Abstract
Background and purpose — An increased incidence rate of acromioplasty has been reported; we analyzed data from the Finnish National Hospital Discharge Register.
Patients and methods — During the 14-year study period (1998–2011), 68,877 acromioplasties without rotator cuff repair were performed on subjects aged 18 years or older.
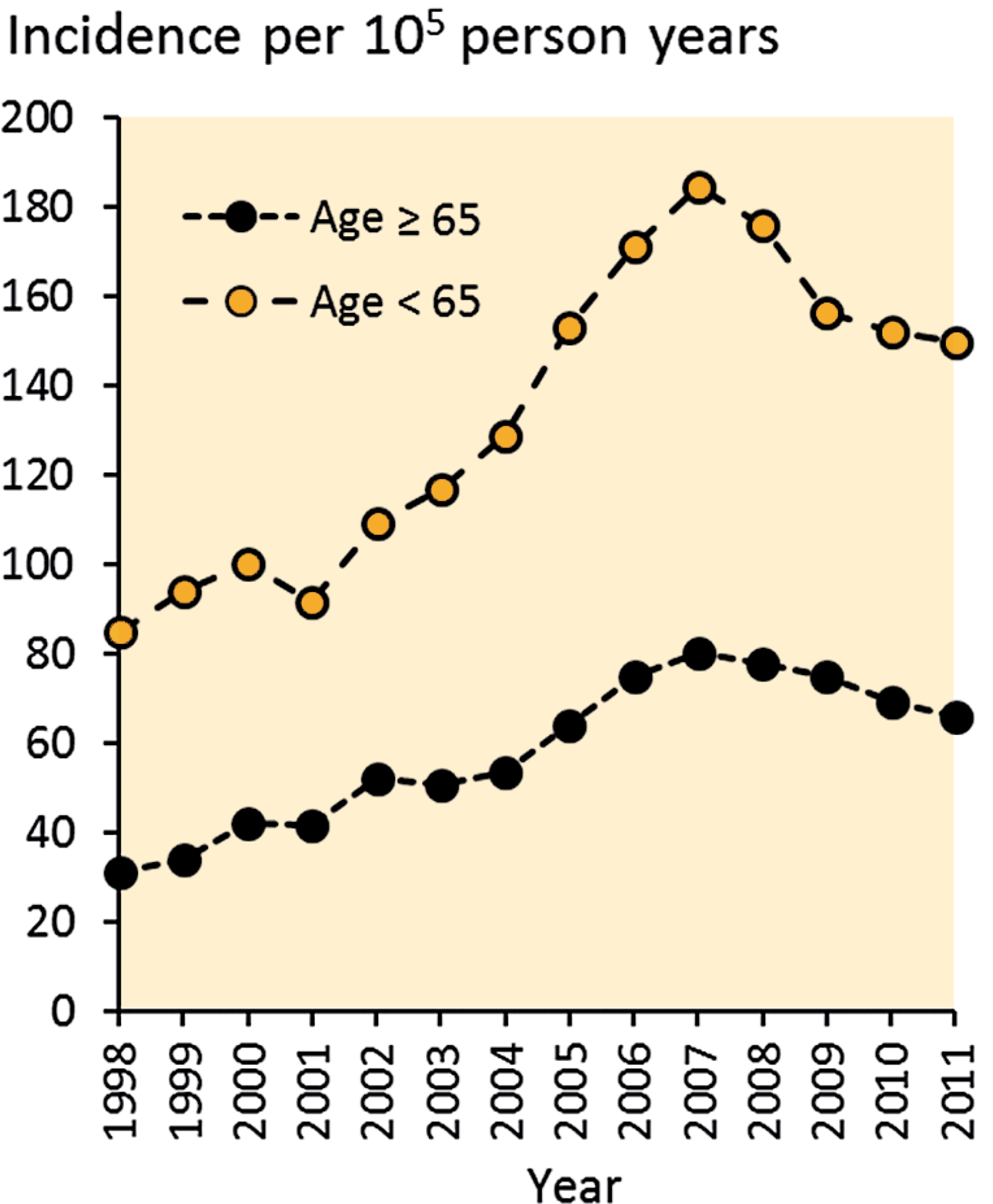
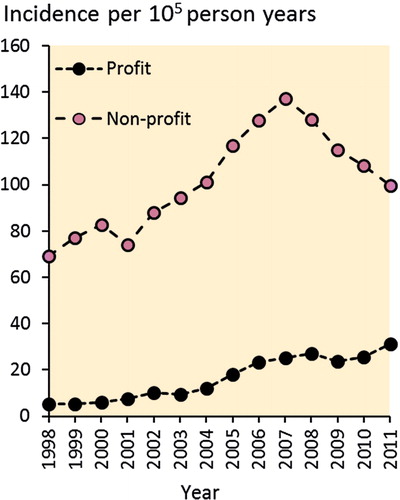
Results — The incidence of acromioplasty increased by 117% from 75 to 163 per 105 person years between 1998 and 2007. The highest incidence was observed in 2007, after which the incidence rate decreased by 20% to 131 per 105 person years in 2011. The incidence declined even more at non-profit public hospitals from 2007 to 2011. In contrast, it continued to rise at profit-based private orthopedic clinics.
