Abstract
Background and purpose — Treatment of Dupuytren’s contracture (DC) with collagenase Clostridium histolyticum (CCH) consists of injection followed by finger manipulation. We used a modified method, injecting a higher dose than recommended on the label into several parts of the cord, which allows treatment of multiple joint contractures in 1 session and may increase efficacy. We studied the occurrence of skin tears and short-term outcome with this procedure.
Patients and methods — We studied 164 consecutive hands with DC, palpable cord, and extension deficit of ≥ 20º in the metacarpophalangeal (MCP) and/or proximal interphalangeal (PIP) joint (mean patient age 70 years, 82% men). A hand surgeon injected all the content of 1 CCH vial (approximately 0.80 mg) into multiple spots in the cord and performed finger extension under local anesthesia after 1 or 2 days. A nurse recorded skin tears on a diagram and conducted a standard telephone follow-up within 4 weeks. A hand therapist measured joint contracture before injection and at a median of 23 (IQR: 7–34) days after finger extension.
Results — A skin tear occurred in 66 hands (40%). The largest diameter of the tear was ≤ 5 mm in 30 hands and > 10 mm in 14 hands. Hands with skin tear had greater mean pretreatment MCP extension deficit than those without tear: 59º (SD 26) as opposed to 32º (SD 23). Skin tear occurred in 21 of 24 hands with MCP contracture of ≥ 75º. All tears healed with open-wound treatment. No infections occurred. Mean improvement in total (MCP + PIP) extension deficit was 55º (SD 28).
Interpretation — Skin tears occurred in 40% of hands treated with collagenase injections, but only a fifth of them were larger than 1 cm. Tears were more likely in hands with severe MCP joint contracture. All tears healed without complications. Short-term contracture reduction was good.
Collagenase Clostridium histolyticum (CCH) injection is a non-surgical treatment option for patients with Dupuytren’s contracture (DC) of the fingers (CitationHurst et al. 2009). Treatment with CCH involves injection of CCH into the cord, followed after about 24 hours (according to the label) by finger manipulation (extension) under local anesthesia. Skin tears may occur during this extension. In the first multicenter randomized trial (with finger extension done without anesthesia), skin tears occurred in 11% of cases (CitationHurst et al. 2009). Other authors have reported skin tears in up to 19% of CCH-treated patients (CitationSkirven et al. 2013, CitationManning et al. 2013). Finger extension after CCH injection is a painful procedure. Although use of local anesthesia may improve contracture reduction, it may also increase the risk of skin tears. No studies have specifically investigated skin tears that occur during finger extension.
According to the standard method, contractures of the metacarpophalangeal (MCP) joint and proximal interhlangeal (PIP) joint are treated separately. For fingers with both MCP and PIP contracture, 2 injections are given at an interval of 1 month. We have used a modified method, injecting a higher dose than recommended on the label in multiple spots in the cord in one session (CitationAtroshi et al. 2014). With this method, fingers with both MCP and PIP joint contracture are treated in 1 stage. We performed a prospective cohort study of collagenase injections in DC to determine the incidence, characteristics, risk factors, and healing of skin tears, and also the short-term contracture outcome.
Patients and methods
We conducted a prospective cohort study at one orthopedic department (Hässleholm, Kristianstad, and Ystad Hospitals) in Southern Sweden. The department is the only center to treat patients with DC in a region of approximately 300,000 inhabitants. The eligibility criteria for CCH injections were the presence of a palpable cord and a total extension deficit of ≥ 20º in the metacarpophalangeal (MCP) and/or proximal interphalangeal (PIP) joint in at least 1 finger. Between December 2012 and November 2013, 164 hands of 146 consecutive patients with DC treated with CCH injections were included. Mean patient age was 70 (SD 8) years, and 134 of the hands (82%) belonged to men. In 23 hands, the finger treated had been operated previously with fasciectomy whereas 3 hands had been operated previously with percutaneous needle fasciotomy.
