Abstract
Endoscopic-assisted techniques in plastic and craniofacial surgeries are limited. We present a patient with infraorbital nerve entrapment following traumatic facial injury that failed conservative management. Compression of the nerve was treated with an endoscopic-assisted nerve release of the surrounding soft tissue with a circumferential foraminal osteotomy.
Introduction
Endoscopic techniques have become widely available to multiple surgical disciplines [Citation1]. From its inception in gynecologic surgery, minimally invasive technology gained momentum and was largely applied to general surgery. However, its use in plastic surgery is limited. Procedures that have incorporated total endoscopic approaches include carpal tunnel, ulnar nerve, and tarsal tunnel release [Citation2-4]. Other procedures specific to the craniofacial region have established endoscopic-assisted surgical techniques [Citation5]. An increasing body of evidence in the neurosurgery and otolaryngology literature supports the use of endoscopic techniques as well [Citation6-9].
The advantages of using endoscopic techniques include improving visualization of the surgical field, optimizing maneuvers in complex and tight spaces, decreasing hospital stay, decreasing incision size, and minimizing postoperative pain [Citation5]. Although plastic and reconstructive surgeons do not traditionally utilize endoscopic approaches in craniofacial surgery, a novel endoscopic-assisted technique is described that may be of great value to the surgeon and the patient. Below we present a patient with infraorbital nerve (ION) entrapment following traumatic injury that is treated with endoscopic-assisted nerve release and circumferential foraminal osteotomy. The ION is the terminal branch of the maxillary nerve and has a significant topography supplying sensation to the skin and mucosa of the midface. Anatomic studies have shown that the surface area covered by this nerve extends superiorly to the lower eyelid margin, laterally to the lateral canthus of the eyes, inferiorly to the oral commissures and medially to 0.5 cm to midline. The nerve is vulnerable to injury especially with midface access procedures to the maxilla [Citation10]. Loss of sensation or severe pain has been reported in patients when the nerve has been injured [Citation10]. However, patients with worsening symptoms may benefit from surgical intervention, which can diagnose nerve entrapment and treat it simultaneously [Citation11,12]. To our knowledge, the use of endoscopic-assisted techniques for diagnosis and treatment of infraorbital nerve entrapment has not previously been reported and is the first of its kind.
Case report
A 35-year-old Caucasian male presented to our clinic with pain (visual analog scale 7/10) over the left infraorbital nerve distribution. Two months prior, the patient sustained a left zygomaticomaxillary complex (ZMC) and orbital fracture following blunt facial trauma. He had previously undergone a trial of pregabalin for neuropathic pain, which failed to resolve his symptoms. Six months following injury, the patient reported worsening pain (visual analog scale 9/10). Clinical examination revealed exquisite tenderness to light palpation over the infraorbital nerve radiating to the maxillary teeth.
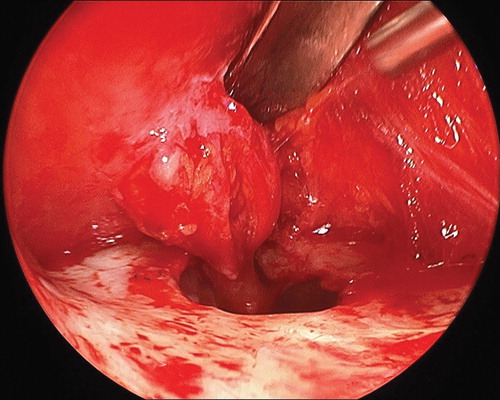
A computerized tomography scan of the head at the time of his accident showed possible compression of the infraorbital nerve. The patient underwent an endoscopic infraorbital nerve decompression and circumferential osteotomy of the infraorbital foramen. The left upper buccal sulcus was incised and dissection was carried out in the subperiosteal plane to the maxilla. A Tessier elevator was then used to carefully lift periosteum and scar to allow access for a 30° endoscope (Stryker, San Jose, CA, USA). Visualization of the left infraorbital nerve and the infraorbital foramen revealed multiple soft tissue adhesions from the anterior soft tissue causing nerve compression (). Endoscopic visualization allowed for precise adhesiolysis using long tenotomy scissors with preservation of the nerve and its branches revealing viable neural tissue.
Figure 1. Illustration showing the infraorbital nerve entrapment with visualized soft tissue adhesions and bony narrowing.
