Abstract
Purpose: Measurements play a vital role in providing devices that meet the individual needs of users. There is increasing evidence of devices being abandoned. The reasons for this are complex but one key factor that plays a role in non-use of equipment is the lack of fit between the device, environment and person. In addition, the abandonment of devices can be seen as a waste of public money. The aim of this paper is to examine the type, the readability, and the content of existing guidance in relation to measuring home furniture.
Method: An online national survey involving health and social care trusts in the UK. We conducted a synthesis of leaflets associated with measurement of furniture to identify existing guidance. The content and readability of this guidance was then evaluated.
Results: From the 325 responses received, 64 therapists reported using guidance. From the 13 leaflets that were analysed, 8 leaflets were found to meet Level 3 Adult Literacy Standards (age 9–11). There were differences in the way in which the measurement of furniture items occurred within the leaflets with no measurement guidance reported for baths.
Conclusion: There is a need to standardize guidance to ensure that measurements are reliable.
Our research has highlighted the need to confirm and agree measurement techniques for home furniture in the provision of assistive devices.
Inaccurate guidance can lead to abandonment of devices.
Inaccurate guidance could prevent service users from not participating within the self-assessment process for devices.
Implications for Rehabilitation
Introduction
Assistive devices are growing in importance within health and social care as they are thought to promote function independence [Citation1–3] increase self-efficacy [Citation4] and quality of life.[Citation5,Citation6] The devices market was valued at USD 12.37 billion in 2012 and is expected to reach an estimated value of USD 19.68 billion in 2019.[Citation7] This is hardly surprising since the use of devices increases with age.[Citation8,Citation9] In addition, there is evidence that the right prescription of assistive devices could deliver cost saving for health and social care providers.[Citation10–12] Nevertheless, despite the reported benefits, there appear to remain a number of barriers to the ensuring that assistive technology is successfully adopted and used. In fact, 29.3% of all devices are abandoned.[Citation13] These barriers can include lack of knowledge about the device, involvement in the process of selecting it, attitudes towards the technology and lack of fit of the assistive technology between service users and their environment.[Citation14] Interestingly, a Canadian study suggests that the medias views of older adults could lower the use of assistive devices.[Citation15] As a consequence, the service user’s independence is reduced and there are cost implications for the health and social care providers.[Citation16] One possible solution is collaborative shared decision-making and person-centred practice.[Citation17,Citation18]
Customization of measurements plays a vital role in order to ensure the successful fit of the assistive device to the person.[Citation19,Citation20] It is essential if the device is to match the needs of the person.[Citation21] If a device is to be customized it needs to be measured and assessed within the persons chosen environment since the actual dimensions of a piece of furniture can affect the individual’s ability to use it. For example, evidence suggests that when a chair seat is lower than knee height, a longer time is taken to rise from sit to stand, and an older occupant needs to use faster and larger trunk flexion movements.[Citation22,Citation23] In this case, a device such as a chair raiser can facilitate transfers in and out of a chair. Therapists and service users use measurements of furniture to ascertain the correct fitting of assistive devices to be provided. However, significant differences may occur between therapists and older adults’ perceptions in relation to the best height of a chair.[Citation24] One of the factors that play a role in this could be that the optimum seat height for ease of rising is not necessarily the same as the optimum seat height required for comfort. Therefore, seat height chosen to maximize the ease of rising may be slightly higher than that chosen for comfort.[Citation25] There may also be difference a between how service users and therapists take measurements, or in how measurements are taken among therapists. Nevertheless, currently no guides indicate how much of a difference would be clinically significant.[Citation26]
Therapists measure for assistive devices either by conducting a home visit with or without the patient.[Citation27] In clinical practice, it is also becoming common for family members or service users to measure key items of furniture on behalf of therapists because of time limitations.[Citation28] However, very little is known about the medium therapists use to facilitate the process of information exchange regarding taking measurements to ensure best fit of assistive devices. This is particularly important if service users want to self-assess for the provision of devices.
