Introduction
Total hip arthroplasty (THA) has proven to be a highly successful procedure in terms of improving quality of life and cost-effectiveness in older patients (CitationEthgen et al. 2004, CitationRäsänen et al. 2007). With this success, an extension of indications for total hip arthroplasty was noted and the number of primary hip arthroplasties in Europe has risen to more than 600,000 annually (CitationLabek et al. 2009). Many different types of hip prostheses are currently available. Historically, hip prostheses are categorised according to their method of fixation: with or without bone cement.
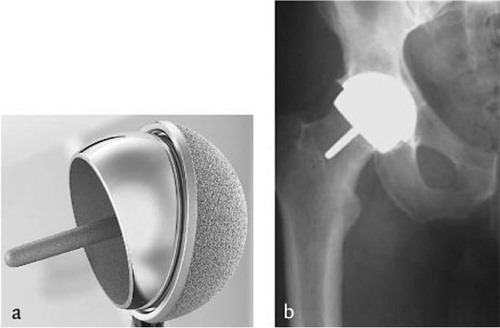
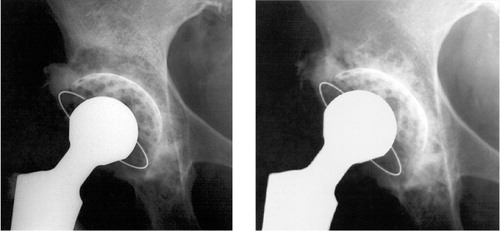
The development of the modern cemented hip prosthesis () started in the 1960s with the low friction arthroplasty designed by Sir John Charnley (Charnley 1961). The design was eventually based on the use of a metal stem with a fixed 22 mm head, which articulates with a polyethylene cup.
Figure 1a. Example of a cemented total hip arthroplasty with polyethylene cup and polished stem. 1b. Radiographic appearance.
This concept was a breakthrough in the development of the modern total hip prosthesis. Sir John Charnley introduced the use of polymethylmethacrylate bone cement to fill the gaps between the implant and bone, hence creating a stable situation for the metal stem and the polyethylene cup. He had excellent results and even today, the long-term data of the survival of the original Charnley prostheses with the polyethylene cup are part of the gold standard of THA. However, the long-term outcomes in younger patients were initially less favourable. Subsequently, technical improvements like a better cementing technique and improvements in implant materials were introduced in an effort to overcome loosening and improve long-term survival. Unfortunately, implant loosening was still seen, especially in younger patients. Loss of implant fixation is mainly caused by aseptic loosening, a multi-factorial process. During hip movement, friction of the metal head against the polyethylene cup results in small particles that accumulate in the joint space. These particles trigger the immune system by means of phagocytosis and activate cell types such as macrophages, fibroblasts, osteoblasts and osteoclasts (CitationIngham et al. 2000, CitationVermes et al. 2001). The inability to degrade these particles leads to a rise in the release of numerous cytokines and mediators that stimulate osteoclast formation and activity, leading to periprosthetic osteolysis (CitationChilds et al. 2001).
This immune response that results in bone resorption around the components causes loosening, which has been described as “particle disease” and related osteolysis by CitationHarris (1994).
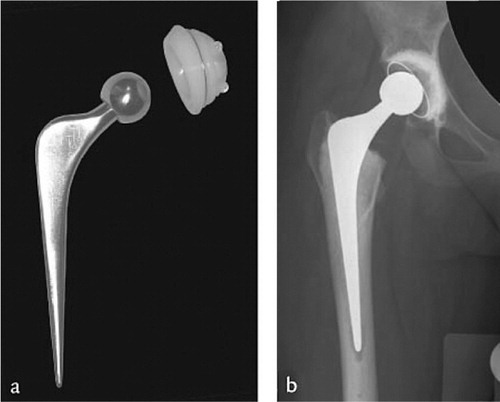
Since initially these wear-related problems were considered to be related to the use of cement, the concept of cementless total hip designs gained popularity (). These designs were developed specially for younger patients suffering from hip osteoarthritis. Initial fixation is achieved by press-fit placement of components. Depending on the design of the implant, additional screws, pegs or fins at the rim of the acetabular component can help to maintain implant position before bone ingrowth and long-term fixation are achieved. In contrast to cemented implants, many of these uncemented implants are made of titanium with a roughened surface or a coating of hydroxyapatite to enhance bony ingrowth and improve fixation. Unfortunately, osteolysis was also observed around these cementless components. It was then realized that this phenomenon was not related to the bone cement itself, but to the generation of wear particles, mainly made from polyethylene.
Figure 2a. Cementless total hip arthroplasty with screw cup and titanium stem. 2b. Radiographic appearance.

To decrease wear-related problems caused by these polyethylene particles, stronger types of polyethylene were developed. Highly cross-linked polyethylene (HXPE) and Vitamin E addition were introduced, but if these new materials will solve the problem remains uncertain, as a long follow-up is needed to determine survival.
A different strategy for solving the wear problem was the development of new bearings, like ceramic on ceramic and metal on metal. Surgeons and producers realized that these new hard bearings could be very attractive for young patients because of lower wear rates and less dislocations by using larger diameter articulations. Based on these technical innovations, the resurfacing hip was introduced in young patients, based on a large metal head and a cup with a large inner diameter (). The resurfacing hip prosthesis was a concept that had previously been used but had been abandoned at the end of the 1970s due to high failure rates. However, with the growing demands of young patients and facilitated by the potential advantage of low wear and new materials, the resurfacing hip prosthesis was introduced again. Part of the new introduction strategy was that the new resurfacing hip designs were considered to better preserve bone on the femoral side than traditional hip designs and it was suggested that these implants are relatively easy to revise in case of loosening. These potential advantages were used in the promotion of these implants in the orthopaedic practice and initially, younger patients were stimulated to take part in high level sports. This advice was adapted when it became known that survival of hip resurfacing had been compromised by high level of sports (LeDuff et al. 2012). Further research showed that the range of motion of a resurfaced and a conventional total hip were not significantly different (CitationPenny et al. 2013), but larger-diameter heads were indeed associated with a lower risk of dislocation (CitationHowie et al. 2012, CitationStroh et al. 2013).
Recent literature shows high failure rates of resurfacing prostheses (CitationLangton et al. 2011) and national registries have confirmed these higher revision rates (National Joint Registry England and Wales). This led in 2010 to withdrawal of 1 type of resurfacing hip prosthesis. However, the high mid-term failure rates were not limited exclusively to this implant and a high number of serious side effects were seen in several designs. The local metal ion debris, which is generated by these implants can cause severe local problems with a high incidence of so-called pseudotumors (CitationPandit et al. 2008, CitationVan der Weegen et al. 2013). In addition to local effects, these metal ions have shown to disseminate to other parts of the body by spreading to the lymph nodes, spleen, liver, and kidneys before being excreted in urine (CitationCase et al. 1994). General side effects have been described in relation to high levels of chromium and/or cobalt; for example, cardiomyopathy (CitationOldenburg et al. 2009), risk of chromosomal aberrations (CitationLadon et al. 2004) and risk of carcinogenesis (CitationLidgren 2008) as well as neurological and endocrinological symptoms (CitationOldenburg et al. 2009, CitationIkeda et al. 2010). The Medicines and Healthcare Products Regulatory Agency (MHRA), responsible for regulating all medicines and medical devices in the United Kingdom, released a Medical Device Alert stating that patients with metal on metal hip implants should be reviewed and monitored on a regular base (www.mhra.gov.uk). The Dutch Orthopaedic Association has endorsed this warning by the MRHA and has formulated a guideline on this subject (www.orthopeden.org). The latest alert states that large diameter head (36 mm or more) metal on metal prostheses should not be implanted until further long-term results guarantee their safety.
Survival of THA in young patients has shown to be worse compared to survival in older patients (CitationKobayashi et al. 1997, CitationSchmalzried et al. 2004). An explanation might be that young patients put higher demands on their prosthesis (CitationSchmalzried et al. 2004). Younger age by itself should be interpreted cautiously because activity levels may differ between patients (CitationDorey 2004). Pre-existing bone loss may also affect the outcome, as many younger patients already had bone stock problems at surgery. In normal hips, primary osteoarthritis is mostly seen in patients over 60 years.
Both cemented and uncemented stems have performed well in young patients showing survival rates of more than 90% at 10 years (Aldinger et al. 2003, CitationEskelinen et al. 2006, CitationBiemond et al. 2011). A study on THA in patients younger than 55 years of age in Finland suggested that uncemented stems show a higher survival rate than cemented stems (CitationEskelinen et al. 2006) although this conclusion has been questioned (CitationSchreurs et al. 2012). In general, we can conclude that survival of the femoral component is acceptable and that failure of the stem is not the main reason for revision of THA in young patients.
Most problems with fixation are seen at the acetabular side and high failure rates have been reported in several series of young patients (CitationKobayashi et al. 1997, CitationMcAuley et al. 2004, CitationEskelinen et al. 2006). Clearly, the shift towards the use of uncemented cups in young patients has not solved the problem. Polyethylene wear and osteolysis compromise the success rate of uncemented cups (CitationEskelinen et al. 2006, CitationUtting et al. 2008, CitationDella Valle et al. 2009, CitationKim et al. 2011, CitationKim et al. 2012). CitationEskelinen et al. (2006) concluded from a nationwide study on THA in patients younger than 55 years that survival rates of uncemented cups are unsatisfactorily low when liner exchanges are taken into account. Evaluating modern hip designs, only the Harris Galante II cup showed a 10-year survival rate of more than 80%, with revision of the cup for any reason as endpoint. A recent report from the Swedish Hip Register showed that after stratification into age groups, the long-term component survival with revision for any reason was lower after uncemented THA in all but the oldest age group (CitationHailer et al. 2010). A separate analysis of the cup revealed that uncemented cups had a significantly higher risk of cup revision due to aseptic loosening than cemented cups. This difference persisted even after exclusion of those revisions in which only liner exchange had been performed. Remarkably, the 2010 report of the Swedish Hip Registry stated that a reduced risk of cup revision was found for uncemented cups in patients up to 69 years (www.shpr.se, CitationAnnual Report 2010). This clearly demonstrates that the most durable option for acetabular fixation in young patients is still a topic of debate.
