Abstract
Objective:
Abdominal paracentesis is commonly performed for diagnostic, therapeutic, and palliative indications, but the use of ultrasound guidance for these procedures is relatively recent, variable, and not well documented. A retrospective database analysis of abdominal paracentesis procedures was performed to determine whether ultrasound guidance was associated with differences in adverse events (AEs) or hospital costs, compared to procedures without ultrasound guidance.
Methods:
The hospital database maintained by Premier was used to identify patients with abdominal paracentesis International Classification of Diseases – 9th Revision – Clinical Modification (ICD-9 code 54.9, Common Procedural Terminology CPT-4 codes 49080, 49081) in 2008. Use of ultrasound guidance was determined via patient billing data. The incidence of selected AEs and patients’ hospitalization costs were calculated for two groups: procedures with ultrasound guidance and those without. Univariate and multivariable analyses were performed to evaluate differences between groups.
Results:
This study identified 1297 abdominal paracentesis procedures, 723 (56%) with ultrasound and 574 (44%) without. The indications for paracentesis were similar between the two groups. The incidence of AEs was lower in ultrasound-guided procedures: all AEs (1.4% vs 4.7%, p = 0.01), post-paracentesis infection (0.41% vs 2.44%, p = 0.01), hematoma (0.0% vs 0.87%, p = 0.01), and seroma (0.14% vs 1.05%, p = 0.03). Analyses adjusted for patient and hospital covariates revealed significant reductions in AEs (OR = 0.349, 95% CI = 0.165, 0.739, p = 0.0059) and hospitalization costs ($8761 ± $5956 vs $9848 ± $6581, p < 0.001) for procedures with ultrasound guidance vs those without.
Limitations:
There are several limitations to using claims data for clinical analyses; causality cannot be determined, the possibility of miscoded or missing data, and the inability to control for elements not captured in claims data that may influence clinical outcomes.
Conclusions:
The use of ultrasound guidance in abdominal paracentesis procedures is associated with fewer AEs and lower hospitalization costs than procedures where ultrasound is not used.
Introduction
Abdominal paracentesis is a well-accepted and widely performed invasive procedure, with diagnostic, therapeutic, and palliative indicationsCitation1. It is performed in both inpatient and outpatient settings. The main hazards of this procedure derive from the inadvertent perforation or laceration of a blood vessel, organ, or other vital structureCitation2,Citation3.
Although such complications are rareCitation4, the use of ultrasound guidance to assist with patient selection and needle localization to further reduce these adverse outcomes seems logicalCitation5,Citation6. There are few studies to date, however, that have demonstrated an actual reduction in complicationsCitation7 or improved rates of successfully aspirated ascites with ultrasound guidance in abdominal paracentesisCitation8. Also, although the US Healthcare Cost and Utilization Project (HCUP) reports frequency and cost data for all abdominal paracentesesCitation9, the frequency of use of ultrasound guidance in abdominal paracentesis procedures is not well documented. Nor are there any published assessments of the economic impact of ultrasound guidance in abdominal paracentesis.
To help address these evidence gaps, a retrospective analysis of abdominal paracentesis procedures in a large database of US hospitals was performed to determine whether the application of ultrasound guidance was associated with differences in complications or hospital costs when compared to procedures without ultrasound guidance.
Patients and methods
Data source
The Premier hospital database was used, a large US hospital-based, service-level, all-payer, comparative database, containing information on ∼5.5 million annual hospital discharges (∼one-sixth of all hospitalizations in the US) from primarily non-profit, non-governmental, community and teaching hospitals, and health systemsCitation10. The Premier database includes hospitalizations from more than 600 hospitals for the period 2000 to the present. In addition to the service-level data recorded in most standard hospital discharge files, the Premier database provides a daily log of all billed items, including procedures, medications, laboratory tests, and diagnostic and therapeutic services, at the individual patient level. Derived in part from the Uniform Billing (UB)-92 and UB-04 discharge forms, the database also provides demographic characteristics, discharge diagnoses, and discharge status. Unlike datasets that draw directly from the UB-92 and UB-04 forms and thereby limit diagnosis and procedure codes to 10 and 6, respectively, the Premier data include all International Classification of Diseases – 9th Revision – Clinical Modification (ICD-9-CM) diagnosis and procedure codes recorded by the hospital, as well as a limited set of Common Procedural Terminology (CPT)-4 codes used primarily for outpatient visits and procedures.
A protocol describing the analysis objectives, criteria for patient selection, data elements of interest, and statistical methods was submitted to the New England Institutional Review Board (NEIRB) and exemption was obtained.