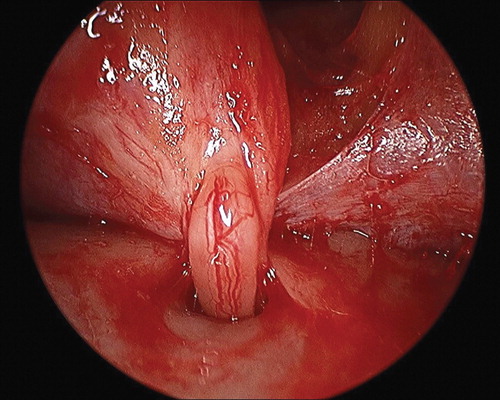
A 1-mm osteotome was then used to perform a circumferential osteotomy of the left infraorbital foramen in a box-like fashion (). The endoscope was then introduced into the foramen to visualize nerve tracking posteriorly ensuring that there was no proximal impingement. Closure of the buccal mucosa resulted in a 1.5-cm scar which was much smaller than a standard sulcus access incision. The patient reported immediate resolution of symptoms following the procedure. On 3-year follow up, the patient remained symptom-free.
Discussion
The use of endoscopic-assisted techniques in craniofacial surgery is seldom used by plastic surgeons, but several procedure-specific approaches have shown promise. Authors have reported success in applying endoscopic approaches to craniosynostosis repair, frontal cranioplasty, facial fractures, and cosmetic brow lifts [Citation13-17]. Recently, endoscopy has been incorporated in maxillofacial surgery for parotid tumor resection and dental implant placement [Citation18,19]. These techniques also have a role in cranial nerve release, as depicted in our case report and previous reports of supraorbital neurolysis in the treatment of chronic migraine [Citation12,20] and nerve entrapment [Citation11,12]. The major criticism of endoscopy is the associated increased cost of equipment, but many facilities have already purchased and are utilizing these instruments for other surgeries. Another major deterrent is the learning curve associated with learning novel technical procedures. The benefits of endoscopic techniques are apparent across various surgical procedures and have shown to reduce operative times, length of hospital stay, and costs, compared to open procedures [Citation5]. As such, the likelihood of expanding the use of endoscopy in plastic surgery is likely inevitable.
The decision-making process in treating this patient was dependent on accurate diagnosis and worsening symptoms. Although many patients sustaining a ZMC fracture may develop a neuropraxia, conservative non-operative management with close follow up will often lead to resolution of pain within months. Although this treatment strategy was pursued and later augmented with medical therapy, the severity of the patient’s symptoms worsened with intractable pain. At this point, the diagnosis of a post-traumatic neuropraxia was in question and a suspicion for trigeminal neuralgia secondary to nerve entrapment became a concern. The use of botulinum toxin injections were considered as they may offer symptomatic relief for patient with trigeminal neuralgia [Citation21,22], but often the treatment is not curative and requires multiple visits for routine injections that may leave the patient with unsightly facial asymmetry [Citation23]. The patient did not live in close proximity to our office nor did he welcome the idea of recurrent visits for chronic injections.
To surgically correct suspected nerve entrapment, direct visualization was necessary to confirm the diagnosis and subsequent adhesiolysis and osteotomy would serve to relieve tension and compression of the ION. Clauser and Tieghi [Citation24] describe a transconjunctival open approach to decompress the ION, but this approach was avoided due to the patient’s prior orbital injury. Rather an aesthetically hidden incision through the buccal sulcus was used to access the ION. In an effort to limit the size of incision, degree of tissue manipulation, and optimize visualization for the procedure, an endoscopically assisted approach was chosen. Although repair of the ZMC fracture was considered, the patient’s fracture was non-comminuted and non-displaced precluding the need for surgical correction.
Our approach maintained a cosmetically conscious approach by avoiding a larger incision, while safely dissecting through a relatively avascular plane. The 4 mm 30° endoscope allows for an easier inspection of an extremely narrow space around the infraorbital nerve. The endoscope also provides a better optical resolution of the surgical field under higher levels of magnification but comes at the cost of a narrower field of vision. Maintaining a subperiosteal plane of dissection minimized blood loss and provided a clearer image on the monitor. Similarly, Boustred described an endoscopic excision of a supraorbital Schwannoma, using a small hairline incision and 0° endoscope [Citation25]. The patient went home the same day. In our case, minimal trauma to the tissue allowed for a speedy recovery as he was discharged home the same day of surgery.
The purported benefits of endoscopic-assisted techniques are well described, but they cannot be extrapolated to all surgery. The potential for applying endoscopic-assisted techniques to craniofacial surgery is apparent and should be explored. There is a lack of consensus for determining absolute indications or contraindications for endoscopic-assisted cranial nerve release. The short- and long-term sequelae of this novel technical approach requires more studies as success rates must be compared to conventional methods of open surgery. This case serves as a reminder that endoscopy can aid the craniofacial surgeon and should be kept in one’s treatment armamentarium.
Conclusion
The novel description of an endoscopic-assisted approach to decompress the infraorbital nerve is a minimally invasive technique that provides better visualization for adhesiolysis, nerve dissection, circumferential osteotomy, and it decreases the manipulation of tissue with that of an open approach. As endoscopic techniques evolve and surgeons become more adept at incorporating endoscopy into craniofacial surgery, we advocate this approach to decompress the infraorbital nerve.
