Abstract
Primary malignant tumor of the parapharyngeal space (PPS) is rare. After surgical resection, primary closure could be considered if the oropharynx mucosa remains. This report describes two patients who underwent reconstruction by free tissue transfer after the resection of PPS tumors.
This report was presented at the 56th annual meeting of the Japanese Society of Plastic and Reconstructive Surgery, 4 April, 2013.
Introduction
The literature on reconstruction after resection of malignant parapharyngeal space (PPS) tumor is sparse. Although there have been a number of studies describing surgical approaches to PPS tumor excision, few studies have focused on reconstruction. In the patients of oropharynx reconstruction, it seems that most reconstructive surgeons reconstruct the parapharynx at the same time; thus it seems to be rare to just reconstruct the PPS. PPS tumors are rare and comprise approximately 0.5% of head and neck tumors. Moreover, 70–80% of these tumors are benign [Citation1]; therefore, malignant PPS tumors are quite uncommon. Nevertheless, in such patients, special attention is required during surgical treatment because the PPS has anatomical complexities. This space contains many important structures, including the internal carotid artery, the internal jugular vein, the last four cranial nerves, the sympathetic chain, and lymph nodes, including the node of Rouvière [Citation2]. It has been shown that PPS tumors expand medially or inferiorly due to the superior, posterior, and lateral bony limits of the space and, therefore, the common clinical symptoms are speech and swallowing problems due to medial distortion of the lateral oropharyngeal wall or soft palate [Citation3]. Functional reconstruction that facilitates speech and swallowing is required in patients with wide resection of the PPS tumor and the oropharyngeal wall, and this reconstruction should be performed with transferred tissue that has sufficient volume. In addition, important structures such as the internal carotid artery should be securely covered by muscle. This report describes two patients who underwent PPS tumor reconstruction at our institute.
Clinical reports
Patient 1
A 45-year-old woman complaining of right ear pain was first seen in a nearby hospital. Magnetic resonance imaging (MRI) revealed a tumor occupying the PPS with a size of 43 × 38 × 35 mm, which had the characteristics of a trigeminal nerve sheath tumor (), and the nearby hospital referred the patient to our hospital. Fine-needle aspiration cytology of the tumor revealed spindle or pleomorphic sarcoma. The patient underwent resection of the PPS tumor along with part of the middle constrictor muscle, internal pterygoid muscle, and palatine tonsil because of tumor invasion (), using a median mandibular osteotomy approach. The resected tumor had a size of 80 × 65 × 45 mm. A free rectus abdominis musculocutaneous flap, with a size of 35 × 50 mm after trimming, was transferred to cover the internal carotid artery and to compensate for the oropharyngeal defect (). The lingual artery and the external jugular vein were used as the recipient vessels, and one artery end-to-end anastomosis and one venous end-to-end anastomosis were performed. The transfer of a sufficient tissue volume and the use of the Gehanno method were important for the achievement of optimum velopharyngeal and oropharyngeal function. Total surgical time was 653 minutes and total blood loss was 410 ml. The histopathological examination revealed that the tumor was a carcinosarcoma that arose from the minor salivary gland. A postoperative lower mental gingival fistula occurred after surgery, but with conservative treatment, this complication healed in 3 weeks. Therefore, oral ingestion was started 30 days after surgery. About 9 months after surgery, solitary neck lymph node metastasis and lung metastatic recurrence appeared, even though the patient had received postoperative radiotherapy (60 Gy/30 Fr/51 days), which was the only adjuvant therapy that was used. The neck and lung metastatic recurrences required additional surgery. At present, 21 months after the first surgery, the patient is being followed up on an outpatient basis and has shown no further evidence of disease.
Figure 1. (a) Preoperative magnetic resonance T2 images of patient 1. (b, c) Illustrations showing patient 1 just after tumor resection. (b) The mandible osteotomy approach was selected. The resection resulted in a large oropharyngeal defect, and the internal carotid artery was exposed (black arrow). (c) Illustration showing the grossly resected tumor.
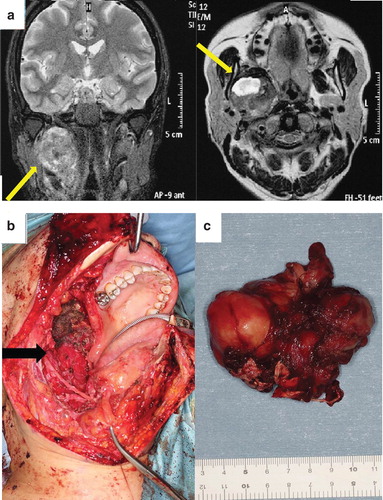
Figure 2. Illustrations showing the reconstruction of patient 1: (a) the rectus abdominis musculocutaneous flap. (b) The flap was transferred into the oroparapharyngeal space. The lingual artery and external jugular vein were used as the recipient vessels. (c, d) Illustrations showing the oropharynx immediately after surgery (c) and 3 weeks after surgery (d).
