Abstract
Background and purpose — Total knee arthroplasty (TKA) for treatment of end-stage posttraumatic arthritis (PTA) has specific technical difficulties and complications. We compared clinical outcome, postoperative quality of life (QOL), and survivorship after TKA done for PTA with those after TKA performed for primary arthritis (PA).
Patients and methods — We retrospectively reviewed patients who were operated on at our institution for PTA between 1998 and 2005 (33 knees), and compared them to a matched group of patients who were operated on for PA during the same period (407 knees). Clinical outcomes and postoperative QOL were compared in the 2 groups using Knee Society score (KSS), range of motion (ROM) of the knee, and the knee osteoarthritis outcomes score (KOOS). Implant survival rate was calculated using Kaplan-Meier analysis.
Results — At a mean follow-up of 11 (5–15) years, KSS knee increased from mean 39 (SD 18) to 87 (SD 16) in the PA group (p = 0.003), and from 31 (SD 11) to 77 (SD 15) in the PTA group (p = 0.003). KSS function increased from 55 (12) to 89 (25) in the PA group (p = 0.008) and from 44 (SD 14) to 81 (SD 10) in the PTA group (p = 0.008). Postoperative ROM also improved in both groups, from 83° to 108° in the PTA group (p < 0.001) as opposed to 116° to 127° in the PA group (p = 0.001), with lower results in the PTA group (p < 0.001). KOOS was lower in the PTA group (p < 0.001). The survival rate of TKA at 10 years with an endpoint defined as “any surgery on the operated knee” showed better results in the PA group (99%, CI: 98–100 vs. 79%, CI: 69–89; p < 0.001).
Interpretation — Patients and surgeons should be aware that clinical outcome and implant survival after TKA for PTA are lower than after TKA done for PA
Posttraumatic arthritis (PTA) of the knee is a common complication of intra- or extra-articular fracture of the knee, with incidence estimated to be from 21% to 44%. There are conflicting views concerning the best management of fractures around the knee, but it is generally accepted that articular irregularity, misalignment of the lower limb, and joint instability are the leading causes of PTA (CitationRademakers et al. 2007, CitationSchenker et al. 2014). In end-stage PTA, when nonoperative treatment has failed, TKA is a valid option (CitationBedi and Haidukewych 2009). In PTA, surgeons have to deal with technical difficulties including previous scars, possible history of infection, misalignment related to malunion, stiffness, and sometimes ligament imbalance. Thus, performing TKA in PTA is more challenging than in primary osteoarthritis.
Conflicting results have been reported concerning TKA in PTA. Several publications have described the challenges and outcomes after TKA for PTA, with a high rate of complications (from 17% to 57%) (CitationLonner et al. 1999, 2000, CitationSaleh et al. 2001, CitationBuechel 2002, CitationPapadopoulos et al. 2002, CitationWeiss et al. 2003a and Citationb, CitationHaidukewych et al. 2005, CitationWu et al. 2005, CitationMorag et al. 2006, CitationPapagelopoulos et al. 2007), whereas some studies have found good results in young patients who have had TKA for secondary traumatic osteoarthritis (CitationDalury et al. 1995, CitationTai and Cross 2006). We therefore compared (1) the functional improvement, (2) quality of life (QOL) postoperatively, and (3) implant survival rate of TKA for PTA with the same parameters for TKA performed for primary arthritis (PA).
