Abstract
Objective:
Congenital hemophilia patients with inhibitors are at greater risk for developing arthropathy and orthopedic complications compared to those without inhibitors. Elective orthopedic surgeries (EOS) may be an option for these patients and may provide long-term cost savings due to reduced bleed frequency. However, patient motivations and goals for undergoing or delaying such surgeries are not well understood. A US-based patient/caregiver survey was designed to describe inhibitor patient experiences and outcomes following EOS and to develop a comprehensive understanding of patient preferences for EOS, which are lacking in the literature.
Methods:
The paper–pencil questionnaire was mailed to 261 US inhibitor patients/caregivers and included history and timing of EOS, quality-of-life (QoL) and potential benefits of and barriers to receiving EOS. Univariate/bivariate descriptive analyses were performed to characterize those with/without a history of EOS.
Results:
For 103 subjects who responded, the mean age was 20.9 years. Approximately 25% (n = 26) of respondents underwent EOS, most commonly on the knee (21, 81%); 73.1% of surgery recipients reported the surgery improved or greatly improved their QoL based on single-item response. The highest ranked perceived benefits were less pain, fewer bleeds, and improved mobility. However, the leading concerns reported were lack of improved mobility (62.2%), fear of uncontrolled bleeding (61.3%), and surgical complications, such as blood clot (60.0%).
Limitations:
The study consisted of a small sample size, primarily due to the difficulty in trying to reach inhibitor patients or their caregivers, thereby restricting inferential and stratification analysis.
Conclusions:
QoL improved for most inhibitor patients who reported having EOS. For those considering surgery, there is optimism about the potential benefits, but realistic concerns associated with bleed control and post-op complications.
Introduction
Congenital hemophilia is an X-linked recessive blood disorder affecting clotting factors VIII or IX. The disorder is rare, affecting between ∼1 in 5,000–10,000 males born in the USCitation1. There are two categories of congenital hemophilia: hemophilia A, which represents nearly 85% of cases, and hemophilia BCitation2. Patients with hemophilia A are deficient of clotting factor VIII, while those with hemophilia B are deficient of factor IXCitation3. Patients with hemophilia suffer from a life-long impairment in their blood clotting, which can lead to excessive internal and external bleedingCitation4. Bleeding most typically occurs in joints and can eventually result in joint degradation, severe pain, and arthropathyCitation5. Treatment for acute bleeds includes replacement of the missing clotting factor when a bleed occurs, or more commonly routine replacement for those with a severe deficiency. As these patients may not have circulating FVIII or FIX, some individuals develop alloantibodies (‘inhibitors’) in response to the ‘foreign’ factor being administered. The blocking ability of the antibody response is reflected by an inhibitor titer and classified typically as high or low. Up to one third of hemophilia A patients develop factor VIII inhibitors, requiring a switch from factor replacement to bypassing agents (such as FEIBA (factor VIII inhibitor-bypassing activity), activated prothrombin complex concentrate (aPCC), and NovoSeven® (recombinant factor VIIa, rFVIIa)) in order to stop bleedingCitation6.
Treatment of patients with hemophilia and inhibitors is challenging, complex, and costly as they demonstrate greater likelihood of orthopedic complications due to more difficult to treat bleedsCitation7. Bleeding with joints leads to an acute inflammatory process (synovitis), which over time results in overgrowth of the synovial lining of the joint, increased susceptibility to further bleeding, and ultimately damage to cartilage and bone. While less invasive procedures like synovectomies are commonly performed on hemophilia patients with inhibitors to reduce bleed frequency, joint replacement surgery may eventually be necessary as joint damage progresses.
As replacement of the missing coagulation factors that can be monitored with lab tests is ineffective, this presents a therapeutic challenge in elective or emergency surgeryCitation8. Recent advances in treatments with bypassing agents, particularly influenced by two randomized clinical trials with recombinant activated factor VII (rFVIIa, NovoSeven®RT, Novo Nordisk, Bagsvaerd, DK), have made minor and major surgeries possible for hemophilia patients with inhibitors and led to development of treatment protocols in most hemophilia treatment centersCitation9–11. Recombinant factor VIIa is approved for prevention of bleeding during surgery by intermittent bolus injections, although trials have investigated an alternate approach using continuous infusionCitation10,Citation12,Citation13.