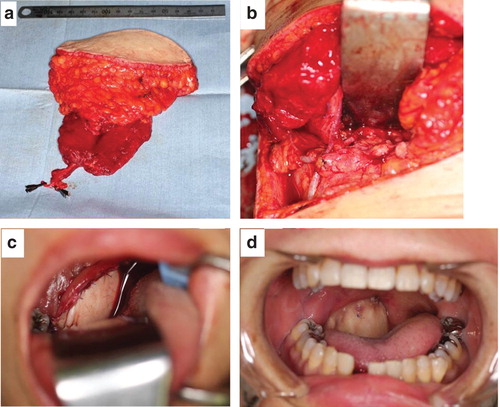
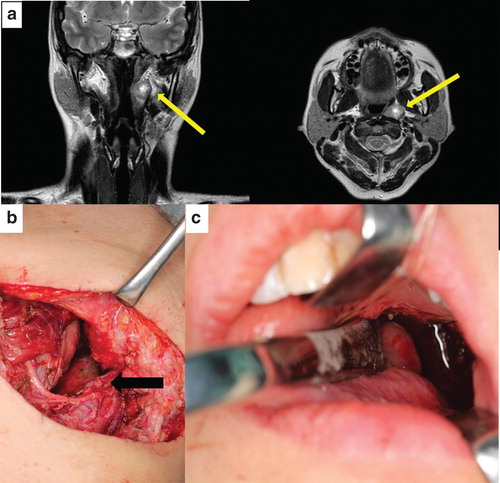
Figure 3. (a) Preoperative magnetic resonance T2 images of patient 2. (b, c) Illustrations showing patient 2 just after tumor resection. (b) Resection was achieved by using the cervical approach. The internal carotid artery was exposed (black arrow). (c) The oropharyngeal defect resulting from the resection is shown.
Patient 2
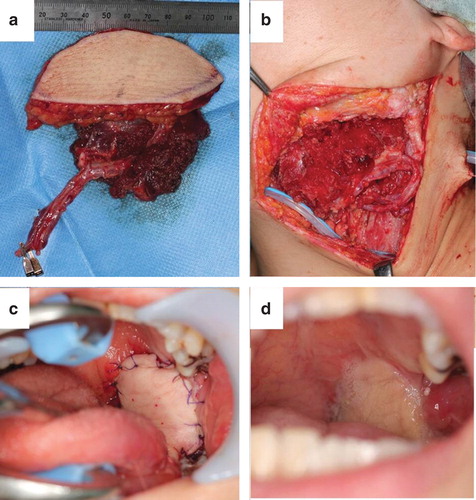
The second patient was a 40-year-old woman with malignant myoepithelioma of PPS, who had undergone two surgical interventions in the preceding 10 years without tissue transfer. However, biopsy of the tumor and MRI revealed a recurrent myoepithelioma occupying the PPS with a size of 17 × 13 × 19 mm. The positron emission tomography showed no lymphatic or systematic metastasis. The patient underwent resection of the PPS tumor along with part of the middle constrictor muscle, internal pterygoid muscle, and lateral part of the oropharynx wall. The mandibular osteotomy approach was not used, and the resected tumor had a size of 18 × 13 × 20 mm. A free anterolateral thigh vastus lateralis musculocutaneous flap with a size of 50 × 50 mm after trimming was transferred to cover the internal carotid artery and to compensate for the oropharyngeal defect (). The suprathyroid artery, the common facial vein, and the external jugular vein were used as the recipient vessels, and one artery end-to-end anastomosis and two venous end-to-end anastomosis were performed. The transfer of sufficient tissue volume and the use of the Gehanno method were important for the achievement of optimal velopharyngeal and oropharyngeal function. Total surgical time was 590 minutes and total blood loss was 175 ml. Histopathology revealed that the tumor was a malignant myoepithelioma. Oral ingestion was started 14 days after surgery. The postoperative course was uneventful and 13 months after the surgery, there were no signs of recurrence.
Figure 4. Illustrations showing the reconstruction on patient 2: (a) the anterolateral thigh vastus lateralis musculocutaneous flap. (b) The flap was transferred into the oroparapharyngeal space. The suprathyroid artery and common facial vein were used as the recipient vessels. (c, d) Illustrations showing the oropharynx immediately after surgery (c) and 4 months after surgery (d).
Discussion
Complete resection of the tumor, optimal functional reconstruction, and prevention of complications are key elements for successful PPS surgery.
Given the anatomical complexity of the PPS, surgical treatment of PPS tumors requires functional oropharynx reconstruction and covering of important structures such as the internal carotid artery and the internal jugular vein. In the two patients described here, a rectus abdominis musculocutaneous flap and an anterolateral thigh vastus lateralis musculocutaneous flap were transferred, respectively. In each reconstruction, the internal carotid artery and jugular vein were covered securely by the vascularized muscle to prevent infection. In addition, the transfer of muscle into the dead space of the PPS prevented pooling of blood or fluid and the development of hematoma or abscess. Several authors have reported that hematoma or dehiscence can occur after primary suture of the oropharyngeal mucosa following PPS tumor resection [Citation4,5]. We consider that muscle transfer effectively prevents such problems.
