Abstract
Background and purpose An earlier Nordic Arthroplasty Register Association (NARA) report on 280,201 total hip replacements (THRs) based on data from 1995–2006, from Sweden, Norway, and Denmark, was published in 2009. The present study assessed THR survival according to country, based on the NARA database with the Finnish data included.
Material and methods 438,733 THRs performed during the period 1995–2011 in Sweden, Denmark, Norway, and Finland were included. Kaplan-Meier survival analysis was used to calculate survival probabilities with 95% confidence interval (CI). Cox multiple regression, with adjustment for age, sex, and diagnosis, was used to analyze implant survival with revision for any reason as endpoint.
Results The 15-year survival, with any revision as an endpoint, for all THRs was 86% (CI: 85.7–86.9) in Denmark, 88% (CI: 87.6–88.3) in Sweden, 87% (CI: 86.4–87.4) in Norway, and 84% (CI: 82.9–84.1) in Finland. Revision risk for all THRs was less in Sweden than in the 3 other countries during the first 5 years. However, revision risk for uncemented THR was less in Denmark than in Sweden during the sixth (HR = 0.53, CI: 0.34–0.82), seventh (HR = 0.60, CI: 0.37–0.97), and ninth (HR = 0.59, CI: 0.36–0.98) year of follow-up.
Interpretation The differences in THR survival rates were considerable, with inferior results in Finland. Brand-level comparison of THRs in Nordic countries will be required.
There is a long tradition of arthroplasty registries in the Nordic countries. The Swedish Hip Arthroplasty Register was established in 1979 (Malchau et al. Citation2002), the Finnish Arthroplasty Register in 1980 (Paavolainen et al. Citation1991, Puolakka et al. Citation2001), the Norwegian Arthroplasty Register in 1987 (Havelin et al. Citation2000), and the Danish Hip Arthroplasty Register in 1995 (Lucht Citation2000). The Nordic Arthroplasty Register Association (NARA) was established in 2007 by Sweden, Norway, and Denmark to improve the quality of total hip and knee arthroplasty through registry-based research collaboration. Finland became a full member of NARA in 2010.
A multinational implant registry is needed in order to detect inferior implants as early as possible. To date, the NARA database is the most developed multinational database worldwide. However, NARA results are not available on the internet or in yearbooks; the information is shared using scientific papers. Monitoring and comparison of country-specific results is a step forward in the development of NARA activity. An earlier NARA report on 280,201 THRs, based on data from the period 1995–2006 from Sweden, Norway, and Denmark, was published in 2009 (Havelin et al. Citation2009). In the present paper, we have updated the survival results for THR in the Nordic countries with the Finnish data included and we consider and discuss the differences found.
Material and methods
Sources of data
The registries of Sweden, Denmark, Norway, and Finland participated. From 1995, all 4 registries have used individual-based registration of operations and patients. The data therefore include THRs performed during the period 1995–2011. A minimal NARA dataset was created to contain data that all registries could deliver (Havelin et al. Citation2009). The degree of coverage and completeness of the Nordic registries is high (Arthursson et al. 2005, Espehaug et al. Citation2006, CitationDHAR 2011, CitationSHAR 2011, Peltola 2013).
Selection and transformation of the respective datasets and de-identification of the patients, including deletion of the national civil registration numbers, was performed within each national registry. Anonymous data were then merged into a common database.
Ethical approval of the study was obtained through each national registry.
Inclusion and exclusion criteria
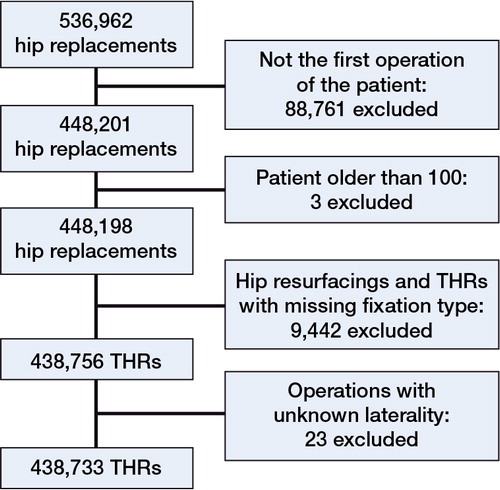
Until 2011, 536,962 primary hip replacements had been included in the NARA database. A flow chart of the exclusion of hip replacements according to our study criteria is presented in . If a patient had replacement of both hips in the database, only the first one was included due to potential bias from bilaterality (Ranstam et al. Citation2011). We also wanted to make sure that the potential errors in recording of laterality did not bias the analyses. 88,723 hips were excluded due to the bilaterality criteria. 38 revision operations were excluded. The 3 patients over 100 years old were excluded from the study due to suspected coding errors. 2,312 hip replacements were excluded because information on the type of fixation was not available. 7,130 hip resurfacings were excluded from the analyses. In addition, 3 patients were excluded due to having “bilateral” as an operative side. 20 hips were excluded because the laterality of the first operation was not mentioned.