For all hands, mean MCP contracture for the treated finger (the finger with the most severe total extension deficit in hands with more than 1 treated finger) was 43º (SD 27, median 45), mean PIP contracture was 36º (SD 29, median 33), and mean total extension deficit was 79º (SD 34, median 75). Considering only joints with a contracture of at least 10º (139 MCP and 128 PIP), mean MCP contracture was 50º (SD 22, median 50) and mean PIP contracture was 47º (SD 25, median 45). In the 23 hands with previous fasciectomy in the treated finger (at least 10º of contracture in 17 MCP and 22 PIP joints), mean MCP contracture was 46º (SD 26, median 50) and mean PIP contracture was 54º (SD 27, median 60).
A single hand surgeon (IA) treated all the patients. Before treatment, 1 of 3 hand occupational therapists examined the patient and measured extension deficit in the affected fingers with a goniometer. The hand surgeon then injected CCH into the cord using a modification of the standard technique (CitationAtroshi et al. 2014). After reconstituting CCH with 0.39 mL of diluent (for both MCP and PIP joints), all the reconstituted CCH that could be withdrawn into the syringe (corresponding to approximately 0.80 mg) was injected into multiple spots in the cord. The surgeon distributed the contents of the syringe in 3 or 4 spots along the palpable cord, from the PIP joint to the palmar crease. Occasionally, in a finger with PIP contracture, the surgeon injected a clearly palpable cord distal to the PIP joint (usually a cord along the lateral or medial aspect of the small finger). Injection into areas of dense adherence of the cord to skin and flexion creases was avoided. Following CCH injection, a nurse applied a soft dressing and the therapist gave the patient verbal and written instructions regarding edema prophylaxis and avoidance of heavy use of the hand.
In 22 hands (22 patients) with DC in 2 or 3 fingers with separate cords, 2 CCH injections (approximately 0.80 mg each) were given in the same session. 2 patients received 2 injections for contracture in the same finger in 2 separate sessions at an interval of 3 months (because of failure to achieve satisfactory correction and presence of a palpable cord).
The surgeon initially performed finger extension 1 day or 2 days after CCH injection, as the schedule permitted, but used only a 2-day interval after the first 53 hands. Before finger manipulation, the surgeon injected a local anesthetic proximal to the palmar crease to block the nerves to the treated finger. The anesthetic used was 10 mg/mL mepivacaine, buffered by diluting 20 mL mepivacaine with 5 mL 50 mg/mL sodium bicarbonate. The amount of anesthetic injected was 10 mL in patients who had received a single CCH injection and 15–20 mL in those who had received 2 concurrent injections. The anesthetic injection site was a few centimeters proximal to the CCH injection sites (for example, in the small finger it was in the proximal part of the hypothenar region). The aim was a pain-free manipulation. After about 20 min, the surgeon performed finger manipulation. The surgeon applied pressure with the thumb along the whole length of the cord to disrupt it and then manipulated the finger by extending the MCP and PIP joints, holding the PIP joint flexed while extending the MCP joint and vice versa. The goal was to achieve the best possible correction, so manipulation was not stopped on suspecting that a skin tear was impending.
The assisting nurse documented the occurrence of skin tears (defined as full-thickness skin rupture of any size), measured their size (the largest diameter) with a surgical ruler, and recorded the location and size on a hand diagram. The nurse applied a wound dressing consisting of Mepilex silicone foam (Mölnlycke Health Care, Gothenburg, Sweden) covered by an adhesive dressing or a soft bandage. For tears smaller than 6 mm, the nurse used only a simple adhesive dressing. The nurse informed the patients about telephone follow-up and asked them to record the date when they consider the tear to have completely healed. Immediately after finger extension, the patients went to the hand therapist and received a static splint with maximally extended fingers; the therapist gave instructions on range of motion exercises, to use the hand as tolerated during daytime, and to use the splint at night for 8 weeks. Patients who sustained skin tears (except those with small tears that required only a simple adhesive dressing) were scheduled for a nurse visit at the orthopedic department or were advised to visit the primary care nurse within 2–5 days for a change of dressing. Depending on the wound status at that visit, further visits for inspection of the wound and dressing change followed as necessary. The patients were advised to call the department or primary care if they needed further wound care. The patients returned to the therapist 1 week after treatment for splint adjustment, and they made further visits to the therapist when it was judged necessary based on hand status. The therapist measured extension deficit during each visit.
