Abstract
Background and purpose — Distraction osteogenesis (DO) has been used to gain height in short statured individuals. However, there have been no studies comparing the clinical outcome of limb lengthening based on the etiology of the short stature. We assessed whether different underlying diagnoses are associated with varied clinical outcomes in these patients.
Methods — We performed a systematic review of the literature pertaining to lower limb lengthening using external fixation for short stature. Clinical outcomes including amount of lengthening, healing index (HI), and complications based on the underlying diagnosis for the short stature were documented.
Results — 18 clinical studies were included, with 547 patients who underwent 1,581 lower limb segment lengthening procedures. Mean follow-up was 4.3 years. The average age at lengthening was less for individuals with achondroplasia/hypochondroplasia (A/H) (14.5 years) than for those with Turner’s syndrome (TS) (18.2 years) or with constitutional short stature (CSS) (21.7 years). Mean height gained was greater in patients with A/H (9.5 cm) than in those with TS (7.7 cm) or CSS (6.1 cm) group. The HI was better in A/H (30.8 days/cm) and CSS (32 days/cm) than in TS (45.1 days/cm). The reported complication rate per segment was lower for A/H (0.68) and TS (0.71) than for CSS (1.06).
Interpretation — Patients with A/H tolerated larger amounts of lengthening with fewer complications than those with other diagnoses.
Distraction osteogenesis (DO) uses a corticotomy or osteotomy to allow formation of new bone in the gap created by controlled distraction of the bone segments. In 1905, Codivilla proposed limb lengthening through distraction (Codivilla Citation2008), and this concept was reintroduced in 1969 by Ilizarov (Ilizarov and Deviatov Citation1969) and in 1977 by Wagner (Citation1977) using external fixation (EF). Since then, DO has been used to address non-unions, skeletal defects, and limb deformities, including limb length discrepancy (Aronson Citation1997, Liu et al. Citation2011).
More recently, this surgical modality has been used to increase standing height in individuals of short stature (Koczewski et al. Citation2002). Although there are several challenges associated with DO such as length of treatment, the psychological consequences of treatment, and permanent complications, with advances in DO—including the availability of newer implants and techniques—more individuals with a variety of underlying diagnoses will undergo limb lengthening. However, to our knowledge, there have been no large comparative studies on the clinical outcome of lower limb lengthening for short stature based on the underlying diagnosis.
We performed a systematic review of the literature on lower limb lengthening and assessed whether there were any differences in the reported clinical parameters, such as lengthening percentage (LP) and healing index (HI), based on the etiology of short stature. From previous literature (Paley Citation1988), we hypothesized that patients with achondroplasia and hypochondroplasia would have undergone greater degrees of lengthening with fewer reported complications than those with other diagnoses for their short stature.
Patients and methods
Search strategy and criteria
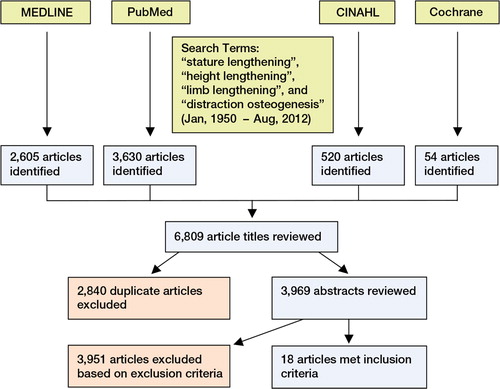
On October 18, 2012, we searched PubMed, MEDLINE, the Cumulative Index to Nursing and Allied Health (CINAHL), and the Cochrane Library for articles published between 1950 and 2012. The search terms used were “stature lengthening”, “height lengthening”, “limb lengthening”, and “distraction osteogenesis”. After discarding all duplicate articles and restricting the search to manuscripts available in the English language and pertaining to human subjects, 2 of us (SJK, WP) reviewed each remaining abstract manually. The search was further narrowed to include only those articles that focused on bilateral lower limb lengthening for short stature using EF only and that included the patient’s underlying diagnosis and limb segment(s) (femur/tibia) that were lengthened (Figure). An orthopedic surgeon (SJK) and an orthopedic resident (WP) independently assessed the eligibility of all relevant studies based on our inclusion criteria. Disagreements between the reviewers were resolved by discussion. The inclusion criteria included (1) full-length articles published from January 1, 1950 to August 18, 2012, (2) articles written in the English language about human subjects, (3) cases of lengthening using EF only, and (4) articles that documented complications. The exclusion criteria included (1) cases of lengthening over nail (LON), (2) review articles focusing on the technique of lengthening, (3) articles without clinical outcomes such as LP and HI, and (4) evaluation of any segment other than the lower limb (for example, lengthening of the humerus). In order to minimize bias related to the technique of DO, we excluded patients who had undergone lengthening involving intramedullary (IM) nails, with or without EF. Limits regarding the number of patients in each study or the minimum duration of follow-up were not used. All study designs of levels I–IV were included. Bibliographies of the studies included were also searched to identify other relevant studies. Based on the above search criteria, 18 clinical studies were available for the final analysis ().