Altogether, 438,733 hip replacements were included: 278,315 cemented, 101,940 uncemented, 36,322 hybrid (uncemented cup, cemented stem), and 22,156 reverse hybrid (cemented cup, uncemented stem).
Statistics
We used Kaplan-Meier analysis to study prosthetic survival at 10 and 15 years until there were at least 100 THRs left at risk. Patients were censored at death or December 31, 2011, whichever came first. Outcome was any revision, defined as removal or exchange of at least 1 of the components. Liner exchanges were recorded under the same label as cup revisions in the NARA hip database. We used a Cox multiple regression model to assess survival and hazard ratio (HR) with any revision as endpoint, with confidence interval CI, and with adjustment for age, sex, and diagnosis. The stratification was made with the age groups and diagnoses given in . Adjustments were made by stratifying with age groups, diagnosis, and sex for data given in Tables 4 and 5. Adjustments were made by stratifying with diagnosis for data given in Tables 6 and 7 (subgroup analyses). Sweden was chosen as the reference country, because the Swedish Hip Arthroplasty Register had the highest number of THRs recorded.
Table 1. Demographic data, and data concerning fixation technique, surgical approach, cause of revision, and procedure performed at revision for each country
Because the factor country analysis did not fulfill the proportional hazards assumption, the follow-up period was split into 1-year time periods in the analysis of all THRs, cemented THR, and uncemented THR. Also, the first year was divided into 2 periods to assess early postoperative revisions.
The follow-up period for hybrid and reverse hybrid THRs was split into 3-year time periods because of the relatively low number of cases. The first year was divided into 2 periods, < 6 months and 6–24 months, followed by the third period from 2 to 5 years and so on.
We performed survival analyses separately for subgroups of female and male patients aged < 60 years and ≥ 60 years with cemented or uncemented THRs. Because countrywise subgroup analyses did not fulfill the proportional hazards assumption either, the follow-up period for subgroup analysis was split into periods in the same way as for hybrids and reverse hybrids, as described above.
We adjusted for diagnosis in subgroup analyses for female and male patients aged < 60 years and ≥ 60 years. The Wald test was used to calculate the p-values for data obtained from the Cox multiple regression analyses. Differences between groups were considered to be statistically significant if the p-values were < 0.05 in a 2-tailed test.
We performed time-trend analyses to assess changes in the revision rate over a 17-year period (1995 through 2011). The patients were divided into 3 groups according to the year of primary surgery: 1995–1999, 2000–2005, and 2006–2011. The first period, from 1995 through 1999, was used as the reference period. Kaplan-Meier survival analysis with 95% CIs was used to compare cumulative implant survival between subgroups of patients (i.e. patients operated during the 3 time periods).
Results
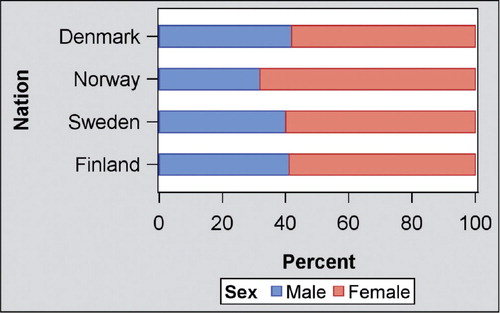
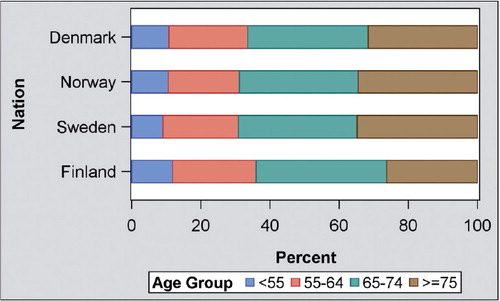
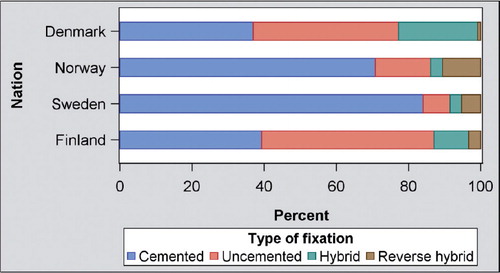
438,733 THRs fulfilled the inclusion criteria for the study (180,839 in Sweden, 92,078 in Denmark, 86,076 in Norway, and 79,740 in Finland). Data concerning demographics, fixation technique, surgical approach, cause of revision, and procedure performed at revision are presented for each country in and in , , and . The proportion of male patients was 42% in Denmark, 40% in Sweden, 32% in Norway, and 41% in Finland. The proportion of patients aged 75 years and over was 32% in Denmark, 35% in Sweden, 35% in Norway, and 26% in Finland. Hip fracture as an indication for THR was more common in Denmark (14%), in Sweden (12%), and in Norway (12%) than in Finland (3.7%). Uncemented fixation was common in Denmark (40%) and in Finland (48%), but rare in Sweden (7.5%) and in Norway (15%). Aseptic loosening was the most common cause of revision in all countries. Cup/liner revision was the most common procedure performed at revision in Denmark (44%), Sweden (32%), and Norway (37%). For Finland, the corresponding data were not available.