The term “young patient” needs to be clarified as this term is used by numerous authors in different ways. The term “young patient” can mean active patients under 65 years (CitationMeftah et al. 2013) but it was also used for a series of patients with a mean age of 25 years (CitationKumar et al. 1998). In the first age group, most patients will suffer from primary osteoarthritis since in the latter, practically all patients will suffer from an underlying disease. This also applies to the series of patients presented in this thesis and therefore, we would like to emphasize that these are different groups of patients and that results should be compared cautiously.
Several factors influence the outcome of THA in young patients. Young patients often suffer from an underlying disease like rheumatoid arthritis, Perthes disease, osteonecrosis or developmental dysplasia of the hip (DDH) that cause degenerative hip disease or secondary osteoarthritis. Because of these underlying diseases, hip anatomy may be altered and the accompanying bone stock deficiencies could make it difficult to achieve stability with a standard implant. Patients with DDH often show a deficient acetabular superolateral rim, whereas protrusio acetabuli is more often seen in rheumatoid patients. These variations in anatomy require a patient-matched solution which might compromise the survival of the reconstruction.
Depending on the type of acetabular defect, several techniques and implants can be used for reconstruction. A useful classification for acetabular defects has been made by the American Academy of Orthopaedic Surgeons (AAOS), committee on the hip (CitationD’Antonio et al. 1989) ().
Table 1. Classification of acetabular deficiencies (AAOS)
A segmental defect (Type I) is a loss of cortical bone in the supporting hemisphere or a segmental defect of the medial wall. However, there should be no volumetric bone stock loss. In most cases with this type of defect, a superior rim defect is seen as in patients with DDH ().
Figure 4. Technique of acetabular solid grafting: (A) Graft is fixated with two cancellous lag screws with its sclerotic convex side toward the defect as an inlay graft. (B) Reaming of the graft to prepare for a cemented socket. (C) Final situation before cementation and insertion of the acetabular component.
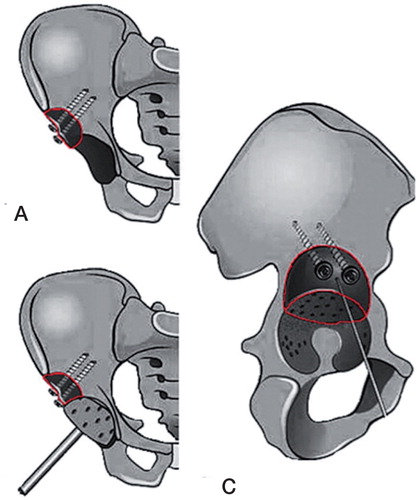
Several authors advocate the restoration of the centre of hip rotation (CitationLinde et al. 1988, CitationYoder et al. 1988, CitationPagnano et al. 1996, CitationStans et al. 1998). If reconstruction with a standard cup is considered in a dysplastic hip, reconstruction of the superolateral rim is mandatory. A frequently reported option is the use of solid grafts with a cemented cup as described by CitationWolfgang (1990) and modified by Lida et al. (2000). Using this technique, the centre of rotation is restored and a standard acetabular implant can be used ().
Comparison of grafting (32 cases) versus nongrafting (48 cases) of severe acetabular defects in a series of 64 patients showed higher survival rates for the grafted cases (CitationGarcía-Cimbrelo et al. 1993).
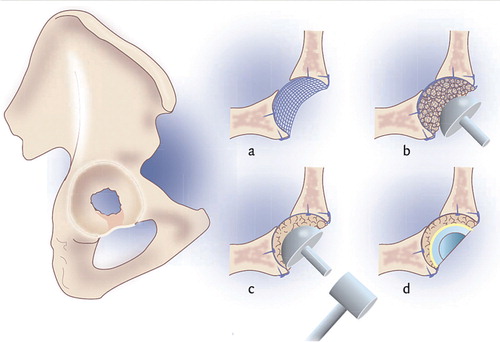
Impaction bone grafting () with reconstruction of the rim using a mesh is a technique which was introduced and described by CitationSlooff et al. (1984).
Figure 5. Technique of acetabular impaction bone grafting: (a) after localisation of the defect a mesh is situated and fixated using screws; (b) the contained defect is now filled with bone graft; (c) the grafts are impacted with a hammer and (d) a cemented cup is inserted.
Survival of 84% at 15 years was reported in a series of 28 acetabular reconstructions in patients with DDH (CitationSomford et al. 2008). Other surgeons prefer to use a reinforcement ring to achieve stability and good results have been reported (CitationGill et al. 1998, CitationPitto et al. 2004, CitationSiebenrock et al. 2005, CitationSadri et al. 2008). Based on the reported radiographic signs of loosening, long-term survival might be a problem in the future (CitationPitto et al. 2004, CitationSadri et al. 2008).
Medial wall defects are rarely seen in isolation but protrusion acetabuli can result in this isolated defect. It can be dealt with in several ways and probably the easiest way is to use an uncemented cup, especially those designs that are based on the principle of side-ingrowth. A disadvantage is that the deficient bone stock is not restored, which can make future revisions complicated. Bone grafting is a more biological approach; both structural grafting (CitationMcCollum et al. 1980) and impaction grafting techniques (CitationSlooff et al. 1984) have proven to be successful, including in patients with acetabular protrusion because of rheumatoid arthritis (CitationRosenberg et al. 2000). Restoration of the original hip centre of rotation is also advocated in patients with acetabular protrusion (CitationBaghdadi et al. 2013, CitationEcker et al. 2013).
A cavitary defect (Type II) consists of a volumetric bone loss of the acetabular cavity while the rim and medial wall remain intact. This is a frequently encountered condition, both in primary and revision hip surgery.
Filling the acetabular cavitary defect with bone cement should be reserved for elderly patients, as high failure rates have been reported for using only cement (CitationSalvati et al. 1975, CitationRanawat et al. 1980) and the use of additional bone grafts has been recommended.
Techniques using bone grafts to reinforce the medial wall have been described (CitationMcCollum et al. 1980, CitationHeywood 1980, CitationHirst et al. 1987) with good results after a mean follow-up of 4 (range 3–9) years for cemented as well as uncemented cups (CitationEbert et al. 1992). Unfortunately, reports of this technique with longer follow-up are lacking. Impaction bone grafting as described above offers another durable solution (CitationSlooff et al. 1984).
Most acetabular defects are combined segmental/cavitary defects (Type III). Treatment is based on 1 of the techniques described above or a combination of them.
In case of pelvic discontinuity (type IV), a rare condition, there is total separation of the superior and inferior part of the acetabulum. As described in a review on the treatment of pelvic discontinuity (CitationVillanueva et al. 2008), the main issues are healing the discontinuity and restoration of bone stock. Depending on the potential for healing, treatment should consist of plating the posterior column in combination with structural grafts or trabecular metal/cages. Custom-made implants can also be used, with or without additional allografts. Clear guidelines on the best type of implant or allograft are lacking because large series of patients treated for this condition are not available.
Treatment of patients with hip osteoarthritis and the related costs are a financial burden for society (CitationRäsänen et al. 2007, CitationJenkins et al. 2013) and if possible, length of hospital stay and costs should be minimised (CitationIbrahim et al. 2013). In addition to the fact that long-term survival is of great importance for the individual patient, the financial impact for society could be limited if only implants with a known long-term survival are used. A recent study on data of the National Joint Registry shows that a possible cost saving to the NHS of more than £18 million per year can be made if cemented instead of cementless hip designs were to be used in England and Wales (CitationGriffiths et al. 2012). As revision surgery of the hip is expensive compared to primary THA (CitationVanhegan et al. 2012), we should choose our primary implants based on the available evidence. Currently, choices of implants are mainly based on the preferences of the surgeon or the tradition of an institute. Better insight in associated costs of implants and revision surgery will result in better use of financial resources.
Questions addressed in this thesis are:
How many hip arthroplasties are performed in young patients in the Netherlands and which types of hip prosthesis are most commonly used?
What is the outcome of cemented THA in patients under 30 years?
What are the radiographic and clinical results of acetabular impaction bone grafting in patients younger than 50 years at long-term follow-up?
What is the outcome of acetabular solid grafting in DDH-patients?
What are the radiographic and clinical results of uncemented THA in patients younger than 50 years?
Are the hip implant-choices for young patients in the Netherlands evidence-based?
What is the most cost-effective treatment of a young patient in need for a THA on the long-term?
Methods and findings
Question 1. How many hip arthroplasties are performed in young patients in the Netherlands and which types of hip prosthesis are most commonly used ?
We have used data of the Dutch Arthroplasty Register to present the details of hip designs currently used in the Netherlands. The Dutch Arthroplasty Register started in 2007 and contains the registration of all primary and revision hip and knee replacements performed in the Netherlands. The number of THAs performed in 1980 was 6,750. This number has risen to 16,000 in 1994 and to more than 24,000 in 2012.
The distribution of the different types of hip designs for patients of all ages used in the Netherlands in 2012 is shown in . Uncemented implants account for more than 62% of all registered primary THAs in patients of all ages.
Figure 6. Fixation method of total registered number of 24,595 primary THAs in patients of all ages in the Netherlands in 2012.
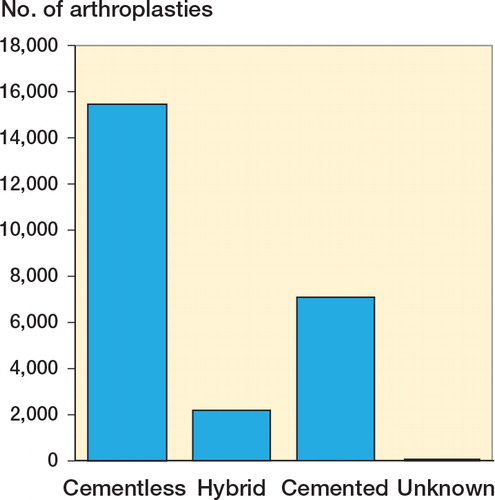
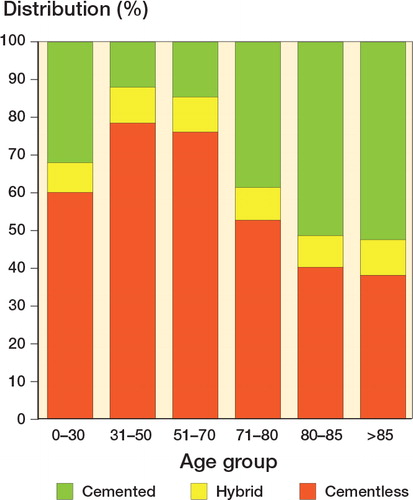
shows the method of fixation distributed per age group. In patients older than 85 at the time of their surgery, 38% were uncemented THAs. In patients younger than 50 years, uncemented implants were used in more than 78% of cases.
