Abstract
Volar dislocations of the thumb metacarpophalangeal joint are uncommon and can be associated with rupture of the ulnar collateral ligament (UCL). We report a case where a volar thumb dislocation was successfully closed reduced, but instability required open repair of the UCL. Early motion protocol helped achieve favorable results.
Introduction
Dislocations of the thumb metacarpophalangeal (MCP) joint are generally infrequent injuries. Volar dislocations are much less common than dorsal dislocations, with the injury caused by hyperflexion of the thumb MCP joint or a force to the proximal phalanx in flexion [Citation1]. Singhal first reported a case of a volar MCP dislocation in 1974, and since then less than 30 cases have been reported in the English literature [Citation2,3]. The vast majority of these injuries are irreducible by closed means and open surgical reduction is often necessary [Citation1]. Many different structures have been identified as a possible block to closed reduction, including an entrapped volar plate, dorsal capsule, collateral ligaments, or interposition of the extensor tendons [Citation4].
In cases where closed reduction was successful, there were no findings of an ulnar collateral ligament (UCL) injury or instability to warrant surgical intervention [Citation1]. A recent case series reported two patients who had successful closed reduction at initial evaluation but at follow up were noted to have persistent instability and required a delayed (>7 days) UCL repair. These patients ultimately had long-term outcomes of persistent subluxation and stiffness significant to the point of ankylosis at the thumb MCP joint [Citation3]. We present the case of a volar thumb MCP joint dislocation where closed reduction under anesthesia was successful, but further examination revealed MCP instability and acute surgical repair of the ruptured UCL was performed. The patient was allowed to begin early range-of-motion (ROM) activities and achieved satisfactory results.
Case report
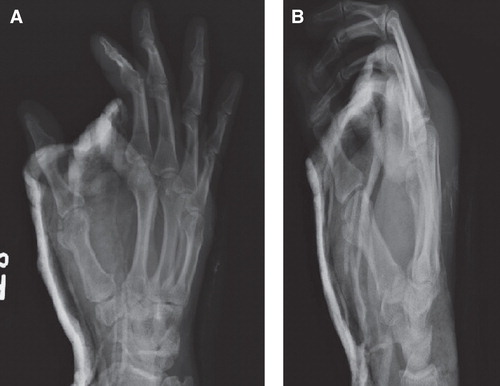
A 37-year-old right-hand-dominant male tripped over a curb and landed on his outstretched right upper extremity. He presented to the emergency department with pain and deformity over his right thumb MCP joint. X-rays obtained showed a volar dislocation of the thumb MCP joint. () A digital block was performed and closed reduction was attempted by hyperflexing the thumb MCP joint with a dorsally directed force applied over the volar base of the thumb metacarpal base. Closed reduction attempts were initially unsuccessful and the decision was made to take the patient to the operating room to perform a closed versus open reduction under anesthesia.
Figure 1. Anteroposterior (A) and lateral (B) view radiographs taken at time of injury demonstrate volar thumb metacarpophalangeal joint dislocation.
Once the patient was induced under general anesthesia, closed reduction of the thumb MCP joint was successful utilizing the same reduction maneuver. On further examination, the thumb had notable radial deviation at the MCP joint with stress testing. Valgus stress was applied to the thumb in neutral position as well as at 30° of flexion. This was confirmed under fluoroscopy with >30° of instability compared with the uninjured contralateral thumb, indicating a complete rupture of the UCL. An open approach was then performed where we were able to identify a complete mid-substance rupture of the UCL as well as disruption of the dorsal capsule and adductor aponeurosis. There was no transposition of tissue noted within the MCP joint. The UCL was primarily repaired with nonabsorbable sutures in a modified Kessler technique.
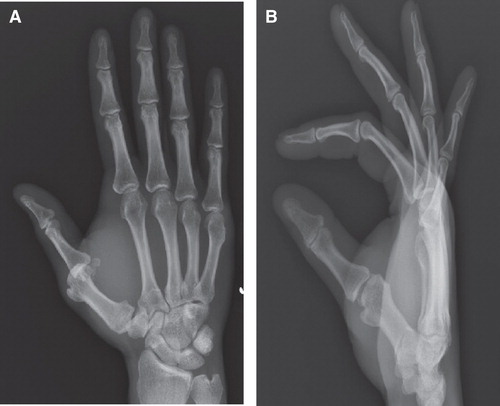
The patient was maintained in a thumb spica splint postoperatively for 2 weeks () after which flexion–extension exercises were begun. The patient was encouraged to perform aggressive ROM exercises five times daily. He was cautioned against forceful pinch or resisted motion of the thumb for an additional 3 weeks. He was maintained in a removable splint for an additional 4 weeks. At 6 months follow up, patient was noted to have stable and congruent MCP joint with fixed flexion deformity of 10° and 70° of flexion with no complaints of pain. At 1 year follow up, the patient continues to be pain-free and reports no limitations of activities. His Disabilities of the Arm, Shoulder, and Hand (DASH) score was 9.2.
Discussion
Although the unprotected position of the thumb leaves the MCP joint particularly vulnerable to injuries, volar MCP dislocations are very rare injuries. UCL injuries, however, are extremely common [Citation5]. The thumb MCP joint has little inherent skeletal stability, with the volar plate, capsule, and collateral ligaments being the primary stabilizers. Although the joint allows for multiplanar motion, the stability of the joint is paramount and a stable thumb MCP joint is critical for pinching and grasping [Citation5]. The collateral ligaments are the key constraints that impart stability to the joint, and missed collateral ligament injuries or delayed treatment can lead to poor operative outcomes or may necessitate arthrodesis [Citation6,7].