Interpretation — We propose that this change in clinical practice is due to accumulating high-quality scientific evidence that shows no difference in outcome between acromioplasty and non-surgical interventions for rotator cuff disease with subacromial impingement syndrome. However, the exact cause of the declining incidence cannot be defined based solely on a registry study. Interestingly, this change was not observed at private clinics, where the number of operations increased steadily from 2007 to 2011.
Shoulder pain is one of the most common musculoskeletal complaints, and rotator cuff disease is considered the leading cause of prolonged shoulder pain and disability (CitationMitchell et al. 2005). The treatment and morbidity of rotator cuff disorders place a substantial economic burden on society (CitationMitchell et al. 2005, CitationOh et al. 2007). Rotator cuff disease is classically considered to be a continuum that ranges from acute inflammation of the tendons to full-thickness rotator cuff tear (CitationNeer 1983). The etiology of rotator cuff disease is multifactorial, and it has been attributed to both extrinsic and intrinsic mechanisms (CitationSeitz et al. 2011).
Acromioplasty, i.e. subacromial decompression procedure, is the most common surgical operation performed on the shoulder. The usual indication for acromioplasty is Neer stage-II rotator cuff disease with subacromial pain or partial tear of the supraspinatus or infraspinatus tendons (CitationChaudhury et al. 2010, CitationPapadonikolakis et al. 2011). The operation is performed by partially removing the anterior-inferior surface of the acromion and the subacromial bursa. The procedure can be performed using either an open approach or an arthroscopic approach, which give similar results in the long term (CitationDavis et al. 2010). The effectiveness of surgical management of stage-II impingement has been questioned recently. 3 high-quality randomized controlled trials (RCTs) compared arthroscopic subacromial decompression to supervised exercises and found no statistically significant or clinically relevant differences between surgical and non-surgical treatment (CitationBrox et al. 1999, CitationHaahr et al. 2005, CitationHaahr and Andersen 2006, CitationKetola et al. 2009, Citation2013). Acromioplasty has also been used in combination with rotator cuff repair to protect the repaired tendon, although recently it was shown that the results of cuff repair are similar without acromioplasty (CitationMilano et al. 2007, CitationMacDonald et al. 2011).
A rapid and continuous increase in the incidence of acromioplasty has been reported in selected patient cohorts (CitationVitale et al. 2010, CitationYu et al. 2010, CitationPapadonikolakis et al. 2011, CitationJudge et al. 2014), but nationwide incidence rates are unknown. Here we conducted a nationwide hospital discharge register-based study in Finland to assess whether the incidence of acromioplasty had changed from January 1998 to December 2011. Our hypothesis was that the overall incidence of acromioplasty is increasing. We also wanted to assess whether the change in incidence rates in public/non-profit hospitals and private/profit-based hospitals are similar.
Patients and methods
Design and setting
We reviewed nationwide data from the Finnish National Hospital Discharge Register (NHDR) for the period 1998–2011. The Finnish National Hospital Discharge Register (NHDR), founded in 1967, is an excellent database for epidemiological studies as it contains data on age, sex, domicile, type of hospital (public or private), length of hospital stay, primary and secondary diagnosis, and operations performed during the hospital stay. Data collection for the Finnish NHDR is mandatory for hospitals, including all public and private institutions. The validity of the NHDR has been found to be good regarding both the coverage and accuracy of data (CitationMattila et al. 2008, CitationSund 2012, CitationHuttunen et al. 2014).