Eligible patients had a primary ICD-9 Procedure Code of 54.91 (paracentesis) and a CPT code of 49080 or 49081 during the year 2008. CPT code 49080 is used for percutaneous drainage of a fluid collection anywhere in the peritoneal space. CPT code 49081 describes peritoneocentesis, abdominal paracentesis, or peritoneal lavage (diagnostic or therapeutic); which indicates an additional paracentesis procedure performed separately on the same patient on the same date. Billing data were used for each patient visit id of interest to search for CPT codes (76930 or 76942) that indicated when ultrasound technology was utilized during the procedure.
For all eligible patients, data elements describing hospital cost, length of stay, and use of ultrasound (identified by billing codes) were obtained. The cost analysis (calculation) reflected the cost of the total hospital stay. The pre-operative Patient Refined Diagnosis Related Groups (APR-DRG) severity level is a derived score that has been validated by 3M and is provided with the Premier databaseCitation11 and used as an index of comorbidity. Socio-demographic characteristics and health insurance status of the patient were also included. Descriptors of the care setting were captured; namely census region, urban or rural setting, teaching hospital status and facility bed count. All procedures analyzed in the dataset were conducted in an inpatient setting.
Adverse events (identified by ICD9 codes—see Appendix) that occurred within the hospital stay of the procedure that could be associated with the primary procedure of interest were extracted. Of particular interest were post-operative pain, hemorrhage, hematoma, seroma, accidental puncture or laceration, infected post-operative seroma, other post-operative infection, post-operative fistula, other specified complication, pneumothorax, and hemothorax.
Statistical analyses
The main study objective was to compare complications and economic outcomes in patients undergoing abdominal paracentesis, with and without the use of ultrasound assistance, including adverse events, hospital costs, and length of stay. Costs were the actual costs incurred by the hospital for all treatments and services related to the entire hospital stay, including the paracentesis procedure. Bivariate and multivariable analyses were performed to examine the association between ultrasound-assisted paracentesis and adverse events, hospital costs, and length of stay. The multivariable analysis controlled for patient severity, patient socio-demographics, and hospital characteristics. This controlled for confounding effects that might otherwise bias the relationship between ultrasound-assisted paracentesis and the outcomes of interest. Each of the variables used in these multivariable models are described in .
Table 1. Patient characteristics of paracentesis procedures with ultrasound and without.
Multivariable models for hospital costs and length of stay were estimated. Using standard practice, hospital costs and length of stay were transformed to natural logarithms in order to normalize their distributions. Smearing estimates were then calculated to allow for comparisons, after modeling, using the original scale of the data. This method is commonly used when predictions and forecasts are required from models that use log-transformed dataCitation12. All analyses were performed using SAS (Cary, NC) Version 9.1.
Results
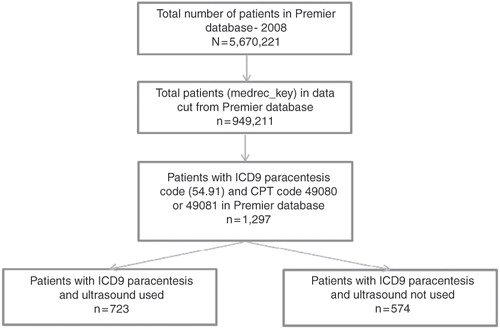
A total of 1297 inpatient records from 89 hospitals were analyzed. A patient attrition diagram is shown in .
Fifty-six per cent of all inpatient paracentesis procedures were performed with the use of ultrasound assistance (n = 723). There were no differences in the age or gender distributions of patients undergoing ultrasound-assisted paracentesis compared to those undergoing paracentesis without ultrasound assistance. A slightly higher illness severity index was noted for the ultrasound group (78.56% vs 72.30%). There were also slight differences in types of primary insurance, with more managed care patients having the procedure without the use of ultrasound (see ).
Characteristics of the 89 hospitals with paracentesis procedures in the database are summarized in . Of these, the majority (n = 60, or 67%) had ultrasound capabilities that were used in paracentesis procedures in 2008. Teaching vs non-teaching, urban vs rural, and hospital size did not differ substantially between ultrasound and non-ultrasound hospital groups. However, there were slight differences in region, with Midwest hospitals less likely to have ultrasound capabilities.
Table 2. Characteristics of hospitals with paracentesis procedures.
Regarding complications, in most cases, ultrasound procedures were associated with a slightly lower incidence of adverse events relative to ultrasound procedures (). Of significance were the overall rate of adverse events (1.4% vs 4.7%, p = 0.0004), post-paracentesis infection (0.41% vs 2.44%, p = 0.001), hematoma (0.0% vs 0.87%, p = 0.01), and seroma (0.14% vs 1.05%, p = 0.03).
