Abstract
We aimed to investigate the value of fourth day serum estradiol levels in predicting cycle outcome in poor responders. The medical records of 426 patients with low oocyte yield following controlled ovarian hyperstimulation (COH) treatment for a procedure in our institution’s center for ART between 2008 and 2013 were evaluated. Eighty-eight patients exhibiting poor ovarian response (POR) were included in the study. The clinical outcomes of IVF/ICSI were compared based on the basal hormone profile, clinical, and laboratory parameters. Cycle day 4 E2 levels below 110 pg/ml had an odds ratio of 6.05 (95% CI 2.33–15.7; p < 0.001) for embryo transfer. The early follicular response to ovarian stimulation can be anticipated with the cycle day 4 estradiol levels during COH. When a low day 4 serum estradiol level is encountered, abandoning the current COH and proceeding with agents that increase ovarian response to ovarian stimulation before the next treatment cycle can be a realistic approach.
Introduction
Poor ovarian response (POR) is one of the hopeless clinical situations that preclude pregnancy success in assisted reproduction since treatment outcome is dependent on both quantity and quality of oocytes and embryos. During controlled ovarian hyperstimulation (COH), the only parameters currently used to guide the choice of gonadotropin dosing is the response of the ovary reflected as follicular development and estrogen production. COH generally results in unsatisfactory oocyte yield for poor responder patients during in vitro fertilization-embryo transfer (IVF-ET) cycles. Since ovarian folliclular reserve of these patients is diminished, this group of patients receives high doses of gonadotropin to attain mature oocytes for IVF-ET. At the end of the European Society of Human Reproduction and Embryology (ESHRE) meeting in Bologna in 2011, a consensus was reached on the minimal criteria needed to define POR to establish a standard definition that will enable a correct estimate of the incidence of POR and comparison of future clinical trials [Ferraretti et al. Citation2011]. Clinical predictive diagnostic measures are needed to uncover the individual poor responder women who are not destined to produce mature oocytes for IVF-ET so that the COH with high dose gonadotropin is withheld earlier to prevent these patients from unnecessary ovarian stimulation [Bentov et al. Citation2013; Somigliana et al. Citation2013; Yang et al. Citation2012]. Early predictive tests that emphasize the probability of achieving high quality oocytes during ovarian stimulation are needed to decide whether to continue or abandon the current cycle. Although high gonadotropin utilization with longer periods of stimulation achieves fewer and possibly low quality follicles and a lower estradiol increase during ovarian stimulation of these patients adversely impact the success of the assisted reproductive techniques [Satwik et al. 2012]. Ovarian response to COH is monitored by serial maternal serum estradiol (E2) level measurements and ultrasonographic surveillance of follicle growth. During assisted reproductive technology (ART) procedures, the first control visit of the patients is on the fourth day of the current ovarian stimulation cycle following three days of gonadotropin administration. However, the dosage of gonadotropins can be changed according to the E2 levels on day 4 of ovarian stimulation to increase the number of follicles recruited, the actual ovarian response to COH cannot be predicted. In this study, we investigated the predictive value of serum E2 level measurement on day 4 of COH regarding the cycle outcome measures including oocyte yield and pregnancy rate.
Results
The clinical characteristic features of the study population are summarized in . Five patients achieved clinical pregnancy and 83 patients failed to achieve clinical pregnancy (5.7%). Overall, the clinical pregnancy rate per ET was 11.9% (n = 42). No cases of ovarian hyperstimulation syndrome were observed during the treatment period. The comparison of COH and IVF-ET outcomes of patients with and without clinical pregnancy as an endpoint is presented in . ET of 46 patients could not be carried out due to lack of oocyte retrieval (n = 25), lack of mature oocytes (n = 9), fertilization failure (n = 11), or failed embryo development (n = 1). The number of two pronuclei (2PN)-embryos and embryos transferred were higher in the group that achieved clinical pregnancy as compared to the group that failed to achieve a clinical pregnancy. This was statistically significant (p = 0.029 and 0.049, respectively). No significant differences were observed regarding the level of cycle day 4 serum E2, the increment coefficient, stimulation days, mean follicle number, serum E2 and progesterone levels on hCG day, endometrial thickness on hCG day, total number of metaphase II oocytes, and fertilization rate between the pregnant and non-pregnant groups. Statistically significant positive correlations were found between cycle day 4 serum E2 levels and total mature follicles, total oocytes, metaphase 2 oocytes, 2PN, and the number of embryos (Pearson correlation test p value and r (correlation coefficient) value, respectively: p < 0.001- r = 0.52; p < 0.001- r = 0.44; p < 0.001- r = 0.48; p < 0.001- r = 0.47; p < 0.001- r = 0.44). The receiver operating characteristic (ROC) curve analysis revealed a positive non-significant relationship between cycle day 4 E2 levels and clinical pregnancy () (area under the curve, AUC: 0.68; p = 0.19; 95% CI 0.51–0.85). AUC for ET was 0.74; p < 0.001; 95% CI 0.63–0.84 (). Cycle day 4 E2 levels below 110 pg/ml had an odds ratio of 6.05 (95% CI 2.33–15.7; p < 0.001) for ET and odds ratio of 2.5 (95% CI 0.4–15.9; p = 0.31) for clinical pregnancy. The 110 pg/ml cut-off value for estradiol had a sensitivity 59.52% (95% CI 43.35–73.98), specificity 80.43% (95% CI 65.62–90.14), positive and negative predictive values (PPV and NPV) 73.53% (95% CI 56.88–85.39) and 68.52% (95% CI 55.25–79.32), respectively, with diagnostic accuracy of 70.45% for the prediction of embryo transfer.