Study population
All inhabitants of Finland aged 18 years or older were included in the study. The operative treatment codes according to the Nomesco Classification of Surgical Procedures were NBG10 (for an open acromioplasty) and NBG15 (for an arthroscopic procedure). Acromioplasties that were associated with either open or arthroscopic rotator cuff repair (procedure code NBL00) were excluded from the analyses due to the secondary nature of acromioplasty compared to rotator cuff repair. During the 14-year study period, 68,877 acromioplasties without concomitant rotator cuff repair were performed on patients aged 18 or older.
Statistics
The primary outcome variable was the incidence of acromioplasty per 105 person years by age, sex, and study year. To compute the incidence rates, the annual population size was obtained from the Official Statistics of Finland, which is a statutory, electronic national population register (CitationStatistics Finland 2014). The incidence was based on the size of the entire population of Finland aged 18 and older rather than on cohort-based estimates. Accordingly, confidence intervals were not calculated. Statistical analyses were performed using SPSS software version 22.0.
Ethics
Ethics approval was granted by the Finnish National Institute of Health and Wellness (Dnr THL/89/5.05.00/2012, dated January 18, 2012).
Results
During the 14-year study period, the mean age of the patients at the time of operation was 52 (SD 10) years. The mean age of men increased from 50 (SD 10) to 53 (SD 11) years, and the mean age of women increased from 51 (SD 9) to 53 (SD 10) years. Over time, there was a consistent shift from open acromioplasty (64% of all acromioplasties in 1998) to arthroscopic procedures (93% in 2011). The mean length of hospital stay was 1.3 (0–32) days.
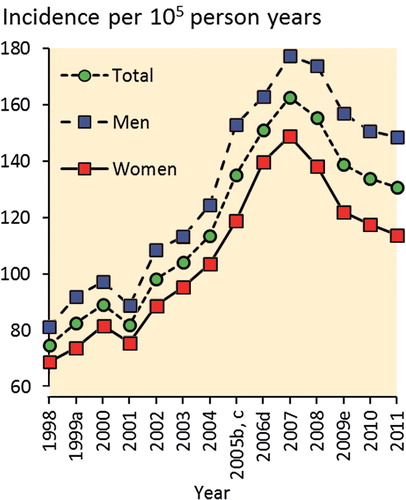
Between 1998 and 2007, the incidence of operations increased from 75 to 163 per 105 person years. After 2007, the incidence started to decline, gradually reaching 131 per 105 person years in 2011 (). The incidence rate in men increased from 81 per 105 person years in 1998 to 177 per 105 person years in 2007, and then declined to 149 per 105 person years in 2011. The corresponding figures for women were 69, 149, and 114, respectively. The male-to-female ratio was 1.2 (). Similar trends were observed in the 18- to 64-year-old population. The change in incidence of acromioplasty was less dramatic in individuals aged 65 or older ().
Figure 1. Incidence rates of acromioplasty in Finland, by year. Randomized controlled trials showing equal outcomes for operative and nonoperative treatment of stage-II impingement syndrome were reported by (a) CitationBrox et al. (1999), (b) CitationHaahr et al. (2005), (c) CitationKetola et al. (2005), (d) CitationHaahr Andersen (2006), and (e) CitationKetola et al. (2009).
The incidence rates of acromioplasty in public, non-profit hospitals peaked in 2007 at 137 per 105 person years and declined steadily thereafter, to 100 per 105 person years by the end of 2011. In contrast, the incidence in profit-based hospitals increased almost linearly from 5 to 31 per 105 person years between 1998 and 2011 (). In the first year of the study (1998), 93% of acromioplasties were performed in public hospitals and 7% were performed in private hospitals; the corresponding percentages in 2011 were 76% and 24%.
Discussion
Our main finding was that the overall incidence of acromioplasty increased steadily and more than doubled between 1998 and 2007. After 2007, there was a 20% decline to 131 per 105 person years in 2011. Notably, changes in the nationwide incidence rates of acromioplasty followed the publication of landmark trials showing that the results of operative and nonoperative treatment of subacromial impingement syndrome are equal. The incidence of acromioplasty started to decline 1–2 years after papers were published by Haahr and co-workers (2005, 2006) and by Ketola and co-workers (2005). The decline continued following publication of a study by CitationKetola et al. in 2009 (). It has been suggested that a combination of scientific, organizational, and behavioral factors drives changes in clinical practice (CitationFerlie et al. 1999). However, there were no organizational or economic factors in Finland during this time period that would explain the entire decline. There is evidence that surgical variation results mainly from differences in physicians’ beliefs about the indications for surgery, and the extent to which patient preferences are incorporated into treatment decisions. A smaller degree of variation in regional surgery rates is caused by differences in illness burden, diagnostic practices, and patient attitudes to medical intervention (CitationBirkmeyer et al. 2013). We therefore propose that orthopedic surgeons are increasingly practicing evidence-based medicine.