The key point of functional oropharynx wall reconstruction may be the transfer of sufficient tissue volume, allowing narrowing of the oropharynx, which is needed to generate velopharyngeal function and oropharyngeal swallowing pressure [Citation6-8]. Moreover, the Gehanno method, which was originally reported in 1985, has been shown to be an effective oropharyngeal reconstruction method [Citation9]. This technique aims to form a narrow border between the superior pharynx and the oropharynx such that nasal breathing is not disturbed and aims to restore the closing function of the nasopharyngeal cavity through the contractility of the pharyngeal myomucosal flap.
In our patients, the postoperative velopharyngeal function and swallowing were excellent because the oropharyngeal walls had been reconstructed by the transfer of sufficient tissue volume and by the Gehanno method.
In terms of the resection technique, several authors recommend the cervical approach, which provides good visibility and allows adequate exposure of the major vessels and nerves [Citation10,11]. However, several alternative osteotomy methods have also been proposed to improve surgical access to the PPS. Without mandible osteotomy, the removal of large tumors remains a blind procedure that increases the probability of tumor rupture and spillage in an otherwise accessible area [Citation12]. Among our patients, patient 1 underwent tumor resection with mandible osteotomy, which made it easy for the surgeon to suture the flap and pharynx and thus greatly facilitated the reconstruction procedure. Patient 1 did develop postoperative lower mental gingival fistula due to mucosal weakness, but with conservative treatment this complication healed in 3 weeks. Patient 2 underwent tumor resection without osteotomy. This hampered reconstruction because the working space was narrow, which made it difficult to suture the flap to the recipient site, but this patient did not have any major postoperative complications. Thus, we believe that although mandible osteotomy facilitates tumor resection and reconstruction, it may increase the risk of intraoral fistula.
Patient 1 had a lung metastatic recurrence 9 months after surgery that was treated by a lung surgeon. Patient 2 had no evidence of disease (follow-up period, 13 months). The small number of patients makes it difficult to assess the oncological efficacy of our methods, but our experiences with PPS tumor resection and reconstruction were instructive to us and may also be useful for other head and neck surgeons. Especially in cases of recurrent tumors, salvage after radiotherapy, and huge tumors, wide resection and tissue transfer reconstruction are required. We believe that patient quality of life is improved when complete tumor resection and functional reconstruction is performed with a sufficient volume of tissue and the Gehanno method.
Conclusion
Two rare occurrences of PPS tumors are reported here. One of the keys to successful PPS reconstruction is maintaining the dead space around the internal carotid artery. We believe that free musculocutaneous flap transfer should be the first choice for PPS reconstruction.
Declaration of interest: None of the authors has any financial interest in any of the products, devices, or drugs mentioned in this article.
References
- Batsakis JG, Sneige N. Pathology consultation: parapharyngeal and retro pharyngeal space disease. Ann Otol Rhinol Laryngol 1989;98:320–1.
- Nanson EM. The surgery of the deep lobe of the parotid salivary gland. Surg Gynecol Obstet 1966;122:811.
- Patten J. Neurological differential diagnosis. Oxford: University press; 1977. p 8–9.
- Papadogeorgakis N, Petsinis V, Goutzanis L, Lostakis G, Alexandridis C. Parapharyngeal space tumors: surgical approaches in a series of 13 cases. Int J Oral Maxillofac Surg 2010;39:243–50.
- O’Malley BWJr, Quon H, Leonhardt FD, Chalian AA, Weinstein GS. Transoral robotic surgery for parapharyngeal space tumors. ORL J Otorhinolaryngol Relat Spec 2010;72:332–6.
- Moerman M, Vermeersch H, Van lierde K, Fahimi H, Van Cauwenberge P. Refinement of the free radial forearm flap reconstructive technique after resection of large oropharyngeal malignancies with excellent functional results. Head Neck 2003;25:772–7.
- Inoue T, Nagata M, Yukawa H, Ogura M, Fujisawa T, Miyamoto M, et al. Evaluation of postoperative function in patients undergoing reconstruction following resection of superior and lateral oropharyngeal cancer: long-term outcomes of reconstruction with the Gehanno method. Int J Oral Maxillifac Surg 2012;41:9–16.
- Kimata Y, Uchiyama K, Sakuraba M, Ebihara S, Hayashi R, Haneda T, et al. Velopharyngeal function after microsurgical reconstruction of lateral and superior oropharyngeal defects. Laryngoscope 2002;112:1037–42.
- Gehanno P, Guēon C, Vēber P, Perreau P, Alalpuf P, Moisy N. Rēhabilitation vēlo-pharyngēe après bucco-pharyngectomie-trans maxillaire ēlargie a la region vēlo-palatine. Ann Oto-Laryng (paris) 1985;102:135–7.
- Wise RA, Baker HW. Tumours of the deep lobe of the parotid gland. Am J Surg 1960;100:323.
- Heenenman H, Maran AGD. Parapharyngeal space tumors. Clin Otolaryngol 1979;4:57.
- Flood TR, Hislop WS. A modified surgical approach for parapharyngeal space tumors: use of the inverted ‘L’ osteotomy. Br J Oral Mxillofac Surg 1991;29:82–6.

