A 42-year-old athletic woman attended our clinic complaining of right groin pain. The pain had begun 2 years previously when jogging. The pain had gradually become worse, limiting her daily activities and any sporting activities.
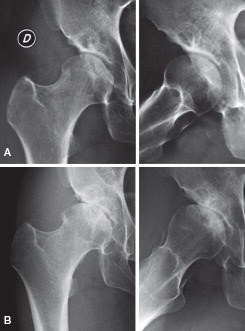
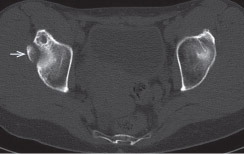
Clinical examination showed a positive impingement test and limitation of internal rotation of up to 20º at 90º of hip flexion. Plain radiogrpahs showed a normal alpha angle, and a 12 × 14 mm “os acetabuli” was present at the superolateral acetabular rim (). The joint was mildly dysplastic with a center-edge angle (CEA) (excluding the “os acetabuli”) of 15º (25º in the contralateral hip). The Tönnis angle was 24º. Differential diagnoses were an “os acetabuli” in a dysplastic hip, chronic avulsion fracture of de anteroinferior iliac spine (CitationLarson et al. 2011), stress fracture (CitationMartinez et al. 2006), or enchondroma-like lesion. The CT described the presence of an “os acetabuli” beside the joint surface with an intact anteroinferior iliac spine ().
Figure 1. Plain AP (A) and lateral view (B) showing a normal alpha angle. A 12 × 14 mm calcified irregular-shaped image was seen at the superolateral acetabular rim. Excluding the “os acetabuli”, the center-edge angle was 15º (25º in the contralateral hip). The Tönnis angle was 24º.
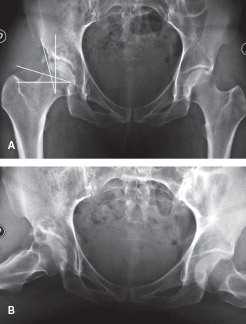
Figure 2. Sagittal plane CT scan image optimized for bone density, showing the “os acetabuli” (arrow).
The patient’s pain persisted, and we made a hip arthroscopy. She was placed supine on the traction table. Due to the shape, size, and location of the lesion, access to the central compartment was difficult and an “outside-in” technique with a T-shaped capsulotomy was performed (CitationHorisberger et al. 2010, CitationCuéllar et al. 2013). Dynamic intraoperative assessment showed impingement between the “os acetabuli” and the superior labrum, which was slightly frayed and detached from the acetabulum (). The bony lesion was dissected and resected, keeping the underlying labrum intact. The labrum was reinserted with three 2.3-mm Bioraptor bone anchors (Smith and Nephew). The capsule was then repaired with interrupted Ultrabride sutures, with 2 side-to-side sutures. No femoral osteochondroplasty was performed.
Figure 3. View of the peripheral compartment from the anteromedial portal with a 30º scope. The close relation between the detached labrum (L) and the “os acetabuli” (O) can be seen. F: femoral head.

After surgery, the patient was instructed not to bear weight for 4 weeks and then to resume partial weight bearing for another 4 weeks. Hyperextension was restricted for the first 3 months, to protect capsular healing. At 4-month follow-up, the patient was walking unaided and was free from pain; she had a full range of motion and radiographs confirmed the complete resection of the “os acetabuli”—but a slight joint narrowing was detected. At 6-month follow-up, she had again developed groin pain. At 10 months, radiographs showed a Tönnis-III degenerative stage (). A total hip replacement was required at 12 months. During the joint replacement, we found osteoarthritis and a reduction of femoral head coverage.
Discussion
The list of indications for arthroscopic hip surgery is growing. Currently, there is an open debate about the indications in borderline hip dysplasia. There are some poor prognostic factors that may contraindicate hip arthroscopic surgery, such as osteoarthritis (Tönnis grade II or more), large chondral lesions that affect the joint loading area, and chondral lesions with subchondral cysts in the femoral head, especially in patients over 50 years of age (CitationPhilippon et al. 2009). Although we found no other poor prognostic factors in our patient, a low postoperative head coverage angle should be added as a poor prognostic factor in hip arthroscopy (CitationBozic 2013).
In an attempt to minimize the risk of hip instability or degenerative joint disease following arthroscopic surgery (CitationMatsuda 2009, CitationRanawat et al. 2009), we repaired the cartilage lesion with fibrin “glue”, re-attached the labrum with bone anchors, closed the capsule with sutures, and finally protected soft tissue healing—keeping the patient from weight bearing for 4 weeks and limiting hyperextension of the hip joint.