Strengths and weaknesses
The strengths of our study are that we used reliable nationwide data and that the study population was the entire adult population of Finland. Because of this coverage of the entire country, including both public and private hospitals, the changes in the incidence of acromioplasty are representative of nationwide clinical practice and trends regarding all actively practicing orthopedic surgeons in Finland. During the study period, there were no changes in diagnostics, in the prevalence of rotator cuff disease, in coding of the surgical procedures, or in the hospital registry that could explain the trend observed. Although the accuracy and coverage of the Finnish NHDR has been found to be excellent regarding hip and knee diseases, there is no specific information about shoulder disorders. However, we assume that the coverage and accuracy are no different from what is seen with knees and hips. A weakness of the study was that NHDR data have not been validated in private healthcare. Also, a confounding factor in the study was that the registry data did not allow us to determine if there was a change in the number of patients with rotator cuff disease who sought treatment at public and private healthcare organizations during the study period. Another weakness is that we are unable to prove that scientific evidence alone has caused the declining incidence of acromioplasty. There may be other factors that influence rates of surgery.
Relation to other studies
Others have reported a continuous increase in the incidence of acromioplasty in previous patient cohorts. In a cohort in Minnesota, CitationYu et al. (2010) reported that the incidence of acromioplasty increased over time from rates of 3 per 105 persons in the period 1980–1985 to 19 per 105 persons in 2000–2005. CitationVitale et al. (2010) studied a cohort in New York and reported that the incidence of acromioplasty both with and without rotator cuff repair increased from 30 per 105 in 1996 to 102 per 105 in 2006. In a recent study, the rate of subacromial decompression rose from 5 to 40 per105 between 2000 and 2010 in NHS hospitals across England (CitationJudge et al. 2014). Similar trends of increasing acromioplasty incidence have been reported using data from the Florida Healthcare Cost and Utilization Project’s State Ambulatory Surgery Database (HCUP SASD; 170 per 105 person years in 2007) and from the Centers for Medicare and Medicaid Services (CMS) in the USA (95 per 105 patients over 65 years of age, in 2006) (CitationPapadonikolakis et al. 2011). These studies were based on highly selected samples, and our study is the first to report nationwide incidence. The increased incidence rate (from 75 to 163 per 105 adults per year) in Finland is similar to the rates reported using data from the HCUP SASD and CMS in the USA, but it is substantially higher than rates reported by others. Here we calculated the incidence rates only for those aged 18 years or older. If the entire population had been included, the incidence rates would be approximately 20% lower, ranging from 58 to 129 per 105 person years. It was reasonable to exclude individuals younger than 18 years because the incidence of acromioplasty in this population is very low. To our knowledge, we are the first to report a declining incidence of acromioplasty. CitationJudge et al. (2014) reported an increasing incidence in England during almost the same time period. The reasons for the observed variation in incidence are likely to be multifactorial—including patient-based, surgeon-based, and systems-based factors.
Clinical implications and implications for society
Approximately half of patients who undergo acromioplasty due to rotator cuff disease with shoulder impingement syndrome are also treated using active nonoperative management (CitationYlinen et al. 2013). Adherence to current recommendations for exercise therapy has been found to be insufficient in clinical practice (CitationYlinen et al. 2013). While current research shows that operative treatment is not more effective than nonoperative management, a nonoperative approach should be preferred (CitationBrox et al. 1999, CitationHaahr et al. 2005, CitationHaahr and Andersen 2006, CitationCoghlan et al. 2008, CitationKetola et al. 2009, CitationKetola et al. 2013). Several randomized, controlled studies have shown that a progressive exercise therapy regimen that focuses on training of the rotator cuff and scapular muscles together with specific stretching exercises is effective in improving shoulder function and in reducing pain (CitationHolmgren et al. 2012, CitationKromer et al. 2013, CitationStruyf et al. 2013). The mechanism is presumed to be related to an increased range of movement and strength, which helps normalize scapulohumeral function.
