Abstract
Objective:
Joint pain and swelling during gout flares may lead to considerable morbidity and disability, having an impact on patient work productivity and social participation. The objective of this study was to assess how gout flares affect these activities in patients with chronic gout refractory to conventional therapy.
Methods:
A 1-year prospective observational study was conducted among patients with symptomatic disease in the United States in 2001. Inclusion criteria required patients (1) to be age 18 years or older, (2) to have documented, crystal-proven gout, (3) to have symptomatic gout, and (4) to be intolerant or unresponsive to conventional therapy, reflected by SUA ≥ 6.0 mg/dL. Patients were evaluated every 2 months. At each visit, patients completed a gout diary, which included number of flares experienced, duration and severity of each flare, and whether the flare caused: (1) work loss, (2) missed appointments or social events, or (3) impairment of self-care activities. The Short-Form Health Survey (SF-36) was also completed each visit.
Results:
Analyses were restricted to those who completed the first 6 months of the study (n = 81). Mean number of flares per patient per year was 8.8. Of the patients who were <65 years, 78% reported at least 1 work day lost due to a gout attack during the year. Mean annual work day loss for those <65 years was 25.1 days. A total of 545 of patients reported at least one flare per year that impaired social activities, with a mean of 17.1 social days lost and 52% reported at least one flare per year that compromised normal self-care activities, with a mean of 16.9 days impairment. Correlations between the diary reports and activity-related questions from the SF-36 were significantly positive.
Limitations:
The study is limited by small sample size, lack of reference group, and inability to explicitly collect employment information. Age under 65 years was used as a proxy for employment eligibility.
Conclusion:
Flares in patients with chronic gout refractory to conventional therapy significantly affect patient work productivity and social activities.
Introduction
Gout is a disorder in which urate crystal deposition in joints and soft tissues results in episodic acute arthritis and can ultimately lead to chronic arthropathy and tophus formation. Management of recurrent or progressive gout aims to reduce and maintain serum uric acid (SUA) levels below 6.0 mg/dL, a goal usually requiring a urate-lowering agent such as a xanthine oxidase inhibitor (e.g., allopurinol or febuxostat), a uricosuric agent (e.g., probenecid) or both.
Progression of gout to a chronic disabling disorder is encountered most often among patients who are intolerant to currently available urate-lowering agents or who have medical comorbidities limiting their use; persons not prescribed or not adherent to sufficient urate-lowering therapy; and patients with organ transplants whose immunosuppressant therapy may diminish renal function and result in hyperuricemia.
Chronic gout that is refractory to conventional urate-lowering therapy with a high burden of symptoms, such as frequent flares and tophi, is estimated to occur in approximately 25,000–100,000Citation1 of the 3–6 million Americans who suffer from goutCitation2,Citation3. Prevalence of gout of all types is believed to be increasingCitation4–9.
The economic burden of treatment-refractory chronic gout contributes disproportionately to the overall healthcare burden of the gout population. A study of the insurance claims (1999–2005) of 13 million beneficiaries in 40 private health plans in the US, estimated that older adults (≥65 years) with gout and SUA levels greater than 9 mg/dL incurred an additional $3,100 per year in incremental costs as compared to those with SUA levels below 6 mg/dLCitation10. In addition, the study found that presence of tophi contributed an additional $5,500 in regression-adjusted all-cause health care costsCitation10.
The loss of work and social activity in a population of patients with chronic gout refractory to conventional urate-lowering therapy has not been previously reported, although two studies have examined productivity loss in the general gout population. As reported by Roubenoff (1990)Citation11, the National Health Interview Survey, self-identified gout patients reported that gout restricted their activities an average of approximately 16.8 days per year. An analysis of absenteeism records of 300,000 employees of several large US employers found that 1,171 gout patients missed work an average of approximately 4.6 more days than the employees without goutCitation12. Another analysis of the same data included a calculation of the productivity dollar difference between gout and non-gout as $1,337, including sick leave, short-term disability, long-term disability, and worker’s compensationCitation13. Patients with chronic gout refractory to conventional therapy generally have greater disease burden and are likely to experience greater compromise in productivity.
To gain a better understanding of treatment-refractory chronic gout, a natural history study has been conducted in which individuals with chronic gout refractory to conventional urate-lowering therapy were followed for up to 1 year. Results on health-related quality of life and functional ability have been publishedCitation14. The results indicated that treatment-refractory chronic gout is associated with functional disability and poor health-related quality of life. This adverse impact is especially prominent for patients who experience more gout flares and have a greater number of involved joints.
