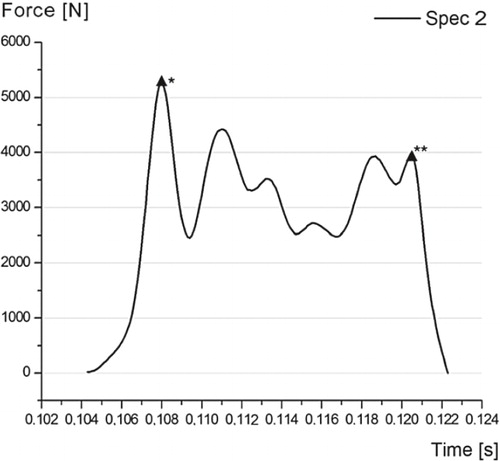
According to the high-speed images, radius and ulna bow away from each other in the transversal plane under the explosive loading conditions, due to bending of the 2 bones. This leads to tension in the interosseous membrane in a transversal direction. Thus, with increasing axial load, the interosseous membrane ruptures in a transversal direction. An immediate proximal movement of the radius towards the capitellum was noticed in the images. This forceful proximalization of the radius then led to fracture of the radial head and the subluxation of the radio-capitellar joint (). The displacement of the radius against the ulna led to dislocation of the distal radio-ulnar joint, resulting in a full-blown Essex-Lopresti lesion. The observations regarding the chronological order of the development of the lesions were consistent in all 4 specimens (Table). The force measurements showed that the initiated impulse (superior force sensor) was higher than the diverted impulse (inferior force sensor), representing a damping action by the specimen.
Initiated and diverted impulses, calculated with the measured forces (Ns) of the superior and inferior sensor
Figure 5. Curve representing force over time in specimen 2. * marks the moment of failure of the interosseous membrane, as in Figure 3C. ** marks the moment of fracture and proximalization of the radius, as in Figure 4B. The irregular lines in-between can be explained by dislocation movements of the radial head before the fracture, resulting in complete longitudinal instability.
Discussion
Owing to the lack of fresh human bones, formalin-fixed specimens are frequently used in biomechanical testing, and this is what we did. It has been shown that formalin alters bone and soft tissues by crosslinking the proteins without altering the secondary structure (Wilke et al. Citation1996, Burkhart et al. Citation2010). Thus, we cannot claim to have created fully realistic conditions, despite the laborious setup.
Full-blown Essex-Lopresti lesions are rare entities. In 2003, CitationMcGinley et al. were the first to simulate complex forearm injuries with a drop-weight test bench (McGinley et al. Citation2003). They investigated the influence of different rotational positions of the forearm on the resulting lesion. With the specimen in pronation, Essex-Lopresti lesions were created repeatedly. In the present setup, we used pronation in addtition with slight flexion. This also led to the desired injuries. We chose 15° flexion of the elbow, as it made positioning of the specimens in the test bench much easier. Unlike CitationMcGinley et al., we documented the development of the lesion visually.
In a recent MRI study, it was supposed that even in low-grade radial head fractures, involvement of the corresponding soft tissues is more likely than previously assumed (Hausmann et al. Citation2009). When performing MR imaging on 14 patients with Mason type-I radial head fractures, at least partial lesions of the interosseous membrane were found in 9 of the individuals. It is common knowledge that a high incidence of concomitant injuries of the collateral ligaments is encountered with fractures of the radial head (Davidson et al. Citation1993, Itamura et al. Citation2005). In our experimental setup, we found that through application of high-energy loads, the first structure to yield was the interosseous membrane due to transverse movement of the radius and ulna. The longitudinal stabilizing effect of the interosseous membrane is thereby lost, followed by the fracture of the radial head.
It cannot be stated from our study that every fracture of the radial head is accompanied with a relevant injury to the interosseous membrane or the distal radio-ulnar joint. On the one hand, we used fixed specimens—and on the other hand, the dynamic stabilizing effect of the forearm muscles was absent. Yet the results of the study indicate a connection between the lesion of the interosseous membrane and of the one of the radial head in high-energy axial trauma to the forearm. We must emphasize awareness of complex lesions of the forearm when treating radial head fractures. Clinical and radiological examination of the whole forearm unit along with the medial and lateral elbow is important, so that concomitant ligamentous injuries will not be missed. If radial head fractures are operated on, one should consider intraoperative tests to check for longitudinal forearm instability (Smith et al. Citation2002, Soubeyrand et al. Citation2006).