Figure 7. Method of fixation per age group in the Netherlands in 2012. Redrawn from source data LROI - graphics LROI-Dashboard in ProMISe accessed December 2013.
A standard definition of a “young patient” is lacking in literature and the term has been used for different age groups of patients, as explained in the Introduction. This is illustrated by observing the indications for THA in the different age groups. shows the primary diagnosis of patients receiving a THA in 2012. In patients of all ages, more than 87% received a THA because of primary osteoarthritis. A diagnosis as dysplasia for example counted only for 1.9%.
Table 2. Primary diagnosis of patients receiving a THA in 2012. Source data LROI accessed December 2013. Values are percentages
In patients younger than 50 years at the time of surgery, primary osteoarthritis counted for 62.2% of cases. Dysplasia counted for 12.9% of cases.
In patients younger than 30 years at the time of their THA, only 27% had primary osteoarthritis as the diagnosis; almost 18% had dysplasia of the hip. Secondary osteoarthritis accounted for 73.1% of 78 registered THAs.
Question 2. What is the outcome of cemented THA in patients under 30 years?
This study (paper 1) shows the outcome of 48 patients (69 THAs) younger than 30 years who had a primary cemented THA performed between 1988 and 2004. The indications were mainly osteonecrosis of the femoral head (21 cases) and juvenile rheumatoid arthritis (18 cases). All patients suffered from an underlying disease, except for 3 patients, whose diagnosis was unknown. 19 hips had previous surgeries at the hip. The study group consisted of 32 females (46 hips) and 16 males (23 hips) with a mean age at operation of 24.6 (16–29) years. No patient was lost to follow-up but 3 patients with 4 THAs had died.
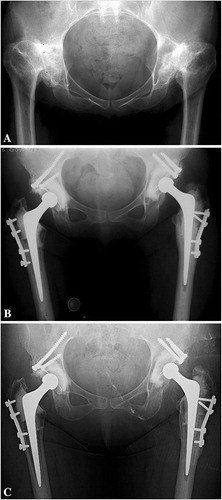
A posterolateral approach was used in all hips without a trochanteric osteotomy. Acetabular defects were classified as a Type I defect in 5 hips, a Type II defect in 16 hips and a Type III defect in 8 hips. A metal mesh was used in 14 hips to reconstruct a segmental defect. The remaining cavitary defect was reconstructed with bone impaction grafting in 29 cases. Cemented THA was performed using second-generation cementing technique in all cases ().
Figure 8. A. A preoperative radiograph of a 29-year-old woman with bilateral secondary osteoarthritis due to Bechterew’s disease. B. The hips after bilateral cemented THA with acetabular impaction bone grafting of a cavitary defect. C. At 17 and 18 years after the reconstruction there was incorporation of the bone graft and no signs of loosening except for an acetabular radiolucent line at the right hip in zone III.
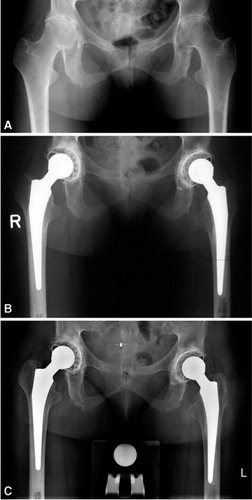
The mean Harris Hip Score (HHS) of the 57 surviving THAs in 37 living patients was 89 (55–100) and the mean Oxford Hip Questionnaire Score (OHQS) was 19 (12–42) after a mean follow-up of 8.4 (2–18) years. 8 hips were revised after a mean follow-up of 8.4 (2–18) years: 3 for infection and 5 for aseptic loosening. 1 additional cup was considered a radiographic failure.
Survival was 83% with revision for any reason and 90% with revision for aseptic loosening as the end point after 10 years of follow-up.
Question 3. What are the radiographic and clinical results of acetabular impaction bone grafting in patients younger than 50 years?
Acetabular defects are often seen in young patients with secondary osteoarthritis of the hip and several treatment options exist. In papers 2 and 3, we have investigated whether impaction bone grafting in combination with a cemented cup to reconstruct acetabular defects is a durable long-term solution. We studied 42 consecutive acetabular reconstructions in 37 patients younger than 50 years old (average 37.2 years) at the time of operation. 23 primary and 19 revision operations had been performed. The mean follow-up was 23 (20–28) years and at final review one patient was lost to follow-up and 8 patients (10 hips) had died. 16 cups had been revised, 2 because of septic loosening and 8 because of aseptic loosening. Another 4 cups had been revised because of wear and osteolysis and 2 cups during a stem revision but these were found to be well-fixed. Of the 19 hips in 17 patients with the implant still in situ (), 12 cups appeared to be well-fixed with uniform radiodensity of the graft and the host bone and without progressive radiolucent lines. 3 cups were considered loose radiographically.
Figure 9. Radiographs of acetabular reconstruction using impaction bone grafting with a mesh covering the graft; at the right the incorporation of the graft can be seen at 16 years of follow-up
Survival of the acetabular reconstructions, with end point revision for any reason, was 73% after 20 years and 52% after 25 years. With revision for aseptic loosening as the end point, survival was 85% after 20 years and 77% after 25; for signs of loosening on radiographs, survival was 71% at 20 years and 62% at 25 years.
Question 4. What is the outcome of solid grafting of the acetabulum in DDH-patients?
Socket fixation in patients with acetabular dysplasia can be technically demanding. Most surgeons try to restore the centre of hip rotation and in most cases this is possible with a standard cup. In the more severe cases however, bone stock may not be sufficient to support a standard cup, which makes reconstruction of the acetabulum necessary. Structural or solid grafts can help to reconstruct the original centre of hip rotation and restore normal hip biomechanics. In this study (paper 4) we have described the results of 62 patients with DDH who had 74 cemented THAs with solid acetabular roof grafts according to the technique described in the introduction. Mean age at surgery was 45 (19–71) years and the mean follow-up was 10.4 (5–16) years. Patients with grafting had higher Oxford scores compared with the control group (p=0.04) but other scores were equal.
2 hips were revised for aseptic acetabular loosening and one hip for polyethylene wear. All grafts were incorporated and no additional radiographic loose cups were seen (). The survival rate at 10 years of follow-up for revision for any reason was 98% (95% CI: 92.5–100.0).
Figure 10. (A) Preoperative radiograph of a 55-year-old woman with bilateral DDH, classified as a Crowe III, Hartofilakidis C, and Edinburgh system A2 F3. (B) Postoperative radiograph showing bilateral reconstruction using roof grafts and a cemented Exeter THA after femoral shortening osteotomy. (C) Radiograph 15 years after the reconstruction showing incorporation of the roof grafts without evidence of loosening or resorption of the graft but signs of wear.
Question 5. What are the radiographic and clinical results of uncemented THA in patients younger than 50 years?
Currently, uncemented THA seems to be the most popular solution for young patients with degenerative hip disease. Good mid-term results using the Zweymüller Alloclassic total hip arthroplasty have been reported (Delaunay et al. 2001, CitationGarcia-Cimbrelo et al. 2003, CitationPospischill et al. 2005, CitationGrübl et al. 2006, CitationSuckel et al. 2009), but long-term outcomes in young patients are scarce (CitationReigstad et al. 2008). The aim of this study (paper 5) was to evaluate the clinical and radiological results of the Alloclassic Zweymüller stem in combination with the conical self-tapping cement-free (CSF) titanium threaded cup in patients younger than 50 years of age, with a follow-up of at least 15 years. In 5 different hospitals in the Netherlands we have identified 73 consecutive Zweymüller total hip arthroplasties in 67 patients with a mean age of 43 (23–49) years and a mean follow-up of 17.5 (15–21) years. 3 patients (3 hips) had died and an additional 7 patients (8 hips) without any reoperation had no radiographic follow-up. 3 hips had been revised for septic loosening, one for a periprosthetic fracture and 3 cups for aseptic loosening. The mean HHS was 90 (52–100) and the mean Oxford Score was 22 (14–43). Of the 66 unrevised hips, follow-up radiographs were complete for 55 hips at final review (). 3 cups of the unrevised hips were considered loose. Osteolysis was seen at acetabular zone 2 and 3 in 3 cases.
Figure 11. Radiograph of a Zweymüller stem (type Hochgezogen) with the CSF cup in a 69-year old man more than 21 years after the index operation with no evidence of loosening but showing polyethylene wear.

Survival with an end-point of revision for any reason was 89% (95% CI: 85–93) and of revision for aseptic loosening was 94% (95% CI: 95–99) at 17 years. In a worst-case scenario for the cup where radiological failures were included and patients without a recent radiograph were considered failures, the survival rate was 84% (95% CI: 81–87) at 17 years.
Question 6. Are the implant-choices for young patients in The Netherlands evidence-based?
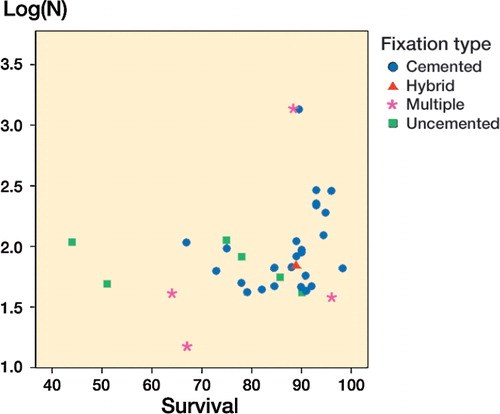
As many types of THAs exist to treat young patients with degenerative hip disease, we have reviewed the available literature on this topic to determine the optimal treatment (paper 6). We examined all reported outcomes of uncemented and cemented total hip arthroplasty in patients younger than 50 years of age listed in Medline between 1966 and 2009 as well as those mentioned in PubMed. In addition we scrutinised the reference lists of relevant papers and evaluated relevant data of the Swedish Hip Arthroplasty Register. Inclusion criteria were as follows: primary total hip arthroplasty, age at index surgery younger than 50 years and a minimal mean follow-up of 10 years. We have identified 109 relevant articles of which 37 had a mean follow-up longer than 10 years. At the time of this study only 1 report, based on uncemented custom made implants, fulfilled the criteria of survival by 90% at the 10-year follow-up, as recommended by the National Institute for Clinical Excellence (NICE). Cemented implants have been in use for a longer period with many studies meeting the survival criteria.