Patients and methods
Patient selection
In this retrospective study, all patients who were operated on at our institution for a PTA between 1998 and 2005 (the PTA group) were included and compared to a matched group of patients who were operated on for primary arthritis during the same period (the PA group). Using the computerized database at our institution, we identified 1,757 primary unilateral TKAs that were performed during the study period for an end-stage tri-compartmental osteoarthritis of the knee according to the Ahlback grading system (CitationAhlback 1968). In the PTA group, we included patients with a previous history of intra-articular and extra-articular fracture around the knee, regardless of the initial treatment of the fracture. In both groups, patients treated with unicompartmental knee arthroplasties were excluded and a minimum follow-up of 5 years was required. 33 TKAs of the 1,757 (2%) (involving 33 patients) were done because of PTA and 1,628 of the 1,757 (93%) were TKAs for PA. Among the unilateral cases in the PA group, based on clinical records and the institutional database, patients were matched according to demographics including age, BMI, Charnley classification, and follow-up. Following this matching, 407 patients (407 knees) were assigned to the PA group and compared to the PTA group (). In the PTA group, the mean delay from the original trauma to TKA was 14 (SD 7) years. Initial fracture management, fracture characteristics, amount of bone loss (classified according to the Anderson Orthopaedics Research Institute Bone Defect Classification (CitationJacofsky el al. 2010)), and scar pattern are reported in .
Table 1. Summary of the main characteristics of the patients in the 2 groups
Table 2. Summary of the main characteristics of fractures and scar patterns in the PTA group
Surgical procedure
Before TKA, all patients had had a standardized preoperative radiographic evaluation including anteroposterior (AP), lateral, varus, and valgus stress radiographs and Merchant views of the knee, in addition to a full-length standing hip-to-ankle radiograph.
In the PA group, a cemented posterior-stabilized TKA (LPS Flex Mobile; Zimmer, Warsaw, IN) was used in all cases. A standard medial parapatellar approach was always performed, both femoral and tibial components were cemented, and the patella was systematically resurfaced. No additional osteotomies were necessary for the purpose of exposure in the PA group. No intraoperative fractures were reported.
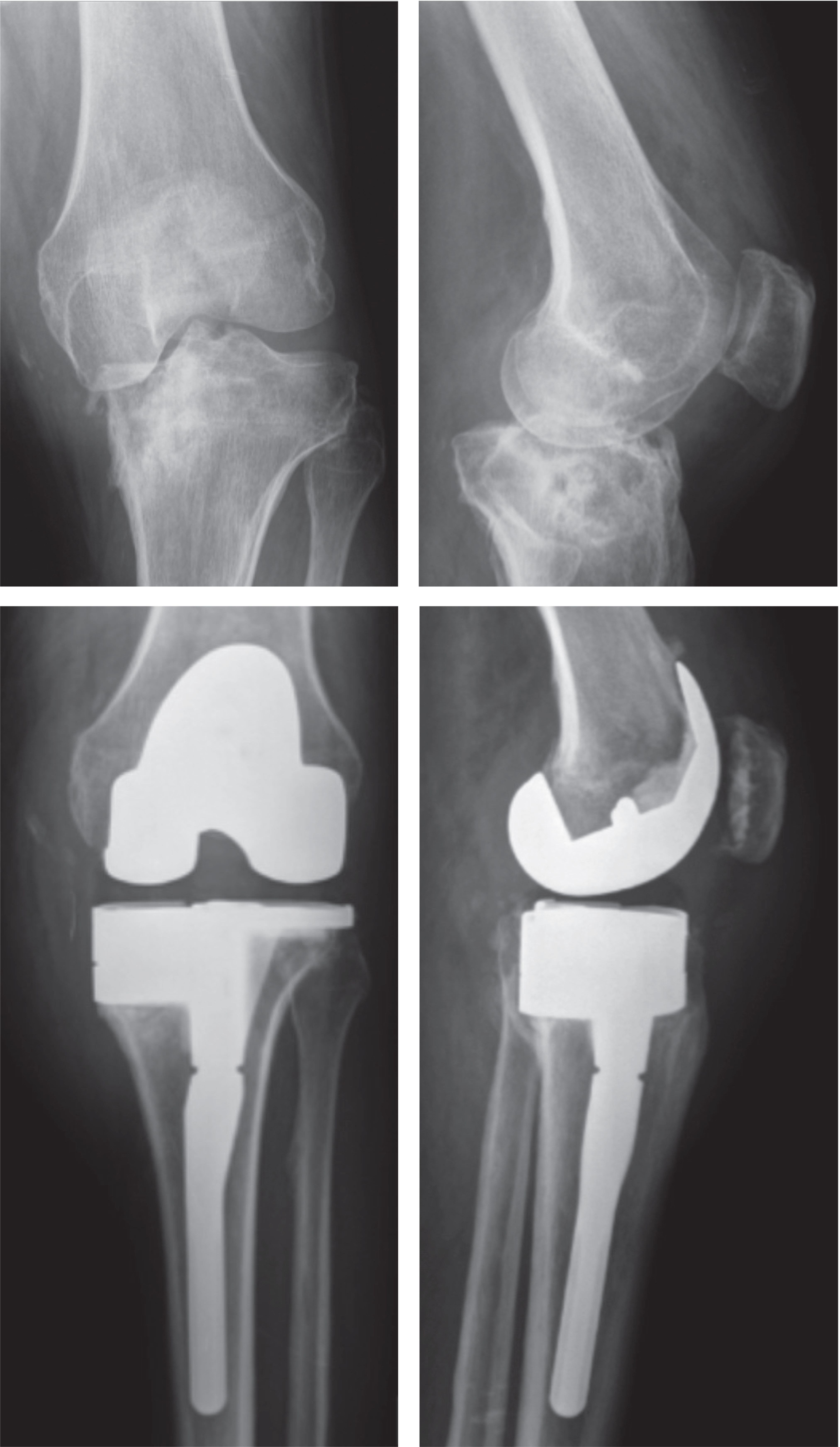