All the authors contributed to interpretation of the data and to revision of the final manuscript. KW, KB, KE, ME, and RH conducted the experiments. PB and LM contributed to the conception of the study and wrote the study protocol. KE, ME, and RH collected and analyzed the data. KE, ME, and RH did the statistical analysis. KW wrote the first draft of the manuscript.
No competing interests declared.
- Burkhart KJ, Nowak TE, Blum J, Kuhn S, Welker M, Sternstein W, et al. Influence of formalin fixation on the biomechanical properties of human diaphyseal bone. Biomed Tech (Berl) 2010; 55 (6): 361-5.
- Davidson PA, Moseley JB, Jr., Tullos HS. Radial head fracture. A potentially complex injury. Clin Orthop 1993; (297): 224-30.
- Essex-Lopresti P. Fractures of the radial head with distal radio-ulnar dislocation; report of two cases. J Bone Joint Surg (Br) 1951; 33 (2): 244-7.
- Götz LP, Schulz R. Komplexe instabile Luxationsfrakturen des Ellenbogens – Klinische Ergebnisse nach Versorgung unter prothetischem Ersatz des Radiusköpfchens. Obere Extremität 2013; 8 (1): 22-6.
- Green JB, Zelouf DS. Forearm instability. J Hand Surg Am 2009; 34 (5): 953-61.
- Hausmann JT, Vekszler G, Breitenseher M, Braunsteiner T, Vecsei V, Gabler C. Mason type-I radial head fractures and interosseous membrane lesions—a prospective study. J Trauma 2009; 66 (2): 457-61.
- Itamura J, Roidis N, Mirzayan R, Vaishnav S, Learch T, Shean C. Radial head fractures: MRI evaluation of associated injuries. J Shoulder Elbow Surg 2005; 14 (4): 421-4.
- Jungbluth P, Frangen TM, Arens S, Muhr G, Kalicke T. The undiagnosed Essex-Lopresti injury. J Bone Joint Surg (Br) 2006; 88 (12): 1629-33.
- Markolf KL, Dunbar AM, Hannani K. Mechanisms of load transfer in the cadaver forearm: role of the interosseous membrane. J Hand Surg Am 2000; 25 (4): 674-82.
- McGinley JC, Hopgood BC, Gaughan JP, Sadeghipour K, Kozin SH. Forearm and elbow injury: the influence of rotational position. J Bone Joint Surg (Am) 2003; 85 (12): 2403-9.
- Noda K, Goto A, Murase T, Sugamoto K, Yoshikawa H, Moritomo H. Interosseous membrane of the forearm: an anatomical study of ligament attachment locations. J Hand Surg Am 2009; 34 (3): 415-22.
- Shepard MF, Markolf KL, Dunbar AM. Effects of radial head excision and distal radial shortening on load-sharing in cadaver forearms. J Bone Joint Surg (Am) 2001; 83 (1): 92-100.
- Smith AM, Urbanosky LR, Castle JA, Rushing JT, Ruch DS. Radius pull test: predictor of longitudinal forearm instability. J Bone Joint Surg (Am) 2002; 84 (11): 1970-6.
- Soubeyrand M, Oberlin C, Dumontier C, Belkheyar Z, Lafont C, Degeorges R. Ligamentoplasty of the forearm interosseous membrane using the semitendinosus tendon: anatomical study and surgical procedure. Surg Radiol Anat 2006; 28 (3): 300-7.
- Wegmann K, Dargel J, Burkhart KJ, Bruggemann GP, Muller LP. The Essex-Lopresti lesion. Strategies Trauma Limb Reconstr 2012; 7 (3): 131-9.
- Wilke HJ, Krischak S, Claes LE. Formalin fixation strongly influences biomechanical properties of the spine. J Biomech 1996; 29 (12): s1629-31.