At the time of this study, data of the Swedish Hip Arthroplasty Register in 2007 show that survivorship of both cemented and uncemented implants is under 90% at 10 years. At 16 years, implant survival of cemented THAs in males was 75% and 73% in females. Implant survival of uncemented THAs was 57% in males and 54% in females. The highest survival rates of THA in young patients were related to cemented implants.
A scatter plot of all studies with a follow-up longer than 10 years with any survival rate was created (). 23 studies covering 3759 patients with cemented THA and 7 studies of uncemented THA covering 372 patients were included. A weighted regression analysis showed significantly better survival of cemented THA compared to uncemented THA: 88% versus 75% (p< 0.001).
Question 7. What is the most cost-effective treatment of a young patient in need for a THA on the long-term?
We have chosen to give an extended summary of this study with the main methods and findings, because this is an unpublished paper. In case the reader would like to obtain more details, additional information can be obtained on request.
Total hip arthroplasty has proven to be a very cost-effective procedure in older patients (CitationEthgen et al. 2004, CitationRäsänen et al. 2007) but young patients often outlive their implant. Particularly in these young patients, we need techniques and hip prostheses with a favourable long-term outcome as they are at great risk for revision. The outcome of both primary and revision surgery plays an important role in the cost-effectiveness of treatment of these patients. Clearly, the cup is the weakest link of THA (CitationNorwegian Arthroplasty register 2010, CitationDe Kam et al. 2011). Young patients with hip osteoarthritis often have acetabular bone stock defects at their primary surgery due to underlying diseases, which may hamper the longevity of the cup even more. Uncemented hip designs have gained worldwide popularity and are the first choice of treatment in young patients at the moment, also in case of acetabular defects. Impaction bone grafting in combination with a cemented cup is another treatment option for these young patients (CitationSlooff et al. 1984) in which the deficient acetabular bone stock is restored. Excellent long-term survival data of this technique are reported (CitationSchreurs et al. 2001, CitationGarcia-Cimbrelo et al. 2010, CitationBusch et al. 2011, Citationde Kam et al. 2011) including long-term data of revision cases (CitationComba et al. 2009, CitationSchreurs et al. 2009, Citationvan Egmond et al. 2011). However, this technique is time-consuming and is technically more demanding. In this study (paper 7) we determined the cost-effectiveness of acetabular impaction bone grafting and a cemented cup compared to the use of uncemented cup designs without grafting.
We have designed a decision model () to determine the cost-effectiveness of acetabular impaction bone grafting. The model has 2 modalities for the young patient in need for a THA with an acetabular defect: a cemented cup with acetabular impaction bone grafting versus an uncemented cup. The branching points thereafter represent transition to a different health state (survival, post revision THA, post revision THA II, post revision THA III and death). The model has cycles of 1 year to estimate QALYs and costs accumulating over a time period of 15 years. We have expressed our findings in terms of costs, quality-adjusted life years (QALYs) and incremental costs per QALY gained.
Figure 13. Markov model with cycles of 1 year to estimate QALYs and costs accumulating over a time period of 15 years.
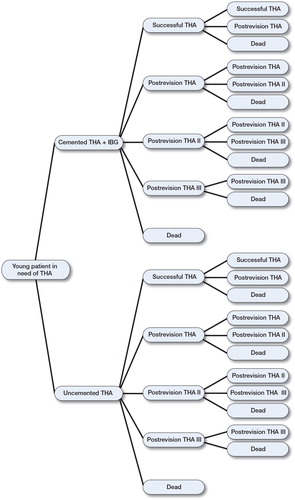
Overall, through our model we considered a hypothetical population aged 37 years or older in need for a hip replacement. As we were interested in long-term results of both techniques, we have incorporated survival of 3 revision surgeries with accompanying costs. Our model took into account the uncertainty around several input parameter point estimates. Survival data of cemented cups with impaction bone grafting were based on paper 3 (CitationBusch et al. 2011).
Survival at 15 years was 84% with failure for all reasons as the endpoint. For the first revision in our model, we have used survival data of 62 acetabular revisions in 58 patients with a mean age of 59 (23–82) years (CitationSchreurs et al. 2009). Survival at 15 years was 84% with failure for all reasons as end point.
For the uncemented option in the model, data were obtained from the Norwegian Arthroplasty Register. Unpublished data of 1289 patients younger than 50 years with primary hip osteoarthritis, who had received an uncemented cup, were analyzed and survival rates were determined. The most commonly used cups were Trilogy (Zimmer), Tropic (Landos), Duraloc (DePuy) and Reflection uncemented (Smith&Nephew). The probability of survival of primary uncemented cups was 61% at 15 years. Survival of the first uncemented cup revision was based on 76 patients and was 52% at 15 years. As survival rates of the cup solely were not available for the second revision, we used the same data for both cemented and uncemented revisions as presented by CitationLie et al. (2004), with a survival rate of 60% at 10 years.
The costs of an intervention consisted of material costs, costs of operation theatre and costs of hospital admission. Material costs are based on costs of a total cemented or total uncemented hip arthroplasty. For calculation of costs of the cemented option with acetabular impaction bone grafting, we used data of 79 most recently operated patients younger than 50 years in the period 2007–2010 at the Radboud UMC in the Netherlands. Costs of the uncemented option were calculated as if they were performed at the Radboud UMC. We have averaged the registered prices of 3 very commonly used uncemented total hip designs in the Netherlands. The mean operation time of cemented hip arthroplasty using impaction bone grafting was 123 minutes and we assumed that an uncemented hip arthroplasty at our hospital would take 40 minutes less (20 minutes for the impaction bone grafting procedure, two times 10 minutes for cementation). This assumption was made for both primary and revision operations. The costs of all revisions were assumed to be equal. The mean duration of hospital admission for a cemented hip arthroplasty using impaction bone grafting at Radboud UMC was 7.2 days. We assumed that the length of stay in hospital of patients with an uncemented hip arthroplasty was 5 days. Hospital admission time was set at ten days for all revision cases. Multiple sensitivity analysis was used to assess the contribution of the variables included in the model’s outcome.
We found that a cemented cup with impaction bone grafting is more cost-effective compared to the uncemented option, in terms of costs per QALY ().
Figure 14. Incremental cost-effectiveness plane showing 2 scenario’s. In the baseline scenario (black dots), almost 90% of the simulated ICERs lay in the southeast quadrant meaning that cemented with grafting is more cost-effective than the uncemented option. The second scenario with equal survival rates for both options (red dots) still shows an effect gain (higher QALY) for cemented with grafting but at higher costs.
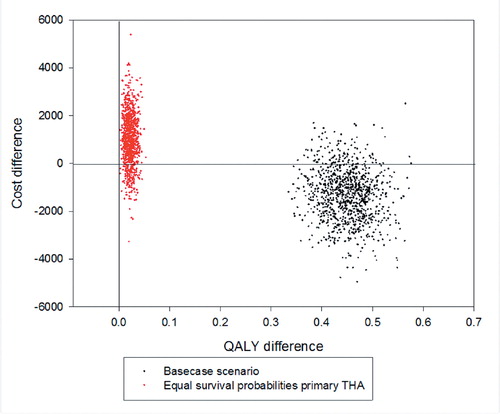
A second scenario suggesting equal primary survival rates of both cemented and cementless cups continues to show an effect gain for the cemented cup but at a higher cost. So, patients still have a rise in QALY’s on the long term but at higher costs compared to an uncemented cup.
General discussion
The aim of this thesis is to determine the clinical outcome of THA in young patients and how to deal with acetabular defects. In this General discussion we will discuss our findings.
Question 1. How many hip arthroplasties are performed in young patients in the Netherlands and which types of hip prosthesis are most commonly used?
The data of the Dutch Arthroplasty Register show us that around 5% of all patients receiving a THA were younger than 50 years at the time of operation and more than 75% of all hip replacements in these young patients were uncemented designs.
This trend is not restricted to the Netherlands. Also in other countries, the use of uncemented hip implants has increased over the years. The National Joint Registry of England and Wales reported that of all procedures in 2005, 22% were uncemented designs whereas in 2011 this figure had grown to 41% in patients of all ages (National Joint Registry England and Wales, CitationAnnual Report of 2012, page 65, Figure 2.3). In patients younger than 50 years, uncemented hip replacements accounted for approximately 64% of females and 60% of males. These rates were approximately 16% in females and 12% in males for cemented hip designs. The remaining 20% of females and 28% of males in this age group received a hybrid construction of resurfacing hip prosthesis.
The Swedish Hip Arthroplasty Register has also shown a slight increase in the use of uncemented implants, but cemented implants are still used for more than 80% of cases, regardless of the patient’s age (Swedish Hip Arthroplasty Register, Report of 2011). Between 1992 and 2011, a shift towards the use of uncemented implants and hybrid constructions can be seen in the younger age group.
In Norway, reversed hybrid constructions with a cemented acetabulum and an uncemented stem have been performed more frequently in the age group under 60 years (The Norwegian Arthroplasty Register, Report of 2010).
In general, we can conclude that it is an international trend to use uncemented hip designs and components in young patients. In later studies we will discuss whether this trend is in agreement with clinical evidence.
Question 2. What is the outcome of cemented THA in patients under 30 years?