Kaplan-Meier 10- and 15-year survival data are presented by country for all THRs, cemented THR, uncemented THR, hybrid THR, and reverse hybrid THR in and . The 15-year survival for all THRs was 86.3% (CI: 85.7–86.9) in Denmark, 88.0% (CI: 87.6–88.3) in Sweden, 86.9% in Norway (CI: 86.4–87.4), and 83.5% (CI: 82.9–84.1) in Finland.
Table 2. Kaplan-Meier 10- and 15-year survival data with 95% CI for all THRs, cemented THR, uncemented THR, hybrid THR, and reverse hybrid THR by country. The 7.3-year survival of reverse hybrid THR in Denmark was 92.8% (95% CI: 90.3–94.7)
Figure 5. Kaplan-Meier survival for all total hip replacements in the NARA database (by country), with any reason for revision as endpoint.
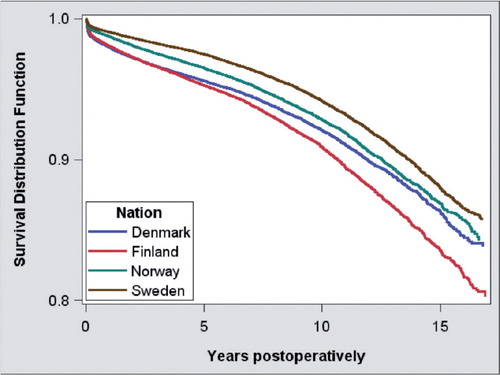
Figure 6. Kaplan-Meier survival for cemented total hip replacement in the NARA database (by country), with any reason for revision as endpoint.
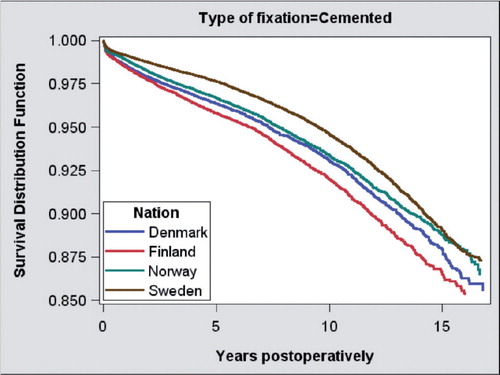
Figure 7. Kaplan-Meier survival for uncemented total hip replacement in the NARA database (by country), with any reason for revision as endpoint.
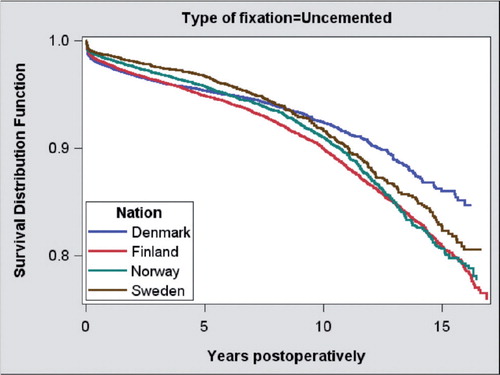
Figure 8. Kaplan-Meier survival for hybrid total hip replacement (cemented cup, cementless stem) in the NARA database, by country, with any reason for revision as endpoint.
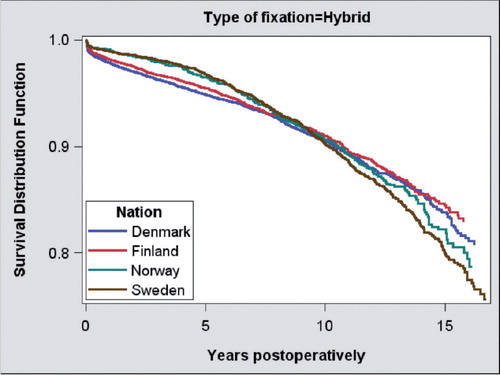
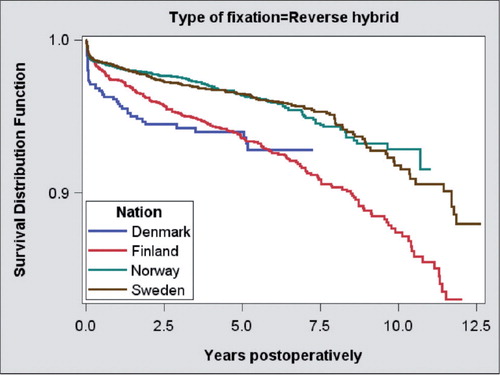
Figure 9. Kaplan-Meier survival for reverse hybrid total hip replacement (uncemented cup, cemented stem) in the NARA database, by country, with any reason for revision as endpoint.
Kaplan-Meier 10- and 15-year survival data for subgroup analyses performed separately for female and male patients aged < 60 years and ≥ 60 years are presented for cemented and uncemented THR by country in . The 15-year survival for uncemented THR in female patients aged < 60 years was 82.3% (CI: 79.4–84.7) in Denmark, 81.3% (CI: 77.8–84.3) in Sweden, 79.3% (CI: 76.8–81.5) in Norway, and 75.5% (CI: 73.4–77.5) in Finland. The 15-year survival for uncemented THR in male patients aged < 60 years was 87.2% (CI: 84.8–89.2) in Denmark, 82.1% (CI: 78.5–85.2) in Sweden, 78.0% (CI: 75.0–80.7) in Norway, and 80.1% (CI: 78.1–81.9) in Finland.