Despite these advances, major elective orthopedic surgeries (EOS) are costly and continue to be perceived as high risk for hemophilia patients with inhibitors, which may prevent them from being considered or recommended as a treatment optionCitation14,Citation15. As a result, hemophilia patients with inhibitors may suffer from increased morbidities compared with hemophilia patients without inhibitors. Further joint degeneration across multiple joints increases the likelihood that more extensive surgical procedures will be neededCitation15. Recent economic modeling from a healthcare payer perspective suggests that EOS can provide cost savings in the medium- to long-term as compared to not having had surgery due to a decrease in the number of bleeding episodes requiring treatment in patients who underwent surgeryCitation16.
Certainly there is no single therapeutic modality for dealing with the various challenges posed by hemophilia patients with inhibitors. Overall goals to any such treatment should be to preserve or improve mobility, functional capabilities, and quality-of-life, with the provision of cost-effective care that aims to maintain physical functionCitation17. An understanding of patient and caregivers’ subjective outcomes following EOS, as well as their motivations and perceived barriers to considering EOS, may help payers better understand their members needs and the therapeutic landscape and its possibilities. Both of these issues have not been described in the literature.
The objective of this US-based patient/caregiver survey was to describe patient experiences and outcomes associated with EOS in hemophilia patients with inhibitors to develop a comprehensive understanding of patient preferences for EOS.
Patients and methods
Questionnaire development
The survey tool was a 20-page single-assessment, cross-sectional survey self-administered via paper–pencil. A systematic literature review was conducted to inform content development of the questionnaire and identify data gaps in the literature. The search was conducted in PubMed and applied established limits, including: studies published in the past 10 years, human study, English language. Key areas for this literature review included treatment guidelines and outcomes for congenital hemophilia inhibitor patients, joint repair/replacement surgery, patient/caregiver perspectives on treatment options, and QoL in the inhibitor population. The questionnaire was validated by two, independent benign hematologists specializing in treatment of hemophilia patients and particularly around surgical procedures.
Four different versions of the survey tool were used in order to accommodate different age groups: (1) adult patient; (2) caregiver of child aged 4–7 years; (3) caregiver of child aged 8–12 years; (4) caregiver of child aged 13–16 years. For all versions, questions were organized into the following sections: Demographic characteristics, hemophilia profile (including titer level and current treatment regimen), preventive care and surgical treatment. This paper centers around the questions related to surgical treatment (‘Would you be interested in joint surgery as a treatment option if it had the potential to improve mobility/improve independence/reduce pain/reduce the number of bleeds experienced on a monthly basis/improve joint health?’). Individual questions in the surgical section included history and timing of EOS. For subjects with a history of EOS, timing and joint location (knee, ankle, shoulder, elbow, hip) of surgery, along with the impact of surgery on QoL via a single item question (‘How has the surgery impacted your quality of life?’; responses included a Likert scale of greatly improved/improved/neither improved nor worse/worse/much worse), were assessed. For subjects without a history of EOS, potential benefits of and barriers to receiving EOS were assessed.
Study cohort
The target sample was hemophilia patients with inhibitors (or the caregivers/parents of patients less than 18 years old) and was identified through their attendance at recent educational summits. The paper–pencil questionnaire was mailed to 261 hemophilia patients with inhibitors and caregivers during July 2010, for immediate return. Households that did not respond to the initial mailing within 3 weeks received a duplicate packet. Households that returned a completed survey and informed consent document were paid $100 USD.
All respondents had to satisfy certain inclusion criteria to be considered in the study data set. Patients (or caregivers/parents of minors) had to: (1) provide evidence of a personally signed and dated informed consent form indicating that the subject has been informed of all pertinent aspects of the study; (2) be identified as a patient or caregiver/parent of a minor patient with hemophilia and inhibitors; and (3) be able to speak, write, and understand both verbal and written English. Patients were excluded from the study if they had non-eligible diagnoses (i.e., were not hemophilia patients with inhibitors). Ethics approval for the study was granted by the Western Institutional Review Board.
Statistical analysis
For categorical measures, the distribution of subjects across the categories of each characteristic was described using cross-tabulation analysis. For continuous measures, descriptive statistics included the mean, median, standard deviation and ranges, collectively providing an interpretation of the distributional characteristics of the data.
Since one of the main objectives of the survey was to characterize demographically and clinically sub-populations both with and without a history of EOS, bivariate (comparative) analysis was used to identify such relationships (based upon the Chi Square test or Fisher’s Exact test if cell value <5; Wilcoxon rank sum on the median). Bivariate analysis was limited to subjects ages 15 and greater (n = 57) based on clinical judgment that this is the age when joint degradation begins to manifest. It was therefore considered most meaningful to compare patients who had prior joint surgery with those who were at risk for it. Statistical significance was set at p < 0.05 where sample size permitted.
