Abstract
Background and purpose — Obesity is a risk factor for osteoarthritis in the lower limb, yet the cardiovascular risks associated with obesity in hip or knee replacement surgery are unknown. We examined associations between body mass index (BMI) and the risk of a major adverse cardiovascular event (MACE: ischemic stroke, acute myocardial infarction, or cardiovascular death) or the risk of all-cause mortality in a nationwide Danish cohort of patients who underwent primary hip or knee replacement surgery.
Methods — Using Danish nationwide registries, we identified 34,744 patients aged ≥ 20 years who underwent elective primary hip or knee replacement surgery between 2005 and 2011. We used multivariable Cox regression models to calculate the 30-day risks of MACE and mortality associated with 5 BMI groups (underweight (BMI < 18.5 kg/m2), normal weight (18.5–24 kg/m2), overweight (25–29 kg/m2), obese 1 (30–34 kg/m2), and obese 2 (≥ 35 kg/m2)).
Results — In total, 232 patients (0.7%) had a MACE and 111 (0.3%) died. Compared with overweight, adjusted hazard ratios (HRs) were 1.2 (95% CI: 0.4–3.3), 1.3 (0.95–1.8), 1.6 (1.1–2.2), and 1.0 (0.6–1.9) for underweight, normal weight, obese 1, and obese 2 regarding MACE. Regarding mortality, the corresponding HRs were 7.0 (2.8–15), 2.0 (1.2–3.2), 1.5 (0.9–2.7), and 1.9 (0.9–4.2). Cubic splines suggested a significant U-shaped relationship between BMI and risks with nadir around 27–28.
Interpretation — In an unselected cohort of patients undergoing elective primary hip or knee replacement surgery, U-shaped risks of perioperative MACE and mortality were found in relation to BMI. Patients within the extreme ranges of BMI may warrant further attention.
Obesity is one of the most prominent risk factors for the development and progression of osteoarthritis in the lower limb, especially in the knee (Felson et al. Citation1988, Sturmer et al. Citation2000). As a result, overweight people are overrepresented among patients undergoing joint replacement surgery (Bostman Citation1994, Cooper et al. Citation1998, Karlson et al. Citation2003, Jain et al. Citation2005). With an increasing proportion of elderly people and the high prevalence of overweight/obesity in the general population, the demand for joint replacement surgery is expected to rise (Kurtz et al. Citation2007). Considerable risks of peroperative and postoperative complications have been reported for obese patients undergoing hip or knee replacement surgery (Winiarsky et al. Citation1998, Foran et al. Citation2004a, Schwarzkopf et al. Citation2012), although with conflicting results (Pritchett and Bortel Citation1991, Griffin et al. Citation1998, Hawker et al. Citation1998, Winiarsky et al. Citation1998, Spicer et al. Citation2001, Foran et al. Citation2004a, Citationb, Flegal et al. Citation2005, Davis et al. Citation2011). The majority of previous studies have focused on orthopedic-related outcomes, e.g. risks of infection and prosthesis dislocation (Smith et al. Citation1992, Griffin et al. Citation1998, Deshmukh et al. Citation2002, Amin et al. Citation2006, Hamoui et al. Citation2006). Major surgical procedures, including joint replacement surgery, also carry a significant risk of adverse cardiovascular events and mortality. Previous research has suggested that obesity may increase perioperative cardiovascular and mortality risks, but it has not concentrated specifically on elective hip and knee replacement surgery (Bamgbade et al. Citation2007). We therefore evaluated the relationship between body mass index (BMI) and perioperative cardiovascular events and mortality, as well as 1-year mortality, in patients undergoing elective total hip or knee replacement in a nationwide setting. We hypothesized that obese patients would have higher risk of adverse cardiovascular events than patients who were not obese.
Methods
In Denmark (with 5.5 million citizens), medical care is tax-financed, free of charge to private individuals, and available to all. For administrative purposes, the government has kept records on several healthcare-related variables, which were used for the present study.