The assisting nurse conducted a telephone follow-up 2–4 weeks after finger extension, asking the patient about whether the skin tear had healed, the approximate date when the patient considered the tear to have healed, and about the presence of residual pain or any other complications.
All the patients responded to the telephone follow-up. 5 patients did not attend the post-treatment examination performed by the therapist.
Statistics
Before the study, we estimated that 150 hands would receive CCH injections during 1 year. In our previous study of CCH injections, skin tear had occurred in 9 of 16 patients (CitationAtroshi et al. 2014). Assuming a similar proportion of skin tears, 150 hands would be adequate to study the characteristics and possible risk factors and complications. Based on the earlier results, this number of hands would also be adequate to study short-term contracture outcome.
We calculated the proportion of hands that sustained a skin tear of any severity. The tears were analyzed according to the finger involved, location (distal palm, proximal digital crease, or distal to that level), and size (largest diameter up to 5 mm, 6–10 mm, or more than 10 mm). We compared hands that sustained a tear with those that did not sustain a tear with regard to patient age and sex, previous fasciectomy in the treated finger, interval between injection and finger extension (1 or 2 days), number of CCH injections received in one session, and pretreatment MCP and PIP extension deficits. We categorized the time to wound healing reported by the patient as < 1 week, 1–2 weeks, and > 2 weeks. We calculated the post-treatment extension deficit recorded at the last therapist visit after finger extension; the median number of days was 23 (interquartile range (IQR): 7–34). The missing values for the 5 patients who did not attend follow-up examination were not replaced. We used Fisher’s exact test and t-test for categorical and continuous variables, respectively, and fixed-time Cox regression for adjusted analyses. A 2-sided p-value of < 0.05 indicated statistical significance.
Ethics
This research was reviewed by the Regional Ethics Review Board in Lund (journal no. 2013/656) and was conducted in accordance with the Helsinki Declaration of 1975 as revised in 2000.
Results
Skin tears
Skin tears occurred in 66 hands of 64 patients (40% of the treated hands), 12 of which had 2 tears. The skin tear involved the small finger in 39 of the 66 hands (59%), the ring finger in 18 (27%), the middle finger in 8 (12%), and the index finger in 1 hand. The location of the tear was the distal palm in 20 hands (30%), the proximal digital crease in 27 hands (41%), and in the finger distal to that level in 19 hands (29%). The largest diameter of the tear was ≤ 5 mm in 30 hands (45%), 6–10 mm in 22 hands (33%), and > 10 mm in 14 hands (21%).
The hands that sustained a skin tear did not differ significantly from those that did not sustain a tear with regard to patient age and sex, previous fasciectomy in the treated finger, or injection-extension interval (). A skin tear occurred in 1 of the 3 hands treated with CCH because of contracture recurrence after previous percutaneous needle fasciotomy.
Table 1. Patient characteristics according to the occurrence of skin tears during finger extension after collagenase injection for Dupuytren’s contracture. Unless otherwise indicated, values are n (%)
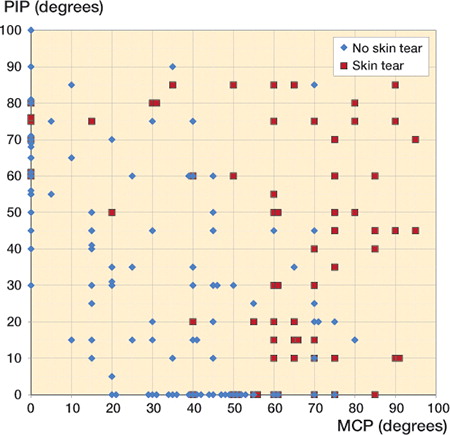
Mean pretreatment MCP extension deficit in hands that sustained a tear was 59º (SD 26); in hands that did not sustain a tear it was 32º (SD 23); mean total (MCP and PIP) extension deficit was 101º (SD 34) and 64º (SD 26), respectively (p < 0.001). A skin tear occurred in 21 of 24 hands with MCP contracture ≥ 75º (). Hands that received 2 injections in the same session were significantly more likely to sustain skin tears, but these hands also had more severe MCP contracture in the most affected finger than those that received 1 injection (mean 60º (SD 18) vs. 40º (SD 28); p < 0.001). Analyses including only the first treatment given to each patient (n = 146) gave similar results.
