Abstract
Purpose: Constriction band syndrome afflicting in utero development can lead to devastating and possibly fatal outcomes. A lack of consensus regarding noninvasive testing and surgical modalities is likely secondary to the continued poorly understood pathology. Methods: We provide a case report of a 6-month-old boy who presented with a functional, nonsensate upper limb after surgical release of midhumeral banding at 3 months of age. Results: Exploration revealed intact, albeit atrophic, peripheral nerves with brachial artery disruption above the elbow. Sural nerve grafting was performed and 2-year follow-up demonstrated return of protective sensation in the median nerve distribution with minimal motor return. Conclusion: This case demonstrates that nerves present distal to the original soft tissue insult oppose the idea of failure of nerve formation. Early nerve grafting at the time of initial Z-plasty release may serve to improve long-term functional outcomes.
Introduction
Intrauterine constriction band syndrome has an incidence estimated to occur between 1:10,000 and 1:15,000 live births [Citation1,2]. The condition encompasses a spectrum of terminology including Streeter’s syndrome/dysplasia, annular band/grove/defect, amniotic band syndrome, ring constriction syndrome, fetal amputation, and intrauterine amputation. The congenital event can lead to or is associated with other abnormalities such as facial cleft, club foot, pseudarthrosis, acrosyndactyly, Ehlers–Danlos syndrome, osteogenesis imperfecta, visceral defects and aplasia cutis [Citation2–9].
A definitive etiology has yet to be elucidated, although it is widely accepted that there is no hereditary component. In 1832, Montgomery first observed and described what he believed to be a ‘string of great force’ in stillborns he evaluated, causing depressions and possibly leading to amputations [Citation10]. Streeter offered an opposing view in 1930, whereby the proposed mechanism was a result of defective germ-plasm [Citation11]. A prevalent theory today is a result of Torpin’s ‘extrinsic theory’ work in the 1960s and his reintroduction of intrauterine fibrous banding causing disruption. The source of the bands is thought to be a result of early amniotic membrane rupture – concluded after extensive placental tissue examination [Citation12]. Further, a reproducible animal model suggests that prenatal environmental factors such as intrauterine or extrauterine trauma support extrinsic mechanism9s for maldevelopment [Citation13]. Yet, the extrinsic theory may not account for large body wall defects or visceral abnormalities, perhaps a result of vascular insults [Citation14,15].
The traditional surgical approaches to constricting bands have largely remained unchanged, since described by Stevenson in 1946 [Citation16]. Decompression is achieved through multiple Z-plasty techniques, direct excision and/or adjacent tissue rearrangement with fat–fascia advancement flaps [Citation16–18]. Resolutions of swelling and lymphedema, neurosensory loss recovery and improved cosmesis have all been described as a result of the above procedures [Citation19–21].
However, there is a paucity of data pertaining to the course of treatment when motor dysfunction is present. We present a case report of a constriction band in the upper arm of a child who has complete peripheral motor nerve deficits despite Z-plasty release at an early age.
Case report
A 6-month-old boy was referred from an outside hospital for evaluation of amniotic band syndrome and peripheral nerve palsy to his left upper extremity. The patient’s past medical history is significant for a birth by cesarean section at 32 weeks and being a twin. He is otherwise healthy. The gravida 2, para 2 mother had an uncomplicated pregnancy till the time of birth. While at an outside hospital, the patient was evaluated for an arm that was completely flaccid below the elbow with no wrist or finger movement. There was a midhumeral constriction band just distal to the deltoid insertion. The patient did have shoulder function with deltoid and pectoralis muscle function. He underwent multiple Z-plasty releases, performed circumferentially around the entire midhumeral arm in series to the constriction at 3 months of age. He did not show any neurological improvement by 6 months of age. Physical examination at 6 months of age and 3 months following initial release revealed no peripheral motor or sensory nerve function below the site of the released constriction band; however, forearm and finger tone was present with no flexion or extension contractures (). There was a significant limb-length discrepancy and the patient had weak radial and ulnar arteries by signal. After extensive consultation, the family elected for surgical exploration for possible nerve revision or repair. No preoperative electromyogram (EMG) testing or imaging was performed. The patient at the time of the surgical exploration was 7 months old.
Figure 1. The 7-month-old boy has persistent flail arm after constriction band release with Z-plasty at 3 months of age at an outside hospital. The arm had limb length discrepancy but did show evidence of tone to hand and forearm.