Table 3. Kaplan-Meier 10- and 15-year survival data with 95% confidence intervals from subgroup analyses performed separately for female and male patients aged < 60 years and ≥ 60 years and for cemented and uncemented THR, by country. The 9.7-year survival of uncemented THR in Sweden for female patients aged ≥ 60 years was 91.4% (95% CI: 86.5–94.5)
Revision risk for all THRs was statistically significantly less in Sweden than in all other countries during the first 5 years of follow-up (Table 4 (see supplementary data) and ).
Figure 10. Countrywise hazard ratio (HR) for risk of revision of all THRs compared to the reference country, Sweden (HR = 1). HRs are presented in 1-year time periods, except that the first year has been divided into 2 periods. If there were less than 20 cases in the group, the HRs were not included in the graphs due to the intervals being too wide. The model was stratified by sex, age group, and diagnosis.
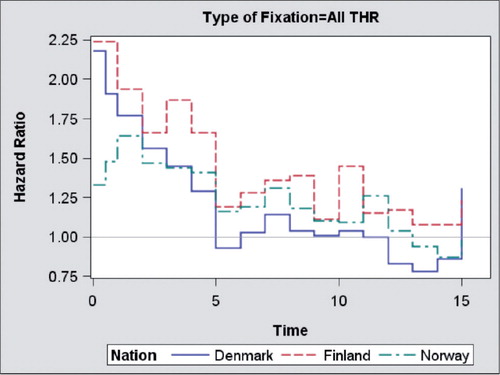
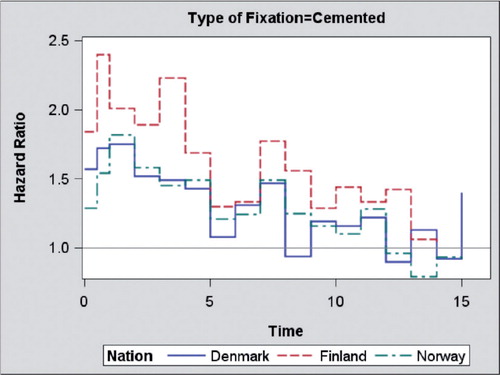
Revision risk for cemented THR was statistically significantly less in Sweden than in all other countries during the first 8 years of follow-up (Table 4 (see supplementary data) and ).
Figure 11. Countrywise hazard ratio (HR) for risk of revision of cemented THA compared to the reference country, Sweden (HR = 1). HRs are presented in 1-year time periods, except that the first year has been divided into 2 periods. If there were less than 20 cases in the group, the HRs were not included in the graphs due to the intervals being too wide. The model was stratified by sex, age group, and diagnosis.
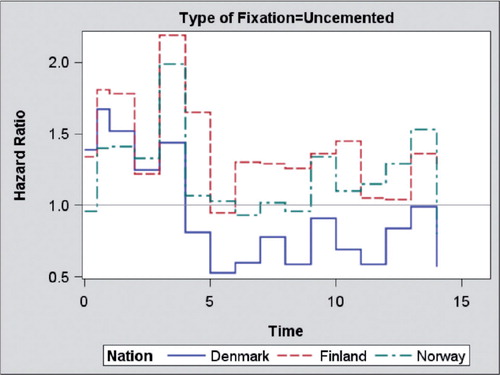
Regarding uncemented THR, the risk of revision was statistically significantly less in Denmark than in Sweden during the sixth year (HR = 0.53, CI: 0.34–0.82; p = 0.005), the seventh year (HR = 0.60, CI: 0.37–0.97; p = 0.04), and the ninth year (HR = 0.59, CI: 0.36–0.98; p = 0.04) of follow-up (Table 4 (see supplementary data) and ).
Figure 12. Countrywise hazard ratio (HR) for risk of revision of uncemented THA compared to the reference country, Sweden (HR = 1). HRs are presented in 1-year time periods, except that the first year has been divided into 2 periods. If there were less than 20 cases in the group, the HRs were not included in the graphs due to the intervals being too wide. The model was stratified by sex, age group, and diagnosis.
Revision risk for hybrid THR was less during the first 5 years after THR in Sweden than in Denmark and Finland. Revision risk for reverse hybrid THR was less in Sweden during the time period from 0.5 to 8 years after THR than for the equivalent period in Finland (Table 5, see supplementary data).
Revision risk for uncemented THR in male patients aged less than 60 years was less in Denmark during the time period from 5 to 14 years after THR than in Sweden (Table 6, see supplementary data). Revision risk for cemented THR in female patients aged less than 60 years was higher in Finland during the first 5 years and in male patients during the first 2 years after THR than in Sweden (Table 6, see supplementary data). Revision risk for cemented THR in women aged 60 years and over was higher in the 3 other countries than in Sweden during the first 8 years, except during the first half-year period in Norway (Table 7, see supplementary data). Revision risk for cemented THR in men aged 60 years and over was higher in Finland and Norway during the first 8 years than in Sweden (Table 7, see supplementary data).
