Abstract
Background and purpose — The local infiltration analgesia (LIA) technique has been widely used to reduce opioid requirements and to improve postoperative mobilization following total hip arthroplasty (THA). However, the evidence for the efficacy of LIA in THA is not yet clear. We determined whether single-shot LIA in addition to a multimodal analgesic regimen would reduce acute postoperative pain and opioid requirements after THA.
Patients and methods — 116 patients undergoing primary THA under spinal anesthesia were included in this randomized, double-blind, placebo-controlled trial. All patients received oral opioid-sparing multimodal analgesia: etoricoxib, acetaminophen, and glucocorticoid. The patients were randomized to receive either 150 mL ropivacaine (2 mg/mL) and 0.5 mL epinephrine (1 mg/mL) or 150 mL 0.9% saline. Rescue analgesic consisted of morphine and oxycodone as needed. The primary endpoint was pain during mobilization in the recovery unit. Secondary endpoints were pain during mobilization on the day after surgery and total postoperative opioid requirements on the first postoperative day.
Results — The levels of pain during mobilization—both in the recovery unit and on the day after surgery—and consumption of opioids on the first postoperative day were similar in the 2 groups.
Interpretation — LIA did not provide any extra analgesic effect after THA over and above that from the multimodal analgesic regimen used in this study.
Implementation of accelerated clinical pathways based on the fast-track principles reduces morbidity and enhances recovery for patients undergoing THA (CitationKehlet and Wilmore 2008). One of the key prerequisites is optimized pain relief, allowing early postoperative mobilization (CitationKehlet and Wilmore 2008). This requires that the pain treatment should be safe and effective, both at rest and during activity (CitationSrikandarajah and Gilron 2011).
The concept of multimodal analgesia for acute postoperative pain is to combine analgesics with additive or synergistic effects, which is meant to reduce the use of—and the adverse effects of—opioids and to allow early mobilization (CitationKehlet and Dahl 1993, CitationKehlet et al. 1999, CitationBuvanendran and Kroin 2009). Multimodal analgesia in THA usually includes analgesics such as opioids, gabapentin, NSAIDs, acetaminophen, glucocorticoids, and local infiltration (CitationKardash et al. 2008, CitationKerr and Kohan 2008, CitationToms et al. 2008, CitationFredheim et al. 2011, CitationMaund et al. 2011, CitationZhang et al. 2011).
CitationKerr and Kohan (2008) reported reduced opioid requirements and reduced hospital stay with the use of LIA consisting of ropivacaine and NSAIDs. However, trials investigating the effect of ropivacaine in LIA have not determined whether ropivacaine alone gives similar improvements following THA (CitationLunn et al. 2011, CitationDobie et al. 2012, CitationZoric et al. 2014). Studies using LIA have often combined different analgesics (CitationKerr and Kohan 2008, CitationKuchalik et al. 2013), and this complicates interpretation of the results regarding the extent to which ropivacaine alone contributes to the outcome.
Various studies have shown that LIA does not provide any additional analgesic benefit or reduce opioid consumption after THA (CitationLunn et al. 2011, CitationDobie et al. 2012, CitationSolovyova et al. 2013, CitationZoric et al. 2014), and some authors do not recommend LIA in addition to a multimodal analgesic regimen after THA (CitationAndersen et al. 2011, CitationLunn et al. 2011). Other studies have shown that LIA reduces the opioid consumption (CitationAndersen et al. 2007, CitationKerr and Kohan 2008, CitationBusch et al. 2010, CitationMurphy et al. 2012, CitationKuchalik et al. 2013) and shortens the hospital stay after THA (CitationKerr and Kohan 2008, CitationScott et al. 2012) The results are thus conflicting, and the role of LIA in THA surgery still needs to be clarified.
We investigated whether a single-shot LIA with ropivacaine in addition to a multimodal analgesic regimen would reduce acute postoperative pain and opioid requirements after THA.
Material and methods
Patients
Patients scheduled for elective primary THA in the orthopedic outpatient clinic of St. Olav’s Hospital in Trondheim were screened for inclusion in this study from March 2013 through March 2014. Preoperatively, the patients attended a patient educational seminar. All patients were included regardless of age, ASA score, or type of prosthesis. THA was performed with a standard direct lateral approach.