From the Danish National Patient Register and the Danish Anesthesia Register, we identified patients who had undergone elective primary hip and knee replacement surgery between 2005 and 2011. Data on admission dates, operation dates, discharge dates, and diagnoses were available in these registers. Diagnoses were coded according to the international classification system (ICD tenth revision: ICD-10) and surgical procedures were coded according to a national classification system for surgeries (NOMESKO NCPS). When defining comorbidities, we considered validated in-hospital discharge codes up to 5 years before surgery (Thygesen et al. Citation2011). However, to minimize the risk of confounding, discharge codes from in-hospital stays and also outpatient clinics at any point prior to surgery (back until 1994 when the ICD-10 system was introduced) were considered for rheumatoid arthritis (ICD-10 codes M05–06), as these patients were excluded from analysis.
Information on vital status, date of birth, and sex was collected from the National Population Register and information on causes of deaths was obtained from the National Causes of Death Register. Information on smoking, alcohol consumption, American Society of Anesthesiology (ASA) risk score, and BMI was retrieved from the Danish Anesthesia Register. BMI was calculated from self-reported and/or measured weight and height registered for all patients before surgery. Patients were classified according to the definitions of the World Health Organization (WHO), as underweight (BMI < 18.5 kg/m2), normal weight (18.5–24 kg/m2), overweight (25–29 kg/m2), obese 1 (30–34 kg/m2), or obese 2 (≥ 35 kg/m2).
Pharmacological treatment prior to surgery was identified from the Danish Register of Medicinal Product Statistics, where all prescriptions claimed have been registered since 1995. In accordance with previous work (Schramm et al. Citation2008, Andersson et al. Citation2012), diabetes was defined by a claimed prescription being registered for glucose-lowering medication in the 120 days before the index date. Treatment with vitamin K antagonists, aspirin, clopidogrel, beta-blockers, calcium channel blockers, angiotensin-converting enzyme/angiotensin II (ACE) inhibitors, and aldosterone blockers was defined by the same method and using the same time window (120 days) (Andersson et al. Citation2014). Severity of heart failure was estimated using loop diuretic dosages, as described previously (Andersson et al. Citation2010).
Study population
We identified all patients aged ≥ 20 years who had undergone elective primary hip or knee replacement (NOMESKO NCPS codes KNGB20–40 (knee) or KNFB20–40 (hip)) between 2005 and 2011. We discriminated between cemented prostheses (KNGB30–40, KNFB30–40) and uncemented prostheses (KNGB20, KNFB20). To create as homogenous a population as possible, we excluded patients with rheumatoid arthritis (ICD-10 codes M05–06) or a hip/knee fracture within 30 days prior to surgery (ICD-10 code DS72 (hip surgery) and DS82 (knee surgery)). In total 34,744 patients were included, almost half of whom received a total knee replacement (45%). Altogether, 1.0% of patients were classified as underweight, 28% as normal weight, 40% as overweight, 21% as obese 1, and 10% as obese 2 ().
Table 1. Baseline characteristics
Outcome measures
The main outcome measures were 30-day risk of MACE (non-fatal acute myocardial infarction (ICD-10 code I21), non-fatal ischemic stroke (ICD-10 code I63–64; I64 refers to unspecified stroke, but previous data have demonstrated that the majority of these strokes are of ischemic type) (Krarup et al. Citation2007) or cardiovascular mortality (ICD-10 codes I00–I99)), and all-cause mortality. Secondary endpoints were 1-year risk of all-cause mortality and cardiovascular mortality.
Ethics
The study was approved by the Danish Data Protection Agency. In Denmark, retrospective registry-based studies do not need ethical approval.