Declaration of interest: Dr Christy has received research and educational grant support and speaker honoraria for unrelated activities from DePuy Synthes CMF, Osteomed and KLS Martin. The rest of the authors do not have any disclosures or conflicts of interest.
References
- Spaner SJ, Warnock GL. A brief history of endoscopy, laparoscopy, and laparoscopic surgery. J Laparoendosc Adv Surg Tech A 1997;7:369–73
- Hansen TB, Majeed HG. Endoscopic carpal tunnel release. Hand Clin 2014;30:47–53
- Flores LP. Endoscopically assisted release of the ulnar nerve for cubital tunnel syndrome. Acta Neurochir (Wien) 2010;152:619–25
- El Shazly O, El Shazly A, Desouky A, El Zohiery AK, Sakr HM. Anatomical bases of endoscopic tarsal tunnel release: anatomical and ultra–sonographic study with a preliminary clinical report. Surg Radiol Anat 2011;33:929–36
- Francis CS, Wong RK, Cohen SR. Endoscopic delivery of calcium phosphate cement for secondary craniofacial reconstruction. J Craniofac Surg 2012;23:2057–60
- Krischek B, Godoy BL, Zadeh G, Gentili F. From craniofacial resection to the endonasal endoscopic approach in skull base surgery. World Neurosurg 2013;80:56–8
- Gendeh BS, Salina H, Selladurai B, Jegan T. Endoscopic--assisted craniofacial resection: a case series and post–operative outcome. Med J Malaysia 2007;62:234–7
- Nicolai P, Castelnuovo P, Bolzoni Villaret A. Endoscopic resection of sinonasal malignancies. Curr Oncol Rep 2011;13:138–44
- Ben Simon GJ, Schwarcz RM, Mansury AM, Wang L, McCann JD, Goldberg RA. Minimally invasive orbital decompression: local anesthesia and hand–carved bone. Arch Ophthalmol 2005;123:1671–5
- Hillerup S. Iatrogenic injury to oral branches of the trigeminal nerve: records of 449 cases. Clin Oral Invest 2007;11:133–42
- Ramirez OM, Pozner JN. Endoscopically assisted supraorbital nerve neurolysis and correction of eyebrow. Plast Reconstr Surg 1997;755–8; discussion 759–760
- Adant JP, Bluth F. Endoscopic supraorbital nerve neurolysis. Acta Chir Belg 1999;99:182–4
- Cohen SR, Holmes RE, Ozgur BM, Meltzer HS, Levy ML. Fronto–orbital and cranial osteotomies with resorbable fixation using an endoscopic approach. Clin Plast Surg 2004;31:429–42
- Tawfilis A. Subperiosteal endoscopic cranial augmentation (SECA): endoscopic approach to cranioplasty. J Oral Maxillofac Surg 2003;61:145–7
- Warner J, Wang TD, Marcus BC. Frontal cranioplasty: the endoscopic approach. Plast Reconstr Surg 2008;121:341–2
- Jacobovicz J, Lee C, Trabulsy PP. Endoscopic repair of mandibular subcondylar fractures. Plast Reconstr Surg 1998;101:437–41
- Chiu ES, Baker DC. Endoscopic brow lift: a retrospective review of 628 consecutive cases over 5 years. Plast Reconstr Surg 2003;112:628–33
- Li B, Zhang L, Zhao Z, Shen G, Wang X. Minimally invasive endoscopic resection of benign tumours of the accessory parotid gland: an updated approach. Br J Oral Maxillofac Surg 2013;51:342–6
- Beltrán V, Fuentes R, Engelke W. Endoscopic visualization of anatomic structures as a support tool in oral surgery and implantology. J Oral Maxillofac Surg 2012;70:1–6
- Liu MT, Chim H, Guyuron B. Outcome comparison of endoscopic and transpalpebral decompression for treatment of frontal migraine headaches. Plast Reconstr Surg 2012;129:1113–19
- Ngeow WC, Nair R. Injection of botulinum toxin type A (BOTOX) into trigger zone of trigeminal neuralgia as a means to control pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:47–50
- Kitamura Y, Matsuka Y, Spigelman I, Ishihara Y, Yamamoto Y, Sonoyama W, et al. Botulinum toxin type a (150 kDa) decreases exaggerated neurotransmitter release from trigeminal ganglionneurons and relieves neuropathy behaviors induced by infraorbital nerve constriction. Neuroscience 2009;159:1422–9
- Hu Y, Guan X, Fan L, Li M, Liao Y, Nie Z, et al. Therapeutic efficacy and safety of botulinum toxin type A in trigeminal neuralgia: a systematic review. J Headache Pain 2013;14:72
- Clauser L, Tieghi R. New mini-osteotomy of the infraorbital nerve in bony decompression for endocrine orbitopathy. J Craniofac Surg 2010;21:222–4
- Boustred AM. Endoscopic excision of a supraorbital schwannoma. Ophthal Plast Reconstr Surg 2007;23:66–2368