When service users feel informed, they are more likely to be satisfied with their devices, engage with them, and retain them.[Citation4] Written guidance could achieve the aim of informing patients, but both the content and lay out of guidance should empower service users to make informed decisions about their own care. If the guidance, however, does not adhere to recommended quality standards in relation to its content, layout and readability, then it may not result in the right decision being made by service users. Moreover, we do not know the extent to which written guidance facilitates the principles of shared decision making and empowerment. Within occupational therapy and physiotherapy little attention has been paid to the effect and quality of information guidance on professional practice.
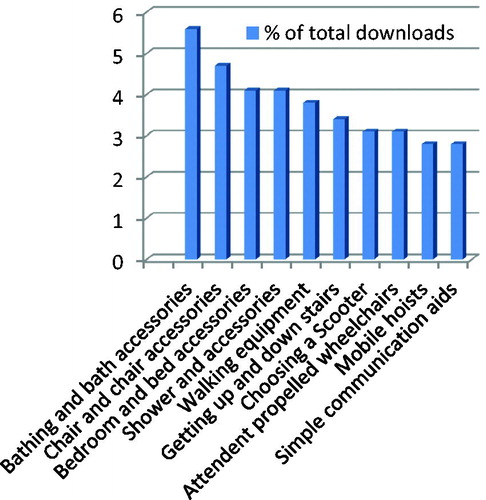
The overall goal of our research is to develop national guidance for services users to enable them to self-assess for provision of minor assistive devices that facilitate bed, chair, stairs, toilet and bath transfers. The pieces of furniture were chosen as they are the most frequently requested items for information by members of the public as recorded by the Disabled Living Foundation [UK] which is an independent consumer advice centre for provision of assistive technology (). Also, Williamson and Fried [Citation29] have shown that among 230 older adults, 14% had difficulty getting in or out of bed, 14% in or out of a chair and 13% ascending/descending stairs. The aim of this paper is to ascertain what guidance is currently available for measurement of home furniture and assess its readability and content.
Method
An online descriptive national survey involving health and social care settings in England was carried out to determine what guidance is currently available for measurement of home furniture and also to gather this guidance. An online search for documents using a Google search engine was also carried out to ascertain whether any guidance was available online. The keywords that were used for the online search were measurement, occupational therapy, furniture measurement, height (i.e., bed, chair, toilet, stairs and bath), home visit, measurement, hip fracture measurement in combinations.
An online survey was considered to be easier for clinicians to drop-off documents rather than posting via a traditional postal service. In addition, we were of the opinion that an online survey would enhance our response rate when compared to a postal survey as suggested by Lazar and Preece.[Citation30] Available web-based survey platforms such as survey monkey and Bristol surveys were decided against as we wanted to have direct communication with our respondents,[Citation31] and at the same time accommodate file transfer to facilitate the upload of the available guidance. We were sensitive to the fact that occupational therapists have been slow to integrate technology within professional practice and wanted to ensure that the system was not difficult to operate.[Citation32] There is also evidence that internet-based surveys provide an attractive alternative to postal and telephone surveys for health professionals.[Citation33]
NHS settings were targeted, where occupational therapists who are involved in the provision of minor assistive devices work. These were identified by searching through the online NHS service directories page1 and social care settings where therapists work through the online A–Z list of local councils2.
To maximize response rates, we followed Dillman et al.’s [Citation34] guidelines as suggested by Monroe et al. [Citation35] who emphasized the importance of personalization. Therefore, individual emails were sent to each participant by including personalized survey links along with two reminder emails including a statement which specified how long it would take to complete the survey.[Citation36] The survey was one page in length and questions were either closed or of a Likert scale type. Questions were related to the quality of the guidance in terms of currency, development, evaluation and accessibility (). The survey questions were developed from best available guidance.[Citation37–39] To ensure content validity of the survey and coherence of the survey questions, a group of experts were asked to comment on the survey.