Statistics
We calculated hazard ratios with 95% confidence intervals (CIs) by multivariable Cox-proportional regression analyses in 4 steps to assess the relationship between BMI and risk of MACE and that between BMI and risk of mortality. In the first step, age, sex, and type of surgery (hip or knee replacement surgery) were included as covariates. In the second step, heart failure, previous myocardial infarction, chronic ischemic heart disease, atrial fibrillation, peripheral artery disease, cerebrovascular disease, chronic obstructive pulmonary disease, and renal disease were added to the model. The third model was as for the second, but it was additionally adjusted for diabetes. The fourth model was as for the third, but it was additionally adjusted for cemented vs. non-cemented prosthesis. Decision to include these variables was based on guidance from directed acyclic graphs (Shrier and Platt Citation2008). The overweight group was used as the reference for all analyses (quantitatively, this group was the largest).
Unless otherwise indicated, models assumptions were tested and fulfilled (proportional hazard assumption was tested with log(-log(survival)) vs. log(time) plots; linearity of continuous variables assumption was tested by inclusion of an additional categorical variable; and no interactions assumption was tested by inclusion of an interaction term in the overall model). Dose-response graphs (adjusted for age, sex, and hip or knee replacement surgery) were created using restricted cubic spline functions by the SAS macro developed by Desquillbet and Mariotti (Citation2010). Knots were placed at p25, p50, and p75 for 30-day outcome measures and at p10, p25, p50, p75, and p90 for one-year outcome measures. Test for non-linearity was done with the chi-square test. There were complete data on all variables included in the analyses. A 2-sided p-value of < 0.05 was considered significant for all statistical tests. All statistical analyses were performed with SAS version 9.2.
Results
232 patients (0.7%) experienced a MACE within 30 days after surgery. During the same period, 111 patients (0.3%) died—74 of them (0.2%) from cardiovascular causes. The 1-year mortality figure was 582 (1.7%); 265 of these deaths (0.8%) were from cardiovascular causes. Adverse events were more common in underweight patients than in the other groups ().
Table 2. Crude numbers of events and adjusted hazard ratios associated with different BMI groups for the individual endpoints
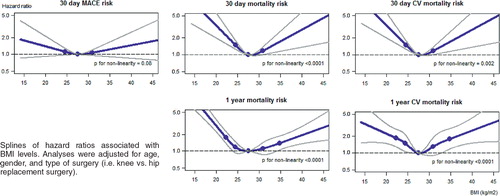
Age, sex, and hip vs. knee replacement-adjusted splines are presented in the Figure. As can be seen, there appeared to be a U-shaped relationship between BMI and the risk of 30-day mortality (overall and CV mortality) as well as 1-year mortality risks (p-value for non-linearity < 0.001 for all endpoints) and a suggestion of a U-shaped relationship for 30-day MACE (p-value for non-linearity = 0.08). As can be seen in the graphs, the nadir BMI was found for overweight patients (BMI around 27–28). Similar associations were found for analyses using the discrete BMI groups (). Compared to overweight, the hazard ratios regarding MACE from the final adjusted model were 1.2 (95% CI: 0.4–3.3), 1.3 (0.95–1.8), 1.6 (1.1–2.2), and 1.0 (0.6–1.9) for underweight, normal weight, obese 1, and obese 2. The 30-day hazard ratios regarding mortality were 7.0 (2.8–15), 2.0 (1.2–3.2), 1.5 (0.9–2.7), and 1.9 (0.9–4.2) for underweight, normal weight, obese 1, and obese 2, compared to overweight.
Splines of hazard ratios associated with BMI levels. Analyses were adjusted for age, gender, and type of surgery (i.e. knee vs. hip replacement surgery).
Of the other variables included in the final model, high age, cardiovascular diseases, renal disease, and diabetes tended to increase risks (). It is notable that hip replacement was not associated with higher hazard ratios for 30-day risk of mortality or MACE, compared to knee replacement. The association between BMI category and outcomes was also not statistically significantly different for hip and for knee replacement surgery (p-values for interactions between BMI groups and hip or knee replacement surgery were 0.28, 0.47, 0.66, 0.055, and 0.14 for 30-day mortality, 30-day CV mortality, 30-day MACE, 1-year mortality, and 1-year CV mortality, respectively).