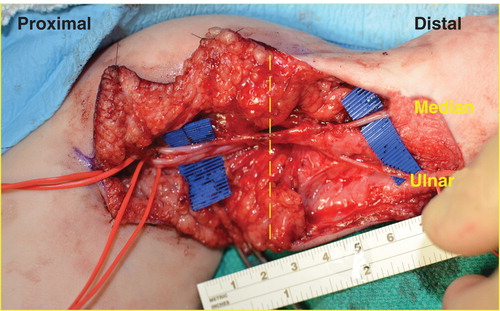
Intraoperatively, a curvilinear incision was made over the constricted tissue and prior scar, extending proximally to the axillary fossa. The neurovascular bundles were identified proximally and followed distally into the band site. Extensive fibrous scarring was evident within the constriction site anteriorly and the caliber of the median and ulnar nerves was tapered. The brachial artery was not continuous through the zone of injury and ended proximal to the antecubital fossa. The ulnar nerve was identified within excessive scar tissue in the cubital tunnel and was dissected proximally. It appeared to be tethered to the humeral bone just proximal to the elbow. Both the median and ulnar nerves were in continuity distal to the band; however, the nerves were clearly atrophic within the band (). Distally, the nerves had intact blood supply and appeared normal in caliber and appearance. Interestingly, no neuroma was identified within the area of compression. The damaged portion of the ulnar and median nerves was resected, leaving a 5-cm gap between normal neural tissues.
Figure 2. Dissection of the median and ulnar nerves revealed narrowing of the nerves in the compressed regions (yellow dashes) with preservation of caliber and vascularity distally. The brachial artery (left vessel loop) abruptly ended at the proximal end of the constricting band with no radial or ulnar artery identified.
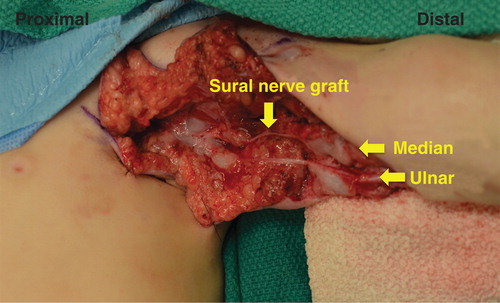
To repair the defect, the sural nerve was taken from the lower extremity and used as a graft for both the median and ulnar nerves. The 9-0 nylon epineural sutures were used to approximate the grafted sural nerve and Tisseel Fibrin Sealant (Baxter International Inc., Deerfield, IL, USA) was added for support (). With extensive dissection through the scar to release the median nerve, it was evident that the blood supply to the hand became tenuous and positioning caused vascular congestion. Doppler signal were unable to capture the radial and ulnar arteries; however, the hand did demonstrate swift capillary refill. The decision was made to not explore the radial nerve due to collateralization being the only source of distal perfusion with brachial artery disruption. The patient was placed in a sling and remained in the hospital for 2 days of vascular observation to the viable, warm hand.
Figure 3. Sural nerve was used to bridge the 5-cm defect in both the median and ulnar nerves with 9-0 nylon and Tisseel fibrin glue. Radial nerve exploration was not undertaken due to vascular threat to limb at this stage of operation.
With 2 years of follow up, the patient has regained protective sensation to the extremity but has minimal motor functional return. Return of sensation is in the median nerve distribution. Consequently, no further diagnostic nerve function testing was undertaken. The patient currently is adaptive to the limited movement of the extremity, and no further surgical interventions are planned with continued observation.
Discussion
Constriction band syndrome represents a rare but potentially devastating developmental process that can lead to unfavorable outcomes. Controversy regarding the pathophysiology may limit a treatment consensus. Appropriate treatment options would vary if the etiology stems from a failure of formation or germ cell dysplasia versus physical banding from amnion rupture [Citation11,12]. In our particular example, the limb manifestation appears to have occurred at a later developmental stage, thus suggesting physical compression with normal prior organogenesis.
Peripheral nerve compression from congenital constriction band syndrome has been described previously [Citation8,9,22–24]. In most reported cases, there were neurosensory deficits with no motor dysfunction. Releasing the constricting band has been shown to result in return of sensation when performed early [Citation5,20].