Table 1. Outline of survey questions.
Descriptive statistics (i.e., frequencies and percentages) were used to analyse the collected data. The readability of the collected guidance leaflets was measured using the SMOG formula (simplified measure of goobledygook) which was formulated by McLaughlin [Citation40] who uses vocabulary difficulty and sentence length to predict the difficulty level of a text.[Citation41] It has been suggested by the national voice for life-long learning as it gives the readability score rather than the high school level. One hundred words from the beginning, middle and end of the document were entered into the SMOG calculator. If the document was short in text, we manually applied the SMOG formula to the text instead of using the website application to work out the readability score.
All of the identified pieces of guidance were sent to two occupational therapists. The therapists read each document independently and included the guidance if this made reference to how to measure bed, chair, toilet, bath and/or stairs. The two therapists discussed and debated aspects of measurement although they did not exclude documents if they perceived the measurement process was flawed. The guidance was then examined using a template to determine how and what measurements are taken and other factors that were related to the measurement. Extracted information included how measurements are taken, either of furniture height only and or with the person present. We also extracted relevant additional factors related to the measurement, such as environmental factors, type of furniture and suggested height of furniture. These were then placed under each relevant table. We then further synthesized the data to ascertain similarities and differences between the content of the guidance ().
Table 2. Synthesis of Measurement Guidance Leaflets.
Results
From a total of 325 responses, 274 were not utilizing any guidance. The highest response rate from a single clinical area () was physical disability in the community,[Citation42] acute physical,[Citation42] social services,[Citation39] physical rehabilitation,[Citation37] acute mental health [Citation28] and neurology.[Citation20] Not all the questions from the survey were completed by the participants (). Guidance was developed specifically for persons in acute care, or in the community with no guidance developed for use in other specialties. Eight guidance leaflets were written in 2008, one document within 2011. Four of the guidance leaflets reported to have been evaluated and six of them had not been evaluated. Four of the documents had been reviewed in 2004, with one guidance reviewed in 2011. In relation to accessibility to service users (nine respondents), three persons rated the guidance to not be accessible at all, whilst three others rated it to be of some use to service users. In relation to how the guidance had been developed, four of the documents were devised by therapists with the remaining four guidance documents having no author. In regard to therapists’ perceptions of the guidance, three (out of seven) therapists rated it as being very much fit for purpose, one very good, and two fairly good. Four (out of 10) perceived the guidance as very easy to use, one good and two fairly easy to use.
Table 3. Response rates from clinical area.
Table 4. Response rates from survey.
Readability
The readability analysis revealed that eight of the guidance leaflets were aimed at National Adult Literacy standard 3 (age 9–11), which means that adults should be able to read short, straightforward texts on familiar topics accurately and independently (learning observatory 2015). The remaining 5 guidance leaflets were aimed at individuals with skills beyond level 3 and who could read a broadsheet newspaper.
Measurement of home furniture
Two guidance documents were received via the post and 13 guidance documents were uploaded. Thirty documents were found online. In total, 15 guidance documents met the inclusion criteria (4 documents from the national survey and 11 documents from the online search). None of the guidance made reference to any published research in the area of measurement and or how the guidance was developed as per the inclusion criteria.
Furniture height
Among the guidance leaflets, there was some agreement in relation to furniture height for the bed and chair. For measuring the height of the toilet there was agreement that the measurement should start on the floor but there were subtle differences as to where the measurement should be taken from and to (i.e., toilet bowl,[Citation6] toilet seat,[Citation2,Citation3] seat up [Citation5]). No guidance was available for bath and/or for stair rail height. The guidance did make specific reference to the “make up” of the furniture, e.g., the type of chair, bed and/or whether adaptive devices were present.
