?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
This paper aims to provide an effective, accurate, and specific diagnostic method for the diagnosis of pancreatic cancer. It discusses the diagnostic value of magnetic res retrograde cholangiopancreatography (MRCP) combined with the detection of tumor marker carbohydrate antigen 19-9 (CA19-9) for pancreatic cancer. A group of confirmed cases of pancreatic cancer in some hospitals were randomly selected and subjected to an MRCP examination as well as serological CA19-9 detection. In addition, a group of patients whose pancreatic cancer was confirmed by surgery and pathology, and who underwent MRCP without the detection of the tumor marker CA19-9, were also selected for research. The experiment found that the rate of accuracy for the group that underwent MRCP combined with CA19-9 detection showed a higher positive value in the diagnosis of pancreatic cancer than in the group that underwent MRCP alone. Therefore, this paper proposes that MRCP combined with CA19-9 detection can be taken as the reliable and effective means for diagnosis of pancreatic cancer.
Introduction
Pancreatic cancer is one of the malignant cancers that threaten people's health. It is a common malignant cancer of the digestive tract, and accounts for 1% to 2% of malignant cancers of the whole body. It has a high degree of malignancy, and its incidence and mortality increases year by year (CitationBhat et al. 2012). The position of pancreatic cancer is hidden. In addition, its clinical symptoms are not typical and it usually shows no symptoms in the early stage. Sometimes, it presents as digestive tract symptoms or endocrine performance. Therefore, diagnosis is quite difficult. When the disease is detected, it has usually reached the end stage. The effect of clinical treatment is poor, and it is one of the malignant cancers with the worst prognosis so far (CitationVincent et al. 2011).
Based on the size of the tumor, small pancreatic cancer refers to that with the tumor diameter of 2 cm or less, regardless of whether it shows pancreatic infiltration or lymphatic metastasis (CitationLenz et al. 2011). The discovery of small pancreatic cancer is of important significance for the improvement in the prognosis of pancreatic cancer. The rate of resection rate in small pancreatic cancer is very high, about 90%. The five year survival rate of patients is above 70%. However, the resection rate of pancreatic cancer in the medium and end stages is low, and the five year survival rate does not exceed 5% (CitationYeo and Lowenfels 2012). However, the onset of small pancreatic cancer is hidden, and the symptoms are not typical. Some even show gastrointestinal symptoms and cryptorrhea. Many research studies, conducted at home and abroad, indicate that the application of one method of examination alone has limited diagnostic value and a high rate of missed diagnosis. Just one event of iconographical examination or the specificity and sensibility of serum indexes still cannot meet the demand of the diagnosis of pancreatic cancer in the clinic (CitationDe Oliveira et al. 2012). Although the scholars at home once conducted a large number of retrospective studies on pancreatic cancer combined with diagnosis in a large sized sample group of people, most of them were the combination of various iconographical examinations. So far, reports on imaging combined with CA19-9 detection and diagnosis of small pancreatic cancer are rare. Therefore, this paper aims to discuss the value of iconography combined with CA19-9 detection in the diagnosis of pancreatic cancer, and analyze the characteristics of small pancreatic cancer.
Materials and methods
Research object
The patients whose pancreatic cancer had been confirmed by surgery and pathology at a hospital, between 2008.1 and 2012.1, were selected randomly. Of these, 80 cases had been subjected to magnetic res retrograde cholangiopancreatography (MRCP) examination and serological CA19-9 detection (CA19-9 level of > 37 U/ml means positive), among which 10 cases were of small pancreatic cancer (proved by the surgery and pathology, as the diameter of the tumor was smaller than 2 cm). In addition, 48 cases with confirmed pancreatic cancer that did conduct MRCP and did not conduct tumor marker CA19-9 detection were randomly selected from a hospital between 2008.1 and 2012.1. The cases were divided into groups according to the diagnostic methods: Group A was the MRCP combined group, that is, those who underwent MRCP combined with CA19-9 detection, comprised of a total of 70 cases. In addition, the group that was subjected to MRCP but not tumor marker CA19-9 detection was group B, with 70 cases, that is, comprising those who underwent MRCP only. Group C consisted those with small pancreatic cancer, and comprised of 10 cases.