Exclusion criteria were contraindications to receive spinal anesthesia, dexamethasone, or acetaminophen. Patients who received general anesthesia and patients who were operated with an approach different to standard direct lateral one were excluded. Patients with osteosynthesis to be removed at the same operation were also excluded from this study.
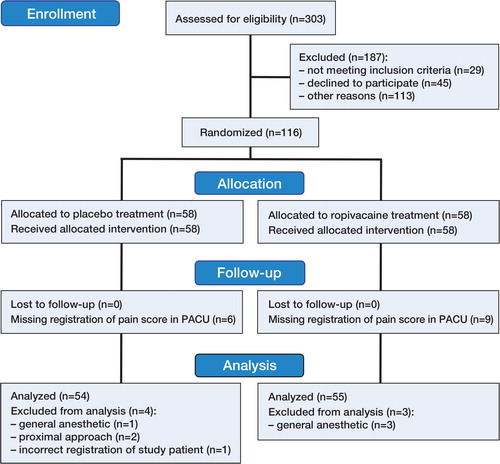
116 patients were included in the study. shows the flow of patients through the study, and the demographic data and baseline data are presented in .
Table 1. Baseline demographic of study patients
Randomization and blinding
This was a randomized, double-blind, placebo-controlled trial.The patients were randomized to receive either LIA or placebo. Randomization was done by the unit of Clinical Health Science at NTNU in Trondheim. Numbered, sealed envelopes were opened by the operating nurse on the day of surgery. The surgeon, the anesthesia personnel, the nursing staff, and the patients were all blind regarding patient allocation throughout the study.
Study intervention
All patients got a premedication cocktail consisting of dexamethasone (16–20 mg), etoricoxib (90 mg) and acetaminophen (1.5–2 g).
All patients were operated under spinal anesthesia with 2.0–3.0 mL bupivacaine, 0.5% plain, preferably at the L2/L3 or the L3/L4 vertebral interspace. Propofol infusion was administered for sedation if required. A standardized program for intraoperative fluid administration was followed, consisting of 1–1.5 L Ringer’s acetate, tranexamic acid (15 mg/kg, max. 1.5 g), and cephalothin (2 g).
The patients were randomized to receive either LIA or placebo. The LIA consisted of 150 mL ropivacaine (2 mg/mL) and 0.5 mL epinephrine (1 mg/mL), not including ketorolac, as described by CitationKerr and Kohan (2008). The other group received 150 mL 0.9% saline.
The solution was prepared in 3 unmarked 50-mL syringes by the operating nurse before the patient, the anesthetic personnel, and the surgeon arrived at the operating room.
Local infiltration analgesia or placebo was injected by the surgeon in a standardized manner (CitationKerr and Kohan 2008). The first 50 mL was injected in the periacetabular tissue after insertion of the acetabular component. After insertion of the femoral component, 50 mL was inserted in the gluteus muscles and the proximal part of the iliotibial tract. The last 50 mL was inserted in the subcutaneous layers.
The patients followed the standardized fast-track clinical pathway for hip and knee arthroplasty at Trondheim University Hospital (CitationWinther et al. 2014), and they were mobilized in the post-anesthesia care unit (PACU) as soon as the effect of the spinal anesthetic had worn off. At the PACU, morphine was given intravenously if required when the patients needed extra pain-reducing medicine.
Thereafter, the patients were transferred to a specialized hip arthroplasty unit with a well-defined and experienced program for multimodal rehabilitation. Multimodal orally administered opioid-sparing analgesia was given to all the patients; NSAIDS and acetaminophen were given at regular intervals and oxycodone was given if needed.
Study parameters
The primary endpoint in this study was pain sensation during mobilization in the PACU. The secondary endpoint was pain during mobilization on the day after surgery and total consumption of opioids on the first postoperative day.
Pain was registered using the numeric rating scale (NRS), by the nurses in the PACU and in the hip arthroplasty ward unit. The patients were asked a standard question: “On a scale from 0 to 10, where 0 is no pain and 10 is the worst imaginable pain, can you define the pain you have right now?”
Mobilization in the PACU consisted of sitting at the bed, and standing and walking a few steps at the bedside with assistance from the nurse. In addition, the patients were given physiotherapy in the hip arthroplasty ward unit.
Pain score was also examined at rest. In addition, the use of opioids, the number of hours mobilized, and the length of hospital stay were registered.
Statistics
The estimated sample size was based on pain score during mobilization in the PACU. With a mean pain score of 2.1 and an SD of 1.8 (known from our own registry data), a level of significance of 0.05%, and a power of 80%, a 1-point difference in NRS would be detected with 52 patients in each group.