Table 3. Hazard ratios associated with other variables from multivariable Cox regression models
Sensitivity analyses
To ensure that the increased mortality risk associated with being underweight was not driven by the high prevalence of chronic obstructive pulmonary disease, a sensitivity analysis excluding these patients was performed. This yielded similar results: hazard ratio 3.53 (1.36–9.12) for 30-day mortality, 0.76 (0.19–3.11) for 30-day MACE, 1.15 (0.15–8.63) for 30-day CV mortality, 2.75 (1.77–4.25) for 1-year mortality, and 1.50 (0.65–3.45) for 1-year CV mortality associated with underweight, compared with overweight.
Discussion
Our main finding was that there appeared to be a U-shaped relationship between the risks of MACE and mortality, with the lowest risk being seen in overweight patients (nadir BMI 27–28). Although the underweight group had rather few patients, this group was associated with the absolutely greatest mortality risk, which may warrant further attention. This was not in agreement with our main hypothesis, but it may be explained by factors such as increased comorbidity burden in this group of patients. We hypothesized that obese patients were doing worse than patients who were not obese. Indeed, analysis of BMI groups showed a tendency of increased risks associated with being obese or very obese, compared to being overweight. In analyses based on cubic spline regressions, very obese patients (with BMI exceeding 35) had an increased risk of MACE and mortality, both in the short term (30 days) and in the long term (1 year). A cubic spline analysis uses BMI as a continuous variable and is therefore more powerful than the conventional categorization of BMI into 5 categories (Greenland Citation1995). The finding that the lowest risks were associated with being overweight is interesting and is in agreement with results from a recent meta-analysis based on 2.9 million individuals (in a non-surgical setting), which showed a similar U-shaped relationship between BMI and mortality, with the lowest risks associated with being overweight (Flegal et al. Citation2013). This might seem contradictory, given that maintenance of a low/normal weight leads to improvement in several cardiovascular risk factors. However, nowadays in modern western societies, the “normal” state is often to be overweight. People who are underweight or even of normal weight may therefore be different in several ways, including having a more sedentary lifestyle with low muscle mass, or suffering from chronic comorbidities such as depression, pulmonary disease, or cardiovascular diseases with low-grade inflammation, which increases cardiovascular and mortality risks (Lavie et al. Citation2009). Moreover, dementia for example is known to have a long preclinical phase with significant weight loss up to a decade before overt disease (Knopman et al. Citation2007). All these considerations may have affected our estimates as well. As seen from , underweight or normal-weight patients were older and had more comorbidity than overweight or obese patients. Although we adjusted the analyses for many of these characteristics, it may be that the increased risks found for these weight groups were in part caused by comorbidity burden and high age. Despite the fact that obese patients were younger and had less comorbidity than normal-weight or overweight patients, they still had higher risks. Thus, it seems unlikely that all of our results were caused by a high comorbidity burden.
It is well known that the risk of orthopedic-related complications such as poor wound healing, chronic deep infection, dislocation of the implant, and periprosthetic fractures are increased in overweight and obese patients, but substantially less data are available on cardiovascular and mortality risks associated with obesity (Smith et al. Citation1992, Griffin et al. Citation1998, Deshmukh et al. Citation2002, Amin et al. Citation2006, Hamoui et al. Citation2006). Ghandi et al. (Citation2006) evaluated the risk of myocardial infarction in a cohort of 3,471 patients undergoing elective hip and knee replacement surgery at a tertiary-care orthopedic center in Canada between 1998 and 2003. The authors reported that 1.8% suffered from perioperative myocardial infarction and showed that high BMI was a risk factor for perioperative myocardial infarction. Other studies have, however, reported substantially lower mortality and lower rates of adverse cardiovascular events in patients undergoing hip or knee replacement surgery. Using a large database of total knee replacement operations (n = 15,943) from Kaiser Permanente (Southern Califormia, USA), Khatod et al. (Citation2008) reported a 90-day mortality rate of 0.3% and an acute myocardial infarction rate of 0.1% in individuals undergoing primary replacement surgery. Mantilla et al. (Citation2002) reported that in a cohort of 10,244 American patients undergoing elective primary hip or knee replacement surgery, 0.4% suffered from a perioperative myocardial infraction and 0.5% died. Other studies have found perioperative mortality and myocardial infraction rates ranging from 0.2% to 0.7%, which is more or less comparable to our findings (Parvizi et al. Citation2001, Lie et al. Citation2002, Ibrahim et al. Citation2005, Blom et al. Citation2006, Pulido et al. Citation2008).
