Abstract
Background and purpose — The frequency and severity of a permanent lesion after brachial plexus birth palsy (BPBP) and its impact on activities of daily living are not well documented. We therefore investigated the outcome of BPBP in adolescents, regarding arm function and consequences for activity and participation.
Participants and methods — Of 30,574 babies born at St. Olavs University Hospital in 1991–2000, 91 had BPBP (prevalence 3 per 1,000), and 69 of these individuals were examined at a median age of 14 (10–20) years. The examination included the modified Mallet classification, range of motion, shoulder rotation and grip strength, Assisting Hand Assessment, and Canadian Occupational Performance Measure. Of the 22 subjects who were not examined, 3 could not be traced and 19 reported having no problems in the affected arm.
Results — At follow-up, 17 adolescents had a permanent lesion (i.e. individual Mallet subscore below 4) with a median Mallet total score of 15 (9–19), while 52 had good or normal shoulder function (median Mallet total score 25 (23–25)). All participants with a permanent lesion had reduced active shoulder rotation (≤ 15°), 16 had elbow extension deficit, and 10 had subnormal grip strength. External rotation was considerably weaker in the affected shoulder. In addition, they had ineffective use of the affected arm in bimanual activities. Even so, all except 1 were independent in activities of daily living, although 15 experienced minor difficulties.
Interpretation — Every fourth to fifth child with BPBP had a permanent lesion as an adolescent. External rotation was the most impaired movement. Despite ineffective use of the affected arm in bimanual activities, all of the participants except one were independent in activities of daily living.
Brachial plexus birth palsy (BPBP) is caused by a traction injury on the brachial plexus during labor (Metaizeau et al. Citation1979). The prevalence of BPBP reported varies by a factor of more than 10, from 0.4 to 5.1 per 1,000 live-born (Evans-Jones et al. Citation2003, Hoeksma et al. Citation2004, Foad et al. Citation2008). In Scandinavian populations, a prevalence of 3 per 1,000 live-born has been reported (Lagerkvist et al. Citation2010, Poyhia et al. Citation2010).
Most children with BPBP have a transient nerve injury, but between 8% and 36% of them will have permanent functional impairments (Michelow et al. Citation1994, Noetzel et al. Citation2001, Hoeksma et al. Citation2004, Poyhia et al. Citation2010). The extent and severity of the nerve injury, varying from transient neurapraxia to avulsion-type root injuries, are the main predictors of recovery. At the time of diagnosis it is not possible to assess the severity of the injury or to predict the long-term outcome (Sunderland Citation1991, Hoeksma et al. Citation2004, Malessy and Pondaag Citation2011). Some babies may spontaneously recover completely, some may recover partially, and some may need reconstructive nerve surgery. The absence of biceps muscle function at 3 months of age indicates a more severe injury and is also a commonly used indicator for surgical plexus exploration (Gilbert and Tassin Citation1984, Waters Citation1999). However, a permanent nerve injury and reduced arm function may also be observed following apparently moderate or less severe injuries.
Individuals with a permanent nerve injury after BPBP have various degrees of functional impairment in their affected extremity. These impairments may be due to reduction in muscle strength as well as limited range of motion caused by soft tissue contractures, muscle co-contractions, and secondary osseous deformities (Hardy Citation1981, Pearl and Edgerton Citation1998, Hoeksma et al. Citation2003, Anguelova et al. Citation2014). Toddlers with incomplete recovery use their affected arm in an asymmetrical way (Lagerkvist et al. Citation2010). Adults with BPBP have reported problems in activities of daily living (Partridge and Edwards Citation2004), but there is limited information regarding when these symptoms occur. Moreover, the frequency and the severity of permanent functional impairment in BPBP are not well documented (Pondaag et al. Citation2004).
We studied the long-term outcome of BPBP in adolescents, regarding arm function and consequences for activity and participation.
Participants and methods
Study design and population
91 adolescents born at St. Olav University Hospital between 1991 and 2000 with a diagnosis of BPBP were eligible to participate in this follow-up study. During 2010 and 2011, 69 of these 91 individuals with median age of 14 (10–20) years came for a detailed examination including measurements of arm length, range of motion, muscle strength, sensibility, how they were able to use the affected arm in bimanual activities, and how they performed functional activities of daily living. Of those who did not participate in the follow-up examination, 1 had moved abroad and 2 did not respond, and 19 declined participation but responded that they had no problems in the involved arm.