In a volar dislocation at the thumb MCP, the mechanism of injury is hyperflexion of the MCP joint or a force directed onto the dorsal proximal phalanx [Citation7]. Senda and Okamoto [Citation3] classified volar thumb MCP dislocations into three categories: stable, blocked, and unstable. Patients with stable dislocations can undergo successful closed reduction and usually have a partial UCL injury without Stener lesion. They do not require any operative intervention. Blocked dislocations are those that cannot be closed reduced, typically due to volarly displaced extensor tendons which block a closed reduction. These patients frequently have substantial UCL injury and should undergo repair at time of open reduction.
According to Senda and Okamoto, unstable volar thumb MCP dislocations are those with gross collateral ligament injury. Closed reduction is often successful, but the ligamentous injury leads to instability. Without collateral ligaments to stabilize the joint, the thumb flexors continue to cause palmar subluxation of the MCP. The authors reported that these patients in their series underwent a successful closed reduction at time of injury, but then had a delayed (>7 days after initial reduction) presentation of recurrent dislocation [Citation3]. The patients’ clinical stability after the initial reduction is unclear.
It has been suggested that closed reduction of a volar MCP dislocation, even with pinning, has a high rate of recurrent dislocation [Citation4,7]. However, it appears that the success of closed treatment of a volar thumb MCP dislocation is greatly tied to the management of the UCL. Whether reduced by closed or open means, it is important to assess the stability of the thumb MCP joint after reduction. Patients who had stable end points on stress examination and absence of Stener lesion after successful closed reduction of volar thumb MCP dislocation had satisfactory results with closed treatment [Citation1]. Partial rupture of the UCL generally heals uneventfully, and a stable examination of the thumb MCP joint is the most important factor even with an associated avulsion fracture [Citation8]. Missed UCL injuries can lead to chronic instability of the thumb MCP, painful arthritis, and impaired prehensile function of the thumb. Late UCL reconstruction (>3 weeks) after missed injury is more complex and the results are less successful compared to acute repair (within 3 weeks) [Citation5]. Instability of the MCP was diagnosed in our patient at the time of injury, allowing us to perform an acute repair and give the patient a greater chance of successful outcome.
When injuries to the UCL are diagnosed, operative management is indicated in cases with complete UCL tears with gross joint instability, presence of Stener lesion, and displaced bony avulsion injuries. Many operative treatment protocols advise immobilization of the thumb MCP joint for 4 weeks, and even include pinning the joint [Citation5,9]. In partial UCL ruptures as well, appropriate non-operative treatment consists of immobilization for up to 4 weeks [Citation6]. However, although this length of immobilization often achieves clinical stability, it is often associated with stiffness and decreased strength [Citation5,9]. Our patient was started with a range of motion protocol at 2 weeks and was able to obtain satisfactory motion while maintaining appropriate joint stability. Literature suggests that ligaments may heal stronger and faster with motion that stresses a repair, as prolonged immobilization may be detrimental to biomechanical remodeling of the ligament. While the repaired ligament is not as strong as the native UCL, biomechanical studies show that the strain in an intact UCL during active motion is three times lower than the strain where ligament ruptures occur [Citation10].
Although these are rare injuries, the treatment of volar dislocations of the thumb MCP can be challenging. In our patient, we were able to obtain a closed reduction under general anesthesia, but proceeded acutely with an open UCL repair due to considerable MCP instability on examination. This acute repair of the UCL and early ROM protocol were likely the most important factors in this patient’s successful return to function. As the thumb MCP is critical to prehensile activities, appropriate treatment of a dislocation and associated injuries is important for a return to everyday function. Although each case presents a complex problem, the present case demonstrates the treatment of a patient where surgical intervention was necessary for a concomitant injury even after a successful closed reduction of the MCP dislocation.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Beck JD, Klena JC. Closed reduction and treatment of 2 volar thumb metacarpophalangeal dislocations: report of 2 cases. J Hand Surg Am 2011;36:665–9
- Singhal RK. Anteromedial dislocation of metacarpophalangeal joint of the thumb with special emphasis on its mechanism of injury. J Indian Med Assoc 1974;62:18–20
- Senda H, Okamoto H. Palmar dislocation of the thumb metacarpophalangeal joint: report of four cases and a review of the literature. J Hand Surg Eur Vol 2014;39:276–81
- Moneim MS. Volar dislocation of the metacarpophalangeal joint. Pathologic anatomy and report of two cases. Clin Orthop 1983;176:186–9
- Helm RH. Hand function after injuries to the collateral ligaments of the metacarpophalangeal joint of the thumb. J Hand Surg Br 1987;12:252–5
- Lee AT, Carlson MG. Thumb metacarpophalangeal joint collateral ligament injury management. Hand Clin 2012;28:361–70; ix-x
- Wood MB, Dobyns JH. Chronic, complex volar dislocation of the metacarpophalangeal joint. J Hand Surg Am 1981;6:73–6
- Sorene ED, Goodwin DR. Non-operative treatment of displaced avulsion fractures of the ulnar base of the proximal phalanx of the thumb. Scand J Plast Reconstr Surg Hand Surg 2003;37:225–7
- Weiland AJ, Berner SH, Hotchkiss RN, McCormack RRJr, Gerwin M. Repair of acute ulnar collateral ligament injuries of the thumb metacarpophalangeal joint with an intraosseous suture anchor. J Hand Surg Am 1997;22:585–91
- Harley BJ, Werner FW, Green JK. A biomechanical modeling of injury, repair, and rehabilitation of ulnar collateral ligament injuries of the thumb. J Hand Surg Am 2004;29:915–20