Degenerative cartilage disease of the hip in very young patients is often secondary to an underlying disease as confirmed by data of the Dutch Arthroplasty Register. The purpose of this study was to determine the clinical and radiological results of cemented hip designs in patients younger than 30 years and evaluate the current state of patients who underwent a revision operation. Survival was 83% with revision for any reason and 90% with revision for aseptic loosening as the end point after 10 years of follow-up. Especially in young patients, we need techniques and implants with a proven long-term survival (CitationMcAuley et al. 2004) and apart from series of patients with exclusively juvenile chronic arthritis (CitationMaric and Haynes 1993, CitationChmell et al. 1997, CitationKumar et al. 1998, CitationOdent et al. 2005, CitationKitsoulis et al. 2006), there is limited literature regarding the survivorship and complications of THA surgery in patients younger than 30 years (CitationHalley and Charnley 1975, CitationChandler et al.1981, CitationSevert et al. 1991, CitationCage et al. 1992, CitationTorchia et al. 1996, CitationSochart and Porter 1998, CitationDudkiewicz et al. 2003). For the acetabular side, CitationTorchia et al. (1996) reported a revision rate for the cemented acetabular component of 43% at an average followup of 12.6 years. CitationSochart and Porter (1998) reported an acetabular rate of revision for cemented cups of 30% at a mean followup of 20 years. CitationMaric and Haynes (1993) described a group of 17 hips, including four uncemented hips, and reported that 6% of the acetabular components were revised after an average followup of 9.3 years. We found a rate of revision of 11.6% for the acetabular component at a mean followup of 8.4 years. We included in our data all patients that underwent revision and found reasonable functional scores except in one case. This study had a relatively large group (26%) of patients with juvenile rheumatoid arthritis. These patients are probably less active compared to the other patients with a localized osteoarthritis of the hip in our series (CitationChandler et al.1981, CitationSevert et al. 1991). In the literature, not all studies have the same conclusion regarding the outcome of THA in patients with rheumatoid arthritis. Some studies reported even worse outcome of this subgroup relative to other plain osteoarthritic cases (CitationChmell et al. 1997, CitationSechriest et al. 2007). In this series of patients younger than 30 years of age, cemented THA shows a 10-year survival rate of 83% with revision for any reason as the end point.
Question 3. What are the radiographic and clinical results of acetabular impaction bone grafting in patients younger than 50 years?
In paper 2 and 3, we have presented the results of acetabular reconstructions using impaction bone grafting in patients younger than 50 years. With end point revision for any reason, survival was 73% after 20 years and 52% after 25 years. Impaction bone grafting is a well-known technique described by CitationSlooff et al. (1984). The original technique was described in combination with cemented THA. Acetabular grafting in combination with uncemented cups is more common nowadays but long-term reports on uncemented cups with bone grafting in young patients are lacking in the literature. However, good mid-term results have been presented in older patients. CitationRudelli et al. (2009) showed a survival rate of 88% of uncemented cups, with an end point revision for any reason, after a mean follow-up of 14 years in a group of 42 patients (43 THAs) with a mean age at surgery of 56 years. Palm et al. (2011) reported a 9-year survival rate of the cup of 90.5% in a group of 79 patients in whom the median age was 67 years. CitationLachiewicz and Poon (1998) have reported the results of 34 patients in whom morselized bone grafts had been used in combination with a Harris-Galante porous-coated cup, and no revision because of loosening had taken place after a mean follow-up of 7 years. Although these are good and promising mid-term results, longer follow-up is needed to demonstrate the true clinical value of these uncemented techniques in young patients.
Pelvic osteolysis, which is seen at a higher frequency around uncemented components, is still an unsolved problem in young patients. In a series by CitationDella Valle et al.(2009), very acceptable results were achieved with use of a porous-coated acetabular component, but osteolysis was observed in more than 30% of patients who were younger than 50 years.
The technique of acetabular reconstruction using impaction bone grafting has basically remained the same over the years, with only minor changes. In the first years, a metal mesh was placed on top of the impacted bone grafts just before cementation. After one decade, it was realized that this mesh was not very functional, so a metal mesh is now used only to reconstruct segmental defects. In addition, the rehabilitation program has been changed. Depending on the size of reconstruction, patients are now mobilized earlier with earlier weight-bearing.
Over time, the results of cemented cups with acetabular impaction bone grafting have deteriorated. However, this study is one of the few worldwide available describing results of THA in young patients with a mean follow-up of 23 years. Impaction bone grafting with a cemented cup is a useful technique to restore bone stock in young patients whose acetabular defects require primary or revision total hip arthroplasty.
Question 4. What is the outcome of solid grafting of the acetabulum in DDH-patients?
In paper 4 we have presented the results of acetabular solid grafting with a cemented cup in a series of patients with DDH. The survival rate at 10 years of follow-up for revision for any reason was 98% (95% CI: 92.5–100). All grafts were incorporated and no additional radiographic loose cups were seen. Using solid grafts is a common technique to reconstruct an acetabular defect but reported survival rates differ considerably in literature ().
Table 3. Overview of literature a of acetabular bulk grafts in patients with DDH with a mean follow-up of 10 years or longer
The outcome of the present study is comparable to those studies that present high survival rates of this technique. We did not observe extensive acetabular osteolysis with cemented socket fixation, which is a well-reported observation around cementless cups (CitationBruzzone et al. 2009, CitationDella Valle et al. 2009). The use of an all-polyethylene cup enables the use of thicker polyethylene in these patients who all have small acetabula; this may further reduce the incidence of polyethylene wear. Wear-induced osteolysis increases the risk of failure and compromises bone stock for future revision surgery.
The treatment protocol at the Royal Infirmary in Edinburgh for dysplastic hips consists of reconstruction of a deficient acetabular roof of more than 20% using a solid graft from the femoral head with a cemented THA. Our data suggest this is a biologically reasonable approach, resulting in restoration of bone stock in these relatively young patients. Although some authors recommend avoiding structural bone graft if possible (CitationIto et al. 2003), bulk grafts for reconstruction of acetabular defects provide additional value for future revisions (CitationBal et al. 1999). The technique was originally described by CitationWolfgang (1990), has been further described by CitationIida et al. (2000), and has been performed in the same way throughout this study. A wedge of the femoral head is taken and fixed with 2 cancellous screws with its sclerotic convex side towards the defect as an inlay graft ( in the Introduction). In the early years, 3 cancellous screws were used for fixation but we believe 2 screws are sufficient.
Question 5. What are the radiographic and clinical results of uncemented THA in patients younger than 50 years?
Paper 5 describes the results of 73 uncemented Zweymüller total hip arthroplasties in 67 patients younger than 50 years. Survival with an end-point of revision for any reason was 89% (95% CI 85–93) after 17 years of follow-up. A worst-case scenario was simulated in which radiological failures and missing patients were considered failures, the survival rate was 84% (95% CI: 81–87) at 17 years. This compares favourably to other reported survival rates of uncemented cups in young patients. CitationAldinger et al. (2009) showed high survival rates of a grit blasted femoral component, but low survival rates (38% and 68% at 17 years) of 2 types of smooth-surface threaded cups which are now no longer in use. It seems that porous-coating of a threaded cup to promote bony in-growth is essential to achieve stability and higher survival rates at longer follow-up. A study of 83 cementless Zweymüller Alloclassic stems with a 28 mm metal-on-metal bearing in 73 young, active patients showed excellent results (CitationDelaunay et al. 2008). Only patients with high activity levels were selected for review; patients with severe dysplasia and rheumatoid arthritis were excluded. 3 different acetabular components had been used of which 24 were titanium threaded. This series of patients showed a 10-year survival rate of 100% (CI: 89.6–100).
CitationEskelinen et al. (2006) concluded in a nationwide study on THA in patients younger than 55 years that survival rates of uncemented cups are unsatisfactorily low when liner exchanges are taken into account. We acknowledge the fact that many types of uncemented hip designs are available which makes comparison between groups of implants difficult. In our series of patients younger than 50 years at the time of operation, high survival rates were achieved at 17 years of follow-up.
Question 6. Are the implant-choices for young patients in The Netherlands evidence-based?
As we have shown before, uncemented hip designs are currently the most popular option to treat young patients with degenerative hip disease. In paper 6, we showed the results of a literature review on this topic to determine whether this choice is based on evidence. At the time of this study, only one report on uncemented hip designs fulfilled the criteria of survival by 90% at 10 year follow-up, as recommended by the National Institute for Clinical Excellence (NICE). Cemented implants have been in use for a longer period with many studies meeting the survival criteria. A confusing factor in assessing studies of uncemented hips is that revision of a failed insert of an uncemented acetabular metal shell has not always been reported as a revision. Not all studies report this exchange as a revision, which can make it difficult to compare survival rates of different studies. Cup survival with an endpoint of revision of the metal shell at 14 years is 70%, but including liner exchange it is 54% (CitationCapello et al. 2003).
A critical note concerning the survival rates as reported by national registries could be that many different types of uncemented hip designs have been gathered and the poorer outcome of those implants with an inferior survival may obscure the outcome of those designs with a better performance. This study concluded that the highest survival rates were related to cemented implants; thus the current trend to use uncemented implants has not yet been supported by the available literature. This conclusion is supported by other reports (CitationMorshed et al. 2007).
If we observe survival rates of acetabular and femoral components separately in literature, there seems to be evidence that uncemented stems perform at least as well as cemented stems (CitationEskelinen et al. 2006). As we have stated before, the weakest link of the reconstruction is the cup (Norwegian Arthroplasty register).
A more recent study (Pederson et al. 2014) based on large numbers of implants in patients younger than 55 years of age seems to show that uncemented implants perform better in relation to long-term risk of aseptic loosening. However, more short-term revisions were necessary because of problems due to dislocation, periprosthetic fracture and infections.
Question 7. What is the most cost-effective treatment of a young patient in need for a THA on the long-term?
As we were interested in the cost-effectiveness of acetabular impaction grafting to treat the bone deficient osteoarthritic hip in a young patient, we have designed a model comparing 2 modalities: a cemented cup with grafting versus an uncemented cup (paper 7). It shows that on the longer term, impaction bone grafting with a cemented cup is more cost-effective than the use of an uncemented cup. As described above, the current trend to use uncemented cups in young patients seems not to be supported in literature. Regarding costs, a recent study on data of the National Joint Registry shows that a possible cost saving to the NHS of more than 18 million pounds per year can be made if cemented instead of uncemented hip designs were used in England and Wales (CitationGriffiths et al. 2012). Another recent study on cost-effectiveness of different types of total hip replacements in older patients concludes that uncemented prostheses do not improve health outcomes sufficiently to justify their higher costs (CitationPennington et al. 2013). These studies confirm our findings in the way that uncemented hip designs are less cost-effective compared to cemented total hip prostheses.