Perinatal data on all 91 children, including maternal risk factors, have already been published by Backe et al. (Citation2008), who reported that 86 of the newborns were classified according to Narakas (group 1, n = 44; group 2, n = 33; and group 3, n = 9). In the present study, information on birth weight, associated fractures of the clavicle or humerus, the age when the baby regained antigravity biceps muscle function, and whether he/she had received surgery during infancy was obtained from hospital records.
Exposure variable
Brachial plexus birth palsy was diagnosed according to the International Classification of Diseases (ICD) 9 and ICD 10 by a pediatrician performing the regular examination of newborns within 24 h of birth.
Main outcome measure
The modified Mallet classification (“Mallet score”) (Mallet Citation1972, Waters Citation1997) was used as the main outcome measure. This classification is used to quantify shoulder function and has been tested for reliability in the BPBP population (Bae et al. Citation2003). In the Mallet score, 5 shoulder movements are graded on a scale from 1 (no motion) to 5 (normal motion equal to that in the unaffected side), resulting in a maximum total score of 25. The 5 shoulder movements (i.e. Mallet subscores) include abduction, external rotation, placing the hand behind the neck, placing the hand as high as possible on the spine, and placing the hand to the mouth. A Mallet subscore of 4 or better is considered to be good shoulder function (Tassin Citation1983, Smith et al. Citation2004). Thus, in this study, participants with a Mallet subscore of 4 or better for each separate shoulder movement were defined as having a transient lesion. Participants with a subscore of less than 4 in any separate shoulder movement were defined as having a permanent lesion.
Body structure and function
Arm length was measured as the sum of the lengths of the upper arm and forearm, measured from the tip of the acromion to the olecranon process and from the olecranon process to the ulnar styloid (Bae et al. Citation2008). The elbow was held in 90° flexion.
Active and passive range of motion in the affected arm was measured using a mechanical goniometer. Active shoulder flexion was measured with the arm in the anterior sagittal plane until the person started to compensate by either extending the back or rotating the arm out of the sagittal plane. Active shoulder abduction was measured as a combined glenohumeral and scapulothoracic motion, and active shoulder external rotation was measured with the arm at the side of the body. Passive external shoulder rotation and passive glenohumeral abduction was measured in both shoulders. Passive glenohumeral abduction was measured with the scapula stabilized while the humerus was passively abducted.
Muscle rotation strength in both shoulders was measured with a stationary Biodex 3 Pro dynamometer system (Biodex Medical Systems, Shirley, NY). Measurements were performed in the seated position with 45° of shoulder abduction in the scapular plane; the elbow was supported in 90° flexion and the forearm was in neutral position. This position has been found to show good reliability for assessment of shoulder rotation torque (Edouard et al. Citation2013). Muscle strength was evaluated during 3 isometric maximal voluntary contractions. The highest peak torque value was used as the strength parameter. In addition, isometric grip strength was measured using Grippit (AB Detektor, Gothenburg, Sweden) in the standardized position recommended by the American Society of Hand Therapists for hand-grip dynamometry (Mathiowetz et al. Citation1984). Grippit is a reliable instrument for measuring peak grip strength in children in different age groups (Svensson et al. Citation2008). 3 maximal trials were performed for each hand, and the highest peak value was used as the strength parameter. To eliminate differences due to handedness, grip strength was considered to be subnormal if the difference was more than 10% (Petersen et al. Citation1989). For each of these strength measurements, the difference between the affected limb and the unaffected limb was calculated as percentage of the unaffected limb.
Tactile stereognosis of both hands was examined with shape/texture identification test (STI test), which consists of shapes and stylized textures of various degrees of difficulty, to be identified without the assistance of vision (Rosen and Lundborg Citation1998, Jerosch-Herold Citation2005). The sensibility of both hands was tested with Semmes-Weinstein monofilaments (North Coast Medical, Campbell, CA) using 5 differently sized monofilaments (calibers 2.83, 3.61, 4.31, 4.56, and 6.65) that exert a force ranging from normal perception to deep pressure sensation (Jerosch-Herold Citation2005, Palmgren et al. Citation2007).
Activity and participation
Effective use of the affected arm in bimanual activities was measured with the Assisting Hand Assessment version 4.4 (AHA) (Krumlinde-Sundholm et al. Citation2006). Scores on AHA were converted to a 0–100 unit scale (Krumlinde-Sundholm Citation2012). The School Kids AHA was used for children up to 12 years, whereas the Ad-AHA research version was used for adolescents over 12 years of age. AHA is reliable, and has been validated for children up to 12 years of age (Krumlinde-Sundholm et al. Citation2007).