Diagnosis standard
Diagnosis standard of pancreatic cancer: there is no standard for clinical diagnosis so far; this research confirmed pancreatic cancer by the results of surgery, pathology, and endoscopic biopsy pathology.
In the standard diagnosis of small pancreatic cancer, in view of the size of the tumor only, it refers to the pancreatic cancer with a diameter of 2 cm or less, regardless of whether there is pancreatic infiltration or lymphatic metastasis.
The MRCP positive standard is the double duct sign, that is, the lesion invades the bile duct and pancreatic duct, while expanding in the meanwhile; the pancreatic duct expands continuously and is suddenly cut off in a lump; the distal end of the common bile duct is suddenly cut off at the level of the pancreatic head and undergoes the unciform process; the pancreatic duct expands unequally and branch pancreatic cancer shows out.
Research method
The rate of diagnostic accuracy regarding pancreatic cancer in the group that was tested with MRCP combined with CA19-9 detection and the group that underwent MRCP only were compared and analyzed. In addition, the characteristics of small pancreatic cancer were analyzed from the perspective of gender, age, initial symptoms (epigastric discomfort, anorexia, weight loss, jaundice, etc.), whether there is a family history of pancreatic cancer or not, whether it is combined with biliary tract disease or diabetes, CA19-9, liver function, etc.
Statistical method
The investigation data adopted the double type-in method. They were put into the analysis database if there was no difference after comparison. Using the Windows 7 operating environment, SPSS19.0 statistical software was adopted to perform statistical analysis. Measurement data was expressed as mean ± variance (). Qualitative data was expressed as frequency and percentage. Clinical quantitative data adopted the t test for comparison. The qualitative data between groups adopted x2 for comparison. A value of P ≤ 0.05 means the difference has statistical significance.
Result
General condition
In , the average age of patients who underwent MRCP combined with CA19-9 detection is 65.8 years. The oldest was 83 years old, and the youngest was 34 years old. The average age the group which underwent MRCP only was 63.5 years. The oldest was 82 years old and the youngest was 39 years old. The difference in the age of patients between the two groups had no statistical significance (P > 0.05).
Table I. General status of age in the MRCP-combined group and the MRCP-only group.
In , the ratio of females in the MRCP-combined group was 37.2% and that in the MRCP-only group was 31.2%. The gender difference between the two groups had no statistical significance (P > 0.05).
Table II. Gender distribution status of the MRCP-combined group and MRCP-only group.
MRCP performance
MRCP positive performance: double duct sign, that is, the lesion invades the bile duct and pancreatic duct, expanding in the meanwhile; the pancreatic duct expands continuously and is suddenly cut off in a lump; the distal end of the common bile duct is suddenly cut off at the level of the pancreatic head and unciform process; the thickness of the pancreatic duct expands unequally and branch pancreatic cancer is present.
It can be seen in that the figure on the left shows that the pancreatic duct has expanded smoothly, evenly, and continuously, and it has been suddenly cut off at the pancreatic head; the middle figure shows that it has expanded unevenly and the branch pancreatic duct shows out; the figure on the right shows that the common bile duct has been suddenly cut off, and the bile duct inside and outside the liver and the pancreatic cancer has obviously expanded away from focus.
A total of 118 cases collected in this research were of those that had undergone the MRCP examination. A hundred and eleven cases were positive, among which, 72 cases showed the double duct sign (64.8%). 91 cases were those of dilated pancreatic duct (81.9%), among which, 66 cases showed smooth and continuous expansion (59.4%), and 25 cases showed expansion with uneven thickness (22.5%). Eighteen cases showed branch pancreatic duct expansion (16.2%). Eighty-two cases were of those that had been suddenly cut off in the lesion or the uncinate process of the pancreatic head (73.9%). There were 83 cases of cholangiectasis (74.8%), among which, 54 cases showed smooth and continuous expansion (48.6%), and 29 cases showed expansion with uneven thickness (26.1%).