Table 3. Complications occurring during the hospital stay in patients.
The use of ultrasound assistance was consistently associated with lower per-patient average total stay hospital costs of $8761 (with ultrasound) vs $9848 (without). The unadjusted results in Tables and suggest that average length of stay was slightly shorter overall, 5.6 vs 5.7 days, for ultrasound-assisted paracentesis.
Table 4. Unadjusted and adjusted results for cost and length of stay.
Table 5. Adverse event—logistic regression.
Given the possibility of confounders in our hospital cost and utilization comparisons, multivariate regression analyses were performed. The model was adjusted for patient demographics, severity, and hospital characteristics. Even after adjusting for these variables, inpatient total stay hospital costs remained lower for ultrasound-assisted paracentesis than for procedures without ultrasound assistance: $8733 (CI $8595, $8,871) vs $9994 (CI $9836, $10,152), respectively. This difference was statistically significant. The difference in adjusted average length of stay was slightly shorter, but perhaps not clinically relevant at 5.6 days for ultrasound procedures vs 5.8 for non-ultrasound. This difference did reach statistical significance.
In an effort to investigate the overall rate of adverse events further, a logistic regression was run controlling for patient and hospital demographics, and patient severity and mortality. Results reveal that, after adjusting for various covariates, ultrasound was still associated with a 65% reduction in adverse events (OR = 0.349, p = 0.0059) (see Tables and ).
shows a comparison of the other top primary diagnoses for patients undergoing paracentesis both with and without ultrasound assistance, indicating no significant differences between the most frequently occurring diagnosis codes between the two groups. The indications for paracentesis were similar between patients between the two groups, including cirrhosis, and other causes of ascites, most of which were liver-related. Thus, no difference in the use of ultrasound appears to be due to other primary diagnoses.
Table 6. Primary diagnoses for patients undergoing paracentesis both with and without ultrasound assistance.
Discussion
In summary, this study showed that more paracentesis procedures were performed with ultrasound guidance (n = 723, 56%) than without ultrasound (n = 574, 44%). The indications for paracentesis, based on ICD-9 diagnosis coding, were similar between patients between the two groups and the incidence of serious complications was low. Notably, ultrasound-guided paracentesis was associated with significantly lower overall rates of adverse events, post-paracentesis infections, hematomas, and seromas. Multivariable regression analysis of adverse events from ultrasound guided paracentesis, controlling for important patient and hospital characteristics, found 65% lower likelihood of complications through the use of ultrasound. Patients who underwent paracentesis with ultrasound guidance were also found to have lower average total hospitalization costs. This finding remained consistent, even after adjusting for patient and hospital demographics.
The limitations of this study include those often associated with administrative databases and the use of claims data in particular. A limitation of administrative databases is the potential over- or under-coding of ICD-9 diagnoses and procedures as well as adverse events. However, there is little reason to suspect that there would be systematic differences in the coding of cases of ultrasound guided paracentesis vs those without ultrasound guidance. As with all analysis of claims data the possibility of miscoded or missing data, and the inability to control for elements not captured in claims data may influence clinical outcomes. The Premier database does not capture data from physician office visits, thus this potential source of adverse event information is not included in this analysis; it is unlikely that this would change the direction of the outcome of this analysis. This analysis found lower average total hospitalization costs associated with the use of ultrasound guidance of abdominal paracentesis. Total hospitalization costs do not include costs to the patient or to society such as lost work time. The incorporation of these additional costs would strengthen the case for the use of ultrasound guidance as this analysis showed significant reductions in adverse events. Observational studies, including the analyses presented here, have the notable limitation of the inability to draw conclusions regarding causality.
These findings agree with an expanding body of observational research using differing data sources and healthcare settings where ultrasound guidance has been shown to improve outcomesCitation13–15. A review of intravascular ultrasound recognized the importance of ultrasound guidance in the evolution and future of interventional cardiologyCitation13. Specifically, the use of intravascular ultrasound has increased the knowledge of stent thrombosis, vessel injury, as well as healing, and recognized a role for ultrasound guidance in drug-eluting stents more so than in routine coronary stent implantation. Kapral et al.Citation14 described the use of ultrasound guidance in regional anesthetic blocks, in 160 patients randomized to ultrasound guidance for interscalene brachial plexus block or to nerve stimulation group. The study found that a block was achieved in significantly more of the ultrasound group (p < 0.01, 99% to 91%) in comparison to the nerve stimulation group. Lin et al.Citation15 described the use of ultrasound guided aspiration and lavage of calcific tendinosis of the shoulder in a retrospective chart review. The study suggested that ultrasound guided aspiration was an effective treatment of calcific tendinosis as pre- and post-treatment questionnaire data showed an improvement in shoulder ratings and a successful outcome in 27 of 36 patients. Despite the fact that it requires training on the part of the user and has somewhat of a learning curve to achieve proficiency, implementation of ultrasound guidance in the clinical setting has the ability to significantly improve clinical outcomes and reduce overall costs. Implementation of ultrasound-guidance across physician specialties involved with the performance of paracentesis procedures within a single hospital system or healthcare plan can result in significantly improved clinical outcomes and reduced costs while improving patient health.