Performance of functional activities in daily living was investigated using the Norwegian version of the semi-structured interview Canadian Occupational Performance Measure (COPM) (Law and Kjeken Citation2008). The 5 most important self-perceived activity problems in the areas of self-care, productivity (i.e. school), and leisure were selected by each participant and rated on a 10-point scale according to the participant’s perception of, and satisfaction with, current performance. COPM is a valid, reliable, and responsive outcome measure (Kjeken et al. Citation2004, Citation2005).
Statistics
Data are expressed as median values with range. They were analyzed using SPSS version 20.0. Within-group differences were tested using the Wilcoxon signed-rank test, and between-group differences were tested with the Mann-Whitney U-test. Chi-squared test was used to analyze differences in proportions between groups. Statistical significance was set at p ≤ 0.05.
Ethics
The study was approved by the regional medical research ethics committee, Central Norway (ref. 2010/1287-10), and signed informed consent was obtained from the participants or from their parents.
Results
Background data ()
Table 1. Background information on study participants (n = 69)
The median birth weight of the 69 participants was 4,220 (2,850–5,680) g. Other background data are given in . During infancy, antigravity biceps muscle function had been regained within 1 month of birth in 38 babies, including 20 of the 27 babies with a fracture in the clavicle. The only participant who had not regained biceps function within 12 months had had a sural nerve grafting to the brachial plexus at the age of 4 months. He had regained contractions in the biceps muscle 16 months after the operation. During childhood, secondary reconstructive surgery with lengthening of the subscapular muscle was performed in 3 other children at the ages of 3, 7, and 10 years. The 4 participants who were treated with surgery are presented separately in .
Permanent lesion at follow-up ()
Table 2. Modified Mallet classification subscores and total scores (median with range) in participants with transient and permanent lesion after brachial plexus birth palsy
Table 3. Active range of motion in affected shoulder and arm (median with range) in participants with transient and permanent lesion
Table 4. Individual difference in passive range of motion (median with range) between affected and unaffected shoulder in participants with transient and permanent lesion
Table 5. Strength differences (median with range) between affected and unaffected shoulder and hand, for each participant with a transient or permanent lesion. The difference is presented in percentage of the unaffected arm with negative difference if the affected arm was the strongest
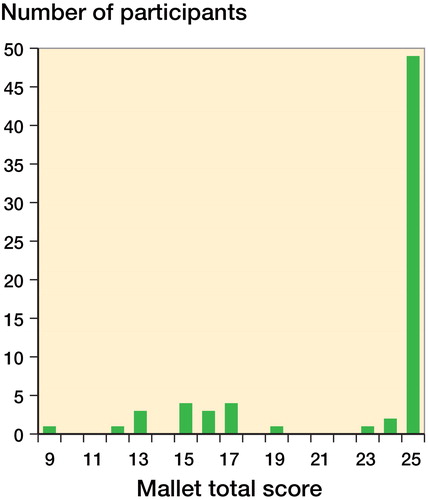
17 of the 69 adolescents had a permanent lesion with a median Mallet total score of 15 (9–19) (). 52 adolescents had a transient lesion, and their median Mallet total score was 25 (23–25) (Figure). Participants with a transient lesion were generally older (median age 15 (11–20) years) than participants with a permanent lesion (median age 12 (10–20) years). The sex distribution was similar between the groups.
Frequency distribution of the modified Mallet classification total score of the 69 participants at follow-up.
Of the 17 adolescents with a permanent lesion, 15 had regained antigravity biceps muscle function later than 3 months of age, whereas this was the case for only 1 of the adolescents with transient lesions.
Body structure and function (Tables , , and )
Of the 17 adolescents with a permanent lesion, the affected arm was shorter than the unaffected arm with a median difference of 2 (–0.5 to 4.0) cm, and 11 of them had a difference in arm length of more than 2 cm. In contrast, none of the participants with a transient lesion had differences in arm length of more than 1 cm, and the median difference between the affected and unaffected arm was 0 (–0.5 to 1.0) cm (p < 0.001).