In the PTA group, a standard postero-stabilized TKA was used for 17 patients (Nexgen; Zimmer), and an augmented posterior-stabilized TKA was used for 16 patients (LCCK with standard PS insert; Zimmer). All the implants were cemented and the patella was always resurfaced. Cutaneous approach was chosen according to previous surgeries, then a standard medial parapatellar approach was used and 3 times osteotomies of the tibial tuberosity were necessary. 6 patients underwent a proximal tibial osteotomy and 3 patients underwent a distal femoral osteotomy simultaneously with TKA due to a malunion leading to a frontal deformity greater than 10 degrees. For all the cases requiring an osteotomy, the osteotomy was done to correct an extra-articular malunion. 4 patients with knee stiffness required soft tissue release. 13 patients (6 femurs and 7 tibias) presented a severe bone defect classified as type 2, which needed stems and augments (). In 3 patients with severe demineralized bone, a femoral or tibial stem extension was used. No intraoperative fractures were noted.
Figure 1. A typical case: a 60-year-old active man with a history of fracture of the medial tibial plateau. TKA required use of stems and augments and a muscular flap. At 8 years, the patient is doing well but still has limitation of flexion at 105° and is limited during his activities of daily living. The implant is radiographically stable.
Follow-up and method of evaluation
At our institution, regular clinical and radiographic follow-up after TKA is performed at 3 months, 1 year, 2 years, 5 years, and every 5 years thereafter (standard AP, lateral and full-length standing hip-to-ankle radiographs). The Knee Society knee score and function score (CitationInsall et al. 1989) and range of knee flexion (using a goniometer) were recorded preoperatively and at the follow-up visits. Data were collected prospectively. Patients were reviewed and the quality of life (QOL) of patients was determined at the last follow-up using the validated version of the self-administrated KOOS (CitationOrnetti et al 2007). At the last review, 30 patients were available in the PTA group: 2 patients had died and 1 patient was lost to follow-up. 402 patients were available in the PA group: 3 patients had died and 2 patients were lost to follow-up. For these 8 patients who had died or were lost to follow-up, the routine 5-year follow-up examination was used. The mean follow-up was 11 (5–15) years.
The survival rate of TKA in both groups was calculated according to CitationTew and Waugh (1982) and was assessed with 2 different endpoints. The first endpoint was defined as “any surgery on the operated knee” and the second was defined as “prosthesis revised for mechanical failure or infection”. Complications were reported as a reoperation when no implant exchange was performed, and as a revision if the prosthesis had been removed and replaced.
