Abstract
The purpose of this study is to demonstrate an occulting metastatic lung cancer diagnosed by a painful mass at right hand. Under early diagnosis and meticulous treatment, this patient has been painless without local recurrence and had full hand function for 3 years.
Keywords:
Introduction
Incidence of cancer metastases of the hand is low, accounting for 0.1% of all bone metastases. In the order of occurrence, the metastatic sites are in distal phalanges (21%), metacarpals (16%), and proximal phalanges (7%); the primary tumors of these metastases are of the lung (34%), gastrointestinal tract (25%), kidney (10%), and breast (5%) [Citation1,2].
Acrometastases may mimic benign tumors and other non-neoplastic conditions, thereby resulting in misdiagnosed and improper treatment [Citation3]. Metastases to terminal extremities are typically late manifestations of known malignancies. However, among patients with acrometastases, 16–30% of patients may have acrometastases as their first sign of malignancy [Citation1,4]. The presence of hand metastasis is a poor prognostic factor, and the patient’s life expectancy is approximately 7 months [Citation1]. This study reports the successful treatment of an acrometastatic lesion in a woman with lung cancer.
Case report
A 53-year-old nonsmoking woman noticed a painful mass over her left hand for 4 months. The tumor was mildly tender, 1 cm2 in size, and located on the dorsum of her left second finger. Plain radiographs revealed an osteolytic lesion with cortical expansion of her second metacarpal proximal to the metacarpal head (). According to the radiological features, we considered enchondroma, giant cell tumor, and malignancy as the most likely differential diagnoses. Due to the tumor being limited around metacarpophalangeal joint, we planned to organize an intralesional excisional biopsy and filled the bone defect with artificial bone grafts (Formosa bone graft, Formosa Biomedical Technology Corp.) to preserve the hand function as much as possible. Postoperatively, the pathology indicated a metastatic adenocarcinoma of pulmonary origin ().
Figure 1. (a) Preoperative plain film showing an expansile osteolytic lesion in the left second metacarpal bone. (b) Immediate postoperative plain film revealing a bone defect with a hyperdense mass. (c) Three-year postoperative plain film showing consolidation and remodeling of the bone lesion without fracture.
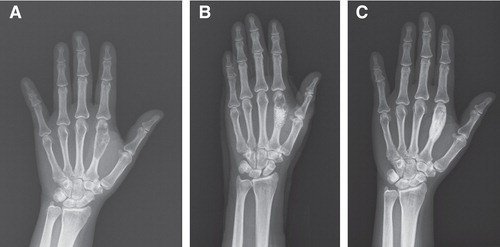
Figure 2. (a) Illustration of left second metacarpal bone showing metastatic adenocarcinoma composed of infiltrating nests of pleomorphic polygonal cells with focal glandular formation and intracytoplasmic vacuoles. (b) Tumor cells of the metastatic lesion (metacarpal bone) are immunoreactive for thyroid transcription factor-1 with nuclear staining. (c) Tumor cells of the metastatic lesion (metacarpal bone) are immunoreactive for cytokeratin 7 with cytoplasmic staining. (d) Histologically, the left lower lung shows features of adenocarcinoma similar to the metastatic lesion.
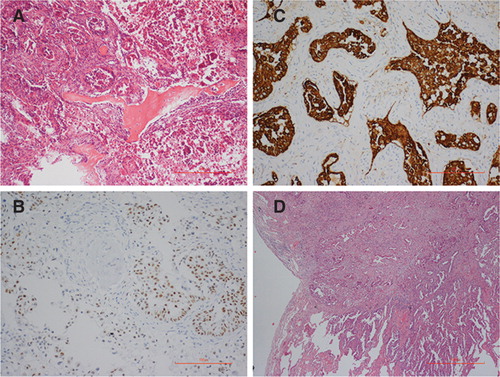
We employed contrast computed tomography (CT) from her chest to her pelvis. CT images of her chest showed a 1.5-cm pulmonary nodule with a spiculated margin in the right lower lobe without detectable lymph node metastasis (). No other metastasis was found after throughout examination. Three weeks after the surgery, the patient underwent video-assisted thoracic surgery involving wedge resection of the right lower lobe of the lung. The pathology showed adenocarcinoma, which is consistent with the metastatic lesion (). The final tumor staging was T2N0M1, according to American Joint Committee on Cancer (AJCC) seventh edition.
Figure 3. Chest computed tomography showing a 1.5-cm pulmonary nodule with spiculated margin in the right lower lobe (arrow).

After surgery, the patient received in combination with gemcitabine and gefitinib. She had regular follow up in our orthopedic and chest departments for more than 3 years. Serial plain film showed preserved left second metacarpal articular cartilage and evident consolidation of metacarpal acrometastases (). Currently, October 2014, she experiences no pain and demonstrates full range of motion in her hand.