Examples of motor nerve dysfunction are much less prevalent in the literature. It has been suggested that surgical exploration in the face of motor nerve dysfunction is futile due to lack of nerves existing distally [Citation25]. However, Weeks published the first case report describing surgical exploration of motor nerve paralysis not amenable to simple band decompression with evidence that distal nerves were present [Citation26]. In the constricted tissue, he observed neuroma formation within the radial nerve as it penetrated the intermuscular septum, requiring resection and sural nerve grafting. He explored the ulnar and median nerves at a later date due to concerns of vascular and lymphatic compromise. Although finding 2 cm severe compression of the nerves, he elected not to perform grafting due to intraoperative nerve stimulation, demonstrating distal function in the hand. In his follow up, he states that 15 months after his sural nerve graft, EMG revealed ‘severe scarcity of units in the wrist extensors’ and many fibrillations. He notes that there was some return of median and ulnar nerve function.
Although long-term outcomes are not presented here, we offer this case to raise the importance of thorough initial neurological examination and potential early surgical intervention in the treatment plan. Weeks’ suboptimal results after nerve grafting may have been due to the delay of almost 12 months to time of nerve exploration. The time frame of nerve regeneration or neurolysis after grafting may have exceeded the motor end plate viability. Further, the time to median and ulnar nerve neurolysis was 15 months in his case report with mild functional improvement. However, Jones et al. report three cases where motor dysfunction of the ulnar nerve was not returned after neurolysis at early age, thus suggesting more extensive distal nerve damage [Citation27].
We explored the constricted site and nerve grafted at 7 months of age. Had the patient been referred at an earlier date for longer observation of motor nerve function, we perhaps would have explored the arm sooner. The tissue within the constricted area was dense and fibrous. The cubital tunnel contained fibrous tissue that closely adhered to the ulnar nerve, making dissection difficult. Neurolysis alone was not undertaken due to the physical appearance of the nerve within the compressed tissue. Although this could be related to a developmental issue, there was a clear constriction band and much distal to the site of injury, the nerve appeared normal. The distal end of the cut nerve also had a normal fascicular pattern. Our results parallel Weeks’ in that we had minimal return of forearm and hand function. Performing the nerve grafting at the time of Z-plasty release may have ameliorated a lack of motor return since 4 months had lapsed between surgeries. The patient did show protective sensation return, suggesting that early exploration and grafting at the time of initial surgery may lead to improved results.
Preventing vascular compromise represented a challenging obstacle intraoperatively. Anterior dissection revealed total disruption of the median artery and no discernible radial or ulnar artery distally. During the operation, position changes caused extensive venous congestion and arterial insufficiency, thus suggesting collateralization as the only vascular provider around the elbow. We felt that addressing the radial nerve during this operation would have had critical vascular insult to the limb. Weeks similarly had concerns over lymphatic and vascular compromise and consequently staged his procedures [Citation26]. Interestingly, the patient did not demonstrate any edema or lymphedema in the postoperative period.
There is no a clear role regarding the use of perioperative imaging and testing in constriction band syndrome. EMG has been described as a method to determine the need for surgical intervention [Citation18,27]. However, utilizing EMG as a diagnostic choice is invasive and not significantly superior to physical examination alone. In this report, the physical examination provided all the details needed. There was an obvious site of pathology and an EMG and nerve conduction studies would not have added to the operative decision making given the clear site of injury. Intraoperatively, a normal caliber nerve was encountered proximally and distally to the site of the constriction band where the nerve was a thin, scarred structure without a neuroma. The proximal and distal ends were cut back until there was a normal fascicular pattern. Weinzweig and Barr found that intraoperative findings did not parallel electrodiagnostic studies performed at 3 months of age [Citation20]. We chose not to perform EMG to prevent further delay as well as senior surgeon preference due to some inconsistencies found in pediatric brachial plexus patients. In contrast, there may be a role with improving ultrasound technology in the preoperative planning and diagnosis of constriction band deformities [Citation28]. Fetoscopic release of banding has been described but come associated with high incidence of premature rupture of membranes [Citation29]. Severity of the contracture may be determined prenatally, allowing for earlier parent exposure, communication and operative planning.
Conclusion
Motor nerve dysfunction as a sequela of constriction band syndrome is a rare event. Timing of surgical intervention may prove crucial in optimizing functional outcomes. We present a case report demonstrating intact distal nerves, potentially repairable by nerve grafting. Limitations to complete peripheral nerve repair involved vascular compromise as a result of compression over the brachial artery. Imaging and nerve conduction studies were not felt to be warranted due to physical examination and may have delayed definitive correction.
Acknowledgment
Pictures used in this abstract were permitted after obtaining the informed consent by the legal guardian. Identifying details have been omitted.