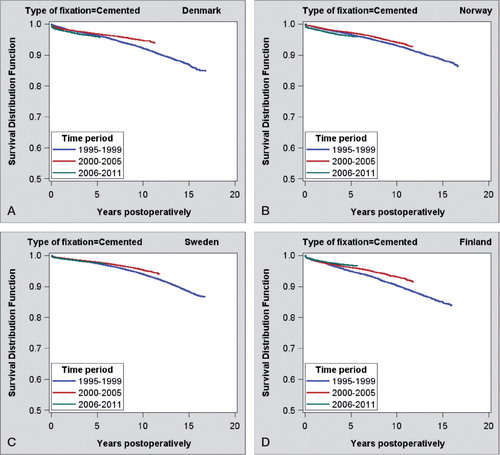
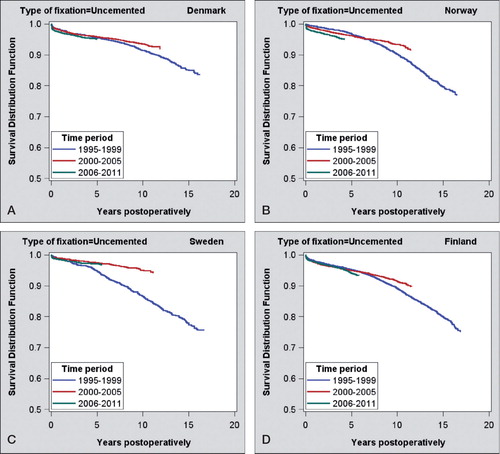
Results of time-trend analysis of cemented and uncemented THR in Denmark, Norway, Sweden, and Finland for the time periods 1995–1999, 2000–2005, and 2006–2011 are presented in Table 8 (see supplementary data) and in and . The 10-year survival of both cemented and uncemented implants was significantly higher in all countries for the time period 2000–2005 than for the time period 1995–1999. The 5-year survival of either cemented or uncemented implants, however, was not higher in any of the countries for the time period 2006–2011 than for the time period 2000–2005. The 5-year survival of uncemented implants was statistically significantly lower for the time period 2006–2011 than for the time period 1995–1999 in Finland (94.1%, CI: 93.6–94.6 vs. 95.2%, CI: 94.7–95.7) and in Norway (95.0%, CI: 94.2–95.7 vs. 96.8%, CI: 96.1–97.4).
Discussion
The differences in THR survival rates among Nordic countries were considerable. The inferior survival results in Finland are probably due to a high proportion of uncemented THRs with high amounts of liner wear revisions. Furthermore, increased use of uncemented implants in elderly patients increases the risk of early periprosthetic fractures. Overall revision risk for both cemented and uncemented THR was lower in Sweden than in the other countries. However, revision risk for uncemented THR was less in Denmark than that in Sweden towards the end of the follow-up, especially in male patients below 60 years of age. These differences may reflect different choices of implant in the different countries.
A major strength of our study was the unique collaboration of 4 national registries to create a multinational database with large numbers of patients and a long follow-up time. The main weakness of the present study was that the minimal NARA dataset includes only basic information common to all national registries. Our data did not include complete information on parameters such as bearing surface material, American Society of Anesthesiologists (ASA) grade, and patient-reported outcome measures (PROMs). Bearing surface data might be an important confounder when studying differences in revision risk between countries. However, we believe that the high number of implants in our study makes the bearing surface bias tolerable. Also, coding of diagnoses and reasons for revision are not the same in the 4 countries. One of the aims of the NARA collaboration is to standardize these issues.
Demographics
The proportion of female patients is higher in Norway than in the other Nordic countries, as described earlier (Lohmander et al. Citation2006, Havelin et al. Citation2009). It has been suggested that the high proportion of women is associated with the high incidence of pediatric hip disease in Norway (Havelin et al. Citation2009). However, the proportion of male patients in Norway has increased by 2 percentage points compared to our previous analysis (Havelin et al. Citation2009). The proportion of patients aged ≥ 75 years was lowest in Finland, and the proportions of the 2 youngest age groups were highest. The fact that overall, THRs are performed in younger patients in Finland than in the 3 other countries may in part explain the inferior implant survival in Finland.
There has been a substantial decrease in the incidence of THR in patients with rheumatoid arthritis after 2001, due to more effective pharmacological treatment (Hekmat et al. Citation2011). The proportion of patients with inflammatory arthritis has decreased in Denmark, Norway, and Sweden compared to our previous study—by about 1 percentage point in each country (Havelin et al. Citation2009). The proportion of patients with inflammatory arthritis was high in Finland. The incidence of inflammatory arthritis may be higher in Finland than in the other Nordic countries.