Analysis of the rate of positive diagnosis of pancreatic cancer diagnosis
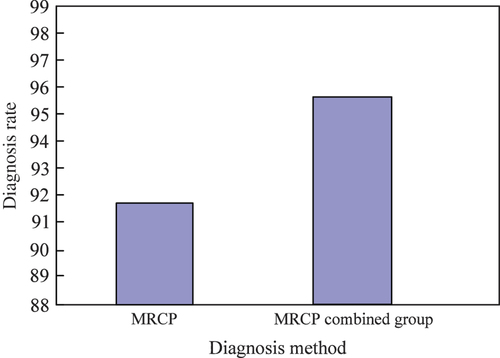
The comparison of pancreatic cancer diagnosis is shown in .
Table III. The comparison of MRCP combined with CA19-9 for the diagnosis of pancreatic cancer.
The rate of positive diagnosis of pancreatic cancer in the group that underwent MRCP combined with CA19-9 detection was 95.7%, and that in the group that underwent MRCP alone, was 91.7%. The difference between the two groups had statistical significance (P < 0.05). The rate of diagnosis in the group that underwent MRCP combined with CA19-9 detection was higher than that of the group that underwent MRCP alone. That is, MRCP combined with CA19-9 detection can improve the rate of accuracy in the diagnosis of pancreatic cancer.
As shown in the figure, the vertical axis represents the accuracy rate of pancreatic cancer diagnosis and the horizontal axis is the diagnostic method.
It can be seen from that the effect on pancreatic cancer diagnosis by MRCP combined with CA19-9 detection was significantly superior to that of the MRCP examination only.
Analysis of clinical characteristics and test rate of small pancreatic cancer
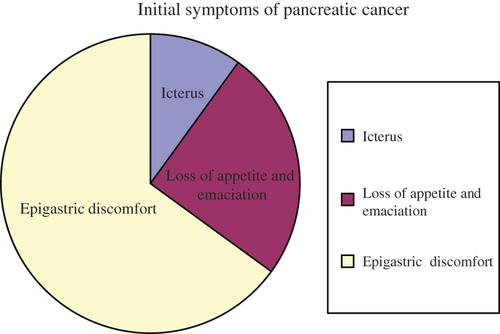
Through the retrospective analysis of 10 cases of small pancreatic cancer, we found that the median age of incidence of small pancreatic cancer was 62.3 years old. It occurs in middle and old age and the ratio of female and male was 6:4. The initial symptoms of small pancreatic cancer are shown in . The most common is epigastric discomfort. There were seven cases that presented this initial symptom. Two cases with loss of appetite and emaciation with unclear reason, one case that presented with icteric sclera, and the laboratory examination hinted at the change in liver function. Total bilirubin (TB) level increased in two cases (> 17.1 U/L), and the level of alkaline phosphatase (ALP) increased in four cases (enzyme rate method > 160 U/L). There were five cases that showed a positive result in serological CA19-9 detection (> 37 U/ml). There were two cases that were merged with diabetes. Pathoglycemia and diabetes were all newly appeared, in patients that had no diabetes and obesity in the past. There were no patients that presented with liver and gall diseases. In one case, the father of the subject died of pancreatic cancer.
shows that the ratio of epigastric discomfort was the largest (70%), ratios of loss of appetite and emaciation were relatively low (20%), and that of icterus was 10%.
Discussion
Pancreatic cancer is a kind of exocrine pancreatic ductal adenocarcinoma, which accounts for 90% to 95% of pancreatic tumors. It usually occurs in the pancreatic head. Its clinical manifestation has no obvious specificity. The common clinical symptoms are epigastric discomfort, dyspepsia, heartburn, loss of appetite, etc. Most patients have serious weight loss. However, these kinds of vague and atypical symptoms are the main reasons that delay the diagnosis by 8 to 10 weeks. Surgery is expected to be a means of treatment. However, it has a low resection rate. The main reason is that the disease is already in the end stage when it is discovered. In clinical practice, early discovery and diagnosis of pancreatic cancer is the key to effective treatment (CitationGuo et al. 2010).