A strength of our study is that in our model we acknowledge the fact that the technique of impaction bone grafting takes additional time and materials and we have included these costs in our model. We also have incorporated three revisions with accompanying costs in our model and we have used advanced statistical software (TreeAge pro Suite 2009) to construct our model. A point of criticism on our study could be that the survival rates of primary uncemented cups are worse than the rates of cemented cups. However, these numbers were derived from the reliable Norwegian Arthroplasty Register and constitute a consecutive series of young patients treated with uncemented cups. We are aware of the fact that our study is based on hip designs used several years ago and that nowadays articulations with highly cross-linked polyethylene are more commonly used than conventional polyethylene. However, long term results of uncemented cups with highly cross-linked polyethylene are not available. To overcome criticism on these limitations in our model, we have explored a second scenario in which the survival rates of primary uncemented cups are made equal to primary cemented cups with impaction bone grafting. In this scenario, an effect gain for a cemented cup with impaction bone grafting was still seen, but at higher costs. So, even with equal survival rates for both acetabular options, reconstruction of an acetabular defect with impaction bone grafting and a cemented cup seems to be beneficial on the long term.
Another limitation of our study might be that costs of treatments and materials may differ between hospitals and that some hospitals may have arranged lower prices. We realise this could be a limitation in applying the conclusions of this study to other hospitals. Nevertheless, costs were calculated as if all prostheses were placed in our hospital without any discounts, to have a baseline comparator of the 2 techniques. The advantage of this model is that the input can be updated with new information in the future.
We have optimized the parameters of the uncemented option by not taking into account any additional material costs for dealing with bone defects or periprosthetic fractures, which are more common using uncemented designs or at uncemented revision operations. Also the estimation of length of stay is in favour of uncemented hip arthroplasty. Besides this, we have compared survival data of cemented cups in difficult cases with acetabular defects to data of uncemented cups without the need for acetabular reconstruction, which might be of positive influence on the outcome of the uncemented treatment. Even using these data, cemented hip arthroplasty with impaction bone grafting is still more cost-effective than the uncemented option in young patients.
Cost effectiveness analysis of orthopaedic treatments may be a helpful tool in clinical decision-making for hospitals and health policy makers. In the present study, cemented cups with acetabular impaction bone grafting were more cost-effective than uncemented cups in terms of costs per QALY for the young patient in need for a hip replacement with an acetabular defect.
Conclusion
Several options are available for treatment of the young patient with degenerative hip disease, but what the most durable solution is remains controversial. This thesis shows that good long-term results can be reached with both cemented and uncemented hip designs. However, to date the majority of papers with high survival rates are based on cemented hip designs. Although the initial outcome of our uncemented study is impressive, there is no information about the outcome of revisions. The debate whether cemented or uncemented THA would be the most durable solution for young patients is also blurred by the fact that results for many different hip designs have been gathered and evaluated as a group. Because we had to base our conclusion on the available literature we had to conclude that, in general, the cemented THA in young patients seems to be the most durable solution for young patients. Perhaps time is the only factor to show us otherwise.
Many different types of hip prostheses are currently used for young patients in the Netherlands. Recently, the Dutch Orthopaedic Association published a list of approved hip designs, classified according to their survival rates known from international registries (e.g. the Swedish Hip Arthroplasty Register) and available literature. We would like to plea for further standardization in the use of only well-performing hip designs in Dutch hospitals, especially in younger patients. In addition, concentration of treatment of “complex hips” by specialised surgeons enables them to build expertise in this field and this might optimize Dutch orthopaedic care for young patients with degenerative hip disease.
With regard to acetabular defects in young patients, we can conclude that it appears that a biological reconstruction is the most durable option as these patients probably face a second or third operation. Reconstruction using grafts, whether solid or morselized, is the preferred method, in combination with a cemented cup. From an economical point of view, reconstruction using impaction bone grafting and a cemented cup is more cost-effective compared to a primary uncemented cup. We hope that the outcome of this thesis will play a role in decision making by hospitals and orthopaedic surgeons when choosing the most durable hip prosthesis for the osteoarthritic hip in young patients.
References
- Akiyama H, Kawanabe K, Iida H, Haile P, Goto K, Nakamura T. Long-term results of cemented total hip arthroplasty in developmental dysplasia with acetabular bulk bone grafts after improving operative techniques. J Arthroplasty 2010; 25: 716-20.
- Aldinger PR, Jung AW, Breusch SJ, Ewerbeck V, Parsch D. Survival of the cementless Spotorno stem in the second decade. Clin Orthop Rel Res 2009; (467): 2297-304.
- Baghdadi YM, Larson AN, Sierra RJ. Restoration of the hip center during THA performed for protrusio acetabuli is associated with better implant survival. Clin Orthop Relat Res 2013; 471(10): 3251-9.
- Bal BS, Maurer T, Harris WH. Revision of the acetabular component without cement after a previous acetabular reconstruction with use of a bulk femoral head graft in patients who had congenital dislocation or dysplasia. A follow-up note. J Bone Joint Surg (Am) 1999; 81(12): 1703-6.
- Bobak P, Wroblewski BM, Siney PD, Fleming PA, Hall R. Charnley low-friction arthroplasty with an autograft of the femoral head for developmental dysplasia of the hip. The 10-to 15year results. J Bone Joint Surg (Br) 2000; 82: 508–11.
- Biemond JE, Pakvis DF, van Hellemondt GG, Buma P. Long-term survivorship analysis of the cementless Spotorno femoral component in patients less than 50 years of age. J Arthroplasty 2011; 26(3): 386-90.
- Bruzzone M, La Russa M, Garzaro G, Ferro A, Rossi P, Castoldi F, Rossi R. Long-term results of cementless anatomic total hip replacement in dysplastic hips. Chir Organi Mov 2009; 93: 131–6.
- Busch VJ, Gardeniers JW, Verdonschot N, Slooff TJ, Schreurs BW. Acetabular reconstruction with impaction bone-grafting and a cemented cup in patients younger than fifty years old: a concise follow-up, at twenty to twenty-eight years, of a previous report. J Bone Joint Surg (Am) 2011; 93:367-71.
- Cage DJ, Granberry WM, Tullos HS. Long-term results of total arthroplasty in adolescents with debilitating polyarthropathy. Clin Orthop Relat Res 1992; (283): 156–62.
- Capello WN, D’Antonio JA, Feinberg JR, Manley MT. Ten year results with hydroxyapatite-coated total hip femoral components in patients less than fifty years old. A concise follow-up of a previous report. J Bone Joint Surg (Am) 2003; 85:885-9.
- Case CP, Langkamer VG, James C, Palmer MR, Kemp AJ, Heap PF, et al.Widespread dissemination of metal debris from implants. J Bone Joint Surg (Br) 1994; 76:701-12.
- Chandler HP, Reineck FT, Wixson RL, McCarthy JC. Total hip replacement in patients younger than thirty years old: a five-year follow-up study. J Bone Joint Surg (Am) 1981; 63:1426-34.
- Charnley J. Arthroplasty of the hip. A new operation. Lancet 1961; 1 (7187):1129-32.
- Childs LM, Goater JJ, O’Keefe RJ, Schwartz EM. Effect of anti-tumor necrosis factor-α gene therapy on wear debris-induced osteolysis. J. Bone Joint Surg (Am) 2001; 83-A:1790-7.
- Chmell MJ, Scott RD, Thomas WH, Sledge CB. Total hip arthroplasty with cement for juvenile rheumatoid arthritis: results at a minimum of ten years in patients less than thirty years old. J Bone Joint Surg (Am) 1997; 79: 44–52.
- Comba F, Buttaro M, Pusso R, Piccaluga F. Acetabular revision surgery with impacted bone allografts and cemented cups in patients younger than 55 years. Int Orthop 2009; 33(3): 611-6.
- van Egmond N, De Kam DC, Gardeniers JW, Schreurs BW. Revisions of extensive acetabular defects with impaction grafting and a cement cup. Clin Orthop Relat Res 2011; 469(2): 562-73.
- D’Antonio JA, Capello WN, Borden LS, Bargar WL, Bierbaum BF, Boettcher WG, Steinberg ME, Stulberg SD, Wedge JH. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res 1989; 243:126-37.
- Data obtained from the database of the Dutch Arthroplasty Register. Obtained December 2013.
- de Jong de PT, Haverkamp D, van der Vis HM, Marti RK. Total hip replacement with a superolateral bone graft for osteoarthritis secondary to dysplasia: a long-term follow-up. J Bone Joint Surg (Br) 2006; 88: 173–178.
- de Kam DC, Gardeniers JW, Hendriks JC, Veth RP, Schreurs BW. Cemented polyethylene cups in patients younger than 40 years. Clin Orthop Relat Res 2009; 467(7): 1753-64.
- Delaunay CP, Bonnomet F, Clavert P, Laffargue P, Migaud H. THA using metal-on-metal articulation in active patients younger than 50 years. Clin Orthop Relat Res 2008; 466(2): 340-6.
- Della Valle CJ, Mesko NW, Quigley L, Rosenberg AG, Jacobs JJ, Galante JO. Primary total hip arthroplasty with a porous-coated acetabular component. A concise follow-up, at a minimum of twenty years, of previous reports. J Bone Joint Surg (Am) 2009; 91(5): 1130-5.
- Dorey FJ. Survivorship analysis of surgical treatment of the hip in young patients. Clin Orthop Relat Res 2004; 418:23-8.
- Dudkiewicz I, Salai M, Israeli A, Amit Y, Chechick A. Total hip arthroplasty in patients younger than 30 years of age. Isr Med Assoc J 2003; 5: 709-12.
- Ebert FR, Hussain S, Krackow KA. Total hip arthroplasty for protrusio acetabuli: a 3- to 9-year follow up of the Heywood technique. Orthopedics 1992; 15(1): 17-20.