All shoulder movements on the affected side were reduced in participants with a permanent lesion compared to those with a transient lesion. This was also the case for the adolescents who had undergone surgery as children. Active external shoulder rotation was limited to ≤ 15° for all 17 participants with a permanent lesion, and 9 of them had less than 0°. Furthermore, 16 of the 17 had an active elbow extension deficit (median 20° (0–60)), as compared to only 1 of the 52 with a transient lesion (p < 0.001). 5 participants with a permanent lesion had limitations (< 60°) in active forearm supination and 2 in active forearm pronation. Of those with a transient lesion, none had limitations in active forearm supination or pronation. There was a difference between the affected shoulder and the unaffected shoulder in passive external rotation (median 50°) and in passive glenohumeral abduction (medial 15°) in participants with a permanent lesion.
Strength of shoulder rotation was measured in 15 of the 17 participants with a permanent lesion and in all 52 with a transient lesion. 1 participant refused to perform the strength testing, and the participant with primary surgery could not hold the force transducer. Of those with a permanent lesion, there was a considerable difference in external shoulder rotation strength between the affected and the unaffected arm (median 45%), but internal shoulder rotation strength and grip strength also differed between the sides. The differences in rotation strength between the shoulders were larger for participants who had undergone surgery. Grip strength was measured in 16 participants with a permanent lesion and 9 had subnormal strength in the hand of the affected limb. In addition, the participant who had undergone primary surgery could not hold and compress the Grippit. In the 52 participants with a transient lesion, we found no median difference in strength between the affected arm and the unaffected arm. All differences between participants with transient lesion and participants with permanent lesion and no surgery were statistically significant ( and ).
Tactile sensibility and stereognosis was normal in the affected hand in 14 (82%) of the participants with a permanent lesion. The participant who had had primary surgery had reduced sensibility and stereognosis in the affected hand. He could only feel deep touch (filament 6.65) in parts of his affected hand, and he did not recognize the shapes of any size in the STI test. Another participant had reduced protective sensory function (filament 4.31) in both hands, and 1 participant did not recognize the smallest shapes (5 mm in diameter) in the STI test. All of the 52 participants with a transient lesion had normal tactile sensibility and stereognosis in the affected hand.
Activity and participation
All the participants with a permanent lesion had reduced effective use of the affected arm, as assessed with AHA. There was no significant difference between the adolescents with secondary surgery (median 86 (82–87) logit-based AHA units) and the other adolescents with a permanent lesion and no surgery (median 87 (77–90) logit-based AHA units). Limitations in spontaneous use of the affected arm were found when reaching for objects, moving the upper arm, or when supinating or pronating the forearm. In addition, 1 participant seldom grasped objects from the table with the affected hand. The participant who had had primary surgery did not use the affected hand at all for grasping. In contrast, none of the participants with a transient lesion had reduced effective use of the affected arm (median 100 (100–100) logit-based AHA units).
According to the COPM, 16 participants with a permanent lesion stated that they were independent in age-related activities of daily living. Even so, 15 of the 16 found that some activities were difficult or strenuous to perform. Limitations were related to sport activities (n = 12), in particular performing ball sports, push-ups, and other bimanual activities that required strength. Other activities frequently mentioned were difficulty in washing the armpit on the unaffected side, styling their hair, putting on tight clothes, buttoning up jeans, tying shoelaces, slicing cheese and bread, carrying large or heavy objects using both hands, or writing on the computer for longer periods of time. Changing gear in a car was also reported to be difficult. Some of these problems could be avoided by using alternative strategies and aids. For other activities, the participants could usually manage to do them independently, but performing them was inefficient and compensatory movements were used. The only participant who had major difficulties in daily activities was the participant who had had primary surgery. This individual was not able to grasp with the involved hand, and needed help to shower, dress, and prepare food. All 52 participants with a transient lesion were independent in age-related activities of daily living.
Discussion
The strength of the present study was the long-term follow-up examination of 69 participants, with additional information on 19 participants who did not undergo the examination. Moreover, all the participants included were born at the hospital, which accounted for 85% of the 35,661 births in the county during this time period. Selection bias was therefore unlikely.
The infants were diagnosed with BPBP within 24 h of birth, by a pediatrician performing the regular examination of newborns. In this early examination, it may be difficult to differentiate BPBP from limb inactivity caused by a fracture of the clavicle or the humerus. Thus, there may have been some misclassification of children as having BPBP when in fact they only had a fracture. The proportion of participants with a permanent lesion at follow-up was therefore probably a minimum estimate.