The objective of the present analysis of this longitudinal natural history study was to determine the effect of gout-related disability on work productivity and other daily activities in patients with treatment-refractory chronic gout. Newer therapeutic agents in development promise to provide the opportunity for much needed improvement in signs and symptoms and patient outcomes in the difficult to manage gout populationCitation15. The effects of the disease on productivity would help evaluate the economic value of these new drugs.
Patients and methods
Patient population
A 1-year prospective observational study was conducted among patients with symptomatic disease at 24 sites in the United States in 2001. Inclusion criteria required patients (1) age 18 years or older, (2) to have documented, crystal-proven gout, (3) to have symptomatic gout, and (4) to be intolerant or unresponsive to conventional therapy, reflected by SUA ≥ 6.0 mg/dL. Symptomatic gout was defined as having at least one of the following: recurring gout flares (≥3 per year); chronic synovitis/arthropathy; presence of tophi confirmed by radiographic or physical examination; or uric acid nephrolithiasis/nephropathy. No restrictions were placed on concurrent medications or proceduresCitation14.
Evaluation
Following a baseline visit, subjects were evaluated at 2-month intervals for 12 consecutive months. During each follow-up visit, subjects completed a symptom diary, in which they were instructed to record information on the overall severity of pain within the preceding 2-month period and on any flare experienced within that time, including the duration of attack, severity (using visual analog scale), joint(s) affected, and treatment. A gout flare was defined as any worsening of signs or symptoms that required the attention of a physician or required the subject to take new medication or an increased dosage or frequency of his/her current gout medication. For each flare, the subject was asked ‘As a result of this flare, were you (check all that apply): unable to perform your usual work, unable to make an appointment or social event, or unable to take care of yourself as you normally do?’ The responses were assumed to apply for the entire duration of the flare. Self-reported quality of life was measured at each visit using the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36; Version 1)Citation16 (SF-36 is a registered trademark of Medical Outcomes Trust.). For each flare, patients were also asked to report whether it resulted in an emergency room or hospital visit (along with the length of stay).
Statistical analysis
The number of flares experienced per year, flare duration, and the related days lost per year for work, social activities and personal care were derived from the symptom diary described above. All results presented are based on descriptive analysis as there is no comparison group evaluated in the study. Because the study did not include questioning the subjects regarding their employment status explicitly, age less than 65 years was used as a proxy for employment eligibility.
Work day loss was computed only for subjects under the age of 65 years. Confidence intervals were calculated for key outcomes assuming Student’s t-distribution. The work and social activity-related items of the SF-36 were analyzed for correlation to the diary data (Pearson correlation coefficients).
While some subjects completed a total of 12 months of study, the analyses were restricted to those who completed at least 6 months of follow-up visits to ensure an adequate sample of time. Because of the intermittent nature of gout flares, the numbers of flares for subjects who completed less than the full 12 months of the study were prorated in order to estimate the numbers for a full year. These projected values were also calculated based on person-years of follow-up (i.e., weighting by person-year rather than by person). No significant differences between the two methods were found.
Calculations were performed with STATA 10 Software from StataCorp (College Station, TX, USA).
Results
A total of 110 subjects were enrolled in the natural history study. At least 6 months of observation were completed for 81 (74%) of the subjects, qualifying them for this analysis. Four subjects died during the course of the study.
The original study was planned for a total follow-up of 12 months, but was discontinued prematurely due to the non-interventional nature of the study in patients with significant disease burden. Of the 81 evaluable patients, 59 (73%) had 12 months of follow-up and 22 (37%) had 6–11 months of follow-up. Of the 81 subjects, 65 (80.2%) had flare diary data of sufficient quality for evaluation of flare occurrence and duration.
Baseline characteristics of study subjects are summarized in . A total of 78% were male and 63% were under the age of 65 years (range 35–90). In all, 15% of subjects reported one or two acute attacks (flares), 63% reported three to six, and 22% reported more than six acute attacks during the year prior to their baseline visit. A total of 74% had tophi. Physicians assessed 29% of the subjects as ‘chronically incapacitated’ based on a yes/no response.
Table 1. Patient characteristics.
Outcome results for the patients with evaluable flare data are summarized in . During the follow-up period, subjects suffered a mean of 8.8 flares per year (median 6, 95% CI [7.0, 10.7]). The mean duration of each flare was 5.3 days (median 4, 95% CI [4.2, 6.3]), and mean self-reported severity on a 0–10 scale was 5.7 (median 6, 95% CI [5.1, 6.4]).
Table 2. Flares and activity loss.