Figure 1. Pretreatment contracture of the metacarpophalangeal (MCP) and the proximal interphalangeal (PIP) joints of each treated finger, in the hands with no skin tear and in those with skin tear, measured at 5° intervals. (Data points representing fingers with identical contractures have been juxtaposed for visual clarity).
At the telephone follow-up, all tears were reported to have healed; time to healing was < 1 week in l3 hands, l–2 weeks in 37 hands, and > 2 weeks in 16 hands. No infections or other complications occurred and none of the patients had residual pain. None of them received antibiotic treatment or underwent surgical intervention for the skin tear.
Short-term contracture outcome
For all 159 treated fingers for which follow-up measurements were available, mean post-treatment contracture for the MCP joints was 9° (SD 14, median 0), and for the PIP joints it was 15° (SD 18, median 10). Mean change (improvement) in total (MCP + PIP) extension deficit was 55º (SD 28). Considering only joints with contracture of at least 10º before treatment and for which follow-up measurements were available (134 MCP and 125 PIP joints), mean improvement in MCP contracture was 39º (SD 20, median 40) and mean improvement in PIP contracture was 28º (SD 19, median 25). In the fingers treated with CCH because of contracture recurrence after fasciectomy, mean improvement in total extension deficit was 43º (SD 28, median 40).
Discussion
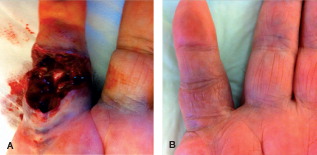
This prospective cohort study showed that 40% of hands with Dupuytren’s contracture treated with CCH injections using a higher dose than on the label sustained a skin tear during finger extension. Of the hands that received a single injection (approximately 0.8 mg) per treatment session, skin tear occurred in one-third. A skin tear was more likely in hands with severe MCP joint contracture. Most tears were minor, measuring 5 mm or less in almost half of the patients. The majority healed within 2 weeks. However, relatively large skin tears with exposed tendon sheath in the fingers also occurred (), but all healed with the wound left open, without any surgical intervention. This suggests that skin tears associated with CCH treatment can heal spontaneously irrespective of size. It is well known that incisions in the palm after limited fasciectomy can be left open (CitationHurst 2010). In fact, the “open palm” method has been one of the established techniques in the surgical treatment of DC. However, with the possible exception of transverse incisions within Z-plasties, it is uncommon to leave open fasciectomy incisions in the fingers. The strong healing potential of relatively large wounds on the palmar aspect of the fingers resulting from CCH injections may be surprising.
Figure 2. Dupuytren’s contracture of the right small finger (extension deficit, 75° in the metacarpophalangeal and 70° in the proximal interphalangeal joint) in a 75-year-old man. A. 2 days after injection, immediately after finger extension. B. 30 days after finger extension.
The exact mechanism and factors involved in the occurrence of skin tears in association with CCH treatment is unknown. We prospectively documented all skin tears, from minor superficial skin breakage to deeper wounds, in a standardized fashion. The rate was higher than in the few previous studies that have reported data on skin tears. This may have several explanations. First, studies may differ in their methodology and the extent to which they document skin tears of any severity. Secondly, difference in the use of anesthesia for finger manipulation is probably an important factor. The multicenter randomized trial (CitationHurst et al. 2009) reported skin tears in 22 of 204 patients but performed finger extension without anesthesia, which may explain the relatively low rate of skin tear. A prospective study that included only patients with PIP contracture exceeding 40º and permitted use of anesthesia found skin tears in 4 of 21 patients (CitationSkirven et al. 2013). Another study that used anesthesia found skin tears in 9 of 40 patients (CitationAlberton et al. 2014). Finger manipulation is a painful procedure, and local anesthesia is now standard.