Table 1. The number of patients from each study and the number of total segments included in outcome analysis
Data extraction
Relevant information such as level of evidence, patient demographics, limb segment lengthened, preoperative height, device(s) used for limb lengthening, amount of lengthening, LP (final regenerate length divided by initial bone length, multiplied by 100) (Givon et al. Citation2001), HI (number of days to union divided by the final regenerate length in cm) (Kim et al. Citation2011), any reported complications, and mean follow-up period were extracted from each of these studies. Clinical outcome measures varied among the studies.
The patient’s underlying diagnosis was categorized under one of the following categories: achondroplasia/hypochondroplasia (A/H), Turner’s syndrome (TS), and constitutional short stature (CSS). The patients with body dysmorphism/normal height were excluded because most of them underwent LON. Achondroplasia and hypochondroplasia were integrated in 1 group because it is often difficult to clearly discriminate achondroplasia patients from hypochondroplasia patients clinically, and patients with these 2 diagnoses are reported together in most reports (Ng et al. Citation2003). If there was a chance that the same patients (patients who were reported in 2 or more studies and treated by the same surgeon over a similar operation period) had been included more than once in the present study, only the patients in the study with a larger cohort were included for data extraction and statistical analysis in order to minimize any potential for sampling bias.
It was difficult to use a uniform classification of complications due to reporting inconsistencies. The study by Paley (Citation1990) was cited by several research groups (Vaidya et al. Citation2006, Park et al. Citation2008, Kim et al. Citation2012c), but then not used to evaluate the patients noted in their articles. We therefore evaluated the total numbers (sum) of complications (problems, obstacles, and sequelae) (Eralp et al. Citation2010, Kim et al Citation2011) and complication rate per segment. It was also challenging to divide complications into problems and obstacles, as these were not consistently reported. Thus, we documented only numbers of sequelae (permanent complications) defined as all problems during lengthening that were not resolved by the end of treatment (Eralp et al. Citation2010, Kim et al Citation2011).
Statistics
We analyzed data using SPSS software. The chi-square test was used to evaluate differences in the complication rates and sequelae between groups. Any p-value of < 0.05 was regarded as significant. It was not possible to conduct a meta-analysis due to the heterogeneity of the reports. An I2 value of 75% was indicated according to the test statistic for evaluation of heterogeneity (Higgins et al. Citation2003).
Results
18 level-IV studies met our inclusion criteria, yielding data on 547 subjects who underwent 1,581 lower limb segment lengthening procedures. No level-I or -II studies were identified in our search. While the underlying diagnoses, limb segments lengthened, and devices used for lengthening were available for all subjects, other variables such as patient age, sex, preoperative height, and length gained were not found on a consistent basis for all studies. 7 of the 18 studies dealt with tibial lengthening only (Cattaneo et al. Citation1988, Noonan et al. Citation1997, McAllister et al. Citation1999, Hahn et al. Citation2003, Catagni et al. Citation2005, Vaidya et al. Citation2006, Park et al. Citation2008), 2 studies (Venkatesh et al. Citation2009, Kim et al. Citation2012a) dealt with femoral lengthening alone, and the remaining 9 studies included patients undergoing combined tibial and femoral lengthening procedures. The average age of the patients at surgery was 16.3 (4–47) years and the mean follow-up time was 4.3 (0.8–16) years. Two-thirds of the patients (367/547) had underlying diagnoses of A/H and underwent the first lengthening procedure between 4 and 35 years of age ().
Table 2. Demographics of patients undergoing limb lengthening for short stature
Based on the information available, the average age at lengthening was less for individuals with A/H (14.5 years) than for those with TS (18.2 years) or CSS (21.7 years). The mean gain in height was greater in patients with A/H (9.5 cm) than in patients with TS (7.7 cm) or CSS (6.1 cm). The HI ranged from 24 to 67 days/cm. It was also better in patients with A/H (31 days/cm) and CSS (32 days/cm) than in those with TS (45 days/cm) ().