We used the Mallet classification to identify adolescents with a permanent lesion. The results regarding other structural and functional limitations and also the impaired bimanual performance support the division of participants into 2 groups: transient lesion and permanent lesion. The structural and functional examinations of the shoulders and arms, as well as AHA and COPM, were not done blind from the Mallet classification, and some information bias cannot therefore be excluded. However, the considerable differences in arm length and range of motion, and the objective measured differences in strength between participants with a transient lesion and those with a a permanent lesion, suggest that such bias is unlikely to explain the main results. There was a statistically significant difference in median age between the groups. Since muscle strength increases with age in a growing child, we calculated the differences in strength between the affected side and the unaffected side for each participant and assessed whether the differences were greater in participants with a permanent lesion. To our knowledge, ROM does not decrease significantly during adolescence in normal shoulders, and these results are therefore unlikely to be confounded by age, while AHA is age-independent (Krumlinde-Sundholm et al. Citation2007). We are the first to report the outcome in an unselected population of adolescents born with BPBP, and in particular to include measures such as bimanual performance and activities of daily living. The structural and functional impairments observed were considerable, and they also had consequences for bimanual hand performance and activities of daily living, even though these impairments were not of the same magnitude.
Our finding that up to one-quarter of the adolescents had a permanent lesion is consistent with previous studies on toddlers. Lagerkvist (Citation2010) examined 98 children at 18 months of age and reported that almost one-fifth had a permanent lesion, even though they used a different definition of permanent lesion. Poyhia et al. (Citation2010) examined 132 children at 12 months of age, and reported that one-fifth had a permanent lesion. However, Poyhia et al. excluded children with birth fracture of the clavicle without sufficient findings to support BPBP at 1 month of age. If we had excluded children with fracture of the clavicle or humerus, the proportion of adolescents with a permanent lesion would have been substantially higher. Permanent lesions have also been studied in pre-school age children, and these studies found higher proportions of children with permanent lesions. Hoeksma et al. (Citation2004) studied 56 children at a mean age of 3 years and 10 months and found incomplete neurological recovery in one-third, which is slightly higher than in our study. This may partly be explained by a more strict definition of recovery, and probably also by a more severely affected population, since 8 of the children in their study had primary nerve surgery. CitationStrömbeck et al. (2000) reported outcome in 247 referred children with BPBP, and only 27% had recovered completely at 5 years. However, this probably included children with more severe BPBP since 28% of the participants had needed primary nerve surgery, compared to only one patient in the present study. In contrast to these studies, Michelow et al. (Citation1994) used a much milder definition of good recovery, adapting the classification of Narakas (Citation1985), and in their study only one-tenth of the participants had poor recovery. Overall, our results and the results of previous studies in toddlers and children suggest that permanent lesions of BPBP are common—and in addition, we now report that they persist into adolescence.
Recovery of biceps muscle function before 3 months predicted outcome fairly well, which is consistent with previous studies (Gilbert and Tassin Citation1984, Waters Citation1999, Smith et al. Citation2004). However, functional recovery of other muscles has also been proposed to improve prognostic accuracy of outcome (Michelow et al. Citation1994, Hoeksma et al. Citation2004).
The affected arm of participants with a permanent lesion was shorter than the unaffected arm. This is consistent with other studies (McDaid et al. Citation2002, Bae et al. Citation2008).
Active and passive external shoulder rotation in the affected arm was limited in almost all participants with a permanent lesion. These findings are in accordance with the work of Kirjavainen et al. (Citation2011), who reported that lack of active external rotation was the most common shoulder impairment following BPBP. Our findings are also consistent with the findings reported by Hoeksma et al. (Citation2003) who compared passive motion of the affected shoulder and the contralateral shoulder in children with a mean age of 3.5 years. They found that the most seriously affected shoulder motion was external rotation. Finally, our results are consistent with another study by Hoeksma et al. (Citation2004), where they found that external rotation and supination were the most affected directions of motion. Thus, despite differences in study populations regarding severity of BPBP and age, our study and those of others consistently suggest that limitations in external shoulder rotation are typical findings of permanent lesions of BPBP.
Elbow extension was limited in nine-tenths of those with a permanent lesion in our study, which is similar to results reported by Strömbeck et al. (Citation2007a), but slightly higher than the 77% reported by Kirjavainen et al. (Citation2011)—who, however, studied children who had undergone surgery.