Despite the rather low overall event rates (0.7% MACE and 0.3% mortality during the first 30 days after surgery), we can, however, conclude that there is a U-shaped relationship between BMI and the risks of MACE and mortality—with the lowest risks being carried by overweight patients. Increased attention and thorough preoperative evaluation is therefore warranted for patients at the extremes of the BMI spectrum. In addition, several comorbidities such as diabetes, vascular diseases, atrial fibrillation, and kidney disease are often present in obese people, which—as also supported by our data ()—is associated with increased risk of perioperative MACE and mortality.
Strengths and limitations
The main strength of our study was the large and representative population. The national registries we used have good specificity and positive predictive values for the diagnoses myocardial infarction and ischemic stroke (Johnsen et al. Citation2002, Madsen et al. Citation2003). However, as measurement of troponins and electrocardiograms were not performed routinely postoperatively, some non-fatal acute myocardial infarctions may have been missed (Devereaux et al. Citation2011). The mortality associated with postoperative myocardial infarctions that are missed is, however, high and would therefore be reflected in the mortality analyses to some extent (Devereaux et al. Citation2011). The numbers of events were rather small for most groups, and statistical type-2 error (i.e. failure to reject a false null hypothesis) can therefore not be excluded. Furthermore, we did not have exact indications for surgery; and although used in research previously, the validity of the Danish Anesthesia Register is unknown. BMI in particular was not obtained in a standardized way and may even have been based on self-reported weight and height measurements in some cases.
In summary, in an unselected cohort of patients who underwent elective primary hip or knee replacement surgery, there appeared to be U-shaped risks of perioperative MACE and mortality in relation to BMI. Notably, underweight and extreme obesity may help to identify patients who are at higher risk and who therefore warrant more attention.
CT wrote the initial draft of the paper. CA performed all the analyses and takes responsibility for the accuracy of the analyses and the integration of data. CT, CA, GHG, and CTP came up with the idea and contributed equally to the study design. All the authors contributed with important intellectual input to interpretation of the data and to the discussion.
None of the authors report any competing interests. GHG was supported by an independent research scholarship from the Novo Nordisk Foundation and CA was supported by an independent research grant from the Danish Agency for Science, Technology, and Innovation (the Danish Medical Research Council, grant no. FSS-11-120873). The sources of funding had no influence on the study design or on interpretation of data.
- Amin AK, Patton JT, Cook RE, Brenkel IJ. Does obesity influence the clinical outcome at five years following total knee replacement for osteoarthritis? J Bone Joint Surg (Br) 2006; 88 (3): 335-40.
- Andersson C, Norgaard ML, Hansen PR, Fosbol EL, Schmiegelow M, Weeke P, et al. Heart failure severity, as determined by loop diuretic dosages, predicts the risk of developing diabetes after myocardial infarction: a nationwide cohort study. Eur J Heart Fail 2010; 12 (12): 1333-8.
- Andersson C, Lyngbaek S, Nguyen CD, Nielsen M, Gislason GH, Kober L, et al. Association of clopidogrel treatment with risk of mortality and cardiovascular events following myocardial infarction in patients with and without diabetes. JAMA 2012; 308 (9): 882-9.
- Andersson C, Merie C, Jorgensen M, Gislason GH, Torp-Pedersen C, Overgaard C, et al. Association of beta-blocker therapy with eisks of adverse cardiovascular events and deaths in patients with ischemic heart disease undergoing noncardiac surgery: A Danish nationwide cohort study. JAMA internal medicine 2014; 174 (3): 336-44.