Imaging technology has developed rapidly, at home and abroad. It provides various means for the diagnosis of pancreatic cancer. Different imaging technologies have their own advantages, which can provide the foundation, such as the location, size and infiltration degree of the tumor, whether it has metastasized, etc. for clinical doctors. However, a single imaging examination has limited diagnostic value and a high rate of missed diagnosis. Although B-ultrasonography has weak sensibility and specificity, it is convenient, economical and noninvasive. In addition, liver and bile duct neoplasms inside and outside the liver can be seen by this technique. Therefore, B-ultrasonography is recognized as the preferred method for screening for pancreatic cancer so far. However, the results of B-ultrasonic examination are closely related to the experimental level of the examiner. Moreover, the result is easily disturbed by intestinal gas and fat in the patients’ body, and thus, the full view of the pancreas cannot be clearly displayed. Spiral CT can clearly show the diseased region with accurate position. It can be used for the judgment of vascular invasion and metastasis before the surgery for pancreatic cancer. For example, in some cases, distant metastases, infiltration of neighboring organs, packing or invasion of blood vessels, and lymphoid lesions are found. Then, the tumor cannot be removed by operation. In addition, this kind of scanner does not rely on operation and is not limited by body form and gastrointestinal gas. It can also be used to confirm liver metastasis, lymphoid lesions, and whether surrounding the blood-vessels are invaded. However, it is not reliable for the diagnosis of lesions smaller than 2 cm or of peritoneal nodules. Percutaneous transthoracic fine needle aspiration biopsy (PTFNAB) can be conducted, under the guidance of CT, to confirm histodiagnosis, which is of more importance, especially for the patients who cannot undergo an operation. CT is also the preferred examination for patients with suspected pancreatic cancer, rather than B-ultrasonography. However, it is not sensitive to change in the density of the lesion, which can easily to lead to a missed diagnosis or a misdiagnosis.
MRCP offers a relatively clear and comprehensive display of the normal construction and space occupying lesion of the bile-pancreatic, system and identifies pancreaticobiliary abnormality and vessel wall infiltration. MRCP adopts T2 water imaging to display static or slow-flowing liquid, while at the same time, it can inhibit the signal structure around the pancreas, comprehensively and clearly display the situation of the pancreas and bile duct, and understand whether that position has any obstruction or lesion (CitationTeng 2011). The double duct sign is the reliable sign for diagnosis of pancreatic head carcinoma, which has been proven by various research studies at home and abroad. The involvement and expansion to the pancreatic duct and bile duct is called the double duct sign. Zhang Yu (CitationZhang 2008) et al. found that MRCP can distinguish chronic pancreatic disease and pancreatic cancer according to the different morphological performances, such as the double duct sign. MRCP shows that the main pancreatic duct shows smooth narrow change or no obvious abnormality when it comes across an inflammatory mass of benign lesions. However, MRCP cannot conduct cytology and genetic testing, and is forbidden for use on patients with lots of abdominal dropsy and electromagnetic susceptibility (CitationLenz et al. 2011). The diagnostic accuracy rate of MRCP in this research was shown to be 92.8%, which approximately conforms to the data reported at home.
Endoscope retrograde cholangio pancreatography (ERCP) is a method of injecting contrast medium by intubation of the duodenal papilla under endoscopy, thus achieving the imaging technology that offers a retrograde display of the pancreatic bile duct. It can clearly reflect the change of the main pancreatic cancerous lesion, and its branch. Wei Jinqi (CitationWei et al. 2010) carried out a retrospective analysis and found that the main performances of ERCP with regard to pancreatic cancer are as follows: stenosis, interruption or shifting of the main pancreatic duct, rough and uneven gland bubble in the area of pancreatic substance, retention of contrast medium, filling-defect of pancreatic juice contrast medium, shifting of branch pancreatic duct, etc. An expanded double duct sign can be displayed when the pancreatic head carcinoma oppresses the main pancreatic duct and the common bile duct. Meanwhile, ERCP can perform a biopsy or cytologic examination of the pancreatic duct using a cytobrush, as well as cytology and gene detection on the collected pancreatic juice. Most pancreatic cancer arises in the ductal epithelium. Cancer cells are expelled after falling off. Therefore, pancreatic cancer can be detected by examining the fallen cancer cells present in the pancreatic juice. The positive rate of pancreatic cancer in cytologic examination ranges from 33–75%.