Statistics
The characteristics of patients, results of KSS knee, KSS function, ROM, and results of the KOOS score are reported as mean (SD). Qualitative variables were compared using chi-squared test and quantitative variables were compared with Student’s t-test. QOL was compared between groups at last follow-up. The Mann-Whitney test for matched-pair comparisons was used to analyze results of clinical outcomes and QOL. Any p-value < 0.05 was considered to be statistically significant. In survivorship analysis, Mantel-Cox log rank was used to assess significance during the construction of all Kaplan-Meyer curves. Confidence intervals (CIs) at the 95% level were determined.
Ethics
Institutional Review Board (IRB)/Ethics Committee approval was obtained (no. 2010-124664-32).
Results
At the last follow-up (), in the PA group the mean KSS knee value improved from 39 (SD 18) to 87 (SD 16) (p = 0.003) and in the PTA group, it improved from 31 (SD 11) to 77 (SD 15) (p = 0.003). Thus, the mean KSS knee value in the PTA group was significantly lower than in the PA group (p = 0.02), but the amount of improvement between the 2 groups was similar (p = 0.4). The mean KSS function improved from 55 (SD 12) to 89 (SD 25) in the PA group (p = 0.008), and from 44 (SD 14) to 81 (SD 10) in the PTA group (p = 0.008). The mean KSS function value was therefore significantly lower in the PTA group than in the PA group (p = 0.03), but the amount of improvement between the 2 groups was similar (p = 0.3).
Table 3. Medium-term results of clinical outcomes and range of motion (ROM) in both groups preoperatively and at the last follow-up. Values are mean (SD)
Postoperative ROM also improved in both groups, from 83° to 108° (p < 0.001) in the PTA group and from 116° to 127° (p = 0.001) in the PA group. Thus, even though the improvement in ROM was better in the PTA group (25° as opposed to 11°), the results were significantly lower than in the PA group (p < 0.001) and the amount of improvement between the 2 groups was significantly different (p < 0.001).
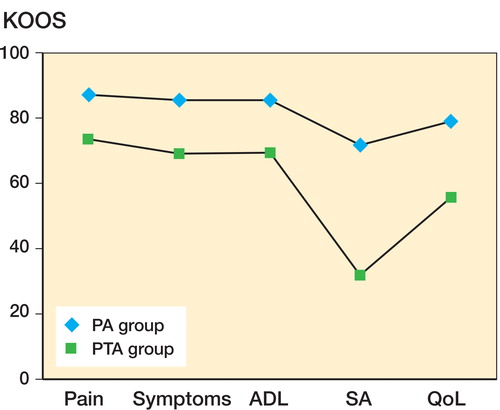
Lower QOL scores were observed in the PTA group for the 5 subcategories of the KOOS (). In the PA group, the mean KOOS pain value was 86 (SD 17) points and it was 72 (SD 20) points in PTA group; the mean KOOS symptoms values were 85 (SD 16) and 68 (SD 15); the mean KOOS activities of daily living values were 85 (SD 18) and 69 (SD 21); the mean KOOS sport activities values were 70 (SD 32) and 31 (SD 18); and the mean KOOS quality of life values were 78 (26) and 55 (25). There were significant differences between groups in all dimensions of KOOS (p < 0.001).
Figure 2. Postoperative results of the KOOS for the 2 groups (the primary arthritis (PA) group and the posttraumatic arthritis (PTA) group). ADL: activities of daily living; SA: sport activity; QoL: quality of life. There were significant differences between groups in all dimensions of KOOS (p < 0.001).
Survival rate at 10 years considering first the endpoint defined as “any surgery on the operated knee” was significantly lower (p < 0.001) in the PTA group (79%, CI: 69–89) than in the PA group (99%, CI: 98–100), with reoperation mainly performed within the 2 first years after the TKA. Survival rate considering the second endpoint defined as “prosthesis revised for mechanical failure or infection” was also significantly lower (p = 0.002) in the PTA group (94%, CI: 89–99) than in the PA group (100%, CI: 99–100).