The proportion of patients with hip fracture was lowest in Finland. There may be inconsistency between countries in recording of acute hip fractures, late failed osteosynthes, and posttraumatic osteoarthritis. In Finland, cases of failed osteosyntheses are not recorded separately but as other reasons for secondary osteoarthritis. Furthermore, in Finland acute hip fractures are often treated with hemiarthroplasty, which may bias the results. Partial hip arthroplasty is not recorded separately in Finland and Denmark, unlike in Norway and in Sweden (Gjertsen et al. Citation2008, CitationSHAR 2011). Hemiarthroplasty data were not included in our study. The relative number of hip fractures has increased in Denmark compared to our earlier report. Hip fractures are also more common in Denmark than in Norway and Sweden (Havelin et al. Citation2009). This may be related to the increased amount of femoral neck fractures due to the aging population, or a tendency to treat more acute hemiarthroplasty with THR.
The proportion of patients who were operated for pediatric hip diseases was highest in Norway, which supports our previous findings (Havelin et al. Citation2009). Childhood hip diseases may be more common in Norway than in other Nordic countries. On the other hand, diagnostics and treatment of childhood diseases may have been different in earlier days compared to Sweden and Denmark (Havelin et al. Citation2009). The proportion of pediatric hip diseases was lowest in Finland, whereas the proportion of “other reasons for secondary OA” was highest in Finland. In the Finnish data collection form, there is an option called secondary osteoarthritis. Some pediatric hips are probably coded under the heading of secondary osteoarthritis along with dysplastic hips. Thus, we believe that the category “other reasons” in the NARA database most probably includes some Finnish patients with dysplastic hips. There have been no remarkable changes concerning the proportion of pediatric hip disease diagnosis in any of the 3 countries (Havelin et al. Citation2009).
The proportion of all THR diagnoses that are nontraumatic femoral head necrosis is low, and has remained the same in Denmark, Norway and Sweden (Havelin et al. Citation2009). The proportion of this diagnosis in Finland is lower than in other countries, which may be due to classification into “other reasons for secondary osteoarthritis”.
Implant fixation
The proportion of uncemented THRs was higher in Denmark and in Finland than in Sweden and Norway. The Swedish and Norwegian registries were established earlier than the Danish registry. The good results of cemented THR and the inferior results of some uncemented THR brands in Swedish and Norwegian registries have encouraged the continued use of cemented THR in these countries (Havelin et al. Citation2009). During the last 5 years, the proportion of uncemented THRs has also increased in Norway and in Sweden. The proportion of all THRs that are cemented THR has decreased by 9 percentage points in Denmark, 5 percentage points in Sweden, and 8 percentage points in Norway compared to the previous report (Havelin et al. Citation2009). Hybrids were highly common in Denmark and relatively rare in Norway and in Sweden. However, the proportion of hybrids has decreased by about 4 percentage points in Denmark compared to the previous report (Havelin et al. Citation2009). Reverse hybrids are more popular in Norway and Sweden than in Denmark and Finland. The proportion of reverse hybrids has increased in Norway compared to the previous NARA report (Havelin et al. Citation2009), probably due to good results with the concept being reported from the Norwegian national registry (Lindalen et al. Citation2011).
Approach
The posterior approach is common in Denmark but it is relatively rare in Norway. The relatively high number of revisions due to dislocation in Denmark may be associated with the posterior approach, as suggested earlier (Havelin et al. Citation2009). The proportion of posterior approach has remained unchanged in Denmark, Norway, and Sweden compared to our previous report (Havelin et al. Citation2009). In Finland, data on surgical approach have not been available.
Implant survival
The differences in survival rates for cemented THR among the Nordic countries were considerable. Revision risk for cemented THR was lowest in Sweden. The Swedish Hip Arthroplasty Register has provided feedback to the profession for more than 30 years. This appears to have led to the selection of implants with long documentation. Continued training and feedback to surgeons is important, not least for cemented implants. Revision risk for hybrid THR was higher in Denmark and Finland than in Sweden, probably reflecting cementing technique and implant choice considerations. Revision risk for reverse hybrid THR was higher in Finland than in Sweden, perhaps due to different implant selection.
Revision risk for uncemented THR was lower in Sweden than in Finland. This difference was also observed when Denmark was compared to Sweden, but only for the first years after the operation. With increasing follow–up, the survival of uncemented THRs improved in Denmark relative to Sweden and during the sixth, seventh, and ninth year of follow-up it became higher in Denmark. Revision risk was low in Denmark, especially in male patients less than 60 years of age. Implant choices and differences in bearing surface options may explain the relatively high degree of implant survival in Denmark. The use of highly crosslinked polyethylene liners may protect against liner wear and osteolysis. Unfortunately, complete bearing surface data are not available in the NARA dataset. In subgroup analyses of cemented and uncemented THR in female and male patients aged < 60 and ≥ 60 years, the revision risk in Finland was significantly higher than that in Sweden in every category.