All analyses were performed using SAS version 9.1 software (SAS, Cary, NC).
Results
Response rate
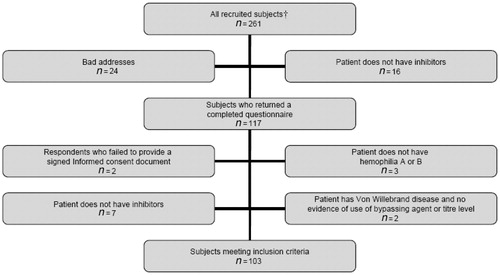
Of the total 261 recruited subjects, 117 (44.8% response rate) patients returned a completed questionnaire, 24 (9.2%) patients were not reached due to bad addresses and 16 (6.1%) patients did not have hemophilia with inhibitors. Of the 117 patients, 14 were excluded for the following reasons: informed consent document (two failed to provide a signed document); no hemophilia A or B (three); no inhibitors (determined upon review of the survey in hand) (seven); or disease characteristics (two had Von Willebrand’s disease and no evidence of use of bypassing agent or high titer level). The remaining 103 subjects (63 of which were caregiver respondents) met the study inclusion criteria as shown in .
Patient characteristics
Among the respondents, the age range of referenced patients was 1–67 years (mean = 20.7, median = 15, SD = 17.4), with the greatest number of patients in the 4–7 years age group (25.2%) (other age group stratifications were: 1–3 years (3.9%); 8–12 years (12.6%); 13–16 years (12.6%); 17–24 years (14.6%); 25–44 years (19.4%); 45–64 years (8.7%); and 65+years (2.9%)). More than half of the subjects were unemployed, with 41.1% of those unemployed due to the hemophilia or its complications. Sixty-six percent of the respondents reported their household income was less than $100,000 per year, while the majority of respondents had health insurance either through an employer or school (47.6%) or Medicaid (43.7%).
The majority of respondents (93.2%) were treated primarily at home, and most patients had high titer inhibitors requiring bypassing agents (69.9%). An on-demand treatment method was utilized by 42.7% of the respondents, while the same number reported that they took treatments regularly to prevent bleeding. Bleeds required a trip to the emergency room for only 29.1% of respondents, while 39 respondents reported a mean (SD) of 2.99 (3.19) bleeds per month in the 3 months prior to survey administration. describes both the patient demographic and clinical characteristics.
Table 1. Patient demographic and clinical characteristics at enrollment.
Patient history of joint surgery
The majority of survey respondents reported that they have not had surgery to repair hemophilia-related damage in any of their joints (n = 77). For those that had surgery (n = 26), the majority underwent surgery in the past 5 years. Most of the surgeries took place after the development and diagnosis of inhibitors and were performed on a single joint, with the knee (n = 15) being the most common. Six respondents had surgery on more than one joint, with knee and ankle the most frequently mentioned combination. In total, 21 patients (81%) reported surgery that included the knee joint.
The potential correlation between elective orthopedic surgery and an improvement in patient’s quality-of-life was examined at a descriptive level. The majority of surgery recipients felt that the surgery met their expectations (n = 15, 57.7%) and either ‘improved’ (n = 10, 38.5%) or ‘greatly improved’ (n = 9, 34.6%) their QoL based on the single item assessment. One caregiver felt that the surgery left the patient with a ‘much worse’ quality-of-life vs their quality-of-life prior to the surgery.
Bivariate analysis between respondents that did and did not have a history of joint surgery highlighted potential correlation amongst these respondent sub-groups. In this sub-group, Hemophilia B (p = 0.0060), a history of immune tolerance therapy (ITI) (p = 0.0169), not receiving only recombinant Factor VIII (p = 0.0187), and currently receiving preventive care (p = 0.0333) were all significant variables associated with having a history of joint surgery. depicts the variables that exhibited a trend (p < 0.05) in bivariate analyses.
Table 2. Patient characteristics by history of joint surgery (patients aged 15 and greater).