Person present
The measurement of the person (i.e., popliteal height) was viewed as an important measurement for provision of chair, toilet, and bed devices. All but one of the guidance leaflets agreed that the measurement should occur from the floor to the “back of the knee” with one guidance (Guidance 9) only stating that it occurs “just behind the knee”. Footwear was only mentioned in relation to measuring a chair. In relation to the measurement of toilets and chairs, it was suggested that an additional 2 inches (5 cm) should be added for persons with a hip replacement. However, one document suggested that the additional measurement should be 2.5 cm (Guidance 8).
Discussion
Health literacy is defined as the ability to “access, understand, evaluate, and communicate information as a way to promote, maintain, and improve health in various settings over the life-course”.[Citation42] Guidance is only effective if service users can read and understand the information provided. One means of determining the quality of provided guidance is to use the International Patient Decision Aid Standard (IPDAS). The IPDAS was formulated after an online Delphi Process with an international group of collaborators to assess the quality of decision aids.[Citation43] Three of the 9 rating scales are based around, conflict of interest, structure and lay out, and reliability.
The findings from our research found that guidance was not always updated or attributed to an author or accessible to an author. However, what was of interest is that despite these limitations some therapists rated guidance as being very much fit for purpose, i.e., one very good, two fairly good. Four (out of 10) perceived the guidance as very much easy to use, one good and two fairly easy to use. This could suggest that therapists are not aware of how quality guidance should be devised and also supports a better education campaign about the importance of guidance. A positive factor of the research was that the readability of eight of the documents was aimed at National Adult Literacy standard three (Guidance leaflets 9–11), although the remaining five guidance leaflets were aimed at individuals with skills beyond level three. The average reading age in the UK population is nine years old. It should be noted, however, that that the expectation of a person reaching level three in the literacy standards is able to read “short, straightforward texts on familiar topics accurately and independently”. The process of measurement may not be familiar and therefore developers of guidance should take this into account, e.g., within the measurement guidance in our study terminology such as “midline”, “depressed” and or “ninety degrees” may not be understood by service users and carers. Our research suggests that more needs to be done if we are to ensure service users have access to high quality information within the measurement process for devices.
The data from the national survey found that 84% of trusts were not using any guidance. This could mean that therapists are undertaking unnecessary home visits to take measurements for devices and/or that the measurements that are being submitted are not accurate or consistent. We do not know the effect that measurement error has on function and further work is needed to determine this, as well as its effect on patient safety. In addition, information is needed to enable service users to contribute to shared decision making and facilitate self-assessment.[Citation17]
This research is unable to comment on the accuracy of information as suggested by the IPDAS, although we can comment on similarities and differences. Our research found that in relation to bed, chair and toilet height to fit the person, the measurement that was used for the person was from the floor to the back of the knee which is sometimes referred to as popliteal height. However, the reliability and validity of this measurement has been questioned.[Citation44]
Measurement of bed height is particularly important in relation to falls management and functional independence. One strategy in fall prevention is to keep beds in a low position.[Citation45] The analysis of the guidance revealed that the content related to the measurement of bed height to fit the person was consistent. Likewise the same measurements are used in a research paper by Capezuti et al.[Citation46] The findings from our study found some consistency between the different guidance leaflets. For both the measurement of the furniture and to fit the person, guidance emphasized that mattresses should be depressed. However no further guidance is given as to whether this included duvet covers or where the person should sit. Nevertheless, Tzeng et al. [Citation45] suggest the measurement should be from the floor to the “middle of the bed”.