Public healthcare in Finland is provided by the community, and is open to every person at a minimal cost. Surgeons receive a fixed monthly salary. People are also free to use private healthcare, in which the costs are paid for by insurance companies, employers, or by the patients themselves; in this system, surgeons receive extra fees for each operation. Interestingly, the change in the incidence of acromioplasty during the past few years has been bidirectional and appears to be associated with the type of hospital (non-profit or profit-based). A remarkable downward trend in the incidence of acromioplasty was observed in public, non-profit healthcare organizations, whereas the incidence continues to rise at private, profit-based healthcare institutions (a 490% increase over 14 years). One explanation for these contrasting trends is that there may have been a change in the proportion of patients seeking treatment for shoulder problems in private hospitals rather than public hospitals. The absolute number of operations is likely to rise if more patients seek treatment at private orthopedic clinics, even if there are no changes in the indications for surgery. Furthermore, the Ministry of Social Affairs and Health in Finland published uniform criteria for referral to non-emergency treatment in public special healthcare regarding rotator cuff disease in 2009 (CitationMinistry of Social Affairs and Health 2010). It is thus possible that some patients may have been denied access to a public hospital through adoption of the new guidelines, and elected to be treated by the private sector instead. However, the incidence of acromioplasty started to decline already in 2007, before these guidelines were available. Another explanation is the possible influence of financial interests on clinical practice in private hospitals, since the income of both the hospital and the orthopedic surgeon is related to the number of operations. In public hospitals, there is no such relationship between income and operations.
Conclusions
We observed a declining incidence of acromioplasty. The exact reason for this change cannot be defined based on registry data alone. This decline was not observed in private orthopedic clinics, where the incidence rates have continued to increase even in recent years. The possible influence of the type of practice (profit or non-profit) on the decision to recommend surgery or nonoperative management for rotator cuff disease merits further investigation.
JP: design of study, acquisition of data, analysis and interpretation of data, and writing of the manuscript. VL: design of study, interpretation of data, and critical revision of the manuscript. JK, JY, and VÄ: interpretation of data and critical revision of the manuscript. VM: design of study, acquisition and interpretation of data, and critical revision of the manuscript.
JP, VL, JK, JY, and VM have no competing interests to disclose. JK received personal fees from Abbvie, Mundipharma, MSD, and UCB, unrelated the present work. This work was supported by an Academy of Finland grant.
- Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE. Understanding of regional variation in the use of surgery. Lancet 2013; 382 (9898): 1121-9.
- Brox JI, Gjengedal E, Uppheim G, Bohmer AS, Brevik JI, Ljunggren AE, Staff PH. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): A prospective, randomized, controlled study in 125 patients with a 2 1/2-year follow-up. J Shoulder Elbow Surg 1999; 8 (2): 102-11.
- Chaudhury S, Gwilym SE, Moser J, Carr AJ. Surgical options for patients with shoulder pain. Nat Rev Rheumatol 2010; 6(4): 217-26.
- Coghlan JA, Buchbinder R, Green S, Johnston RV, Bell SN. Surgery for rotator cuff disease. Cochrane Database Syst Rev 2008; (1): CD005619.
- Davis AD, Kakar S, Moros C, Kaye EK, Schepsis AA, Voloshin I. Arthroscopic versus open acromioplasty: A meta-analysis. Am J Sports Med 2010; 38 (3): 613-8.
- Ferlie E, Wood M, Fitzgerald L. Some limits to evidence-based medicine: A case study from elective orthopaedics. Qual Health Care 1999; 8 (2): 99-107.
- Haahr JP, Andersen JH. Exercises may be as efficient as subacromial decompression in patients with subacromial stage II impingement: 4-8-years’ follow-up in a prospective, randomized study. Scand J Rheumatol 2006; 35 (3): 224-8.
- Haahr JP, Ostergaard S, Dalsgaard J, Norup K, Frost P, Lausen S, Holm EA, Andersen JH. Exercises versus arthroscopic decompression in patients with subacromial impingement: A randomised, controlled study in 90 cases with a one year follow up. Ann Rheum Dis 2005; 64 (5): 760-4.
- Holmgren T, Bjornsson Hallgren H, Oberg B, Adolfsson L, Johansson K. Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: Randomised controlled study. BMJ 2012; 344: e787.
- Huttunen TT, Kannus P, Pihlajamäki H, Mattila VM. Pertrochanteric fracture of the femur in the Finnish National Hospital Discharge Register: validity of procedural coding, external cause for injury and diagnosis. BMC Musculoskelet Disord 2014; 15 (1): 98.
- Judge A, Murphy RJ, Maxwell R, Arden NK, Carr AJ. Temporal trends and geographical variation in the use of subacromial decompression and rotator cuff repair of the shoulder in England. Bone Joint J 2014; 96-B (1): 70-4.