In participants with a permanent lesion, both with and without surgery, the strength of external and internal shoulder rotation and grip was reduced compared to the unaffected arm. Strength in external shoulder rotation was most reduced. This is in accordance with the findings of Kirjavainen et al. (Citation2011). We found subnormal grip strength in 9 and no grip ability in 1 of 17 participants with a permanent lesion. Our findings on grip strength are partly consistent with the findings of Stömbeck et al. (Citation2007a) and Kirjavainen et al. (Citation2011).
In the present study, only 2 participants with a permanent lesion had reduced sensibility in the involved hand. This finding is in accordance with other studies that found that sensibility is markedly less affected than motor function following BPBP (Anand and Birch Citation2002, Strömbeck et al. Citation2007b).
All participants with a permanent BPBP lesion had limitations in bimanual activities, as measured with AHA. Only 1 had severe limitations, while all had asymmetrical movements of the affected upper extremity. We are not aware of any previous studies that have used AHA to assess bimanual activities in follow-up studies of BPBP. However, our results are partly consistent with the study of Lagerkvist et al. (Citation2010) who found that 18-month-old children with persistent symptoms after BPBP used the injured arm and hand quite well, but mostly in an asymmetrical way. In another study in pre-school children by Hoeksma et al. (Citation2003), the parents of half of the children noticed that their child had asymmetrical appearance.
16 of the 17 participants with a permanent lesion were independent in activities of daily living according to the COPM, although 15 found some activities strenuous to perform. 12 reported concerns related to sports activities, especially activities requiring 2 hands or specific positioning of the arm. This is in line with the study by Strömbeck and Fernell (Citation2003) who found differences in self-esteem for sport and motor activities. In another study, Strömbeck et al. (Citation2007a) found that all adolescents with a permanent lesion following BPBP were independent in activities of daily living, but one-quarter experienced some difficulties and found that some activities were difficult and cumbersome. Hoeksma et al. (Citation2004) asked parents of 53 children with BPBP 6 questions about daily activities. Most children in their study did not have difficulties in activities of daily living. In contrast to these results and the results of the present study, Kirjavainen et al. (Citation2007) found that one-third of adolescents who had primary nerve surgery after BPBP needed help with activities of daily living, which is consistent with the inclusion of children with more severe injuries in their study.
In summary, we found that every fourth to fifth adolescent who had brachial plexus palsy at birth now had a permanent lesion, including substantial impairments in structure and function of the affected arm and shoulder. External shoulder rotation is the movement that is most affected, and asymmetric bimanual use of the arms is common. Although most adolescents with a permanent BPBP lesion are independent in activities of daily living, they need to use compensatory movements to perform activities requiring specific positioning or movement of the affected arm. We suggest that attention should be given to children and adolescents with less severe BPBP injuries, to improve their outcome and minimize their functional limitations.
GH, MB, and AKE initiated and designed the study and collected data. AKE and TV did the statistical analysis. GH wrote the initial draft of the manuscript. All the authors contributed to interpretation of the data and revision of the final manuscript.
This study was funded in part by HiST; the Faculty of Health Education and Social Work, Sør-Trøndelag University College; the Liaison Committee between the Central Norway Regional Health Authority (RHA) and the Norwegian University of Science and Technology (NTNU); St. Olavs University Hospital; and Unimed Innovation AS.
No competing interests declared.
- Anand P, Birch R. Restoration of sensory function and lack of long-term chronic pain syndromes after brachial plexus injury in human neonates. Brain 2002; 125 (Pt 1): 113-22.
- Anguelova GV, Malessy MJ, van Zwet EW, van Dijk JG. Extensive motor axonal misrouting after conservative treatment of obstetric brachial plexus lesions. Dev Med Child Neurol 2014. doi: 10.1111/dmcn.12490. [Epub ahead of print]
- Backe B, Magnussen EB, Johansen OJ, Sellaeg G, Russwurm H. Obstetric brachial plexus palsy: a birth injury not explained by the known risk factors. Acta Obstet Gynecol Scand 2008; 87 (10): 1027-32.
- Bae DS, Waters PM, Zurakowski D. Reliability of three classification systems measuring active motion in brachial plexus birth palsy. J Bone Joint Surg Am 2003; 85-A (9): 1733-8.
- Bae DS, Ferretti M, Waters PM. Upper extremity size differences in brachial plexus birth palsy. Hand (New York. NY) 2008; 3 (4): 297-303.