Accurate measurement of chair height is important as the seat height influences the performance of older adults.[Citation46] When a chair seat is lower than knee height, a longer time is taken to rise to standing and the older occupant needs to use faster and larger trunk flexion movements to rise.[Citation22,Citation23] Less effort is needed to rise from a high chair although research by Chen et al. [Citation25] found that older adults felt it was less safe to rise and sit at lower and higher seat heights. It has been established that a seat height equivalent to knee height is most easy to rise from.[Citation22,Citation23] Within the chair guidance, specific reference was made to the positioning and angle of knees, hips and ankles. Rationale for this is probably because of the 90°–90°–90° position which is regarded as the best ergonomic seated position.[Citation47] It is related to the view that the aim should be able to achieve symmetry on both sides of the body to avoid obliquity, rotation and posterior pelvic tilt [Citation48] which may account for the reference made to the assignment of the pelvis in one guidance. However, the optimum seat height for comfort is not necessarily the same as the height required for ease of rising. A chair chosen for optimum comfort would allow the user to rest the feet squarely on the floor and would ensure that there was no pressure under the thighs that could limit blood circulation. In addition, the seat height chosen to maximize the ease of rising would be slightly higher than that chosen for comfort.[Citation25] In relation to the measurement of the chair seat height only with no person sitting on it, the measurement leaflets from our study are different from those used in studies by Weiner et al. [Citation49] and Kirvesoja et al.[Citation24]
Our research found that only one guidance made reference to measurements to fit a stair rail specifically for a service user. We found no published research to substantiate the measurement guidance for a stair rail. It is important that attention to building regulations should be adhered to. An interesting stair formula for the calculation of a stair rail for service users is suggested by Ishihara et al.[Citation50] Whilst it looks promising, this formula remains untested in practice.
Few guidance leaflets made reference to toileting which was surprising since toileting is an essential activity of daily living. In our study, there was subtle difference in relation to the measurement of the toilet height. However, there were no identified studies about prescription of toileting devices for older adults or their usage by health care professionals. Studies of users’ perceptions of toileting devices have not been published either. Although one paper was found that made reference to measurement of toilet,[Citation46] this paper spent little time discussing optimal toilet height.
Unfortunately, our research found no guidance that made reference to the measurement of the bath. Despite research outlining the importance of bathing to service users,[Citation51] bathing is often given a low priority by health care professionals as it is not regarded as an essential activity of daily living.
Conclusion
This research is unable to comment on the accuracy of information gathered, although we can comment on identified similarities and differences. Our research suggests that there are both different techniques and ways of presenting measurement information within a given guidance. There is need to ensure that information within guidance is not only evidence based but is accurate as well. Thus, our research has highlighted the need to confirm and agree measurement techniques for home furniture in the provision of assistive devices. This will then allow guidance to be tested for accuracy and ensure the best fit of devices. Moreover it could in turn enable service users to self-assess and consequently reduce the need for therapists to perform measurements of furniture and spend their time more efficiently.
Acknowledgements
The authors would like to acknowledge the UK Occupational Therapy Foundation (UKOTRF), which funded and supported the project and all participants in the survey for their time and effort in our work.
Disclosure statement
The authors report no conflicts of interest.
Notes
Notes
1 see http://www.nhs.uk/servicedirectories/Pages/ServiceSearch.aspx. [cited 2016 Apr 19].
2 see http://www.direct.gov.uk/en/dl1/directories/localcouncils/atozoflocalcouncils/index.htm. [cited 2016 Apr 19].
References
- Agree EM. The influence of personal care and assistive devices on the measurement of disability. Soc Sci Med. 1999;48:427–443.
- Wilson DJ, Mitchell JM, Kemp BJ, et al. Effects of assistive technology on functional decline in people aging with a disability. Assist Technol. 2009;21:208–217.
- Verbrugge L, Rennert C, Madans J. The great efficacy of personal and equipment assistance in reducing disability. Am J Public Health. 1997;87:384–392.
- Sanford JA, Griffiths PC, Richardson P, et al. The effects of in-home rehabilitation on task self-efficacy in mobility-impaired adults: a randomized clinical trial. J Am Geriatr Soc. 2006;54:1641–1648.
- Damant J, Knapp M, Watters S, et al. The impact of ICT services on perceptions of the quality of life of older people. J Assist Technol. 2013;7:5–21.