- Ketola S, Lehtinen J, Westenius H, Arnala I, Nissinen M, Malmivaara A, Rousi T. Olkanivelen kiertäjäkalvosimen hankausoireyhtymän (impingement)leikkaushoidon satunnaistettu vertaileva vaikuttavuustutkimus. Suomen Ortopedia Ja Traumatologia 2005; 28 (3): 348-50.
- Ketola S, Lehtinen J, Arnala I, Nissinen M, Westenius H, Sintonen H, Aronen P, Konttinen YT, Malmivaara A, Rousi T. Does arthroscopic acromioplasty provide any additional value in the treatment of shoulder impingement syndrome? A two-year randomised controlled trial. J Bone Joint Surg Br 2009; 91 (10): 1326-34.
- Ketola S, Lehtinen J, Rousi T, Nissinen M, Huhtala H, Konttinen YT, Arnala I. No evidence of long-term benefits of arthroscopicacromioplasty in the treatment of shoulder impingement syndrome: Five-year results of a randomised controlled trial. Bone Joint Res 2013; 2 (7): 132-9.
- Kromer TO, de Bie RA, Bastiaenen CH. Physiotherapy in patients with clinical signs of shoulder impingement syndrome: A randomized controlled trial. J Rehabil Med 2013; 45 (5): 488-97.
- MacDonald P, McRae S, Leiter J, Mascarenhas R, Lapner P. Arthroscopic rotator cuff repair with and without acromioplasty in the treatment of full-thickness rotator cuff tears: A multicenter, randomized controlled trial. J Bone Joint Surg Am 2011; 93 (21): 1953-60.
- Mattila VM, Sillanpaa P, Iivonen T, Parkkari J, Kannus P, Pihlajamaki H. Coverage and accuracy of diagnosis of cruciate ligament injury in the finnish national hospital discharge register. Injury 2008; 39 (12): 1373-6.
- Milano G, Grasso A, Salvatore M, Zarelli D, Deriu L, Fabbriciani C. Arthroscopic rotator cuff repair with and without subacromial decompression: A prospective randomized study. Arthroscopy 2007; 23 (1): 81-8.
- Ministry of Social affairs and Health. Uniform criteria for access to non-emergency treatment 2010. 2010. Available from http://urn.fi/URN:ISBN: 978-952-00-3100-8.
- Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: Diagnosis and management in primary care. BMJ 2005; 331 (7525): 1124-8.
- Neer CS, 2nd. Impingement lesions. Clin Orthop Relat Res 1983; (173): 70-7.
- Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Indications for rotator cuff repair: A systematic review of the literature. Clin Orthop Relat Res 2007; 455: 52-63.
- Papadonikolakis A, McKenna M, Warme W, Martin BI, Matsen FA. Published evidence relevant to the diagnosis of impingement syndrome of the shoulder. J Bone Joint Surg Am 2011; 93 (19): 1827-32.
- Seitz AL, McClure PW, Finucane S, Boardman ND3rd, Michener LA. Mechanisms of rotator cuff tendinopathy: Intrinsic, extrinsic, or both? Clin Biomech (Bristol Avon) 2011; 26 (1): 1-12.
- Statistics Finland. Population structure. 2014 [cited 2014 Jan 31]. Available from http://www.stat.fi/til/vaerak/index_en.html.
- Struyf F, Nijs J, Mollekens S, Jeurissen I, Truijen S, Mottram S, Meeusen R. Scapular-focused treatment in patients with shoulder impingement syndrome: A randomized clinical trial. Clin Rheumatol 2013; 32 (1): 73-85.
- Sund R. Quality of the Finnish hospital discharge register: A systematic review. Scand J Public Health 2012; 40 (6): 505-15.
- Vitale MA, Arons RR, Hurwitz S, Ahmad CS, Levine WN. The rising incidence of acromioplasty. J Bone Joint Surg Am 2010; 92 (9): 1842-50.
- Ylinen J, Vuorenmaa M, Paloneva J, Kiviranta I, Kautiainen H, Oikari M, Hakkinen A. Exercise therapy is evidence-based treatment of shoulder impingement syndrome. Current practice or recommendation only? Eur J Phys Rehabil Med 2013; 49 (4): 499-505.
- Yu E, Cil A, Harmsen WS, Schleck C, Sperling JW, Cofield RH. Arthroscopy and the dramatic increase in frequency of anterior acromioplasty from 1980 to 2005: An epidemiologic study. Arthroscopy 2010; 26 (9 Suppl): S142-7.