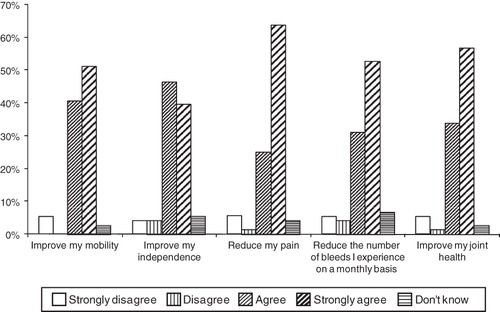
Interest in and potential benefits of surgical treatment
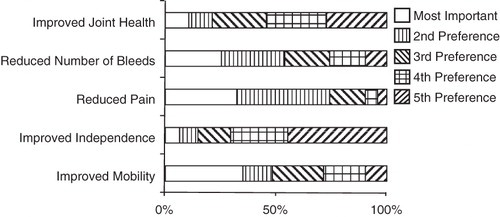
Within the sub-group of patients with no history of joint surgery (n = 77), there is interest in elective orthopedic surgery as a potential treatment option. Respondents would be interested in joint surgery as a treatment option if it had the potential to ‘reduce my pain’ (n = 46, 63.9%), ‘improve my joint health’ (n = 42, 56.8%) or ‘reduce the number of bleeds I experience on a monthly basis’ (n = 39, 52.7%), as respondents ‘strongly agree’ with these sentiments. displays the other attributes of joint surgery that have the potential to interest respondents with no history of joint surgery. When asked to rank order the potential benefits of joint surgery, 35.1% of the respondents indicated that ‘improved mobility’ was the most important potential benefit. ‘Reduced pain’ was the second most important potential benefit of joint surgery, mentioned by 41.9% of respondents. displays all of the potential benefits of joint surgery, in the order of respondent preference (all ages). A stratification analysis showed that the potential benefits of joint surgery are consistent, regardless of the age of the patient.
Concerns related to joint surgery
The concerns respondents expressed related to joint surgery may be identified by examining the frequency of responses that ‘agree’ and ‘strongly agree’ with specific concerns. The fear that surgery would not result in any better mobility than before was the leading concern (62.2%), followed by the fear of uncontrolled bleeding during the surgery (61.3%). There were differences in the concerns related to joint surgery between children (<18 years of age) and adult patients (≥18 years of age). Fear of post-operative pain was a concern of the majority of patients ≥18 years of age (82.9%) as compared to only 24.0% of the younger patient population. Similarly, worry about missing work/school was a concern of 73.8% of the older patients but not as much for the younger patients (50.0%). The remaining leading concerns, for all ages, are listed in .
Table 3. Concerns related to joint surgery (respondents with no history of joint surgery; all ages).
Discussion
Our survey shows that among those patients who have had EOS surgery, it met their expectations and may have improved their quality-of-life. Approximately 25% of the patients underwent EOS, with the knee (n = 15) being the most common joint, and most procedures occurring in the past 5 years. While the majority of survey respondents (92%) are interested in EOS due to its potential to ‘improve my mobility’, they did express their perceived concerns that EOS might not result in any better mobility than before (62.2%). The fear of uncontrolled bleeding during the surgery was similarly rated as a concern by the survey respondents (61.3%).
EOS appears to have become a more viable treatment option for hemophilia patients with inhibitors over the course of the last decade. This is potentially due to new agents having been shown to be effective prophylaxis during elective surgeryCitation10,Citation11 as well as physicians becoming more comfortable in the procedures themselvesCitation9, leading to a greater expectation of success and an improved quality-of-lifeCitation18,Citation19. In a retrospective hospital attendance study conducted for the period 1988–1997 for individuals who were aged 18 years or over (n = 246), there were 50 orthopedic operations (defined as joint replacements, arthrodeses, synovectomies, O’Donoghue’s procedures, ulnar nerve decompressions, excision of radial heads and other miscellaneous orthopaedic procedures) conducted during that time period (0.203 surgeries per patient),Citation20 as compared to 26 orthopedic operations for our survey population of 103 individuals over a 5-year time period (0.25 surgeries per patient). Perhaps slowly, elective orthopedic surgery is a treatment option that more hemophilia patients with inhibitors are beginning to consider more strongly as a viable treatment option.
Our survey sample (among respondents with no prior history of surgery) highlighted improvement in mobility and reduction in pain as two leading perceived benefits of elective orthopedic surgery. Other research have highlighted similar, and additional, benefits of such surgery, such as decreased bleed frequency into a new joint, less time spent in hospital, reduction in pain, increased mobility and improved well-being and functionCitation9,Citation21. From the payer perspective, proper use and management of EOS can have the potential to improve patients’ quality-of-life, with the added benefit of a reduction in downstream medical and pharmaceutical costs due to fewer bleeds.