There are 20 kinds of tumor markers of pancreatic cancer that have been reported by various literatures so far, including the serological tumor markers CA19-9, CEA (carcino-embryonic antigen), CA50, CA195, POA, CA494, SPAN-1, Dupan-2, AFP (alpha fetoprotein), etc. However, CEA and AFP have weak sensibility to pancreatic cancer. They can be involved in cross reaction with other tumor markers, and have limited function in the diagnosis of pancreatic cancer (CitationLiu and Qin 2014).
The serological tumor marker CA19-9 was extracted from colorectal cancer tissue by Kaprowski in 1979. In 1982, Dolvillano detected serological tumor marker CA19-9 in the serum of pancreatic cancer patients. Its normal value is 8.1 ± 3.9 u/m1. Generally, a level greater than 30 u/ml indicates abnormality. The specific value in pancreatic cancer patients is abnormally increased. The serological tumor marker CA19-9 is a kind of carbohydrate antigen, and its detection rate is high in pancreatic cancer patients. CA19-9 is the most common tumor maker for the diagnosis of pancreatic cancer found so far. It has been confirmed by most mathematicians as an effective index. However, it has weak specificity. Through a diagnostic performance analysis of different pancreatic diseases, it is found that the serological tumor marker CA19-9 possesses a huge advantage for the diagnosis of pancreatic cancer. The case analysis found that the pathological examination hinted that a positive result for the serological tumor marker CA19-9 was often seen in pancreatic cancer with metastatic lesions, and the positive rate was 67%. In view of the weak sensitivity and specificity of the serological tumor marker CA19-9, it is mostly used for diagnosis of pancreatic cancer combined with imaging examination (CitationYin et al. 2013). The imaging examination and serological tumor marker CA19-9 detection, as mentioned above, have their own advantages and drawbacks. Combined diagnosis can benefit from the strong points, to offset the weaknesses, and make up for these disadvantages to some extent. However, MRCP has its own limitations and cannot achieve cytologic and genetic diagnosis. Therefore, for those patients with unclear MRCP diagnosis, ERCP is necessary. Considering only the size of tumor, small pancreatic cancer, in clinical terms, refers to pancreatic cancer with lesions with a diameter of 2 cm or less, regardless of whether there is pancreatic infiltration or lymphatic metastasis. It is not always early-stage pancreatic cancer, because pancreatic cancer in the early stage can invade nerves, blood vessels and lymph vessels (CitationBen et al. 2010). Early-stage pancreatic cancer refers to tumors with a diameter of 2 cm or less, is limited to the pancreatic substance, and has no pancreatic infiltration and lymphatic metastasis. The diagnostic standard of early-stage pancreatic cancer is the discovery of small pancreatic cancer, which is of great significance for the improvement of prognosis of pancreatic cancer. Scholars have found that the surgical resection rate of small pancreatic cancer is 90%, which is very high, and the five year survival rate of patients is higher than 70%; however, the surgical resection rate of pancreatic cancer in medium and end stages is 15%, which is low, and the five year survival rate of most patients does not exceed 5%. However, small pancreatic cancer is characterized by a hidden onset and atypical symptoms. Some are gastrointestinal symptoms and cryptorrhea only, and have no specific clinical symptoms and results in serology and imaging examinations. Therefore, the diagnosis is difficult.