Figure 1. The receiver operating characteristic (ROC) curve analysis of the relationship between the rise in serum E2 levels on stimulation day 4 and achieving clinical pregnancy(n = 5/88) (AUC = 0.68; p = 0.19; 95% CI 0.51–0.85).
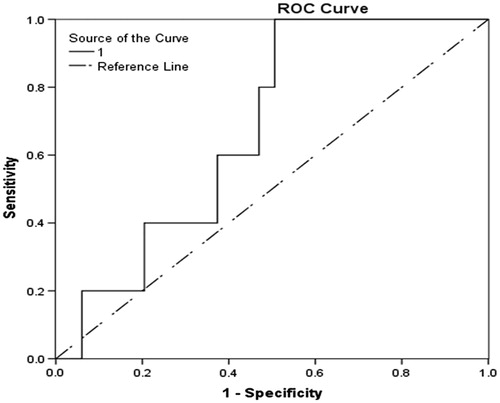
Figure 2. The receiver operating characteristic (ROC) curve analysis of the relationship between the rise in serum E2 levels on stimulation day 4 and achieving embryo transfer (n = 42/88) (AUC: 0.74; p < 0.001; 95% CI 0.63–0.84).
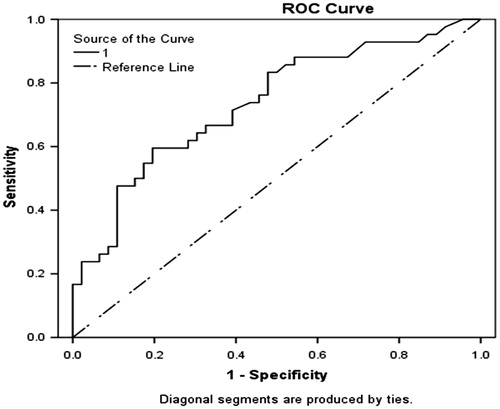
Table 1. Clinical characteristics of the study group.
Table 2. The comparison of poor responder patients according to the cycle characteristics and cycle outcomes based on clinical pregnancy achievement status as a result of the current IVF-ET treatment cycle.
Discussion
POR during ovulation induction presents a major problem for infertility specialists. Not only are the number of the oocytes recovered fewer but the oocyte quality is diminished for these patients with a low pool of follicles. Various screening tests have been introduced to predict poor ovarian responders before initiation of ovulation induction to tailor the treatment strategy and doses of medication to that patient. Previous ART cycle outcomes, age, antral follicle count, ovarian volume, day 3 FSH, E2, inhibin, anti-Müllerian hormone (AMH), and dynamic ovarian reserve tests are currently used as predictive tests for determining ovarian response to COH [Koshy et al. Citation2013; Muasher et al. Citation1988; Mutlu et al. Citation2013; Oudendijk et al. Citation2012; Smotrich et al. Citation1995; Watt et al. Citation2000]. However, apart from the actual ovarian follicular response to ovarian stimulation itself, none of the predictive tests for ovarian reserve have been found to be sufficiently accurate for predicting the ovarian response. Based on the exogenous FSH ovarian reserve test (EFORT), a dynamic ovarian reserve test that evaluates the ability of granulosa cells to produce estradiol as a reflection of the amount of ovarian follicles was developed. We measured the level of serum E2 on day 4 of ovarian stimulation. The ovarian response of an individual patient to COH treatment is the most accurate predictive test for her ovarian reserve that is independent of age. Bentov et al. [Citation2013] evaluated the concentration of serum FSH on cycle day 7 (CD7) during COH treatment of poor responders. They concluded that a CD7 FSH level higher than 22 IU/L reflects the low utilization of serum FSH by granulosa cells. Thus when this clinical scenario is encountered, increasing the dose of FSH seems to be a futile intervention to increase follicular response [Bentov et al. Citation2013]. The ability to predict current cycle outcome during ovarian hyperstimulation for assisted reproduction can change the treatment strategy earlier and protect the patient from unnecessary medical and financial interventions of a treatment cycle that will eventually yield POR.