- Ecker ML. CORR Insights®: Restoration of the hip center during THA performed for protrusio acetabuli is associated with better implant survival. Clin Orthop Relat Res 2013; 471(10): 3260-1.
- Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop 2006; 77: 57-70.
- Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Joint Surg (Am) 2004; 86: 963–974
- Garcia-Cimbrelo E, Cruz-Pardos A, Garcia-Rey E, Ortega-Chamarro J. The survival and fate of acetabular reconstruction with impaction grafting for large defects. Clin Orthop Relat Res 2010 Dec; 468(12): 3304-13
- Garcia-Cimbrelo E, Cruz-Pardos A, Madero R, Ortega-Andreu M. Total hip arthroplasty with use of the cementless Zweymüller Alloclassic system. A ten to thirteen-year followup study. J Bone Joint Surg (Am) 2003; 85: 296-303.
- García-Cimbrelo E, Munuera L. Low-friction arthroplasty in severe acetabular dysplasia. J Arthroplasty 1993; 8(5): 459-69.
- Gill TJ, Sledge JB, Müller ME. Total hip arthroplasty with use of an acetabular reinforcement ring in patients who have congenital dysplasia of the hip. Results at five to fifteen years. J Bone Joint Surg (Am) 1998; 80(7): 969-79.
- Griffiths EJ, Stevenson D, Porteous MJ. Cost savings of using a cemented total hip replacement: an analysis of the National Joint Registry data. J Bone Joint Surg (Br) 2012; 94(8): 1032-5.
- Grübl A, Chiari C, Giurea A, et al.Cementless total hip arthroplasty with the rectangular titanium Zweymuller stem. A concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg (Am) 2006; 88: 2210-5.
- Guidance on the selection of prostheses for primary total hip replacement. NICE 2003.
- Hailer NP, Garellick G, Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop 2010; 81(1): 34-41.
- Halley DK, Charnley J. Results of low friction arthroplasty in patients thirty years of age or younger. Clin Orthop Relat Res 1975; 112: 180–191.
- Harris WH. Osteolysis and particle disease in hip replacement. A review. Acta Orthop Scand 1994; 65: 113-23.
- Hendrich C, Mehling I. Cementless acetabular reconstruction and structural bone-grafting in dysplastic hips. J Bone Joint Surg (Am) 2006; 88: 387-94.
- Heywood AW. Arthroplasty with a solid bone graft for protrusio acetabuli. J Bone Joint Surg (Br) 1980; 62(3): 332-6.
- Hirst P, Esser M, Murphy JC, Hardinge K. Bone grafting for protrusio acetabuli during total hip replacement. A review of the Wrightington method in 61 hips. J Bone Joint Surg (Br) 1987; 69(2): 229-33.
- Howie DW, Holubowycz OT, MiddletonR. Large Articulation Study Group. Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg (Am) 2012; 94(12): 1095-102.
- Ibrahim MS, Khan MA, Nizam I, Haddad FS. Peri-operative interventions producing better functional outcomes and enhanced recovery following total hip and knee arthroplasty: an evidence-based review. BMC Med 2013; 11(1): 37.
- Iida H, Matsusue Y, Kawanabe K, Okumura H, Yamamuro T, Nakamura T. Cemented total hip arthroplasty with acetabular bone graft for developmental dysplasia. Long-term results and survivorship analysis. J Bone Joint Surg (Br) 2000; 82(2): 176-84.
- Ikeda T, Takahashi K, Kabata T, Sakagoshi D, Tomita K, Yamada M. Polyneuropathy caused by cobalt-chromium metallosis after total hip replacement. Muscle Nerve 2010; 42(1): 140-3.
- Inao S, Matsuno T. Cemented total hip arthroplasty with autogenous acetabular bone grafting for hips with developmental dysplasia in adults: the results at a minimum of ten years. J Bone Joint Surg (Br) 2000; 82: 375–377.
- Ingham E, Fisher J. Biological reactions to wear debris in total joint replacement. Proc. Instn. Mech. Engrs. 2000, Part H, J. Engin. in Medicine 214, 21–37.
- Ito H, Matsuno T, Minami A, Aoki Y. Intermediate-term results after hybrid total hip arthroplasty for the treatment of dysplastic hips. J Bone Joint Surg (Am) 2003; 85: 1725-32.
- Jenkins PJ, Clement ND, Hamilton DF, Gaston P, Patton JT, Howie CR. Predicting the cost-effectiveness of total hip and knee replacement: A health economic analysis. J Bone Joint (Br) 2013; 95-B(1): 115-21.
- Kim M, Kadowaki T. High long-term survival of bulk femoral head autograft for acetabular reconstruction in cementless THA for developmental hip dysplasia. Clin Orthop Relat Res. 2010; 468: 1611–1620.
- Kim YH, Kim JS, Park JW, Joo JH. Comparison of total hip replacement with and without cement in patients younger than 50 years of age: the results at 18 years. J Bone Joint Surg (Br) 2011; 93(4): 449-55.
- Kim YH, Kim JS, Park JW, JooJH. Periacetabular osteolysis is the problem in contemporary total hip arthroplasty in young patients. J Arthroplasty 2012; 27(1): 74-81.
- Kitsoulis PB, Stafilas KS, Siamopoulou A, Soucacos PN, Xenakis TA. Total hip arthroplasty in children with juvenile chronic arthritis: long-term results. J Pediatr Orthop 2006; 26: 8-12.
- Kobayashi S, Eftekhar NS, Terayama K, Joshi RP. Comparative study of total hip arthroplasty between younger and older patients. Clin Orthop Relat Res 1997; (339): 140-51.
- Kobayashi S, Saito N, Nawata M, Horiuchi H, Iorio R, Takaoka K. Total hip arthroplasty with bulk femoral head autograft for acetabular reconstruction in developmental dysplasia of the hip. J Bone Joint Surg (Am) 2003; 85: 615–621.
- Kumar MN, Swann M. Uncemented total hip arthroplasty in young patients with juvenile chronic arthritis. Ann R Coll Surg Engl 1998; 80(3): 203–9.
- Labek G, Stöckl B, Janda W, et al. Quality of datasets for outcome measurement of artificial joint implants. 2009. European Arthroplasty Register, EFORT. Available at http: //www.ear.efort.org/downloads/EBOOKQualityofDatasetsfinal.pdf. Accessed December 2014
- Lachiewicz PF, Poon ED. Revision of a total hip arthroplasty with a Harris-Galante porous-coated acetabular component inserted without cement. A follow-up note on the results at five to twelve years. J Bone Joint Surg (Am) 1998; 80: 980-4.
- Ladon D, Doherty A, Newson R, Turner J, Bhamra M, Case CP. Changes in metal levels and chromosome aberrations in the peripheral blood of patients after metal-on-metal hip arthroplasty. J Arthroplasty 2004; 19: 78–83
- Langton DJ, Jameson SS, Joyce TJ, Gandhi JN, Sidaginamale R, Mereddy P, Lord J, Nargol AV . Accelerating failure rate of the ASR total hip replacement. J Bone Joint Surg Br 2011; 93(8): 1011-6.
- Le Duff MJ, Amstutz HC. The relationship of sporting activity and implant survivorship after hip resurfacing. J Bone Joint Surg (Am) 2012; 94(10): 911-8.
- Lee BP, Cabanela ME, Wallrichs SL, Ilstrup DM. Bone-graft augmentation for acetabular de.ciencies in total hip arthroplasty: results of long-term follow-up evaluation. J Arthroplasty 1997; 12: 503-10.
- Lidgren L. Chronic inflammation, joint replacement and malignant lymphoma. J Bone Joint Surg (Br) 2008; 90: 7-10.
- Lie SA, Havelin LI, Furnes ON, Engesaeter LB, Vollset SE. Failure rates for 4762 revision total hip arthroplasties in the Norwegian Arthroplasty Register. J Bone Joint Surg Br 2004; 86: 504-9.
- Linde F, Jensen J, Pilgaard S. Charnley arthroplasty in osteoarthritis secondary to congenital dislocation or subluxation. Clin Orthop Relat Res 1988; (227): 164-71.
- Maric Z, Haynes RJ. Total hip arthroplasty in juvenile rheumatoid arthritis. Clin Orthop Relat Res 1993; (290): 197-9.
- McAuley JP, Szuszczewicz ES, Young A, Engh CASr. Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res 2004; 418: 119-25.
- McCollum DE, Nunley JA, HarrelsonJM. Bone-grafting in total hip replacement for acetabular protrusion. J Bone Joint Surg (Am) 1980; 62(7): 1065-73.
- Meftah M, Klingenstein GG, Yun RJ, Ranawat AS, Ranawat CS. Long-term performance of ceramic and metal femoral heads on conventional polyethylene in young and active patients: a matched-pair analysis. J Bone Joint Surg (Am) 2013; 95(13): 1193-7.
- Morshed S, Bozic KJ, Ries MD, Malchau H, Colford J MJr. Comparison of cemented and uncemented fixation in total hip replacement: a meta-analysis. Acta Orthop 2007; 78(3): 315-26.
- Mulroy R DJr, Harris WH. Failure of acetabular autogenous grafts in total hip arthroplasty. Increasing incidence: a follow-up note. J Bone Joint Surg (Am) 1990; 72: 1536-40.
- National Joint Registry England and Wales. Annual Report of 2012. Available at www.njrcentre.org.uk
- Norwegian Arthroplasty Register, Report of 2010. Available at http: //nrlweb.ihelse.net/eng/Report_2010.pdf
- Odent T, Journeau P, Prieur AM, Touzet P, Pouliquen JC, Glorion C. Cementless hip arthroplasty in juvenile idiopathic arthritis. J Pediatr Orthop. 2005; 25: 465–470.
- Oldenburg M, Wegner R, Baur X. Severe cobalt intoxication due to prosthesis wear in repeated total hip arthroplasty. J Arthroplasty 2009; 24(5): 825.e15-e20.
- Pagnano MW, Hanssen AD, Lewallen DG, Shaughnessy WJ. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty: long-term results of patients who have Crowe type II congenital dysplasia of the hip. J Bone Joint Surg (Am) 1996; 78: 1004-14.