Table 3. Amount of lengthening and healing index
As noted previously, most studies reported untoward events and complications inconsistently. 805 “complications” were reported for 1,057 segments, with 0.76 complications reported per lengthened segment (). In 2 studies (Cattaneo et al. Citation1988, Aldegheri and Dall’Oca Citation2001), the distribution of complications among the patients was reported but the sum of complications was not reported. The complication rate per segment lengthened was lower for A/H (0.68) than for TS (0.71) or CSS (1.06) (p < 0.001). Sequelae were seldom reported, yet occurred in 19 segments, 5 segments, and 4 segments, respectively, with pooled percentages of 1.7% (19/1,111 segments), 2.1% (5/234 segments), and 1.7% (4/236 segments) (). The rate of sequelae was similar between groups.
Table 4. Reported complications for limb lengthening
Table 5. Reported sequelae of limb lengthening
Discussion
While many authors have reported on limb lengthening for increasing standing height (Park et al. Citation2008, Kim et al Citation2009, Citation2012b, Lie and Chow Citation2009), there is limited information on whether there are any differences in outcome based on the patient’s underlying etiology.
Despite the challenges with heterogeneity of the patients, lack of a consistent method of assessment, and reporting of patient-centered outcomes, we were able to gather some clinically relevant information regarding lower limb lengthening for stature by pooling the extracted data from the existing literature. Lower limb lengthening for increasing stature was reported most often (67%) for patients with A/H (Kim et al. Citation2012b). These patients also appeared to undergo the greatest amount of lengthening, to heal faster, and to have fewer reported complications than individuals with other diagnoses undergoing stature lengthening. Stature lengthening in patients with TS is more challenging due to the numerous possible medical conditions including cardiovascular, renal, and endocrine abnormalities and also learning disabilities (Gravholt Citation2004); thus, the indications for limb lengthening may be more limited. While patients with CSS are generally healthy, due to normal muscle to bone length ratio, these individuals can be more predisposed to development of soft tissue contractures following limb lengthening (Schoenau et al. Citation2004). It has been suggested that patients with achondroplasia tolerate lengthening very well because of their ligament and soft tissue laxity, and their muscle length exceeds bone length before lengthening (Paley Citation1988). Lengthening of more than 30% was often reported in A/H patients (Aldegheri et al. Citation1988, McAllister et al. Citation1999, Venkatesh et al. Citation2009, Devmurari et al. Citation2010). In the pooled analysis, the mean gain in height (10cm) and LP (36%) was greater in patients with A/H than in patients with other diagnoses. The HI was also better in patients with A/H and CSS than in those with TS.
Complications arising from DO can be severe, with long-term residuals. Recently, in a separate study that was not included in our analysis (due to lack of documented complications), over half of skeletally immature patients with achondroplasia who underwent DO for stature lengthening had substantial growth inhibition and premature physeal closure of the lengthened femurs and tibias (Song et al. Citation2012). Increasing the magnitude of lengthening is also associated with other complications such as adjacent joint stiffness and fractures (Venkatesh et al. Citation2009). Various authors have explored the complications of extensive limb lengthening and attempted to assess patient satisfaction (Lavini et al. Citation1990, Aldegheri and Dall’Oca Citation2001). It has been suggested that individuals with achondroplasia who have undergone lower limb lengthening without any sequelae generally have a better quality of life and higher self-esteem than those with one or more sequelae (Kim et al. Citation2012c). In the present study, we noted that patients with A/H underwent a larger amount of limb lengthening with fewer reported complications than those with other diagnoses. We found the highest frequency of complications (1 per segment) in patients with CSS. The lower rate of complications in patients with A/H may result from the shortening of treatment time associated with more robust new bone formation at the distraction gap. However, we were unable to find any relationship between the etiology of short stature and sequelae, perhaps because of a limited number of patients with sequelae in published material. Furthermore, there is a distinct possibility of under-reporting of such untoward events related to the retrospective study design and lack of long-term follow-up.
The use of IM implants for DO is gaining popularity (Park et al. Citation2008). It is quite likely that while the newer techniques of lengthening may minimize or avoid the annoyance of having an overlying external fixator, there may be some device-related issues (Guichet et al. Citation2003) that would need further study before one can recommend one technique over the other. We excluded cases involving IM devices for lengthening in order to reduce the number of variables related to the device used.