Following the early cancellation of the treatment cycle, administration of pretreatment adjuvants like dehydroepiandrosterone sulphate (DHEA), growth hormone, and/or testosterone, can reduce the number of cycles of the potentially poor responders without several failed IVF-ET treatment cycles [Eftekhar et al. Citation2013; Fouany and Sharara Citation2013; Fusi et al. Citation2013; Narkwichean et al. Citation2013; Singh et al. Citation2013; Yilmaz et al. Citation2013]. In a randomized study Eftekhar et al. [Citation2013] evaluated the IVF-ET cycle outcome after the addition of growth hormone in an antagonist protocol among poor responders. They concluded that although the number of oocytes retrieved and the number of embryos obtained were significantly higher in patients who received growth hormone therapy during COH treatment, there were no significant differences between groups regarding implantation, and chemical and clinical pregnancy rates.
In this study, we have demonstrated that a higher level of day 4 serum E2 reflects a potentially higher number of oocytes that may be retrieved and increased per cycle ET rate. Poor responder patients represent a heterogeneous group and the fertility treatment outcomes for these patients may vary according to the specific measures including patient age, antral follicle count, day 3 levels of FSH and AMH, or the actual number of oocytes obtained during IVF-ET. These predictive markers of ovarian reserve may help guide treatment choice and provide a strategy to overcome the negative effect of expected low oocyte yield on the pregnancy rate during ovarian stimulation. Cycle outcomes can be informed early by considering total mature follicles, total oocytes, metaphase 2 oocytes, 2PN, and the number of embryos anticipated with the day 4 cycle E2 levels during IVF-ET procedure. Future studies investigating this association will probably increase the predictive value of assessing the day 4 level of E2 for achieving clinical pregnancy. When a low day 4 level of serum E2 is encountered, abandoning the current IVF-ET procedure and proceeding with agents that increase ovarian response to COH before the next treatment cycle may be worth considering. However, additional research is needed to identify more sensitive clinical or biochemical markers that may predict the probability of achieving a clinical pregnancy with poor responding patients before establishing the course of treatment.
Materials and Methods
This retrospective observational study was undertaken in the IVF Centre of a tertiary education and research hospital. The study protocol was approved by the institutional human ethics committee. The medical records of 426 patients with low oocyte yield following COH treatment for an ART procedure in our institution’s center for ART between 2008 and 2013 years have been evaluated. The patients exhibiting POR based on the diagnostic criteria established at Bologna in 2011 by the European Society of Human Reproduction and Embryology (ESHRE) were included in the study after exclusion of the patients with male factor, endometriosis, chromosomal abnormalities in either male or female, any other condition contributing to fertility potential, and the patients with cancelled cycles due to poor response, wrong injections, concomitant diseases or social reasons. The COH and IVF-ET outcomes of 132 patients exhibiting at least two of the following three diagnostic criteria for POR: (i) advanced maternal age or any other risk factor for POR, (ii) a previous POR, and (iii) an abnormal ovarian reserve test (ORT) or two episodes of POR after maximal stimulation in the absence of advanced maternal age or abnormal ovarian reserve test have been evaluated. We excluded another 44 women due to retrieval of oocytes more than or equal to 5 and the remaining 88 patients were included in the analysis.