- Edouard P, Codine P, Samozino P, Bernard PL, Herisson C, Gremeaux V. Reliability of shoulder rotators isokinetic strength imbalance measured using the Biodex dynamometer. J Sci Med Sport 2013; 16 (2): 162-5.
- Evans-Jones G, Kay SP, Weindling AM, Cranny G, Ward A, Bradshaw A, et al. Congenital brachial palsy: incidence, causes, and outcome in the United Kingdom and Republic of Ireland. Arch Dis Child Fetal Neonatal Ed 2003; 88 (3): F185-9.
- Foad SL, Mehlman CT, Ying J. The epidemiology of neonatal brachial plexus palsy in the United States. J Bone Joint Surg Am 2008; 90 (6): 1258-64.
- Gilbert A, Tassin JL. [Surgical repair of the brachial plexus in obstetric paralysis]. Chirurgie 1984; 110 (1): 70-5.
- Hardy AE. Birth injuries of the brachial plexus: incidence and prognosis. J Bone Joint Surg Br 1981; 63-B (1): 98-101.
- Hoeksma AF, Ter Steeg AM, Dijkstra P, Nelissen RG, Beelen A, de Jong BA. Shoulder contracture and osseous deformity in obstetrical brachial plexus injuries. J Bone Joint Surg Am 2003; 85-A (2): 316-22.
- Hoeksma AF, ter Steeg AM, Nelissen RG, van Ouwerkerk WJ, Lankhorst GJ, de Jong BA. Neurological recovery in obstetric brachial plexus injuries: an historical cohort study. Dev Med Child Neurol 2004; 46 (2): 76-83.
- Jerosch-Herold C. Assessment of sensibility after nerve injury and repair: a systematic review of evidence for validity, reliability and responsiveness of tests. J Hand Surg Br 2005; 30 (3): 252-64.
- Kirjavainen M, Remes V, Peltonen J, Kinnunen P, Poyhia T, Telaranta T, et al. Long-term results of surgery for brachial plexus birth palsy. J Bone Joint Surg Am 2007; 89 (1): 18-26.
- Kirjavainen MO, Nietosvaara Y, Rautakorpi SM, Remes VM, Poyhia TH, Helenius IJ, et al. Range of motion and strength after surgery for brachial plexus birth palsy. Acta Orthop 2011; 82 (1): 69-75.
- Kjeken I, Slatkowsky-Christensen B, Kvien TK, Uhlig T. Norwegian version of the Canadian Occupational Performance Measure in patients with hand osteoarthritis: validity, responsiveness, and feasibility. Arthritis Rheum 2004; 51 (5): 709-15.
- Kjeken I, Dagfinrud H, Uhlig T, Mowinckel P, Kvien TK, Finset A. Reliability of the Canadian Occupational Performance Measure in patients with ankylosing spondylitis. J Rheumatol 2005; 32 (8): 1503-9.
- Krumlinde-Sundholm L. Reporting outcomes of the Assisting Hand Assessment: what scale should be used? Dev Med Child Neurol 2012; 54 (9): 807-8.
- Krumlinde-Sundholm L, Holmefur M, Eliasson A-C. Manual: Assisting Hand Assessment (English Research Version 4.3). Karolinska Institutet, Stockholm 2006.
- Krumlinde-Sundholm L, Holmefur M, Kottorp A, Eliasson AC. The Assisting Hand Assessment: current evidence of validity, reliability, and responsiveness to change. Dev Med Child Neurol 2007; 49 (4): 259-64.
- Lagerkvist AL, Johansson U, Johansson A, Bager B, Uvebrant P. Obstetric brachial plexus palsy: a prospective, population-based study of incidence, recovery, and residual impairment at 18 months of age. Dev Med Child Neurol 2010; 52 (6): 529-34.
- Law M, Kjeken I. Canadian occupational performance measure. NRRK, Oslo 2008.
- Malessy MJ, Pondaag W. Nerve surgery for neonatal brachial plexus palsy. J Pediatr Rehabil Med 2011; 4 (2): 141-8.
- Mallet J. Obstetrical paralysis of the brachial plexus. II. Therapeutics. Treatment of sequelae. Must transplants be performed? Rev Chir Orthop Reparatrice Appar Mot 1972; 58: Suppl 1:186.
- Mathiowetz V, Weber K, Volland G, Kashman N. Reliability and validity of grip and pinch strength evaluations. J Hand Surg Am 1984; 9 (2): 222-6.