In time-trend analyses, the 10-year survival of both cemented and uncemented THRs was higher for the time period 2000–2005 than for the time period 1995–1999 in all countries. We believe that the publication of registry studies pointing out inferior implants and cements has played an important role in this development. The 5-year survival of cemented or uncemented THRs, however, was not higher for the time period 2006–2011 than for the time period 2000–2005 in any of the countries. It is worrisome that although the overall survival of THRs in Nordic countries is high, the short-term survival of the most recent implants is no better, or it has become even worse than that of implants inserted in 2000–2005. The poor short-term results for the most recent uncemented THRs in Finland and Norway may be due to changes in the implant choices and the use of uncemented implants in older patients. These data were unadjusted, and the increased use of uncemented implants in elderly patients may perhaps explain our findings. However, the overall adjusted revision rate for uncemented THR was also higher in a relatively recent study based on the Norwegian Arthroplasty Register data from the most recent study period (2003–2007) than in 1998–2002 (Fevang et al. Citation2010). Furthermore, elderly patients with uncemented implants may have more infections (Dale et al. Citation2012).
Thoretically, the threshold for reporting revisions may vary between countries, which would obviously influence survival results. There may also be differences in revision indications between countries. The operative volume of individual surgeons is not known and may bias the results. Uncemented large-diameter head metal-on-metal THR has been used mainly in Denmark and Finland, not in Norway and rarely in Sweden. The results with most large-diameter head metal-on-metal implants have been poor, due to the relatively high incidence of adverse reactions to metal debris (Ollivere et al. Citation2009, AOA 2010, Johanson et al. 2010, Langton et al. Citation2010, NJR Citation2011). It is possible that the revision rate for cementless THR will increase in the future in Denmark and Finland due to revision of large-diameter head metal-on-metal THRs.
Revisions
The proportion of periprosthetic fractures that led to revision was the same in Denmark, Sweden, and Finland (8%). In Norway, the proportion of revisions performed due to periprosthetic fracture was lower (only 4%). The use of cemented implants in Norway may have prevented early periprosthetic fractures. The proportion of periprosthetic fractures that were a reason for revision has increased in Sweden and Denmark—but not in Norway—compared to the previous report, which may be related to the increased use of uncemented implants.
The proportion of revisions due to infection is similar in Sweden, Norway, and Denmark, whereas in Finland it appears to be less frequent. However, NARA data are biased because they only include revision with change of implant parts, such as liner or head, and debridements without any change of liner or head are not included. It has been stated that the low rate of infected knee replacements in the Finnish Arthroplasty Register is an underestimate (Jämsen et al. Citation2009).
Aseptic loosening is the most common reason for revision in all 4 countries. The proportion of revisions for aseptic loosening related to the total numbers was found to be at the same level in Sweden, Norway, and Denmark as it was in the previous report (Havelin et al. Citation2009). The proportion of aseptic loosening is low in Denmark compared to the other countries, including Finland. The proportion of revisions performed for pain only is as low in Sweden as it was previously compared to Norway and Denmark (Havelin et al. Citation2009). Revisions performed for pain only are not recorded in the Finnish registry. The proportion of revisions performed for other reasons is high in Finland. The outdated Finnish data collection form may explain this deficiency.
In Denmark and Norway, the surgical procedure performed at the revision was most often replacement of the cup or liner. In addition to loosening, this may be caused by polyethylene wear of uncemented cups—especially in Denmark, with its long-standing tradition of using uncemented THR. In Sweden, total revisions of both stem and cup were as common as cup revisions only. The proportion of cup or liner revisions has increased in Sweden and Norway compared to the previous report, probably due to the increased amounts of cementless implants (Havelin et al. Citation2009). In Denmark, the proportion of cup and liner revisions has remained the same. The proportion of stem revisions is similar in Denmark, Norway, and Sweden. Most cases recorded as extraction of the prosthesis are probably first-stage revision procedures of 2-stage infection revisions. They might serve as indicators of those deep-infection revisions that are treated in 2 stages as opposed to those treated in 1 stage or with lavage and debridement only. However, this has not been validated. The proportions of all procedures that involved extraction of the prosthesis have decreased in Norway and Sweden by 1 and 3 percentage points, respectively, compared to the previous data (Havelin et al. Citation2009).
Conclusions
The differences in THR survival rates between the 4 Nordic countries studied were considerable. Overall revision risk for THR was less in Sweden than in the other countries. However, revision risk for uncemented THR was less in Denmark than in Sweden for implants with longer follow-up periods corresponding to the sixth, seventh, and ninth year of follow-up. This may reflect differences between implant choices, an issue that requires detailed studies of the specific THR brands used in these 4 Nordic countries.
Supplementary data
Tables 4-8 are available at Acta’s website (www.actaorthop.org), identification number 6792.
Supplementary Material
Download PDF (53.2 KB)This paper is the result of close team work. All the authors participated in the plan¬ning and design of the study and in interpretation of the results. The statisti¬cians MM, PP, JR, and AF performed statistical analy¬ses in collaboration with the orthopedic surgeons and physicians (KM, LH, LE, OF, SO, AP, JK, GG, HM, and AE). KM was responsible for writing the manuscript, and all the authors participated actively in preparation of the manuscript.
No competing interests declared.
- Arthursson AJ, Furnes O, Espehaug B, Havelin LI, Söreide JA. Validation of data in the Norwegian Arthroplasty Register the Norwegian Patient Register: 5,134 primary total hip arthroplasties and revisions operated at a single hospital between. 1987 and 2003. Acta Orthop 2005; 76: 823-8.