We noted several limitations in the existing literature on limb lengthening, which led to our inability to draw firm conclusions. Firstly, this is a pooled analysis of a several level IV evidence studies with a heterogeneous cohort of patients. Consequently, not all the data that we wanted to include in our analysis was consistently available in the studies chosen. Certain variables, such as patient age and sex, length of follow-up, preoperative or postoperative height, LP, and HI were not specified or were not presented in sufficient detail to allow meaningful statistical inferences and comparisons. Secondly, clinical outcomes including functional scores, quality of life, and untoward events were not reported using a validated clinical assessment tool across the majority of the studies. While we did try to reclassify these “complications” in separate categories, given the paucity of comparable data, we could not evaluate the complications using a uniform classification system. Instead, we investigated the rate of complications in each study as we believe that there is less variability in the definition of this term. Thirdly, the younger mean age of patients with A/H (14.5) compared to the average age of remaining patients (19.9) could also have contributed to the better HI and longer lengthening in this subgroup of short-stature individuals. In addition, TS was a female-only group and patients with CSS underwent mostly tibial lengthening. The use of retrospective studies for the pooled analysis makes it difficult to confirm the direct association of the underlying etiology of short stature with healing potential and clinical outcome after stature lengthening.
In conclusion, we found that patients with A/H healed faster with a lower complication rate compared to other groups of individuals undergoing lower limb lengthening using EF. However, the length of follow-up in most available studies was short, with no uniformity in reporting of patient-centered clinical outcomes. As the technology for DO advances, the feasibility of performing limb lengthening using innovative techniques and implants will probably improve. Based on our literature review, limb lengthening for short stature needs further risk-versus-benefit analysis using a more robust study design and a consistent method of reporting patient-centered outcomes with long-term follow-up.
SJK: literature review, implementation, and manuscript preparation and editing. WP: data analysis, literature review, and preparation and editing of manuscript. SS: study design, implementation, and manuscript preparation and editing.
No competing interests declared.
- Aldegheri R. Distraction osteogenesis for lengthening of the tibia in patients who have limb length discrepancy or short stature. J Bone Joint Surg (Am) 1999; 81: 624-34.
- Aldegheri R, Dall’Oca C. Limb lengthening in short stature patients. J Pediatr Orthop B 2001; 10 (3): 238-47.
- Aldegheri R, Trivella G, Renzi-Brivio L, Tessari G, Agostini S, Lavini F. Lengthening of the lower limbs in achondroplastic patients. A comparative study of four techniques. J Bone Joint Surg (Br) 1988; 70 (1): 69-73.
- Aronson J. Limb-lengthening, skeletal reconstruction, and bone transport with the Ilizarov method. J Bone Joint Surg (Am) 1997; 79 (8): 1243-58.
- Bidwell JP, Bennet GC, Bell MJ, Witherow PJ. Leg lengthening for short stature in Turner’s syndrome. J Bone Joint Surg (Br) 2000; 82 (8): 1174-6.
- Catagni MA, Lovisetti L, Guerreschi F, Combi A, Ottaviani G. Cosmetic bilateral leg lengthening: experience of 54 cases. J Bone Joint Surg (Br) 2005; 87 (10): 1402-5.
- Cattaneo R, Villa A, Catagni M, Tentori L. Limb lengthening in achondroplasia by Ilizarov’s method. Int Orthop 1988; 12 (3): 173-9.
- Codivilla A. The classic: On the means of lengthening, in the lower limbs, the muscles and tissues which are shortened through deformity. 1905. Clin Orthop 2008; (466) (12): 2903-9.
- Devmurari KN, Song HR, Modi HN, Venkatesh KP, Ju KS, Song SH. Callus features of regenerate fracture cases in femoral lengthening in achondroplasia. Skeletal Radiol 2010; 39 (9): 897-903.
- Eralp L, Kocaoglu M, Bilen FE, Balci HI, Toker B, Ahmad K. A review of problems, obstacles and sequelae encountered during femoral lengthening: uniplanar versus circular external fixator. Acta Orthop Belg 2010; 76 (5): 628-35.
- Givon U, Schindler A, Ganel A. Hemichondrodiastasis for the treatment of genu varum deformity associated with bone dysplasias. J Pediatr Orthop 2001; 21 (2): 238-41.
- Gravholt CH. Epidemiological, endocrine and metabolic features in Turner syndrome. Eur J Endocrinol 2004; 151 (6): 657-87.
- Guichet J, Deromedis B, Donnan LT, Peretti G, Lascombes P, Bado F. Gradual femoral lengthening with the albizzia intramedullary nail. J Bone Joint Surg (Am) 2003; 85: 838-48.
- Hahn SB, Park HW, Park HJ, Seo YJ, Kim HW. Lower limb lengthening in Turner dwarfism. Yonsei Med J 2003; 44 (3): 502-7.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003; 327 (7414):5 57-60.
- Ilizarov GA, Deviatov AA. Surgical lengthening of the shin with simultaneous correction of deformities. Ortop Travmatol Protez 1969; 30 (3): 32-7.