Ethical Approval: This article does not contain any studies with animal subjects. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Patterson TJ. Congenital ring-constrictions. Br J Plast Surg 1961;14:1–31
- Foulkes GD, Reinker K. Congenital constriction band syndrome: a seventy-year experience. J Pediatr Orthop 1994;14:242
- Agashe MV, Rathod CM, Dhamele JA. Congenital pseudoarthrosis of the tibia with localised gigantism in a case of congenital constriction band syndrome. Indian J Plast Surg 2011;44:139–41
- Coady MS, Moore MH, Wallis K. Amniotic band syndrome: the association between rare facial clefts and limb ring constrictions. Plast Reconstr Surg 1998;101:640–9
- Nagore E, Sánchez-Motilla JM, Febrer MI, et al. Radius hypoplasia, radial palsy, and aplasia cutis due to amniotic band syndrome. Pediatr Dermatol 1999;16:217–19
- Siemers F, Wünsch L, Namdar T, et al. Complete circumferential congenital constriction of the trunk – operation procedures and results. Ger Med Sci 2011;9:Doc17
- Sarnat BG, Kagan BM. Prenatal constricting band and pseudoarthrosis of the lower leg. Plast Reconstr Surg 1971;47:547–51.
- Tada K, Yonenobu K, Swanson AB. Congenital constriction band syndrome. J Pediatr Orthop 1984;4:726–30
- Moses JM, Flatt AE, Cooper RR. Annular constricting bands. J Bone Joint Surg 1979;61A:562
- Montgomery WF. Observations in the spontaneous amputation of the limbs of the fetus in utero, with an attempt to explain the occasional cause of its production. Dublin Med J Chem Sci J 1832;1:140–4
- Streeter GL. Focal deficiencies in fetal tissues and their relation to intra-uterine amputation. Contrib Embryol 1930;22:1–41
- Torpin R. Amniochorionic mesoblastic fibrous strings and amniotic bands: Associated Constricting fetal malformations or fetal death. Am J Obstet Gynecol 1965;91:65
- Kino Y. Clinical and experimental studies of the congenital constriction band syndrome, with emphasis of its etiology. J Bone Joint Surg 1975;57A:636–43
- Van Allen MI. Fetal vascular disruptions: mechanisms and some resulting birth defects. Pediatr Ann 1981;10:219–33
- Goldfarb CA, Sathienkijkanchai A, Robin NH. Amniotic constriction band: a multidisciplinary assessment of etiology and clinical presentation. J Bone Joint Surg Am 2009;91:68–75
- Stevenson TW. Release of circular constricting scar by Z Flaps. Plast Reconstr Surg (1946) 1946;1:29–42
- Upton J, Tan C. Correction of constriction rings. J Hand Surg 1991;16A:947
- Hall EJ, Johnson-Giebink R, Vasconez L. Management of the ring constriction syndrome: A reappraisal. Plast Reconstr Surg 1982;69:532
- Di Meo L, Mercer DH. Single-stage correction of constriction ring syndrome. Ann Plast Surg 1987;19:469–74
- Weinzweig N, Barr A. Radial, ulnar, and median nerve palsies caused by a congenital constriction band of the arm: single-stage correction. Plast Reconstr Surg 1994;94:872–6
- Mutaf M, Sunay M. A new technique for correction of congenital constriction rings. Ann Plast Surg 2006;57:646–52
- Blackfield HM, Hause DP. Congenital constricting bands of the extremities. Plast Reconstr Surg 1951;8:101–9
- Uchida Y, Sugioka Y. Peripheral nerve palsy associated with congenital constriction band syndrome. J Hand Surg 1991;16B:109
- Flatt AE. Constriction ring syndrome: in the care of congenital hand anomalies. St. Louis: C. V. Mosby; 1977. p 213–27
- Moses JM, Flatt AE, Cooper RR, et al. Annular constricting bands. J Bone Joint Surg Am 1979;61:562–5
- Weeks PM. Radial, median, and ulnar nerve dysfunction associated with a congenital constricting band of the arm. Plast Reconstr Surg 1982;69:333–6
- Jones NF, Smith AD, Hedrick MH. Congenital constriction band syndrome causing ulnar nerve palsy: early diagnosis and surgical release with long-term follow-up. J Hand Surg 2001;26:467–73
- Paladini D, Foglia S, Sglavo G, et al. Congenital constriction band of the upper arm: the role of three-dimensional ultrasound in diagnosis, counseling and multidisciplinary consultation. Ultrasound Obstet Gynecol 2004;23:520–2
- Paletta CE, Huang DB, Sabeoiro AP. An unusual presentation of constriction band syndrome. Plastic Reconstr Surg 1999;104:171–4