The continuous numeric variables for pain scores and opioid consumption were tested for normality of distribution with the Kolmogorov-Smirnov test, histogram and QQ-plot.
The 2 groups were compared with the Mann-Whitney U-test, as the data were not normally distributed. Pain score and total consumption of opioids are therefore presented as median with interquartile range.
Both morphine and ketobemidone were given to the patients in the PACU. These opioids are considered to be equipotent (CitationRygnestad and Slordal 2000), and they were merged when the total consumption of opioids was calculated.
All statistical analyses were conducted with IBM SPSS version 21.
Ethics and registration
Written and verbal informed consent was obtained from each patient before inclusion in the study, and the study was conducted in accordance with the Declaration of Helsinki. The project was approved by the regional committees for medical and health research ethics (2012/1999). The study was registered at ClinicalTrials.gov (identifier NCT02359136).
Results
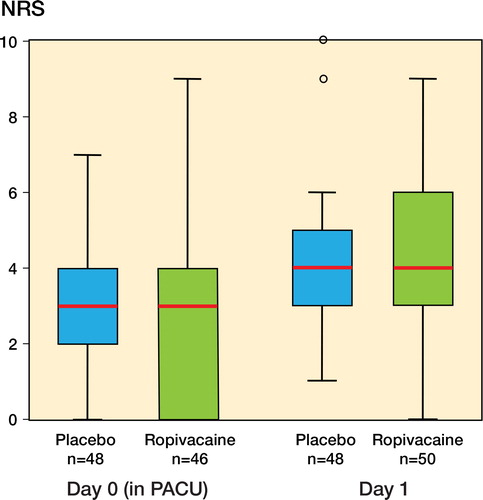
The median pain score during mobilization in the PACU was 3 in boths groups (p = 0.7). The median pain score during mobilization on the first postoperative day was 4 in both groups (p = 0.3) ().
Figure 2. Box plot showing pain score (NRS) during mobilization in the post-anesthesia care unit (PACU) and on the first postoperative day. The horizontal lines indicate median. The boxes represent interquartile range and the whiskers extend to the minimum or maximum case/value within 1.5 times the height of the boxes.
Median opioid consumption in the PACU was 0 (0–3.1) mg and 0 (0–5) mg in the placebo and the ropivacaine group respectively (p = 0.9) ().
Table 2. Results
Total oxycodone consumption on the first postoperative day was 20 (10–30) mg in both groups (p = 0.3) ().
Discussion
We found that LIA with 0.2% ropivacaine does not provide any analgesic effect after THA in addition to a multimodal analgesic regimen consisting of spinal anesthesia, NSAID, acetaminophen, and glucocorticoid. There was no statistically significant increase in pain score or consumption of opioids during mobilization in the PACU or on the day after surgery.
The widespread LIA technique was described by CitationKerr and Kohan (2008) to reduce opioid requirements and improve postoperative mobilization after THA. They added ketorolac to the ropivacaine and epinephrine mixture and the effect of LIA alone was therefore not studied. The authors found a low pain score—generally in the range of 0–3—both at rest and while walking, and reduced opioid consumption. Almost half of the patients were directly discharged home on the first postoperative day.
Using both NSAIDs and opioids in LIA is controversial, and few studies have attempted to identify which components in the mixture contribute to the outcome. Addition of NSAIDs to the LIA mixture without giving NSAIDs to the control group makes the results of the studies difficult to interpret (CitationAndersen et al. 2007, CitationKerr and Kohan 2008, CitationKuchalik et al. 2013, CitationSolovyova et al. 2013) as NSAIDs have both a systematic and a local anti-inflammatory effect (CitationRomsing et al. 2000). Instead of measuring the effect of the local infiltration analgesia, it may be the effect of NSAID(s) that is measured, which complicates the comparison between LIA and placebo.
Several trials investigating the effect of LIA following THA have used different pain treatment modalities such as spinal analgesic, epidural analgesic, or systematic analgesic. In addition, these are often used in combination with a LIA catheter placed intraoperatively giving repeated injections postoperatively (CitationAndersen et al. 2007, CitationKerr and Kohan 2008, CitationMurphy et al. 2012, CitationKuchalik et al. 2013, CitationSolovyova et al. 2013, CitationZoric et al. 2014). This further complicates interpretation and comparison of the results. In the present study, the patients received a single-shot local infiltration analgesic with ropivacain and epinephrine. NSAID was given as a part of a multimodal pain regimen. This makes the results of our study valid, as the only difference between the 2 groups was whether ropivacaine was administered.