Thirdly, the force used for finger manipulation may also be a factor. With finger manipulation, we aimed to achieve the best possible correction irrespective of the risk of tear. An alternative could be to stop manipulation when skin tear appears to be imminent, which would imply the need for further treatment sessions of manipulation—or even repeat injections to achieve better correction. For example, CitationHurst et al. (2009) reported a relatively low skin tear rate, but an average of more than 2 separate 0.58-mg injections per patient was given.
Finally, the CCH dose injected may influence the occurrence of skin tear. CitationHurst et al. (2009) injected 0.58 mg CCH into 1 part of the cord, whereas we injected all the retrievable content of 1 CCH vial (approximately 0.80 mg) into multiple parts of the cord. We believe that injecting a higher dose increases the efficacy of a single injection. Rupturing or dissolving several segments of the cord mimics surgical fasciectomy. It is not possible to determine the extent to which injection of a higher dose or the use of multiple injection sites may have contributed to a higher incidence of skin tears. However, the surgeon injected the CCH into multiple areas along the cord, so the amount injected in any part of the cord would not have exceeded the amount usually injected according to the on-label procedure. We did not, however, record the exact amount of CCH injected into each spot. The fact that, despite receiving the same dose, no patient with MCP contracture below 40º, isolated or combined with PIP contracture below 50º, sustained skin tear () suggests that the amount of CCH is not a major factor. In fact, skin rupture can occur without CCH. A study of percutaneous needle fasciotomy (PNF), done under local anesthesia, found the occurrence of skin “fissures”, described as “small tears that sometimes occur at the site of skin penetration during PNF once a cord has been divided and the treated digit is extended”, in 29 of 60 hands (Citationvan Rijssen et al. 2006).
A recent study that assessed the efficacy and safety of 2 concurrent 0.58-mg CCH injections found skin tears in 15 of 60 patients; the authors reported that local anesthesia was permitted but not required, and provided no further information about its use (CitationColeman et al. 2014). In the present study, 14 of the 22 patients who received 2 concurrent 0.80-mg CCH injections sustained a skin tear, but the number of injections was not a statistically significant factor when the severity of pretreatment contracture was adjusted for. We have shown that injection of 1.60 mg of CCH in 1 session is safe; this finding, not reported previously, should be helpful in facilitating quicker management of collagenase-treated patients. We believe that, as is the case with surgery, the aim should be to offer patients a 1-stage treatment of the affected hand. However, in clinical practice the treating surgeon should consider that injecting collagenase in this higher dose is currently an off-label procedure.
According to the standard method, each affected finger joint (MCP or PIP) is treated with 1 injection of 0.58 mg CCH, repeated at 1-month intervals if adequate correction has not been achieved. This implies that a patient with both MCP and PIP joints of 2 fingers affected (which is not unusual in clinical practice) would require at least 4 0.58-mg injections given in 4 sessions at 1-month intervals, and additional sessions in case of inadequate correction. In our study using a modified method, almost all the patients were treated with only 1 injection per finger. In a European study of 254 patients who received CCH, 112 (44%) received 2 or more injections (9% received 4 or 5 injections) and the mean number of injections per joint was 1.2 (CitationWarwick et al. 2015); mean improvement in total extension deficit on day 7 (maintained by day 90) was 42°. Thus, while we used fewer injections per patient than in studies using the standard method, the 55° improvement in total extension deficit is comparable to previous results. This suggests that our findings would be generalizable to patients with DC treated with collagenase.
Skin tears were slightly more frequent in the 23 hands treated with CCH injection because of contracture recurrence after previous fasciectomy than in those with no previous surgery, but the difference was not statistically significant, perhaps because of the small subgroup size. Although the fingers with recurrence after fasciectomy had more severe pre-injection PIP contracture than the fingers with no previous surgery, the short-term outcome was good, with a median improvement in total extension deficit of 40°.
Currently, there are no data on whether larger skin tears may lead to worse longer-term outcome due to scarring, or whether skin tears could facilitate better initial correction and possibly lower recurrence. Further follow-up of these patients may provide information regarding any relationship between skin tears during initial treatment and final contracture outcome.