At the last follow-up, the overall rate of complications was significantly higher in the PTA group than in the PA group (p < 0.001) ().
Table 4. Overall rate of complications a
Discussion
We found worse clinical results in the PTA group than in the PA group in terms of pain, flexion, walking ability, and stair climbing. The QOL was also significantly worse in the PTA group than in the PA group. Finally, one-fifth of the patients in the PTA group required a reoperation within 2 years after TKA. The 10-year survivorship was also lower in the PTA group than in the PA group. It is worth noting that the net improvement over baseline in subjective and functional scores was similar for PTA TKAs and TKAs performed for osteoarthritis. This suggests that the overall differences noted in these parameters may be largely due to differences in the preoperative status of the patients rather than being intrinsic to the success of the procedure. In other words, the procedure improved the subjective parameters equally in both patient groups, and the PTA group simply started with worse knee function.
Our study had certain limitations. Most importantly, it was retrospective. Secondly, patients included in the PTA group had initially had different modalities of fracture management, and due to the lack of exact fracture management history for most of the patients, we were unable to analyze the influence of each type of initial treatment. However, it was not our purpose to examine the influence of initial treatment on outcomes. Thirdly, patients with arthritis secondary to intra- and extra-articular fractures around the knee were included. These 2 entities can be considered to be different problems in terms of surgical management. However, we included both types of fractures in our study because—in terms of information, infection prevention, and potential skin problems—management is the same (CitationLonner et al. 1999, Citation2000, CitationWeiss et al. 2003a and Citationb). Indeed, the initial treatment of the fracture, the alignment, and the positioning of implants appear to be the most important predictors of outcome, both in intra-articular and extra-articular fractures (CitationLonner et al. 1999, Citation2000, CitationWeiss et al. 2003a and Citationb). Despite these limitations, to our knowledge the present study is the first comparative study to include functional outcome, QOL, and survival rate after TKA for PTA, with a minimum follow-up of longer than 5 years.
Our medium-term results showed that patients’ functional results improved after TKA for PTA but the final results were lower than after primary TKA. Our results are similar to the results of previous major studies covering 223 TKAs performed after tibial and femoral fractures (CitationLonner et al. 1999, CitationPapadopoulos et al. 2002, CitationWeiss et al. 2003, CitationMorag et al. 2006). Indeed, both postoperative KSS scores (knee and function) improved similarly in the 2 groups, but they remained lower in the PTA group. The natural history of osteoarthritis after intra- or extra-articular fracture includes trauma, which leads to hemarthrosis or periarticular hematoma and to an initial treatment involving one or more operations with or without an immobilization. This sequence of events has several implications for prosthetic surgery: first, the existence of a posttraumatic fibrosis of the joint; second, damage to the cartilage joint; and finally, deformation of the lower limb. Fibrosis makes surgery more difficult (CitationMassin et al. 2011, CitationShearer el al. 2013). Thus, in our series an osteotomy of the tibial tuberosity was necessary in 3 patients to obtain better exposure, and in 4 patients a soft tissue release was performed. Additional procedures to facilitate exposure have also been reported in previous studies, and the goal is to choose the least aggressive one while preserving the extensor mechanism (CitationLonner el al. 1999, CitationMassin et al. 2011, CitationShearer el al. 2013), with no risk of compromising the result (CitationMassin et al. 2011). Our results showed this difference to be related to fibrosis, especially for postoperative ROM, where results in the PA group (127°) were better than in the PTA group (108°), but in the PTA group the gain in flexion was higher than in the PA group (25° and 11°, respectively). Several previous studies have outlined this gain of flexion in patients with posttraumatic arthritis (CitationLonner et al. 1999, CitationPapadopoulos et al. 2002, CitationWeiss et al. 2003a and Citationb, CitationMorag et al. 2006, CitationMassin et al. 2011) and the final flexion and the gain in flexion were correlated to the preoperative flexion (CitationMassin et al. 2011). However, superior gain in flexion can be achieved in severe cases of limitation of flexion by releasing the extensor apparatus, in the absence of cutaneous scar tissue retractions and recent infection (CitationMassin et al. 2011). Recently, CitationShearer et al. (2013) concluded that isolated articular deformities have the greatest improvement in pain and function while patients with combined tibial and femoral deformities and also patients with soft tissue compromise experience poor outcomes. The number of patients in our study was not large enough to allow us to conduct any multivariable statistical analysis, but the factors identified in these studies (CitationMassin et al. 2011, CitationShearer et al. 2013) such as combined tibial and femoral deformities and soft tissue compromise were similar to the factors identified in our study.