A written informed consent was obtained from all patients before the COH procedure started. COH procedures of the patients commenced with long agonist, antagonist, or microdose flare-up protocols. Nine patients (10.2%) received a long agonist protocol, 51 (58%) patients received an antagonist protocol, and 28 (31.8%) patients received a microdose flare-up protocol. During the long agonist protocol, subcutaneous (sc) daily 0.75 mg leuprolide acetate (Lucrin; Abbott, Cedex, France) injections were started on day 21 of the preceding cycle and decreased to 0.5 mg upon ovarian suppression confirmed by serum LH levels of 5 IU/mL and E2 levels of <50 pg/ml, and followed by utilization of hMG (human menopausal gonadotropin) (Menogon; Ferring, Istanbul, Turkey) and/or recombinant FSH (Gonal-F; Serono, İstanbul, Turkey). During the antagonist protocol, patients received hMG and/or recombinant FSH starting on days 2 or 3 and 0.25 mg cetrorelix (Cetrotide; Asta Medica, Frankfurt, Germany) was administered daily when two or more follicles reached 13–14 mm in diameter. The doses of hMG and recombinant FSH were adjusted according to the ovarian response for both groups till the day of final oocyte maturation. Recombinant hCG (250 micrograms sc, Ovitrelle, Serono, Istanbul, Turkey) was administered when at least one leading follicle reached a mean diameter of 18 mm and the serum E2 concentration was >500 pg/mL. Thirty six h after hCG injection transvaginal oocyte retrieval was performed. Following oocyte retrieval, metaphase II oocytes were reviewed and ET was performed using pelvic ultrasonography for all patients. For all patients who achieved the ET milestone, luteal phase support was carried out by vaginal progesterone (Crinone 8% gel, Serono, İstanbul, Turkey) supplementation twice a day until menstruation or for 12 w following the ET procedure in case of a clinical pregnancy establishment. The presence of a gestational sac with accompanying fetal heartbeat by ultrasound at least 4 w after ET was defined as a clinical pregnancy. The COH and IVF-ET outcomes of 132 patients were compared based on the mean serum E2 levels on day 4 of ovarian stimulation. Serum E2 levels were assayed using a competitive binding immunoenzymatic assay (Beckman Coulter UniCel® DxI 800, Brea, CA, USA). Intraassay and interassay coefficients of variation of estradiol were less than 10% and 15%, respectively. Statistical analysis was performed by using IBM SPSS Statistics Software (21.0, SPSS Inc., Chicago, IL, USA). Categorical variables were compared with Fisher’s exact or Pearson chi-square tests when available. Kolmogorov- Smirnov test was used to determine the normality of the distributions of data. The continuous variables were presented as mean ± standard deviation values and compared by using the independent samples t test when distributed normal. Mann-Whitney U test was used when the results were not found to be distributed normal or for comparison of non-parametric data. Spearman's rank correlation coefficient (r) was used to assess associations. The accuracy of each test was evaluated separately. The detection and false-positive rates in the prediction of outcome were estimated by using ROC curves analysis and diagnostic power of these screening tests were assessed by comparison of AUC. The sensitivity, specificity, PPV, and NPV with their associated 95% CI were determined for each method. Two-tailed p value of <0.05 was considered to be statistically significant.
| Abbreviations | ||
| 2PN | = | two pronuclei |
| AMH | = | anti-Müllerian hormone |
| ART | = | assisted reproductive technology |
| AUC | = | area under curve |
| CD7 | = | cycle day 7 |
| CI | = | confidence interval |
| COH | = | controlled ovarian hyperstimulation |
| DHEA | = | dehydroepiandrosterone sulphate |
| E2 | = | estradiol |
| EFORT | = | exogenous FSH ovarian reserve test |
| ESHRE | = | European Society of Human Reproduction and Embryology |
| ET | = | embryo transfer |
| FSH | = | follicle stimulating hormone |
| hCG | = | human chorionic gonadotropin |
| hMG | = | human menopausal gonadotropin |
| ICSI | = | intracytoplasmic sperm injection |
| IVF | = | in vitro fertilization |
| LH | = | luteinizing hormone |
| NPV | = | negative predictive value |
| POR | = | poor ovarian response |
| PPV | = | positive predictive value |
| ROC | = | receiver operating characteristic |
Declaration of interest
The authors report no declarations of interest. There remain no relevant potential conflicts of interest related to this original article. Also, there remains no affiliation with any organization with a financial interest, direct or indirect in the subject matter or materials discussed in the manuscript. The authors did not receive any funding and/or financial support from any commercial or other association for this study.
Author contributions
All authors contributed significantly to this study, all authors are in agreement with the content of the manuscript and approved the final version of the paper. All authors participated in all works needed for preparing the final original research. Concept, design, and all comments of this original research are prepared and established by all of the authors as active participants. Conceived and designed the study: YE-U, NY; Collected the data: SK, OHY, SY, IK; Analyzed the data: SK, ASO-E; Wrote the manuscript: SK, OHY, ASO-E.