A recent study with a similar design also had results comparable to ours. CitationLunn et al. (2011) reported that infiltration with a single dose of 150 mL 0.2% ropivacaine with epinephrine following THA did not reduce postoperative consumption of opioids or reduce postoperative pain (CitationLunn et al. 2011). In this study, they used a multimodal analgesic approach consisting of acetaminophen, NSAID, and gabapentin rather than the glucocorticoid used in our study (CitationLunn et al. 2011). Gabapentin has possible side effects such as dizziness and visual disturbances, and its use is debatable as part of a multimodal pain regimen following THA (CitationZhang et al. 2011).
A single preoperative dose of dexamethasone is a proven long-acting prophylactic agent for nausea and vomiting, and improves postoperative pain and mobilization (CitationKardash et al. 2008, CitationLunn and Kehlet 2013). A single dose of dexamethasone has no known side effects either in the short term or long term, apart from increased blood glucose level on the first postoperative day (CitationWaldron et al. 2013). There are no general recommendations for use of glucocorticoids following THA, and this suggests that further investigation is still required regarding dose-response and potential side effects.
Pain evoked by movement is often neglected as the primary clinical outcome following THA (CitationSrikandarajah and Gilron 2011). The fast-track methodology requires a procedure-specific pain regimen to allow early mobilization, and thereby reduce the length of convalescence and morbidity (CitationKehlet and Wilmore 2008). In the present study, the patients had low postoperative pain scores irrespective of which study group they belonged to, both at rest and during mobilization. This indicates that the multimodal pain regimen that we used was safe, simple, and satisfactory—and that the patient’s preoperative expectations were met through information and education (CitationHamilton et al. 2013).
Our findings may be limited by missing registration of pain scores for 15 study participants during mobilization in the PACU, i.e. the primary outcome of this study. Nevertheless, this was a randomized trial, and we consider that the number of patients registered had a sufficient response rate to give reliable results.
One strength of our study was that the patients allocated to this trial were unselected. Our findings can therefore be generalized to other populations when using a multimodal pain regimen like ours after THA.
In conclusion, local infiltration analgesic with ropivacaine did not provide any extra analgesic effect after THA over and above that from the multimodal analgesic regimen consisting of acetaminophen, NSAID, and glucocorticoid.
All the authors contributed substantially to planning of the study and drafting of the article. JKH and TSW wrote the article and conducted the study. TSW, OAF, JKH, and SBW conducted the data analyses and interpreted the results.
We thank the nursing staff who participated in collection of the registry data used in this study. Special thanks to the operating nurses in the orthopedic operating ward unit responsible for organizing and conducting the study intervention.
No competing interests declared.
- Andersen KV, Pfeiffer-Jensen M, Haraldsted V, Soballe K. Reduced hospital stay and narcotic consumption, and improved mobilization with local and intraarticular infiltration after hip arthroplasty: a randomized clinical trial of an intraarticular technique versus epidural infusion in 80 patients. Acta Orthop 2007; 78 (2): 180–6.
- Andersen LO, Otte KS, Husted H, Gaarn-Larsen L, Kristensen B, Kehlet H. High-volume infiltration analgesia in bilateral hip arthroplasty. A randomized, double-blind placebo-controlled trial. Acta Orthop 2011; 82 (4): 423–6.
- Busch CA, Whitehouse MR, Shore BJ, MacDonald SJ, McCalden RW, Bourne RB. The efficacy of periarticular multimodal drug infiltration in total hip arthroplasty. Clin Orthop Relat Res 2010; 468 (8): 2152–9.
- Buvanendran A, Kroin JS. Multimodal analgesia for controlling acute postoperative pain. Current opinion in anaesthesiology 2009; 22 (5): 588–93.
- Dobie I, Bennett D, Spence DJ, Murray JM, Beverland DE. Periarticular local anesthesia does not improve pain or mobility after THA. Clin Orthop Relat Res 2012; 470 (7): 1958–65.
- Fredheim OM, Borchgrevink PC, Kvarstein G. [Post-operative pain management in hospitals]. Tidsskr Nor Laegeforen 2011; 131 (18): 1772–6.