Despite the perceived benefits of EOS, according to both our survey sample as well as the peer-reviewed literature, there remain some fears and concerns to the procedures. Survey respondents indicated concerns related to uncontrolled bleeding during the surgery as well as the belief that they won’t have any better mobility than before the surgery. While respondents did not think that their physician would prefer to not perform the surgery, there is evidence that physicians remain skeptical about the potential complications of elective orthopedic surgery on hemophilia patients with inhibitorsCitation15. However, with strong motivation and a multidisciplinary team approach, outcomes are generally goodCitation8–11,Citation22,Citation23. Further research on the identification of appropriate patient segments and the timing of such surgery may allay some of this skepticism.
Surveys that include patients and caregivers certainly have limitations and the potential for inconsistencies. When compared to the benefits of EOS cited in prior studies and research, there was some inconsistency in the benefits of surgery mentioned by our survey sample. This underscores the potential need for an education program to further highlight EOS as an option for inhibitor patients along with its risks and benefits. Another inconsistency in the results can be seen in the fact that less than half of the survey respondents reported that they are not worried about their out-of-pocket costs related to joint surgery. In contrast, other survey results indicate that respondents are experiencing a financial burden due to the disease (although not statistically significant). The additional collection of real world data would help to alleviate some of these discrepancies, as well as to further understand how to educate stakeholders regarding the actual benefits and risks associated with surgery.
Study limitations
Although this study provides valuable insight into the perceived benefits and barriers to EOS by hemophilia patients with inhibitors, there are some limitations that warrant mention. Based on extrapolation from data collected by the Centers for Disease Control and PreventionCitation24, it is estimated that there are ∼1200 hemophilia patients with inhibitors in the US, ∼700 of which receive some type of treatment for hemophilia. The study consisted of a small sample size, primarily due to the difficulty in trying to reach hemophilia patients with inhibitors or their caregivers, thereby restricting inferential and stratification analysis. While our response rate was good (compared to other paper–pencil surveys administered via the mail), the small sample does lend itself to potential response bias. All patients/caregivers contacted participated in educational summits, which in and of itself suggests they may be more educated or engaged in their disease management. Furthermore, those that did respond may reflect patients who have already undergone EOS or have more interest in considering it compared with the non-responders. So while this sample may not be large enough to warrant statistical inference, any study capturing an estimated 9% of the eligible population is likely representative of the patient group.
Our analysis combined both high and low titer patients into one group, due to small sample sizes, so there are no results around the potential differences due to this patient characteristic. In addition, our survey did not focus on patient preferences in the area of EOS, so there is limited data in this aspect of the patients’ experience, one that might require additional research. Additional research may be justified in the area of quality-of-life, as our survey design did not allow for a pre- or post-surgical view on more specific patient quality-of-life and outcomes than general improvement in quality-of-life.
Conclusions
Survey respondents are interested in EOS due to its potential to improve mobility and reduce pain. However, fears around uncontrolled bleeding and lack of improvement following the surgery are barriers that need to be addressed and overcome, particularly given that data is available to support positive outcomes and safety of EOS in inhibitor patients. Insurance coverage and associated lifetime caps are other issues that need to be further explored to allow appropriate patients to seek this treatment option.
Transparency
Declaration of funding
This study was funded by Novo Nordisk, Princeton, NJ, USA.
Declaration of financial/other interest
MD, AP, and WCL have disclosed that they are employees of IMS Consulting Group, a company which received funding from Novo Nordisk to conduct this research. TW, NH, and DC have disclosed that they are employees of Novo Nordisk.
Acknowledgments
The authors acknowledge the assistance of Steven Pipe, MD (University of Michigan, Associate Professor, Department of Pediatrics and Communicable Diseases) and Christopher Walsh, MD, PhD (Mt. Sinai School of Medicine, Associate Professor of Medicine, Hematology and Medical Oncology) for review of the questionnaires.