- Siegel C. Contributions of ambient assisted living for health and quality of life in the elderly and care services – a qualitative analysis from the experts’ perspective of care service professionals. BMC Geriatrics. 2014;14:112.
- Transparency Market Research Elderly and Disabled Assistive Devices Market 2015; [cited 2016 Apr 19]. Available from: http://transparencymarketresearch.com/elderly-disabled-assistive-devices.html.
- Dahlin-Ivanoff S, Sonn U. Use of assistive devices in daily activities among 85-year-olds living at home focusing especially on the visually impaired. Disabil Rehabil. 2004;26:1423–1430.
- Gitlin LN, Winter L, Dennis MP, et al. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc. 2006;54:809–816.
- Mann WC, Ottenbacher KJ, Fraas L, et al. Effectiveness of assistive technology and environmental interventions in maintaining independence and reducing home care costs for the frail elderly. a randomized controlled trial. Arch Fam Med. 1999;8:210–217.
- Gosman-Hedström G, Claesson L, Blomstrand C, et al. Use and cost of assistive technology the first year after stroke. A randomized controlled trial. Int J Technol Assess Health Care. 2002;18:20–27.
- Graybill EM, McMeekin P, Wildman J. Can aging in place be cost effective? A systematic review. PLoS One. 2014;9:e102705.
- Phillips B, Zhao H. Predictors of assistive technology abandonment. Assist Technol. 1993;5:36–45.
- Martin JK, Martin LG, Stumbo NJ, Morrill, et al. The impact of consumer involvement on satisfaction with and use of assistive technology. Disabil Rehabil Assist Technol. 2011;6:225–242.
- Fraser SA, Kenyon V, Lagacé M, et al. Stereotypes associated with age-related conditions and assistive devices in Canadian media. Gerontologist. 2015;pii:gnv094.
- Verza R, Lopes Carvalho ML, Battaglia MA, et al. An interdisciplinary approach to evaluating the need for assistive technology reduces equipment abandonment. Mult Scler. 2006;12:88–93.
- Johnston P, Currie LM, Drynan D, et al. Getting it “right”: how collaborative relationships between people with disabilities and professionals can lead to the acquisition of needed assistive technology. Disabil Rehabil Assist Technol. 2014;9:421–431.
- Gramstad A, Storli SL, Hamran T. Exploring the meaning of a new assistive technology device for older individuals. Disabil Rehabil Assist Technol. 2014;9:493–498.
- Kintsch A, DePaula R. A framework for the adoption of assistive technology. Boulder: University of Colorado; 2002; [cited 2016 Apr 19]. Available from: https://pdfs.semanticscholar.org/87af/970a0aadf2804b056600b6787e4e99d6e864.pdf.
- American Occupational Therapy Association. Assistive technology within occupational therapy practice. Am J Occup Ther. 2004;58:678–680.
- Scherer M. Assistive technology: matching device and consumer successful rehabilitation. Washington (DC): American Psychological Association; 2001.
- Alexander NB, Galecki AT, Nyquist LV, et al. Chair and bed rise performance in ADL-impaired congregate housing residents. J Am Geriatr Soc. 2000;48:526–533.
- Hughes MA, Weiner DK, Schenkman ML, et al. Chair rise strategies in the elderly. Clin Biomech. 1994;9:187–192.
- Kirvesoja H, Väyrynen S, Häikiö A. Three evaluations of task-surface heights in elderly people’s homes. Appl Ergonom. 2000;31:109–119.
- Chen SH, Lee YH, Chiou WK, et al. A pilot study examining seat heights and subjective ratings during rising and sitting. Int J Ind Ergonom. 2010;40:41–46.
- Hoffmann T, Russell T. Pre-admission orthopaedic occupational therapy home visits conducted using the Internet. J Telemed Telecare. 2008;14:83–87.