- Hamilton DF, Lane JV, Gaston P, Patton JT, MacDonald D, Simpson A H RW, et al. What determines patient satisfaction with surgery? A prospective cohort study of 4709 patients following total joint replacement. BMJ Open 2013; 3 (4).
- Kardash KJ, Sarrazin F, Tessler MJ, Velly AM. Single-dose dexamethasone reduces dynamic pain after total hip arthroplasty. Anesth Analg 2008; 106 (4): 1253–7.
- Kehlet H, Dahl JB. The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg 1993; 77 (5): 1048–56.
- Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 2008; 248 (2): 189–98.
- Kehlet H, Werner M, Perkins F. Balanced analgesia: what is it and what are its advantages in postoperative pain? Drugs 1999; 58 (5): 793–7.
- Kerr DR, Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. Acta Orthop 2008; 79 (2): 174–83.
- Kuchalik J, Granath B, Ljunggren A, Magnuson A, Lundin A, Gupta A. Postoperative pain relief after total hip arthroplasty: a randomized, double-blind comparison between intrathecal morphine and local infiltration analgesia. Br J Anaesth 2013; 111 (5): 793–9.
- Lunn TH, Kehlet H. Perioperative glucocorticoids in hip and knee surgery - benefit vs. harm? A review of randomized clinical trials. Acta Anaesthesiol Scand 2013; 57 (7): 823–34.
- Lunn TH, Husted H, Solgaard S, Kristensen BB, Otte KS, Kjersgaard AG, et al. Intraoperative local infiltration analgesia for early analgesia after total hip arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med 2011; 36 (5): 424–9.
- Maund E, McDaid C, Rice S, Wright K, Jenkins B, Woolacott N. Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs for the reduction in morphine-related side-effects after major surgery: a systematic review. Br J Anaesth 2011; 106 (3): 292–7.
- Murphy TP, Byrne DP, Curtin P, Baker JF, Mulhall KJ. Can a periarticular levobupivacaine injection reduce postoperative opiate consumption during primary hip arthroplasty? Clin Orthop Relat Res 2012; 470 (4): 1151–7.
- Romsing J, Moiniche S, Ostergaard D, Dahl JB. Local infiltration with NSAIDs for postoperative analgesia: evidence for a peripheral analgesic action. Acta Anaesthesiol Scand 2000; 44 (6): 672–83.
- Rygnestad T, Slordal L. [Morphine, pethidine or ketobemidone in acute pain--are there significant differences?]. Tidsskr Nor Laegeforen 2000; 120 (21): 2548–9.
- Scott CE, Streit J, Biant LC, Breusch SJ. Periarticular infiltration in total hip replacement: effect on heterotopic ossification, analgesic requirements and outcome. Arch Orthop Trauma Surg 2012; 132 (5): 703–9.
- Solovyova O, Lewis CG, Abrams JH, Grady-Benson J, Joyce ME, Schutzer SF, et al. Local infiltration analgesia followed by continuous infusion of local anesthetic solution for total hip arthroplasty: a prospective, randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am 2013; 95 (21): 1935–41.
- Srikandarajah S, Gilron I. Systematic review of movement-evoked pain versus pain at rest in postsurgical clinical trials and meta-analyses: a fundamental distinction requiring standardized measurement. Pain 2011; 152 (8): 1734–9.
- Toms L, McQuay HJ, Derry S, Moore RA. Single dose oral paracetamol (acetaminophen) for postoperative pain in adults. The Cochrane database of systematic reviews 2008; (4): CD004602.
- Waldron NH, Jones CA, Gan TJ, Allen TK, Habib AS. Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br J Anaesth 2013; 110 (2): 191–200.
- Winther SB, Foss OA, Wik TS, Davis SP, Engdal M, Jessen V, et al. 1-year follow-up of 920 hip and knee arthroplasty patients after implementing fast-track. Acta Orthop 2014: 1–8.
- Zhang J, Ho KY, Wang Y. Efficacy of pregabalin in acute postoperative pain: a meta-analysis. Br J Anaesth 2011; 106 (4): 454–62.
- Zoric L, Cuvillon P, Alonso S, Demattei C, Vialles N, Asencio G, et al. Single-shot intraoperative local anaesthetic infiltration does not reduce morphine consumption after total hip arthroplasty: a double-blinded placebo-controlled randomized study. Br J Anaesth 2014; 112 (4): 722–8.