Discussion
Acrometastasis is a rare disease, most likely because the distal part of upper extremities contains little red marrow and sluggish venous flow [Citation1]. Two hypotheses have been proposed to explain the mechanism of acrometastases: one is an increase in vascularity and the other is trauma-induced. Healey et al. [Citation5]. proposed that acrometastases more frequently affect the dominant hand than the non-dominant one. This finding was based on the assumption that the dominant hand involved comparatively heavier workloads and larger quantities of blood flow. Joll [Citation6] considered that frequent injury can destroy the surrounding tissue and can facilitate the deposition of tumor emboli in bones.
According to previous studies, they proposed that bone metastases are from hematogenous seeding. Pulmonary malignant cells have direct access to the arterial system; however, other visceral tumors are less likely because the tumor emboli are trapped in the hepatic and pulmonary capillary beds [Citation2]. This hypothesis explains why lung cancers account for most metastases of the hands.
Prognoses of acrometastases are poor and the average life expectancy is approximately 7 months [Citation1]. A number of modalities exist to treat this disease and control its local recurrence. First, amputation has been considered a reasonable option for treating acrometastases to distal phalanges [Citation2]. Where acrometastases involve the joint (such as in this case, which was proximal to the metacarpophalangeal joint), amputation causes impairment in hand function. Second, a previous study used radiotherapy to treat metastasis of the metacarpal, and promising results were reported [Citation2]. However, irradiation-induced pathological fractures should be of concern to physicians [Citation7]. Third, polymethylmethacrylate (PMMA) bone cement was an effective structural bone void filler. In some locally aggressive tumors, such as giant cell tumors, some physicians prefer to fill bone defects with PMMA and elevate the temperature in polymerization to kill residual tumor cells [Citation8].
Good primary tumor and metastatic tumor control are due to targeted therapy [Citation9]. The local intralesional excision, alcohol ablation, and impaction artificial bone grafting are salvage procedures for preventing further cortical collapse and deformation of the metacarpal. The patient has adhered to follow up for more than 3 years, and she is free of pain and has full range of motion in the affected hand. Compared with ray amputation and wide excision, the salvage procedure can preserve more function and is cosmetically acceptable. Although previous research reported a zero bone-healing rate involving pathological fractures of pulmonary origin [Citation10], this patient exhibited bone-healing potentials in a metastatic lesion. We observed that artificial bone grafting for reconstructing bone defects after performing intralesional excision can enhance bone formation. Further research is necessary to establish the role of bone grafting in metastatic bone tumors of pulmonary origin.
Acknowledgments
The authors report no conflicts of interest. WCL wrote the manuscript after reviewing relevant articles. CKL and SHC performed the surgery and followed up the patient. CCW conducted the pathological examination. WCL, CJH, YCF, and SHC edited the final manuscript, which all of the authors approved.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Reference
- Afshar A, Farhadnia P, Khalkhali H. Metastases to the hand and wrist: an analysis of 221 cases. J Hand Surg Am 2014;39:923–32; e17
- Flynn CJ, Danjoux C, Wong J, Christakis M, Rubenstein J, Yee A, et al. Two cases of acrometastasis to the hands and review of the literature. Curr Oncol 2008;15:51–8
- Kerin R. The hand in metastatic disease. J Hand Surg Am 1987;12:77–83
- Borgohain B, Borgohain N, Khonglah T, Bareh J. Occult renal cell carcinoma with acrometastasis and ipsilateral juxta-articular knee lesions mimicking acute inflammation. Adv Biomed Res 2012;1:48
- Healey JH, Turnbull AD, Miedema B, Lane JM. Acrometastases. A study of twenty-nine patients with osseous involvement of the hands and feet. J Bone Joint Surg Am 1986;68:743–6
- Joll CA. Metastatic tumours of bone. Br J Surg 1923;11:38–72
- Wu JS, Wong R, Johnston M, Bezjak A, Whelan T; Cancer Care Ontario Practice Guidelines Initiative Supportive Care G. Meta-analysis of dose-fractionation radiotherapy trials for the palliation of painful bone metastases. Int J Radiat Oncol Biol Phys 2003;55:594–605
- Klenke FM, Wenger DE, Inwards CY, Rose PS, Sim FH. Giant cell tumor of bone: risk factors for recurrence. Clin Orthop Relat Res 2011;469:591–9.
- Gilardi R, Rosa ND, Pancaldi G, Landi A. Acrometastasis showing an occult lung cancer. J Plast Surg Hand Surg 2013;47:550–2.
- Biermann JS, Holt GE, Lewis VO, Schwartz HS, Yaszemski MJ. Metastatic bone disease: diagnosis, evaluation, and treatment. J Bone Joint Surg Am 2009;91:1518–30