Conclusion
The use of ultrasound guidance to guide needle insertion for percutaneous entry for abdominal paracentesis procedures is associated with a lower rate of complications and lower cost of hospitalization than procedures where ultrasound is not used. These findings suggest that using ultrasound guidance during abdominal paracentesis procedures is beneficial from an outcomes and cost perspective.
Transparency
Declaration of funding
Funding for the study was provided by GE Healthcare. Pankaj A. Patel participated in the planning and conducting of the study, interpreting data, and drafting the manuscript. Frank R. Ernst participated in the planning and conducting of the study, collecting and interpreting data, and drafting the manuscript. Candace L. Gunnarsson participated in the planning and conducting of the study, interpreting data, and drafting the manuscript. All authors have approved the final draft submitted.
Declaration of financial/other relationships
Pankaj A. Patel is an employee of GE Healthcare, which sponsored the study. Frank R. Ernst is employed by Premier healthcare alliance, which contracted with GE healthcare to conduct the study. Candace L. Gunnarsson is a paid consultant to GE Healthcare, through S2 Statistical Solutions, Inc.
Acknowledgments
No assistance in the preparation of this article is to be declared.
References
- Lee SY, Pormento JG, Koong HN. Abdominal paracentesis and thoracocentesis. Surg Laparosc Endosc Precutan Tech 2009;19: e32-5
- Mallory A, Schaefer JW. Complications of diagnositic paracentesis in patients with liver disease. JAMA 1978;239:6289-30
- Webster ST, Brown KL, Lucey MR, et al. Hemorrhagic complications of large volume abdominal paracentesis. Am J Gastroenterol 1996;91:366-8
- Runyon BA. AASLD Practice Guidelines Committee. Management of adult patients with ascites due to cirrhosis: an update. Hepatology 2009;49:2087-107
- Wiese SS, Mortensen C, Bendtsen F. Few complications after paracentesis in patients with cirrhosis and refractory ascites. Dan Med Bul 2011;58:A421
- Moore CL, Cope JA. Point-of-care ultrasonography. N Engl J Med 2011;364:749-57
- Gottardi A, Thevenot T, Spahr L, et al. Risk of complications after abdominal paracentesis in cirrhotic patients: a prospective study. Clin Gastroenterol Hepatol 2009;7:906-9
- Nazeer SR, Dewbre H, Miller AH. Ultrasound-assisted paracentesis performed by emergency physicians vs the traditional technique: a prospective, randomized study. Am J Emerg Med 2005;23:363-7
- U.S. Department of Health & Human Services Agency for Healthcare Research and Quality. Appendix: 2003 Statistics on all-listed procedures in U.S. Hospitals. U.S. Department of Health & Human Services. Available at: http://www.ahrq.gov/data/hcup/factbk7/factbk7d.htm. Accessed December 1, 2010
- Premier Research Services – Premier Inc. Available at: http://www.premierinc.com/prs. Accessed December 1, 2010
- Averill R, Goldfield N, Hughes J, et al. What are APR-DRGs? An introduction to severity of illness and risk of mortality adjustment methodology [White Paper]. Saltlake City, UT: 3M™Health Information Systems, 2003. Available at: http://solutions.3m.com/3MContentRetrievalAPI/BlobServlet?locale=it_IT&lmd=1218718280000&assetId=1180603360910&assetType=MMM_Image&blobAttribute=ImageFile. Accessed September 13, 2011
- Duan N. Smearing estimate: a nonparametric retransformation method. J Am Stat Assoc 1983;78:605-10
- Orford JL, Lerman A, Holmes DR. Routine intravascular ultrasound guidance of percutaneous coronary intervention: a critical reappraisal. J Am Coll Cardiol 2004;43:1335-42
- Kapral S, Greher M, Huber G, et al. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med 2008;33:253-8
- Lin JT, Adler RS, Bracilovic A, et al. Clinical outcomes of ultrasound-guided aspiration and lavage in calcific tendinosis of the shoulder. HSS J 2007;3:99-105