- Palm L, Jacobsson SA, Kvist J, Lindholm A, Ojersjo A, Ivarsson I. Acetabular revision with extensive allograft impaction and uncemented hydroxyapatite-coated implants. Results after 9 (7-11) years follow-up. J Arthroplasty 2007; 22: 1083-91.
- Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, Ostlere S, Athanasou N, Gill HS, Murray DW. Pseudotumours associated with metal-on- metal hip resurfacings. J Bone Joint Surg (Br) 2008; 90: 847–51.
- Pedersen AB, Mehnert F, Havelin LI, Furnes O, Herberts P, Kärrholm J, Garellick G, Mäkela K, Eskelinen A, Overgaard S. Association between fixation technique and revision risk in total hip arthroplasty patients younger than 55 years of age. Results from the Nordic Arthroplasty Register Association. Osteoarthritis Cartilage 2014; 22(5): 659-67.
- Pennington M, Grieve R, Sekhon JS, Gregg P, Black N, van der Meulen JH. Cemented, cementless, and hybrid prostheses for total hip replacement: cost effectiveness analysis. BMJ 2013; 346: f1026.
- Penny JØ, Ovesen O, Varmarken JE, Overgaard S. Similar range of motion and function after resurfacing large-head or standard total hip arthroplasty. Acta Orthop 2013; 84(3): 246-53.
- Pieringer H, Auersperg V, Griessler W, Böhler N. Long-term results with the cementless Alloclassic brand hip arthroplasty system. J Arthroplasty 2003; 18: 321-8.
- Pitto RP, Schikora N. Acetabular reconstruction in developmental hip dysplasia using reinforcement ring with a hook. Int Orthop 2004; 28: 202–5.
- Pospischill M, Knahr K. Cementless total hip arthroplasty using a threaded cup and a rectangular tapered stem. Followup for ten to 17 years. J Bone Joint Surg (Br) 2005; 87: 1210-5.
- Ranawat CS, Dorr LD, Inglis AE. Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J Bone Joint Surg (Am) 1980; 62-A,1059-65.
- Räsänen P, Paavolainen P, Sintonen H, Koivisto AM, Blom M, Ryynänen OP, Roine RP. Effectiveness of hip or knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthop 2007; 78: 108-15.
- Reigstad O, Siewers P, Røkkum M, Espehaug B. Excellent long-term survival of an uncemented press-fit stem and screw cup in young patients: follow-up of 75 hips for 15-18 years. Acta Orthop 2008; 79: 194-202.
- Rodriguez JA, Huk OL, Pellicci PM, Wilson P DJr. Autogenous bone grafts from the femoral head for the treatment of acetabular de.ciency in primary total hip arthroplasty with cement: long-term results. J Bone Joint Surg Am 1995; 77: 1227-33.
- Rosenberg WW, Schreurs BW, de Waal Malefijt MC, Veth RP, Slooff TJ. Impacted morsellized bone grafting and cemented primary total hip arthroplasty for acetabular protrusion in patients with rheumatoid arthritis: an 8- to 18-year follow-up study of 36 hips. Acta Orthop Scand 2000; 71(2): 143-6.
- Rudelli S, Honda E, Viriato SP, Libano G, Leite LF. Acetabular revision with bone graft and cementless cup. J Arthroplasty 2009; 24: 432-43.
- Sadri H, Pfander G, Siebenrock KA, Tannast M, Koch P, Fujita H, Ballmer P, Ganz R. Acetabular reinforcement ring in primary total hip arthroplasty: a minimum 10-year follow-up. Arch Orthop Trauma Surg.2008; 128(8): 869-77.
- Salvati EA, Bullough P, Wilson PD. Intrapelvic protrusion of the acetabular component following total hip replacement. Clin Orthop Rel Res 1975; 111: 212-27.
- Schmalzried TP, Huk OL. Patient factors and wear in total hip arthroplasty. Clin Orthop Relat Res 2004; 418: 94-97.
- Severt R, Wood R, Cracchiolo AIII, Amstutz HC. Long-term follow-up of cemented total hip arthroplasty in rheumatoid arthritis. Clin Orthop Relat Res 1991; 265: 137-45.
- Schreurs BW, GardeniersJW. Results of 3,668 primary total hip replacements. Acta Orthop 2012; 83(2): 204.
- Schreurs BW, Keurentjes JC, Gardeniers JW, Verdonschot N, Slooff TJ, Veth RP. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented acetabular component: a 20- to 25-year follow-up. J Bone Joint Surg (Br) 2009; 91: 1148-53.
- Schreurs BW, Slooff TJ, Gardeniers JW, Buma P. Acetabular reconstruction with bone impaction grafting and a cemented cup: 20 years’ experience. Clin Orthop Relat Res 2001; 393: 202-15.
- Sechriest VF2nd, Kyle RF, Marek DJ, Spates JD, Saleh KJ, Kuskowski M. Activity level in young patients with primary total hip arthroplasty: a 5-year minimum follow-up. J Arthroplasty 2007; 22: 39-47.
- Severt R, Wood R, Cracchiolo AIII, Amstutz HC. Long-term follow-up of cemented total hip arthroplasty in rheumatoid arthritis. Clin Orthop Relat Res 1991; 265: 137-45.
- Shetty AA, Sharma P, Singh S, Tindall A, Kumar SV, Rand C. Bulk femoral-head autografting in uncemented total hip arthroplasty for acetabular dysplasia: results at 8 to 11 years follow-up. J Arthroplasty 2004; 19: 706-13.
- Shinar AA, Harris WH. Bulk structural autogenous grafts and allografts for reconstruction of the acetabulum in total hip arthroplasty. Sixteen-year-average follow-up. J Bone Joint Surg (Am) 1997; 79: 159-68.
- Siebenrock KA, Tannast M, Kim S, Morgenstern W, Ganz R. Acetabular reconstruction using a roof reinforcement ring with hook for total hip arthroplasty in developmental dysplasia of the hip-osteoarthritis minimum 10-year follow-up results. J Arthroplasty 2005; 20(4): 492-8.
- Slooff TJ, Huiskes R, van Horn J, Lemmens AJ. Bone grafting in total hip replacement for acetabular protrusion. Acta Orthop Scand 1984; 55: 593-6.
- Sochart DH, Porter ML. Long-term results of cemented Charnley low-friction arthroplasty in patients aged less than 30 years. J Arthroplasty. 1998; 13: 123-31.
- Somford MP, Bolder SB, Gardeniers JW, Slooff TJ, Schreurs BW. Favorable survival of acetabular reconstruction with bone impaction grafting in dysplastic hips. Clin Orthop Relat Res 2008; 466: 359-65.
- Stans AA, Pagnano MW, Shaughnessy WJ, Hanssen AD. Results of total hip arthroplasty for Crowe Type III developmental hip dysplasia. Clin Orthop Relat Res 1998; 348: 149-57.
- Stringa G, Pitto RP, Di Muria GV, Marcucci M. Total hip replacement with bone grafting using the removed femoral head in severe acetabular dysplasia. Int Orthop 1995; 19: 72-6.
- Stroh DA, Issa K, Johnson AJ, Delanois RE, Mont MA. Reduced dislocation rates and excellent functional outcomes with large-diameter femoral heads. J Arthroplasty 2013; 28(8): 1415-20.
- Suckel A, Geiger F, Kinzl L, Wulker N, Garbrecht M. Longterm results for the uncemented Zweymuller/Alloclassic hip endoprosthesis. A 15-year minimum follow-up of 320 hip operations. J Arthroplasty 2009; 24: 846-53.
- Swedish hip register, Annual Report 2010, page 16. Available at http: //www.shpr.se/Libraries/Documents/AnnualReport-2010-2-eng.sflb.ashx. Accessed December 2014
- Swedish Hip Arthroplasty Register, Report of 2011. Available at http: //www.shpr.se/Files/Årsrapport%202011%20(eng)%20webb.pdf. Accessed December 2014
- Torchia ME, Klassen RA, Bianco AJ . Total hip arthroplasty with cement in patients less than twenty years old: long-term results. J Bone Joint Surg (Am) 1996; 78: 995-1003.
- Utting MR, Raghuvanshi M, Amirfeyz R, Blom AW, Learmonth ID, Bannister GC. The Harris-Galante porous-coated, hemispherical, polyethylene-lined acetabular component in patients under 50 years of age: a 12- to 16-year review. J Bone Joint Surg (Br) 2008; 90(11): 1422-7.
- Van der Weegen W, Smolders JM, Sijbesma T, Hoekstra HJ, BrakelK, van Susante JL. High incidence of pseudotumours after hip resurfacing even in low risk patients; results from an intensified MRI screening protocol. Hip Int 2013; 23(3): 243-9.
- Vanhegan IS, Malik AK, Jayakumar P, Ul Islam S, Haddad FS. A financial analysis of revision hip arthroplasty: the economic burden in relation to the national tariff. J Bone Joint Surg (Br) 2012; 94(5): 619-23.
- Vermes C, Chandrasekaran R, Jacobs JJ, Galante JO, Roebuck KA, Glant TT. The effects of particulate wear debris, cytokines, and growth factors on the functions of MG-63 osteoblasts. J. Bone Joint Surg (Am) 2001; 83-A:201-11.
- Villanueva M, Rios-Luna A, Pereiro De Lamo J, Fahandez-Saddi H, Böstrom MP. A review of the treatment of pelvic discontinuity. HSS J 2008; 4(2): 128-37.
- Website of MRHA, available at http: //www.mhra.gov.uk/home/groups/dts-bs/documents/medicaldevicealert/con155767.pdf
- Website of Dutch Orthopaedic Association (NOV), available at http: //www.orthopeden.org/uploads/zG/gl/zGglSTglo_X2M1TXrFiT1Q/Uitwerking-NOV-Advies-Metaal-Op-Metaal-3-juni-2012.pdf. Accessed December 2014
- Wolfgang GL. Femoral head autografting with total hip arthroplasty for lateral acetabular dysplasia. A 12-year experience. Clin Orthop Relat Res 1990; 225: 173-85.
- Yoder SA, Brand RA, Pederson DR, O’Gorman TW. Total hip acetabular component position affects acetabular loosening rates. Clin Orthop Relat Res 1988; 228: 79-87.