References
- Soucie JM, Evatt, B, Jackson D. Occurrence of hemophilia in the United States. The Hemophilia Surveillance System Project Investigators. Am J Hematol 1998;59:288-94
- World Federation of Hemophilia. Guidelines for the management of hemophilia. World Federation of Hemophilia; 2005
- Bolton-Maggs PH, Pasi KJ. Haemophilias A and B. Lancet 2003;361:1801-9
- Knight C. Health economics of treating haemophilia A with inhibitors. Haemophilia 2005;11(1 Suppl):11-17
- Valentino LA. Blood-induced joint disease: the pathophysiology of hemophilia arthropathy. J Thomb Haemost 2010;8:1895-902
- Zakarija A, Harris S, Rademaker AW, et al. Alloantibodies to factor VIII in haemophilia. Haemophilia 2011; doi: 10.1111/j.1365-2516.2010.02468.x. [Epub ahead of print]
- Boadas A, Fernandez-Palazzi F, DE Bosch NB, et al. Elective surgery in patients with congenital coagulopathies and inhibitors: experience of the National Haemophilia Centre of Venezuela. Haemophilia 2010; doi 10.1111/j.1365-2516.2010.02427.x. [Epub ahead of print]
- Valentino LA, Cooper DL, Goldstein B. Surgical experience with rFVIIa (NovoSeven) in congenital haemophilia A and B patients with inhibitors to factors VIII or IX. Haemophilia 2011; doi: 10.1111/j.1365-2516.2010.02460.x. [Epub ahead of print]
- Giangrande PLF, Wilde JT, Madan B, et al. Consensus protocol for the use of recombinant activated factor VII [Eptacog alfa (activated); NovoSeven] in elective orthopaedic surgery in haemophilic patients with inhibitors. Haemophilia 2009;15:501-8
- Pruthi RK, Mathew P, Valentino LA, et al. Haemostatic efficacy and safety of bolus and continuous infusion of recombinant factor VIIa are comparable in haemophilia patients with inhibitors undergoing major surgery. Thromb Haemost 2007;98:726-32
- Shapiro AD, Gilchrist GS, Hoots WK, et al. Prospective, randomised trial of two doses of rFVIIa (NovoSeven) in haemophilia patients with inhibitors undergoing surgery. Thromb Haemost 1998;80:773-8
- NovoSeven® RT [Package insert]. Princeton, NJ: Novo Nordisk Inc, 2010
- Bysted BV, Scharling B, Moller T, et al. A randomized, double-blind trial demonstrating bioequivalence of the current recombinant activated factor VII formulation and a new robust 25°C stable formulation. Haemophilia 2007:13:527-32
- Ludlam C. Identifying and managing inhibitor patients requiring orthopaedic surgery – the multidisciplinary team approach. Haemophilia 2005;11(1 Suppl):7-10
- Teitel JM, Carcao M, Lillicrap D, et al. Orthopaedic surgery in haemophilia patients with inhibitors: a practical guide to haemostatic, surgical and rehabilitative care. Haemophilia 2009;15:227-39
- Lyseng-Williamson KA, Plosker GL. Recombinant factor VIIa (eptacog alfa): a pharmacoeconomic review of its use in haemophilia in patients with inhibitors to clotting factors VIII or IX. Pharmacoeconomics 2007;25:1007-29
- Blanchette VS, Manco-Johnson MJ. Meeting unmet needs in inhibitor patients. Haemophilia 2010;1(3 Suppl):46-51
- Rodriguez-Merchan EC, Wiedel JD, Wallny T, et al. Elective orthopedic surgery for hemophilia patients with inhibitors: new opportunities. Semin Hematol 2004;41(1 Suppl):109-16
- Hvid I, Rodriguez-Merchan EC. Orthopedic surgery in hemophilia patients with inhibitors: an overview. Haemophilia 2002;8:288-91
- Miners AH, Sabin CA, Tolley KH, et al. Primary prophylaxis for individuals with severe haemophilia: how many hospital visits could treatment prevent? J Intern Med. 2000;247:493-499.
- Ballal RD, Botteman MF, Stephens JM, et al. Economic evaluation of major knee surgery with recombinant activated factor VII in hemophilia patients with high titer inhibitors and advanced knee arthropathy: exploratory results via literature-based modeling. Curr Med Res Opin. 2008 Mar;24(3):753-68.
- Jimenez-Yuste V, Rodriguez-Merchan EC, Alvarez MT, et al. Controversies and challenges in elective orthopedic surgery in patients with hemophilia with inhibitors. Semin Hematol. 2008 Apr;45(2 Suppl 1):S64-7.
- Caviglia H, Candela M, Galatro G, et al. Elective orthopaedic surgery for haemophilia patients with inhibitors: single centre experience of 40 procedures and review of the literature. Haemophilia. 2011 Feb 22. doi: 10.1111/j.1365-2516.2011.02504.x. [Epub ahead of print]
- Centers for Disease Control and Prevention – Universal Data Collection (UDC) System, Available at http://www.cdc.gov/ncbddd/blooddisorders/udc [Last accessed 19 August 2011]