- Bamgbade OA, Rutter TW, Nafiu OO, Dorje P. Postoperative complications in obese and nonobese patients. World J Surg 2007; 31 (3): 556-60.
- Blom A, Pattison G, Whitehouse S, Taylor A, Bannister G. Early death following primary total hip arthroplasty: 1,727 procedures with mechanical thrombo-prophylaxis. Acta Orthop 2006; 77 (3): 347-50.
- Bostman OM. Prevalence of obesity among patients admitted for elective orthopaedic surgery. Int J Obes Relat Metab Disord 1994; 18 (10): 709-13.
- Cooper C, Inskip H, Croft P, Campbell L, Smith G, McLaren M, et al. Individual risk factors for hip osteoarthritis: obesity, hip injury, and physical activity. Am J Epidemiol 1998; 147 (6): 516-22.
- Davis AM, Wood AM, Keenan AC, Brenkel IJ, Ballantyne JA. Does body mass index affect clinical outcome post-operatively and at five years after primary unilateral total hip replacement performed for osteoarthritis? A multivariate analysis of prospective data. J Bone Joint Surg (Br) 2011; 93 (9): 1178-82.
- Deshmukh RG, Hayes JH, Pinder IM. Does body weight influence outcome after total knee arthroplasty? A 1-year analysis. J Arthroplasty 2002; 17 (3): 315-9.
- Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med 2010; 29 (9): 1037-57.
- Devereaux PJ, Xavier D, Pogue J, Guyatt G, Sigamani A, Garutti I, et al. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Ann Intern Med 2011; 154 (8): 523-8.
- Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med 1988; 109 (1): 18-24.
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005; 293 (15): 1861-7.
- Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 2013; 309 (1): 71-82.
- Foran JR, Mont MA, Rajadhyaksha AD, Jones LC, Etienne G, Hungerford DS. Total knee arthroplasty in obese patients: a comparison with a matched control group. J Arthroplasty 2004a; 19 (7): 817-24.
- Foran JR, Mont MA, Etienne G, Jones LC, Hungerford DS. The outcome of total knee arthroplasty in obese patients. J Bone Joint Surg (Am) 2004b; 86 (8): 1609-15.
- Gandhi R, Petruccelli D, Devereaux PJ, Adili A, Hubmann M, de Beer J. Incidence and timing of myocardial infarction after total joint arthroplasty. J Arthroplasty 2006; 21 (6): 874-7.
- Greenland S. Dose-response and trend analysis in epidemiology: alternatives to categorical analysis. Epidemiology 1995; 6 (4): 356-65.
- Griffin FM, Scuderi GR, Insall JN, Colizza W. Total knee arthroplasty in patients who were obese with 10 years followup. Clin Orthop 1998; (356): 28-33.
- Hamoui N, Kantor S, Vince K, Crookes PF. Long-term outcome of total knee replacement: does obesity matter? Obes Surg 2006; 16 (1): 35-8.
- Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, et al. Health-related quality of life after knee replacement. J Bone Joint Surg (Am) 1998; 80 (2): 163-73.
- Ibrahim SA, Stone RA, Han X, Cohen P, Fine MJ, Henderson WG, et al. Racial/ethnic differences in surgical outcomes in veterans following knee or hip arthroplasty. Arthritis Rheum 2005; 52 (10): 3143-51.
- Jain NB, Guller U, Pietrobon R, Bond TK, Higgins LD. Comorbidities increase complication rates in patients having arthroplasty. Clin Orthop 2005; (435): 232-8.
- Johnsen SP, Overvad K, Sorensen HT, Tjonneland A, Husted SE. Predictive value of stroke and transient ischemic attack discharge diagnoses in The Danish National Registry of Patients. J Clin Epidemiol 2002; 55 (6): 602-7.
- Karlson EW, Mandl LA, Aweh GN, Sangha O, Liang MH, Grodstein F. Total hip replacement due to osteoarthritis: the importance of age, obesity, and other modifiable risk factors. Am J Med 2003; 114 (2): 93-8.