According to the present findings, patient QOL improved after TKA for PTA but the final results were lower than after primary TKA. Postoperatively, the 5 items of the KOOS were all better in the PA group than in the PTA group, and the score for the item “function during activities of daily living” was particularly low in the PTA group. The scores were even worse for the items “leisure activities” and “quality of life”. QOL is rarely reported in the literature (CitationLonner et al. 1999, CitationPapadopoulos et al. 2002, CitationWeiss et al. 2003a and Citationb, CitationMorag et al. 2006, CitationMassin et al. 2011, CitationShearer el al. 2013), but CitationSaleh et al. (2001) found low average SF-36 scores for physical functioning and vitality after TKA for PTA, which would appear to confirm our results.
Another consequence of TKA in patients with PTA is the joint destruction associated with bone loss. In order to optimize binding and stability of the implants, we had to use stems and augments in 13 patients, and in 3 patients with severe demineralized bone we had to use femoral or tibial stem extension. We have never used augments and femoral or tibial stem extension in PA group patients. The same need for stem extension and augments has been reported in previous studies (CitationLonner et al. 1999, CitationLonner et al. 2000, CitationSaleh et al. 2001, CitationBuechel 2002, CitationPapadopoulos et al. 2002, CitationWeiss et al. 2003, CitationHaidukewych et al. 2005, CitationWu et al. 2005, CitationMorag et al. 2006, CitationPapagelopoulos et al. 2007, CitationMassin et al. 2011). The articular destruction and the need for different implants may explain the differences in survivorship observed in our study. Survival rate after TKA for PTA has been rarely reported. Studies with the longest follow-up are the series from the Mayo Clinic with a 4.7-year follow-up for TKA following tibial fracture and 6.2-year (clinical) follow-up for TKA following femoral fracture (CitationWeiss et al. 2003a and Citationb). The overall rate of complications in the Mayo Clinic series was 34% (at 4.7 years) for TKA done after tibial fracture and 27% (at 6.2 years) for TKA done after femoral fracture (CitationWeiss et al. 2003a and Citationb).
In summary, even though TKA for PTA can achieve similar net improvements in symptoms and function to those of TKA performed for osteoarthritis, because of the initially poorer status of the PTA TKAs, our study confirms that overall results of TKA performed for PTA are poorer than those of TKA performed for PA.
AL gathered and analyzed the data, and wrote the manuscript. SP designed the study and wrote the manuscript. AG and KGP gathered and analyzed the data. MO also analyzed the data. JNA designed the study and improved the manuscript.
We thank Vincent Pradel for his help with statistical analysis.
No competing interests declared.
- Ahlback S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 1968; 277: 7-72.
- Bedi A, Haidukewych GJ. Management of the posttraumatic arthritic knee. J Am Acad Orthop Surg 2009; 17: 88-101.
- Buechel FF. Knee arthroplasty in post-traumatic arthritis. J Arthroplasty 2002; 17: 63-8.
- Dalury DF, Ewald FC, Christie MJ, Scott RD. Total knee arthroplasty in a group of patients less than 45 years of age. J Arthroplasty 1995; 10: 598-602.
- Haidukewych GJ, Springer BD, Jacofsky DJ, Berry DJ. Total knee arthroplasty for salvage of failed internal fixation or nonunion of the distal femur. J Arthroplasty 2005; 20: 344-9.
- Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 1989; 248: 13-4.