A possible limitation of our study was the use of a telephone interview for follow-up. We believe, however, that most patients should be able to judge with reasonable accuracy whether or not a wound has healed when contacted within 4 weeks of treatment. Although the accuracy of self-reported time of complete healing is uncertain, it should not have had a substantial impact on the results, since we categorized the time to healing. Another limitation was that some patients went to primary care for further wound care. However, considering that no other healthcare facilities in the study region treat patients with DC, it is highly unlikely that patients would have sought other healthcare providers or would have been treated in primary care because of persistent wound problems and then have chosen not to report them during the telephone follow-up.
Although no complications occurred as a result of the skin tears sustained during finger extension after CCH injection in our study, these tears cause discomfort to the patients and increase the overall healthcare costs of this treatment method (because of additional visits for wound care and possible need for sick leave in patients who are employed).
In this study, we have identified the subgroup of patients with DC that is associated with a very high risk of skin tears. Future research should focus on finding methods that can reduce the incidence of skin tears.
IA: conception, design and conduction of study, data analysis and interpretation, and drafting of the manuscript. JN: acquisition and interpretation of data, and revision of the manuscript. AL, EA, and JW: conduction of study and data acquisition. MW: interpretation of data and critical revision of the manuscript.
This research was supported by Hässleholm Hospital.
IA was a member of an expert group on Dupuytren’s disease for Pfizer in 2012 and participated in meetings organized by Sobi in 2014.
- Alberton F, Corain M, Garofano A, Pangallo L, Valore A, Zanella V, Adani R. Efficacy and safety of collagenase clostridium histolyticum injection for Dupuytren contracture: report of 40 cases. Musculoskelet Surg 2014; 98 (3): 225–32.
- Atroshi I, Strandberg E, Lauritzson A, Ahlgren E, Walden M. Costs for collagenase injections compared with fasciectomy in the treatment of Dupuytren’s contracture: a retrospective cohort study. BMJ Open 2014; 4 (1): e004166.
- Coleman S, Gilpin D, Kaplan FT, Houston A, Kaufman GJ, Cohen BM, Jones N, Tursi JP. Efficacy and safety of concurrent collagenase clostridium histolyticum injections for multiple Dupuytren contractures. J Hand Surg Am 2014; 39 (1): 57–64.
- Hurst LC. Dupuytren’s contracture. In: Green’s Operative Hand Surgery (Ed. Wolfe SW, Hotchkiss RN, Pederson WC, Kozin S H)Elsevier. Philadelphia. 2010; 6: 153–4.
- Hurst LC, Badalamente MA, Hentz VR, Hotchkiss RN, Kaplan FT, Meals RA, Smith TM, Rodzvilla J. Injectable collagenase clostridium histolyticum for Dupuytren’s contracture. N Engl J Med 2009; 361 (10): 968–79.
- Manning CJ, Delaney R, Hayton MJ. Efficacy and tolerability of Day 2 manipulation and local anaesthesia after collagenase injection in patients with Dupuytren’s contracture. J Hand Surg Eur 2013; 39 (5): 466–71.
- Skirven TM, Bachoura A, Jacoby SM, Culp RW, Osterman AL. The effect of a therapy protocol for increasing correction of severely contracted proximal interphalangeal joints caused by dupuytren disease and treated with collagenase injection. J Hand Surg Am 2013; 38 (4): 684–9.
- van Rijssen AL, Gerbrandy FS, ter LH, Klip H, Werker PM. A comparison of the direct outcomes of percutaneous needle fasciotomy and limited fasciectomy for Dupuytren’s disease: a 6-week follow-up study. J Hand Surg Am 2006; 31 (5): 717–25.
- Warwick D, Arner M, Pajardi G, Reichert B, Szabo Z, Masmejean EH, Fores J, Chapman DS, Gerber RA, Huard F, Seghouani A, Szczypa PP. Collagenase Clostridium histolyticum in patients with Dupuytren’s contracture: results from POINTX, an open-label study of clinical and patient-reported outcomes. J Hand Surg Eur Vol 2015; 40 (2): 124–32.