At least 3 other cases of iatrogenic instability after hip arthroscopy in patients with dysplasia have been published. In 1 case, the instability was related to debridement of the ligamentum teres and the capsulotomy (CitationMei-Dan et al. 2012). In the other 2 cases, there was severe hip dysplasia with a CEA of only 10º and 11º (CitationMatsuda and Khatod 2012). Our patient had a mild dysplastic hip with a CEA, excluding the “os acetabuli”, of 15º. CitationParvizi et al. (2009) suggested that hip arthroscopy is not useful in dysplasic hips with a CEA of < 20º, but they did not repair the labrum. In contrast, other studies have shown improvement in hips with a CEA of < 20º when labral repair was performed (CitationByrd and Jones 2003).
When an “os acetabuli” like this is encountered, many possible origins of the bone must be considered. An enchondroma at this level is possible, but the CT scan at the arthroscopic evaluation during resection did not show any cartilaginous tissue. A chronic avulsion fracture of the anteroinferior iliac spine has a similar appearance and has been put forward as a cause for impingement (CitationLarson et al. 2011), but an intact spine was found in the CT scan. CitationMartinez et al. (2006) have suggested that these “os acetabuli” are in fact stress fractures of the acetabular rim related to primary impingement. Although this etiology could not be ruled out with certainty, under arthroscopic evaluation the separation line was not perpendicular to the joint surface, which is something that is characteristic of these fractures.
The surgery that we performed in our patient followed the usual recommendations in the literature for mildly dysplastic hips (CitationMatsuda 2009, CitationParvizi et al. 2009, CitationRanawat et al. 2009, CitationMatsuda and Khatod 2012, CitationMei-Dan et al. 2012), but this did not prevent a catastrophic failure. We propose the role of “os acetabuli” to be that of an important static stabilizer that enlarges the surface of the acetabulum. Thus, resection should be carefully planned to avoid poor femoral head coverage postoperatively (CitationMatsuda and Khatod 2012). We should add “os acetabuli” as a contributor to stabilization of a mild dysplastic hip—just like the labrum, the capsule, and ligaments (CitationBedi et al. 2011, CitationMyers et al. 2011, CitationDomb et al. 2013).
Dealing with hip problems in middle-aged patients with mild dysplasia is a challenge, as relatively minor procedures, such as the one presented here, may result in early failure of the hip joint. Perhaps a possible alternative would be to try to fix the “os acetabuli” into the acetabulum, but this has not been attempted.
- Bedi A, Galano G, Walsh C, et al. Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy 2011; 27(12): 1720–31.
- Bozic KJ. Trends in hip arthroscopy utilization in the United States. J Arthroplasty 2013; 28(8 Suppl): 140–3
- Byrd JW, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy 2003; 19(10): 1055–60
- Cuéllar R, Ruiz-Ibán MÁ, Cuéllar A, Sánchez A, et al. The peripheral compartment as the initial gateway for hip arthroscopy in complex cases: technical note. Orthopedics 2013; 36: 456–62.
- Domb BG, Stake CE, Lindner D, et al. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia. AM J Sports Med 2013;41(11): 2591–8.
- Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoroacetabular impingement of the hip: A new technique to access the joint. Clin Orthop Relat Res 2010; 468: 182–90.
- Larson CM, Kelly BT, Stone RM. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy 2011; 27: 1732–7.
- Martinez AE, Li SM, Ganz R, Beck M. Os acetabuli in femoro-acetabular impingement: stress fracture or unfused secondary ossification centre of the acetabular rim? Hip Int 2006; 16: 281–6.
- Matsuda DK. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy 2009; 25: 400–4.
- Matsuda DK, Khatod M. Rapidly progressive osteoarthritis after arthroscopic labral repair in patients with hip dysplasia. Arthroscopy 2012; 28: 1738–43.
- Mei-Dan O, McConckey M, Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy 2012; 28(3): 440–5.
- Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: An in vitro biplane fluoroscopy study. AM J Sports Med 2011; 39: 85–91.
- Parvizi J, Bican O, Bender B, et al. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arhroplasty 2009; 24(6): 110–3.
- Philippon MJ, Briggs K, Yen YM, et al. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br 2009; 9: 16–23.
- Ranawat AS, McClincy M, Sekiya JK. Anterior dislocation of the hip after arthroscopy in a patient wit capsular laxity of the hip: A case report. J Bone Joint Surg Am 2009; 91: 192–7.