- Kim H, Lee SK, Kim KJ, Ahn JH, Choy WS, Kim YI, et al. Tibial lengthening using a reamed type intramedullary nail and an Ilizarov external fixator. Int Orthop 2009; 33 (3): 835-41.
- Kim SJ, Cielo B, Song SH, Song HR, Song SY. Gradual bilateral genu varum correction in skeletal dysplasia using the Ilizarov method. J Orthop Sci 2011; 16 (4): 405-12.
- Kim SJ, Agashe MV, Song SH, Choi HJ, Lee H, Song HR. Comparison between upper and lower limb lengthening in patients with achondroplasia: a retrospective study. J Bone Joint Surg (Br) 2012a; 94 (1): 128-33.
- Kim SJ, Agashe MV, Song SH, Song HR. Fibula-related complications during bilateral tibial lengthening: 60 patients followed for mean 5 years. Acta Orthop 2012b; 83 (3): 271-5.
- Kim SJ, Balce GC, Agashe MV, Song SH, Song HR. Is bilateral lower limb lengthening appropriate for achondroplasia?: midterm analysis of the complications and quality of life. Clin Orthop 2012c; (470) (2): 616-21.
- Kitoh H, Kitakoji T, Tsuchiya H, Katoh M, Ishiguro N. Distraction osteogenesis of the lower extremity in patients with achondroplasia/hypochondroplasia treated with transplantation of culture-expanded bone marrow cells and platelet-rich plasma. J Pediatr Orthop 2007; 27 (6): 629-34.
- Koczewski P, Shadi M, Napiontek M. The surgical treatment of short stature: management strategy and local experience. Ortop Traumatol Rehabil 2002; 4 (4): 421-6.
- Lavini F, Renzi-Brivio L, de Bastiani G. Psychologic, vascular, and physiologic aspects of lower limb lengthening in achondroplastics. Clin Orthop 1990; (250): 138-42.
- Lie CW, Chow W. Limb lengthening in short-stature patients using monolateral and circular external fixators. Hong Kong Med J 2009; 15 (4): 280-4.
- Liu T, Zhang X, Li Z, Peng D. Management of combined bone defect and limb-length discrepancy after tibial chronic osteomyelitis. Orthopedics 2011; 34 (8): 363-7.
- McAllister DR, Parker RD, Cooper AE, Recht MP, Abate J. Outcomes of postoperative septic arthritis after anterior cruciate ligament reconstruction. Am J Sports Med 1999; 27 (5): 562-70.
- Ng B KW, Hung V WY, Cheng J CY, Lam TP. Limb lengthening for short stature: A 10-year clinical experience. Hong Kong J Paediatr 2003; 8: 307-17.
- Noonan KJ, Leyes M, Forriol F. Limb lengthening in Turner syndrome. Iowa Orthop J 1997; 17: 96-101.
- Noonan KJ, Leyes M, Forriol F, Canadell J. Distraction osteogenesis of the lower extremity with use of monolateral external fixation. A study of two hundred and sixty-one femora and tibiae. J Bone Joint Surg (Am) 1998; 80 (6): 793-806.
- Paley D. Current techniques of limb lengthening. J Pediatr Orthop 1988; 8 (1): 73-92.
- Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop 1990; (250): 81-104.
- Park HW, Yang KH, Lee KS, Joo SY, Kwak YH, Kim HW. Tibial lengthening over an intramedullary nail with use of the Ilizarov external fixator for idiopathic short stature. J Bone Joint Surg (Am) 2008; 90 (9): 1970-8.
- Schoenau E, Land C, Stabrey A, Remer T, Kroke A. The bone mass concept: problems in short stature. Eur J Endocrinol (Suppl 1) 2004; 151: S87-91.
- Song SH, Kim SE, Agashe MV, Lee H, Refai MA, Park YE, et al. Growth disturbance after lengthening of the lower limb and quantitative assessment of physeal closure in skeletally immature patients with achondroplasia. J Bone Joint Surg (Br) 2012; 94 (4): 556-63.
- Vaidya SV, Song HR, Lee SH, Suh SW, Keny SM, Telang SS. Bifocal tibial corrective osteotomy with lengthening in achondroplasia: an analysis of results and complications. J Pediatr Orthop 2006; 26 (6): 788-93.
- Venkatesh KP, Modi HN, Devmurari K, Yoon JY, Anupama BR, Song HR. Femoral lengthening in achondroplasia: magnitude of lengthening in relation to patterns of callus, stiffness of adjacent joints and fracture. J Bone Joint Surg (Br) 2009; 91 (12): 1612-7.
- Wagner H. Operative correction of leg length discrepancy. Langenbecks Arch Chir 1977; 345: 147-54.