- McDaid PJ, Kozin SH, Thoder JJ, Porter ST. Upper extremity limb-length discrepancy in brachial plexus palsy. J Pediatr Orthop 2002; 22 (3): 364-6.
- Metaizeau JP, Gayet C, Plenat F. [Brachial plexus birth injuries. An experimental study (author’s transl)]. Chir Pediatr 1979; 20 (3): 159-63.
- Michelow BJ, Clarke HM, Curtis CG, Zuker RM, Seifu Y, Andrews DF. The natural history of obstetrical brachial plexus palsy. Plast Reconstr Surg 1994; 93 (4): 675-80; discussion 81.
- Narakas AO. The treatment of brachial plexus injuries. Int Orthop 1985; 9 (1): 29-36.
- Noetzel MJ, Park TS, Robinson S, Kaufman B. Prospective study of recovery following neonatal brachial plexus injury. J Child Neurol 2001; 16 (7): 488-92.
- Palmgren T, Peltonen J, Linder T, Rautakorpi S, Nietosvaara Y. Sensory evaluation of the hands in children with brachial plexus birth injury. Dev Med Child Neurol 2007; 49 (8): 582-6.
- Partridge C, Edwards S. Obstetric brachial plexus palsy: increasing disability and exacerbation of symptoms with age. Physiother Res Int 2004; 9 (4): 157-63.
- Pearl ML, Edgerton BW. Glenoid deformity secondary to brachial plexus birth palsy. J Bone Joint Surg Am 1998; 80 (5): 659-67.
- Petersen P, Petrick M, Connor H, Conklin D. Grip strength and hand dominance: challenging the 10% rule. Am J Occup Ther 1989; 43 (7): 444-7.
- Pondaag W, Malessy MJ, van Dijk JG, Thomeer RT. Natural history of obstetric brachial plexus palsy: a systematic review. Dev Med Child Neurol 2004; 46 (2): 138-44.
- Poyhia TH, Lamminen AE, Peltonen JI, Kirjavainen MO, Willamo PJ, Nietosvaara Y. Brachial plexus birth injury: US screening for glenohumeral joint instability. Radiology 2010; 254 (1): 253-60.
- Rosen B, Lundborg G. A new tactile gnosis instrument in sensibility testing. J Hand Ther 1998; 11 (4): 251-7.
- Smith NC, Rowan P, Benson LJ, Ezaki M, Carter PR. Neonatal brachial plexus palsy. Outcome of absent biceps function at three months of age. J Bone Joint Surg Am 2004; 86-A (10): 2163-70.
- Strömbeck C, Fernell E. Aspects of activities and participation in daily life related to body structure and function in adolescents with obstetrical brachial plexus palsy: a descriptive follow-up study. Acta Paediatr 2003; 92 (6): 740-6.
- Strombeck C, Krumlinde-Sundholm L, Forssberg H. Functional outcome at 5 years in children with obstetrical brachial plexus palsy with and without microsurgical reconstruction. Dev Med Child Neurol 2000; 42 (3): 148-57.
- Strömbeck C, Krumlinde-Sundholm L, Remahl S, Sejersen T. Long-term follow-up of children with obstetric brachial plexus palsy I: functional aspects. Dev Med Child Neurol 2007a; 49 (3): 198-203.
- Strömbeck C, Remahl S, Krumlinde-Sundholm L, Sejersen T. Long-term follow-up of children with obstetric brachial plexus palsy II: neurophysiological aspects. Dev Med Child Neurol 2007b; 49 (3): 204-9.
- Sunderland S. Traction nerve injury. In: Nerves and nerve injuries (Sunderland S, Ed. Churchill Livingstone, Edinburgh 1991: pp 147-58.
- Svensson E, Waling K, Hager-Ross C. Grip strength in children: test-retest reliability using Grippit. Acta Paediatr 2008; 97 (9): 1226-31.
- Tassin JL. Paralysies obstetricales du plexus brachialis. Evolution spontane, resultats de interventions reparatrices precoces [Thesis]. Universite de Paris, Paris 1983.
- Waters PM. Obstetric brachial plexus injuries: evaluation and management. J Am Acad Orthop Surg 1997; 5 (4): 205-14.
- Waters PM. Comparison of the natural history, the outcome of microsurgical repair, and the outcome of operative reconstruction in brachial plexus birth palsy. J Bone Joint Surg Am 1999; 81 (5): 649-59.