- Atwal A, Spiliotopoulou G, Stradden J, et al. Factors influencing occupational therapy home visit practice: a qualitative study. Scand J Occup Ther. 2012;21:40–47.
- Isaacson M. Best practices by occupational and physical therapists performing seating and mobility evaluations. Assist Technol. 2011;23:13–21.
- Williamson JD, Fried LP. Characterization of older adults who attribute functional decrements to “old age”. J Am Geriatr Soc. 1996;44:1429–1434.
- Lazar J, Preece J. Designing and implementing web-based surveys. J Comp Inform Syst. 1999;39:63–67.
- Andrews D, Nonnecke B, Preece J. Electronic survey methodology: a case study. Comp Inter. 2003;16:185–210.
- Atwal A, Money AG, Spiliotopoulou G, et al. Occupational therapists’ perceptions about the clinical utility of the 3D interior design software. Disabil Rehabil Assist Technol. 2013;4:348–355.
- Braithwaite D, Emery J, De Lusignan S, et al. Using the internet to conduct surveys of health professionals: a valid alternative? Fam Pract. 2003;20:545–551.
- Dillman DA, Smyth JD, Christian LM. Internet, mail, and mixed mode surveys: the tailored design method. Hoboken (NJ): John Wiley and Sons; 2009.
- Monroe MC, Adams DC. Increasing response rates to web-based surveys. J Ext. 2012;50:6T0T7.
- McPeake J, Bateson M, O’Neill A. Electronic surveys: how to maximise success. Nurse Res. 2014;21:24–26.
- Coulter A. Partnerships with patients: the pros and cons of shared clinical decision-making. J Health Serv Res Policy 1997;2:112–121.
- Griffin J, McKenna K, Tooth L. Discrepancy between older clients’ ability to read and comprehend and the reading level of written educational materials used by occupational therapists. Am J Occup Ther. 2006;60:70–80.
- Department of Health. The power of information: putting all of us in control of the health and care information we need. London 2012; [cited 2016 Apr 19]. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213689/dh_134205.pdf.
- McLaughlin GH. SMOG grading – a new readability formula. J Read. 1969;12:639–646.
- Dubay WH. The principles of readability; 2004 [cited 2016 Apr 19]. Available from: http://www.impact-information.com/impactinfo/readability02.pdf.
- Levasseur M, Carrier A. Integrating health literacy into occupational therapy: findings from a scoping review. Scand J Occup Ther. 2012;19:305–314.
- Elwyn G, O’Connor A, Stacey D, et al. International Patient Decision Aids Standards (IPDAS) Collaboration developing a quality criteria framework for patient decision aids: online international Delphi consensus process. Br Med J. 2003;333:417.
- Tuttle NA. Comparison of methods used for measuring popliteal height. Ergonom Aust. 2004;18:14–18.
- Tzeng HM, Yin CY. Heights of occupied patient beds: a possible risk factor for inpatient falls. J Clin Nurs. 2008;7:1503–1509.
- Capezuti E, Wagner L, Brush BL, et al. Bed and toilet height as potential environmental risk factors. Clin Nurs Res. 2008;17:50–66.
- Engström B. Ergonomic seating: a true challenge wheelchair seating and mobility principles. Sweden: Posturalis Books; 2002.
- Lange ML. Focus on positioning philosophies. Occup Ther Pract. 2001;6:15–16.
- Weiner DK, Long R, Hughes MA, et al. When older adults face the chair-rise challenge. A study of chair height availability and height-modified chair-rise performance in the elderly. J Am Geriatr Soc. 1993;41:6–10.
- Ishihara K, Nagamachi M, Komatsu K, et al. Handrails for the elderly: a survey of the need for handrails and experiments to determine the optimal size of staircase handrails. Gerontechnology 2002;1:175–189.
- Ahluwalia SC, Gill TM, Baker DI, et al. Perspectives of older persons on bathing and bathing disability: a qualitative study. J Am Geriatr Soc. 2010;58:450–456.