Work productivity
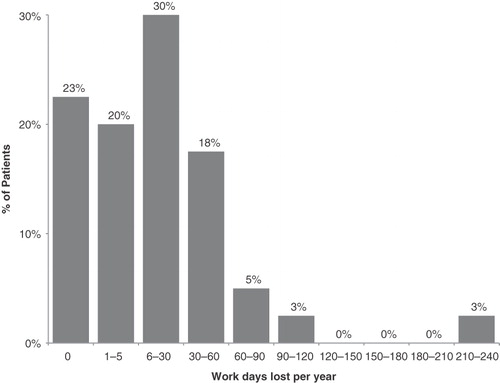
A total of 78% of subjects who were less than 65 years of age reported at least one flare causing absence from work. The mean total work day loss was 25.1 days per year (median 12, 95% CI [11.7, 38.6]), including patients reporting no work loss. As the mean number of flares for patients under age of 65 was 8.1 per year, the average work loss per flare was approximately 3 days. The distribution of work-day loss per year among subjects is shown in .
Self-care and social activity
In all, 52% of patients reported at least one flare per year that compromised normal self-care activities; the overall mean was 16.9 days of impairment (median 3, 95% CI [7.7, 26.1]). A total of 54% of patients reported at least one flare per year that impaired social activities; the overall mean was 17.1 social days lost (median 4, 95% CI [7.7, 26.7]).
The extent to which gout affected work productivity, self-care, and social activity is associated with baseline severity. As shown in , subjects who reported a history of greater than six flares per year prior to study entry had more than twice the work days lost per year; social activities and personal care compared to those who experienced 1–2 flares per year.
Table 3. Mean activity days lost as a function of baseline number of flares per year.
Correlations between the gout diary reports and activity-related questions from the SF-36 were significantly positive, ranging from 0.39 to 0.56. summarizes the correlations between SF-36 measures and diary reports. Full results on health-related quality of life in this longitudinal natural history study have been published elsewhereCitation14.
Table 4. Correlations* between SF-36 and diary-reported measures of activity loss, age <65 years, n = 40.
Seven of the 65 subjects who had flare diary data (10.8%) reported a total of 14 visits to the emergency room due to flares during the course of the study, corresponding to a mean of 0.22 visits per patient per year. Four patients (6.2%) had a total of nine flare-related hospital visits, corresponding to a mean of 0.14 visits per patient per year. The average length of stay per visit was 3.7 days.
Discussion
This longitudinal natural history study is the first prospective study to evaluate the loss of activity for work, self-care and social function, as well as health-related quality of life in patients with chronic gout refractory to conventional urate-lowering therapy. The results of the study demonstrate that treatment-refractory chronic gout significantly affected patients’ work-related, self-care, and social activities. Based on the average 2006 US wage rate of $19.30 per hour, the mean of 25.1 work lost days would result in an approximately $3,900 per patient per year cost (median $1,850, 95% CI [$1,800, $6,000]). A mean of 17.1 social days and 16.9 self-care days were lost per patient per year.
The study findings suggest that, compared to gout population in general, patients who are refractory to conventional urate-lowering therapy are subject to significantly more work productivity and social activity loss. Previous studies described in the Introduction reported an average of 4.6–16.8 days per year of missed work daysCitation11,Citation12 and a total of $1,337 indirect costs associated with gout.
The present study has several limitations that limit the extent to which it can be generalized. The study examines a small sample size with limited follow-up and does not have a gout-free or moderate-gout control population. In terms of lost work productivity, the study did not explicitly collect employment information, so retirement age (65 years) was used as a proxy. There is at least a two-part limitation to using the subject’s age as a proxy for employment eligibility. It fails to address those subjects younger than 65 years who may be unemployed due to gout or co-morbidity related disabilities as well as those older than 65 years who continue to be employed. Another limitation is that subjects were asked to report only about activities lost due to flares, not to tophi, arthropathy, or other gout-related complications.
More work days were lost than social days or personal care days as shown in . This may be due to the more demanding nature of work, or to patients’ interpretation of the question about work fairly broadly (e.g., to include housework as well as how they define the totality of social events). The positive correlation of diary-reported activity loss with corresponding items on a well-established quality of life instrument (SF-36) supports the credibility of the diary reports.
The results are consistent with observed loss of productivity and activity in employed patients with rheumatoid arthritis (RA), another potentially debilitating chronic arthritic condition. A recent systematic review of several RA productivity studies found an average of 66% of individuals (range 36–84%) experiencing work loss due to their condition in the prior 12 months, for a median duration of 39 days (range 7–84 days)Citation17. Others have reported that patients with a variety of musculoskeletal diseases reduce their work hours, take breaks, or may even be forced to change jobs to deal with the pain and disability of their conditionsCitation12,Citation18–20.