- Khatod M, Inacio M, Paxton EW, Bini SA, Namba RS, Burchette RJ, et al. Knee replacement: epidemiology, outcomes, and trends in Southern California: 17,080 replacements from 1995. Acta Orthop 2008; 79 (6): 812-9.
- Knopman DS, Edland SD, Cha RH, Petersen RC, Rocca WA. Incident dementia in women is preceded by weight loss by at least a decade. Neurology 2007; 69 (8): 739-46.
- Krarup LH, Boysen G, Janjua H, Prescott E, Truelsen T. Validity of stroke diagnoses in a national register of patients. Neuroepidemiology 2007; 28 (3): 150-4.
- Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005. J Bone Joint Surg (Am) 2007; 89 (4): 780-5.
- Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol 2009; 53 (21): 1925-32.
- Lie SA, Engesaeter LB, Havelin LI, Furnes O, Vollset SE. Early postoperative mortality after 67,548 total hip replacements: causes of death and thromboprophylaxis in 68 hospitals in Norway from 1987. Acta Orthop 2002; 73 (4): 392-9.
- Madsen M, Davidsen M, Rasmussen S, Abildstrom SZ, Osler M. The validity of the diagnosis of acute myocardial infarction in routine statistics: a comparison of mortality and hospital discharge data with the Danish MONICA registry. J Clin Epidemiol 2003; 56 (2): 124-30.
- Mantilla CB, Horlocker TT, Schroeder DR, Berry DJ, Brown DL. Frequency of myocardial infarction, pulmonary embolism, deep venous thrombosis, and death following primary hip or knee arthroplasty. Anesthesiology 2002; 96 (5): 1140-6.
- Parvizi J, Johnson BG, Rowland C, Ereth MH, Lewallen DG. Thirty-day mortality after elective total hip arthroplasty. J Bone Joint Surg (Am) 2001; 83 (10): 1524-8.
- Pritchett JW, Bortel DT. Knee replacement in morbidly obese women. Surg Gynecol Obstet 1991; 173 (2): 119-22.
- Pulido L, Parvizi J, Macgibeny M, Sharkey PF, Purtill JJ, Rothman RH, et al. In hospital complications after total joint arthroplasty. J Arthroplasty (Suppl 1) 2008; 23(6): 39-45.
- Schramm TK, Gislason GH, Kober L, Rasmussen S, Rasmussen JN, Abildstrom SZ, et al. Diabetes patients requiring glucose-lowering therapy and nondiabetics with a prior myocardial infarction carry the same cardiovascular risk: a population study of 3.3 million people. Circulatio 2008; 117 (15): 1945-54.
- Schwarzkopf R, Thompson SL, Adwar SJ, Liublinska V, Slover JD. Postoperative complication rates in the “super-obese” hip and knee arthroplasty population. J Arthroplasty 2012; 27 (3): 397-401.
- Shrier I, Platt RW. Reducing bias through directed acyclic graphs. BMC Med Res Methodol 2008; 8: 70.
- Smith BE, Askew MJ, Gradisar IA Jr., Gradisar JS, Lew MM. The effect of patient weight on the functional outcome of total knee arthroplasty. Clin Orthop 1992; (276): 237-44.
- Spicer DD, Pomeroy DL, Badenhausen WE, Schaper LA Jr., Curry JI, Suthers KE, et al. Body mass index as a predictor of outcome in total knee replacement. Int Orthop 2001; 25 (4): 246-9.
- Sturmer T, Gunther KP, Brenner H. Obesity, overweight and patterns of osteoarthritis: the Ulm Osteoarthritis Study. J Clin Epidemiol 2000; 53 (3): 307-13.
- Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sorensen HT. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol 2011; 11: 83.
- Winiarsky R, Barth P, Lotke P. Total knee arthroplasty in morbidly obese patients. J Bone Joint Surg (Am) 1998; 80 (12): 1770-4.

