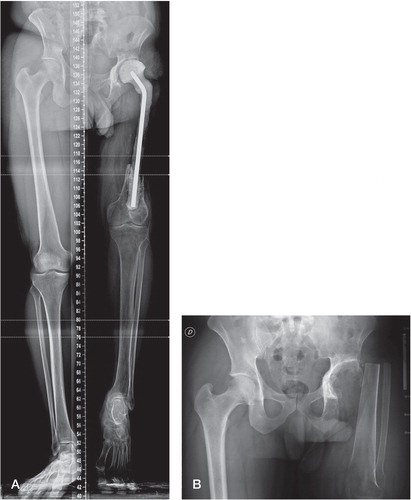
A 34-year-old man had had Ewing’s sarcoma at the age of 18, which was treated with surgical resection, megaprosthesis, and radiotherapy. He had then had multiple failures due to recurrent infection, but no tumor. He was referred to our institution in April 2010. He had had an antibiotic-loaded cement spacer implanted 2 years earlier, and now had active sinus in the lateral aspect of the thigh and fever. Radiographs showed 24-cm circumferential femoral bone loss and a type-3 AAOS acetabular defect (CitationD’Antonio et al. 1989). He was treated at our hospital with spacer removal, irrigation, and debridement, and given a new vancomyicin/gentamycin cement spacer. Cultures taken during the procedure showed a monomicrobial infection with methicillin-resistant Staphylococcus aureus. The patient was treated with intravenous vancomycin for 12 weeks, with 6 months of oral trimethoprin sulfamethoxazole. After 18 months with persistent sinus and increasing pain, he developed persistent fever and presented with a 13-cm shortening of the left leg, a homolateral knee with 15 degrees of flexion, and a fixed equinus deformation of the ankle ().
Surgical therapeutic options included hip disarticulation or a turn-up plasty according to the technique described by CitationSauerbruch (1922) and by van Nes (1948). The patient was operated in June, 2012. The infected wound was isolated and excised; then the remnant femur with the cement spacer was removed. The next step included a distal-third trans-tibiofibular amputation with ligation of neurovascular structures. Then a central dissection through the tibial crest was performed, and 2 flaps were created, one from the lateral aspect of the leg and the other from the medial aspect of the leg.
Next, the leg was turned up in the frontal plane through 180 degrees. The 2 flaps covered the anterior part of the thigh and were sutured to the remnant thigh. The distal leg was placed in the hip socket, working as a resection arthoplasty (), and the hip capsule was sutured to the muscles of the distal leg. The patient received intravenous vancomycin for 8 weeks followed by a 6-month period of oral trimethoprin sulfamethoxazole. For bureaucratic reasons, the patient received his definitive orthesis in December, 2013. In June, 2014 he was able to walk with his orthesis and 1 crutch, and had no clinical signs of infection ().
Discussion
The Sauerbruch-van Nes turn-up plasty was originally used after total or almost total resection of the femur, as in some cases of tumor, osteomyelitis, or severe trauma (CitationSauerbruch 1922, CitationVan Nes 1948). With this type of turn-up plasty, it is possible to provide the patient with a long stump, descending to the level of the lower third of the thigh, giving him/her a better chance of prosthetic rehabilitation. Patients with an amputation at the hip consider themselves to be considerably mutilated and extremely disabled.
Almost all patients with a hip disarticulation suffer from phantom pain (CitationEbrahimzadeh et al. 2013). As van Nes described in 3 patients (Citation1948), one of the main advantages of this technique is that the vessels and nerves corresponding to two-thirds of the proximal leg remain undisturbed. They make a loop in the popliteal fossa and continue their course in an upward direction. The sensitivity is uninterrupted, so that scratching on pinching of the skin on the lateral surface of the stump is localized by the patient to be on the medial side of the former leg.
Sauerbruch-van Nes total turn-up plasty could be included among the salvage procedures proposed to non-oncological patients with severe uncontrolled infection, sepsis, and massive femoral bone loss following THA.
- D’Antonio JA, Capello WN, Borden LS, Bargar WL, Bierbaum BF, Boettcher WG, Steinberg ME, Stulberg SD, Wedge JH. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1989; (243): 126-137.
- Ebrahimzadeh MH, Kachooei AR, Soroush MR, Hasankhani EG, Razi S, Birjandinejad A. Long-term clinical outcomes of war-related hip disarticulation and transpelvic amputation. J Bone Joint Surg Am 2013; 95(16): e114(1-6).
- Sauerbruch F. Die Exstirpation des Femur mit Umkipp-Plastik des Unterschenkels. Chir 1922; 169: 1-12.
- van Nes CP. Transplantation of the tibia and fibula to replace the femur following resection; turn-up-plasty of the leg. J Bone Joint Surg Am 1948; 30A(4): 854-8.