The costs of productivity loss, as well as lost days of self-care and social activities, in patients with chronic gout refractory to conventional urate-lowering therapy are significant. Considering only costs of medical management of treatment-refractory chronic gout, and not addressing the indirect costs associated with this condition, will likely underestimate the total cost burden. In order to accurately assess the true personal and societal costs of chronic gout refractory to conventional therapy, lost productivity and lost capability for personal care and social participation must be considered.
Transparency
Declaration of funding
Financial support for this research was provided by Savient Pharmaceuticals, Inc., East Brunswick, NJ, USA
Declaration of financial/other relationships
S.B and F.P. served as consultants to Savient for this manuscript. N.L.E., J.S.S. and M.A.B. have received research support from Savient and are consultants to Savient Pharmaceuticals, Inc. N.L.E. and M.A.B. are also consultants for Takeda Pharmaceutical North America. A.F. is employed by Savient Pharmaceuticals, Inc.
Acknowledgements:
The authors would like to thank Dr F.D. Ottery, MD, PhD, of Savient Pharmaceuticals Inc., for assistance with the medical writing, fact checking and editing.
References
- Savient Pharmaceuticals Inc. KRYSTEXXA™ (pegloticase) for intravenous infusion BLA No. 125293. Silver Spring, MD: U.S. Food and Drug Administration, 2009 http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ArthritisDrugsAdvisoryCommittee/UCM165814.pdf.August 30, 2010
- Kramer HM, Curhan G. The association between gout and nephrolithiasis: the National Health and Nutrition Examination Survey III, 1988-1994. Am J Kidney Dis 2002;40:37-42
- Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 2008;58:26-35
- Adams PF, Hendershot GE, Marano MA. Current estimates from the National Health Interview Survey, 1996. Vital Health Stat 10 1999:1-203
- Arromdee E, Michet CJ, Crowson CS, et al. Epidemiology of gout: is the incidence rising? J Rheumatol 2002;29:2403-2406
- Edwards NL. Treatment-failure gout: a moving target. Arthritis Rheum 2008;58:2587-2590
- Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum 1998;41:778-799
- Roddy E, Zhang W, Doherty M. The changing epidemiology of gout. Nat Clin Pract Rheumatol 2007;3:443-449
- Wallace KL, Riedel AA, Joseph-Ridge N, et al. Increasing prevalence of gout and hyperuricemia over 10 years among older adults in a managed care population. J Rheumatol 2004;31:1582-1587
- Wu EQ, Patel PA, Yu AP, et al. Disease-related and all-cause health care costs of elderly patients with gout. J Manag Care Pharm 2008;14:164-175
- Roubenoff R. Gout and hyperuricemia. Rheum Dis Clin North Am 1990;16:539-550
- Kleinman NL, Brook RA, Patel PA, et al. The impact of gout on work absence and productivity. Value Health 2007;10:231-237
- Brook RA, Kleinman NL, Patel PA, et al. The economic burden of gout on an employed population. Curr Med Res Opin 2006;22:1381-1389
- Becker MA, Schumacher HR, Benjamin KL, et al. Quality of life and disability in patients with treatment-failure gout. J Rheumatol 2009;36:1041-1048
- Chohan S, Becker MA. Update on emerging urate-lowering therapies. Curr Opin Rheumatol 2009;21:143-149. Review. Erratum in: Curr Opin Rheumatol. 2010 Jan;2022(2011):2106
- Ware JE, Snow KK, Kosinski MK, et al. SF-36 Health Survey: Manual and Interpretation Guide. Boston: The Health Institute, New England Medical Center, 1993
- Burton W, Morrison A, Maclean R, et al. Systematic review of studies of productivity loss due to rheumatoid arthritis. Occup Med (Lond) 2006;56:18-27
- Chorus AM, Boonen A, Miedema HS, et al. Employment perspectives of patients with ankylosing spondylitis. Ann Rheum Dis 2002;61:693-699
- Chorus AM, Miedema HS, Wevers CW, et al. Work factors and behavioural coping in relation to withdrawal from the labour force in patients with rheumatoid arthritis. Ann Rheum Dis 2001;60:1025-1032
- Mancuso CA, Paget SA, Charlson ME. Adaptations made by rheumatoid arthritis patients to continue working: a pilot study of workplace challenges and successful adaptations. Arthritis Care Res 2000;13:89-99