- Jacofsky DJ, Della Valle CJ, Meneghini RM, Sporer SM, Cercek R M; American Academy of Orthopaedic Surgeons. Revision total knee arthroplasty: what the practicing orthopaedic surgeon needs to know. J Bone Joint Surg (Am) 2010; 92: 1282-92.
- Lonner JH, Pedlow FX, Siliski JM. Total knee arthroplasty for post-traumatic arthrosis. J Arthroplasty 1999; 14: 969-75.
- Lonner JH, Siliski JM, Lotke PA. Simultaneous femoral osteotomy and total knee arthroplasty for treatment of osteoarthritis associated with severe extra-articular deformity. J Bone Joint Surg (Am) 2000; 82: 342-8.
- Massin P, Bonnin M, Parratte S, Vargas R, Piriou P, Deschamps G; French Hip Knee Society (SFHG). Total knee replacement in post-traumatic arthritic knees with limitation of flexion. Orthop Traumatol Surg Res 2011; 97: 28-33.
- Morag G, Kulidjian A, Zalzal P, Shasha N, Gross AE, Backstein D. Total knee replacement in previous recipients of fresh osteochondral allograft transplants. J Bone Joint Surg (Am) 2006; 88: 541-6.
- Ornetti P, Parratte S, Gossec L, Tavernier C, Argenson JN, Roos EM, Guillemin F Maillefert JF. Cross-cultural adaptation and validation of the French version of the Knee injury and Osteoarthritis Outcome Score (KOOS) in knee osteoarthritis patients. Osteoarthritis Cartilage 2007; 16: 423-4.
- Papadopoulos EC, Parvizi J, Lai CH, Lewallen DG. Total knee arthroplasty following prior distal femoral fracture. Knee 2002; 9: 267-74.
- Papagelopoulos PJ, Karachalios T, Themistocleous GS, Papadopoulos EC, Savvidou OD, Rand JA. Total knee arthroplasty in patients with pre-existing fracture deformity. Orthopedics 2007; 30: 373-8.
- Rademakers MV, Kerkhoffs GM, Sierevelt IN, Raaymakers EL, Marti RK. Operative treatment of 109 tibial plateau fractures: five- to 27-year follow-up results. J Orthop Trauma 2007; 21: 5-10.
- Saleh KJ, Sherman P, Katkin P, Windsor R, Haas S, Laskin R, Sculco T. Total knee arthroplasty after open reduction and internal fixation of fractures of the tibial plateau: a minimum five-year follow-up study. J Bone Joint Surg (Am) 2001; 83: 1144-8.
- Schenker ML, Mauck RL, Ahn J, Mehta S. Pathogenesis and Prevention of Posttraumatic Osteoarthritis after Intra-articular Fracture. J Am Acad Orthop Surg 2014; 22: 20-28.
- Shearer DW, Chow V, Bozic KJ, Liu J, Ries MD. The predictors of outcome in total knee arthroplasty for post-traumatic arthritis. Knee 2013; 20(6): 432-6
- Tai CC, Cross MJ. Five- to 12-year follow-up of a hydroxyapatite-coated, cementless total knee replacement in young, active patients. J Bone Joint Surg (Br) 2006; 88: 1158-63.
- Tew M, Waugh W. Estimating the survival time of knee replacement. J Bone Joint Surg (Br) 1982; 64: 579-82.
- Weiss NG, Parvizi J, Hanssen AD, Trousdale RT, Lewallen DG. Total knee arthroplasty in post-traumatic arthrosis of the knee. J Arthroplasty 2003a; 18: 23-6.
- Weiss NG, Parvizi J, Trousdale RT, Bryce RD, Lewallen DG. Total knee arthroplasty in patients with a prior fracture of the tibial plateau. J Bone Joint Surg (Am) 2003b; 85: 218-21.
- Wu LD, Xiong Y, Yan SG, Yang QS. Total knee replacement for posttraumatic degenerative arthritis of the knee. Chin J Traumatol 2005; 8: 195-9.