References
- Bentov, Y., Burstein, E., Firestone, C., Firestone, R., Esfandiari, N., and Casper, R.F. (2013) Can cycle day 7 FSH concentration during controlled ovarian stimulation be used to guide FSH dosing for in vitro fertilization? Reprod Biol Endocrinol 11:12. doi: 10.1186/1477-7827-11-12. PubMed PMID: 23433095; PubMed Central PMCID: PMC3607851
- Eftekhar, M., Aflatoonian, A., Mohammadian, F., and Eftekhar, T. (2013) Adjuvant growth hormone therapy in antagonist protocol in poor responders undergoing assisted reproductive technology. Arch Gynecol Obstet 287:1017–21
- Ferraretti, A.P., La Marca, A., Fauser, B.C., Tarlatzis, B., Nargund, G., Gianaroli, L., et al. (2011) ESHRE consensus on the definition of ‘poor response' to ovarian stimulation for in vitro fertilization: The Bologna criteria. Hum Reprod 26:1616–24
- Fouany, M.R., Sharara, F.I. (2013) Is there a role for DHEA supplementation in women with diminished ovarian reserve? J Assist Reprod Genet 30:1239–44
- Fusi, F.M., Ferrario, M., Bosisio, C., Arnoldi, M., and Zanga, L. (2013) DHEA supplementation positively affects spontaneous pregnancies in women with diminished ovarian function. Gynecol Endocrinol 29:940–3
- Koshy, A.K., Gudi, A., Shah, A., Bhide, P., Timms, P., and Homburg, R. (2013) Pregnancy prognosis in women with anti-Mullerian hormone below the tenth percentile. Gynecol Endocrinol 29:662–5
- Muasher, S.J., Oehninger, S., Simonetti, S., Matta, J., Ellis, L.M., Liu, H.C., et al. (1988) The value of basal and/or stimulated serum gonadotropin levels in prediction of stimulation response and in vitro fertilization outcome. Fertil Steril 50:298–307
- Mutlu, M.F., Erdem, M., Erdem, A., Yildiz, S., Mutlu, I., Arisoy, O., et al. (2013) Antral follicle count determines poor ovarian response better than anti-Mullerian hormone but age is the only predictor for live birth in in vitro fertilization cycles. J Assist Reprod Genet 30:657–65
- Narkwichean, A., Maalouf, W., Campbell, B.K., and Jayaprakasan, K. (2013) Efficacy of dehydroepiandrosterone to improve ovarian response in women with diminished ovarian reserve: A meta-analysis. Reprod Biol Endocrinol 11:44. doi: 10.1186/1477-7827-11-44. Review. PubMed PMID: 23680224; PubMed Central PMCID: PMC3663765
- Oudendijk, J.F., Yarde, F., Eijkemans, M.J., Broekmans, F.J., and Broer, S.L. (2012) The poor responder in IVF: Is the prognosis always poor?: A systematic review. Hum Reprod Update 18:1–11
- Satwik, R., Kochhar, M., Gupta, S.M., and Majumdar, A. (2012) Anti-mullerian hormone cut-off values for predicting poor ovarian response to exogenous ovarian stimulation in in-vitro fertilization. J Hum Reprod Sci 5:206–12
- Singh, N., Zangmo, R., Kumar, S., Roy, K.K., Sharma, J.B., Malhotra, N., et al. (2013) A prospective study on role of dehydroepiandrosterone (DHEA) on improving the ovarian reserve markers in infertile patients with poor ovarian reserve. Gynecol Endocrinol 29:989–92
- Smotrich, D.B., Widra, E.A., Gindoff, P.R., Levy, M.J., Hall, J.L., and Stillman, R.J. (1995) Prognostic value of day 3 estradiol on in vitro fertilization outcome. Fertil Steril 64:1136–40
- Somigliana, E., Paffoni, A., Busnelli, A., Cardellicchio, L., Leonardi, M., Filippi, F., et al. (2013) IVF outcome in poor responders failing to produce viable embryos in the preceding cycle. Reprod Biomed Online 26:569–76
- Watt, A.H., Legedza, A.T., Ginsburg, E.S., Barbieri, R.L., Clarke, R.N., and Hornstein, M.D. (2000) The prognostic value of age and follicle-stimulating hormone levels in women over forty years of age undergoing in vitro fertilization. J Assist Reprod Genet 17:264–8
- Yang, S.H., Patrizio, P., Yoon, S.H., Lim, J.H., and Chian, R.C. (2012) Comparison of pregnancy outcomes in natural cycle IVF/M treatment with or without mature oocytes retrieved at time of egg collection. Syst Biol Reprod Med 58:154–9
- Yilmaz, N., Uygur, D., Inal, H., Gorkem, U., Cicek, N., and Mollamahmutoglu, L. (2013) Dehydroepiandrosterone supplementation improves predictive markers for diminished ovarian reserve: Serum AMH, inhibin B and antral follicle count. Eur J Obstet Gynecol Reprod Biol 169:257–60