Through retrospective analysis of ten cases of small pancreatic cancer, this research study has found some warning symptoms of early-stage pancreatic cancer. For example, epigastric discomfort is the most important performance of small pancreatic cancer, and loss of appetite, loss of weight, and icterus should also be highly emphasized. There is research reported that the symptoms in 36 cases of small pancreatic cancer patients were: icterus, accounting for 72%, stomach ache and loss of weight with unclear reason, accounting for 50%, back pain, accounting for 10%, diabetes and loss of weight, accounting for 9% and asymptomatic patients, accounting for 7%. However, this retrospective analysis found that stomach ache with unclear reason is the most common clinical manifestation, which is different from reports in the related literature. It might be due to the small number of experimental cases and the centralized patient distribution in this research. Research on this aspect has yet to be continued, after increasing the sample size.
Conclusion
This paper conducted a comparative research on the accuracy rate of pancreatic cancer diagnosis by MRCP combined with CA19-9 detection, and by MRCP only. The diagnosis rate of the group combining MRCP with CA19-9 detection was increased, compared to the group that underwent MRCP only. MRCP is noninvasive and simple. Therefore, MRCP combined with CA19-9 detection can be regarded as a reliable and effective diagnostic method for the diagnosis of pancreatic cancer. Through the retrospective analysis of ten cases of small pancreatic cancer, it was found that epigastric discomfort, liver function changes, increase of CA19-9 level, diabetes, and familial inheritance were all related to small pancreatic cancer.
Declaration of interest
The authors report no declarations of interest. The authors alone are responsible for the content and writing of the paper.
References
- Ben QW, Wang JC, Liu J, Zhu Y, Yuan F, Yao WY, Yuan YZ. 2010. Positive expression of LI-CAM is associated with perineural invasion and poor outcome in pancreatic ductal adenocarcinoma. Ann Surg Oncol. 17:2213–2221.
- Bhat K, Wang F, Ma Q, Li Q, Mallik S, Hsieh TC, Wu E. 2012. Advances in biomarker research for pancreatic cancer. Curr Pharm Des. 18: 2439–2451.
- De Oliveira T, Abiatari I, Raulefs S, Sauliunaite D, Erkan M, Kong B, et al. 2012. Syndecan-2 promotes perineural invasion and cooperates with K-ras to induce an invasive pancreatic cancer cell phenotype. Mol Cancer. 11:19–25.
- Guo RD, Gu JH, Jiang W, et al. 2010. Effect of GDNF on pancreatic cancer cell proliferation and chemotaxis. Chin J Hepato Sur. 16:204–207.
- Lenz J, Karasek P, Jarkovsky J, et al. 2011. Clinicopathological correlations of nestin expression in surgically resectable pancreatic cancer including an analysis of perineural invasion. Gastrointestin Liver Dis. 20:389–396.
- Liu J, Qin HC. 2014. Clinical significance of CT and serum CA19-9 joint detection in the diagnosis of pancreatic cancer. Mod Prev Medi. 41:531–533.
- Teng YP. 2011. Comparison of the effect of ultrasound B, CT, ERCP and MRCP in diagnosis of hepatolith with concurrence of biliary tract carcinoma. Shandong Medi J. 51:70–71.
- Vincent A, Herman J, Schulick R, Hruban RH, Goggins M. 2011. Pancreatic cancer. Lancet. 378:607–620.
- Wei JQ, Bian Z, Zhou XJ, et al. 2010. Evaluation of ERCP combined with enhancement CT in the diagnosis of pancreatic carcinoma. Chin Pract Medi. 5:50–51.
- Yeo TP, Lowenfels AB. 2012. Demographics and epidemiology of pancreatic cancer. Cancer J. 18:477–484.
- Yin LL, Du YP, Wu CM. 2013. Significance of the detection of serum CA50 combined with CA199 in diagnosis of pancreatic cancer. Medi J Beijing Military Region. 25:31–32.
- Zhang Y. 2008. Diagnostic value of morphology on MRCP in chronic pancreatitis and pancreatic carcinoma. J Prac Radi. 24:919–922.