- Australian Orthopaedic Association. National Joint Replacement Registry. Annual Report 2010.
- Dale H, Fenstad AM, Hallan G, Havelin LI, Furnes O, Overgaard S, et al. Increasing risk of prosthetic joint infection after total hip Arthroplasty. 2,778 revisions due to infection after 432,168 primary THAs in the Nordic Arthroplasty Register Association (NARA). Acta Orthop 2012; 83: 449-58.
- Danish Hip Arthroplasty Register (DHAR). Annual Report 2011. http://www.dhr.dk/
- Espehaug B, Furnes O, Havelin LI, Engesaeter LB, Vollset SE, Kindseth O. Registration completeness in the Norwegian Arthroplasty Register. Acta Orthop 2006; 77: 49-56.
- Fevang B TS, Lie SA, Havelin LI, Engesaeter LB, Furnes O. Improved results of primary total hip replacement. Results from the Norwegian Arthroplasty Register, 1987-2007. Acta Orthop 2010; 81 (6): 649-59.
- Gjertsen JE, Engesaeter LO, Havelin LI, Steindal K, Vinje T, Fevang JM. The Norwegian Hip Fracture Register: Experiences after the first 2 years and 15,576 reported operations. Acta Orthop 2008; 79 (5): 583-93.
- Havelin LI, Engesaeter LB, Espehaug B, Furnes O, Lie SA, Vollset SE. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand 2000; 71 (4): 337-53.
- Havelin LI, Fenstad AM, Salomonsson R, Mehnert F, Furnes O, Overgaard S, Pedersen AB, Herberts P, Kärrholm J, Garellick G. The Nordic Arthroplasty Register Association. A unique collaboration between 3 national hip arthroplasty registries with 280,201 THRs. Acta Orthop 2009; 80 (4): 393-401.
- Hekmat K, Jacobsson L, Nilsson JÅ, Petersson IF, Robertsson O, Garellick G, Turesson C. Decrease in the incidence of total hip arthroplasties in patients with rheumatoid arthritis–results from a well defined population in south Sweden. Arthritis Res Ther 2011; 13(2): R67.
- Johanson PE, Fenstad AM, Furnes O, Garellick G, Havelin LI, Overgaard S, Pedersen AB, Kärrholm J. Inferior outcome after hip resurfacing arthroplasty than after conventional arthroplasty. Evidence from the Nordic Arthroplasty Register Association (NARA) database, 1995 to 2007. Acta Orthop 2010; 81(5): 535-41.
- Jämsen E, Huotari K, Huhtala H, Nevalainen J, Konttinen YT. Low rate of infected knee replacements in a nationwide series – is it an underestimate? Review of the Finnish Arthroplasty Register on 38,676 operations performed in 1997 through 2003. Acta Orthop 2009; 80 (2): 205-12.
- Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: A consequence of excess wear. J Bone Joint Surg (Br) 2010; 92 (1): 38-46.
- Lindalen E, Havelin LI, Nordsletten L, Dybvik E, Fenstad AM, Hallan G, Furnes O, Hovik O, Röhrl SM. Is reverse hybrid hip replacement the solution? Acta Orthop 2011; 82 (6): 639-45.
- Lohmander LS, Engesaeter LB, Herberts P. Ingvarsson T, Lucht U, Puolakka TJ. Standardized incidence rates of total hip replacement for primary hip osteoarthritis in the 5 Nordic countries: similarities and differences. Acta Orthop 2006; 77 (5): 733-40.
- Lucht U. The Danish Hip Arthroplasty Register. Acta Orthop Scand 2000; 71 (5): 433-9.
- Malchau H, Herberts P, Eisler T, Garellick G, Söderman P. The Swedish total hip replacement register. J Bone Joint Surg (Am) (Suppl 2) 2002; 84: 2-20.
- National Joint Registry for England and Wales (NJR England-Wales). 9th Annual Report 2011.
- Ollivere B, Darrah C, Barker T, Nolan J, Porteous MJ. Early clinical failure of the Birmingham metal-on-metal hip resurfacing is associated with metallosis and soft-tissue necrosis. J Bone Joint Surg (Br) 2009; 91: 1025-30.
- Paavolainen P, Hämälainen M, Mustonen H, Slatis P. Registration of arthroplasties in Finland. A nationwide prospective project. Acta Orthop Scand (Suppl 241) 1991; 62: 27–30.
- Peltola M , National Institute for Health and Welfare. Unpublished data.
- Puolakka TJ, Pajamäki KJ, Halonen PJ, Pulkkinen PO, Paavolainen P, Nevalainen JK. The Finnish Arthroplasty Register: report of the hip register. Acta Orthop Scand 2001; 72 (5): 433-41.
- Ranstam J, Kärrholm J, Pulkkinen P, Mäkelä K, Espehaug B, Pedersen AB, Mehnert F, Furnes O; NARA study group. Statistical analysis of arthroplasty data. II. Guidelines. Acta Orthop 2011; 82 (3): 258-67.
- Swedish Hip Arthroplasty Register (SHAR). The Annual Report 2011. http://www.shpr.se/