Abstract
Objective:
The cost-effectiveness of renal replacement therapy (RRT) is affected by the composition of treatment. This study aimed to estimate the costs and outcomes associated with changing the composition of RRT modality over time.
Methods:
By using clinical and cost data from a systematic review, a Markov model was developed to assess the costs and benefits of the four main treatments available for RRT in Japan. The model included direct health service costs and quality-adjusted life years (QALY). Sensitivity analyses were performed to assess the robustness of the results.
Results:
Over the 15-year period of the model, the current composition of RRT (i.e., the base composition of RRT) was $84,008/QALY. The most cost-effective treatment was when the likelihood of a living donor transplant was increased by 2.4-times ($70,581/QALY). Compared with the base composition of RRT, dominant treatments with respect to cost-effectiveness were when the likelihood of a deceased donor transplant was increased by 22-times and when the likelihood of a pre-emptive living donor transplant was increased by 2.4-times. Little difference was found between these two treatments. One-way sensitivity analysis did not change the cost effectiveness except for costs of chronic hemodialysis and a living donor transplant in subsequent years.
Limitations:
It is difficult to increase the rate of transplant overall in the shorter term nationally and internationally.
Conclusions:
Appropriate distribution of all transplant options and hemodialysis is necessary to achieve the most cost-effective solution.
Introduction
The number of patients with end-stage kidney disease (ESKD) continues to increase and the consequent rises in medical costs for renal replacement therapy (RRT) is cause for socioeconomic concern worldwide. RRT, which can include hemodialysis (HD), peritoneal dialysis (PD), and renal transplant, is not a curative treatment for chronic kidney disease, but rather is palliative. In 2008, Japan had 2153 dialysis patients per million population and 1201 kidney transplants were performed, 82.5% of which involved living donorsCitation1,Citation2. In 2003, it was estimated that the annual expenditure per ESKD patient in Japan was US$41,681 (Purchasing Power Parity 2003), an estimate which suggests that total ESRD expenditure accounted for 3.7% of Japan’s total health expenditure that yearCitation3. More recently, it was estimated that there are also more than 19 million potential chronic kidney disease (CKD) patients in JapanCitation4. With RRT now the standard treatment for ESKD, it is expected therefore that the number of RRT patients will rise by a much greater extent in the future. However, although RRT provides life-supporting treatments for renal failure, it also places restrictions on patients’ livesCitation5 as well as considerable financial strain on society. To date, however, there have been few clinical and economic assessments of RRT undertaken in Japan that take into account quality-of-life (QoL) as well as costs.
A Markov model can be used to assess the cost-effectiveness with respect to changes in the composition of RRT, and several studies to this end have been carried out in Denmark, Canada, Australia, and AustriaCitation6–9. The studies in Denmark and Canada predicted that the number of RRT and ESKD patients, respectively, would increaseCitation6,Citation7; the studies in Australia and Austria showed that increased provision of kidney transplants and PD contributes to reducing medical costs and improving quality-adjusted life years (QALY), and that the costs of RRT are reduced by increasing the numbers of patients initially receiving home dialysis with PD. These findings suggest that the cost-effectiveness of RRT is affected not only by the number of ESKD patients but also the composition of treatment; in other words, the treatment modalities usedCitation8,Citation9.
In Japan, a patient’s involvement is recommended in the decision-making process of selecting RRT modality if the patient’s health permits this. Inaguma et al.Citation10 indicated that, among patients with stage 4 and 5 CKD, 70% who participated in an educational program about their disease could prevent the progression of CKD, compared with only 30% of those who did not receive this education. Considering the national circumstances discussed above, it is necessary not only to improve the medical care system to promote prevention of the lifestyle-related diseases, which can help these patients prevent progression of their disease, but also to discuss the cost-effectiveness of the composition of the various RRT modalities available to them.
The purpose of this study was to evaluate the cost-effectiveness of RRT by using QALY, a measure of disease burden of both the quality and quantity of life years, when changing the composition of RRT. Here, medical costs per QALY are estimated as an indicator of cost-effectiveness for the treatment modalities, namely HD, PD, pre-emptive living donor transplant, living donor transplant, and deceased donor transplant. Living donor transplant has a high graft survival rate compared with deceased donor transplant. Additionally, pre-emptive living donor transplant is not affected by dialysis complications. Therefore, since differences exist between transplant options, living donor transplants, pre-emptive living donor transplants, and deceased donor transplants were considered independently.
Materials and methods
Constructing a Markov model
Our Markov cohort model is designed to assess the cost-effectiveness of RRT for new patients with ESKD, where ESKD is defined as a glomerular filtration rate of less than 5 ml/min. Markov cohort models simulate health trajectories by defining distinct health states and tracking transitions between these states. The models simulate the clinical course of individual patients, following simulated patients from entry into the model until deathCitation11,Citation12. shows our Markov cohort model for patients with ESKD. During each 1-year cycle, patients have the possibility of receiving HD, PD, PD and HD combination therapy (PD + HD), a living donor transplant, a deceased donor transplant, resumption of dialysis (after transplant), and death. First, a new ESKD patient requiring RRT chooses one of the RRT modalities of PD, HD, or living donor transplant. Here, the current RRT composition was based on a complete survey of RRT patients in Japan. Note that deceased donor transplant was dropped from the treatments selectable since it is not realistically feasible to perform one before dialysis starts due to constraints that, as a general rule, registration on the kidney transplant waiting list is possible only after a patient has starting dialysis and then patients waiting a longer time are given preference for organ donation. If the treatment modality chosen is not able to control the progression of ESKD, it is changed to another modality. Moving the patients between states is determined depending on the transition probabilities of maintaining RRT and of switching from one modality to another. We assigned a cost and quality-of-life weight (utility) to each health state and derived average values by modelling a large number of patients. Transition probabilities, QoL effects, and costs other than HD and PD costs were determined based on a review of the medical literature. The HD and PD costs were derived from actual data on patients undergoing dialysis ()Citation2,Citation13–21.
Figure 1. Markov state diagram for renal replacement therapy (RRT) for new end-stage kidney disease (ESKD) patients. Schematic representation of the decision model showing a Markov state diagram of the post-hospitalization course for patients with chronic kidney disease (CKD) receiving renal replacement therapy (RRT) in Japan. Circles indicate various health states; arrows, transitions between the various states.
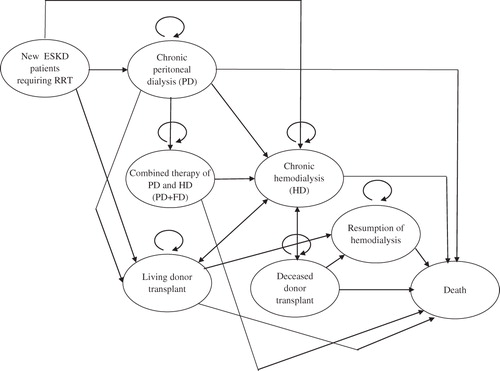
Table 1. Base-case values used in the Markov model for RRT in Japan.
Model assumptions
We made the following assumptions in the construction of our Markov cohort model. First, a patient diagnosed with ESKD was to select one of the RRT modalities of PD, HD, or living donor transplant. Second, as shown in , the patient was to continue treatment until the end of life. Third, the treatment period of PD was limited to a maximum of 8 years even if the patient experienced no problems with itCitation22. Fourth, PD patients could start PD + HD combination therapy in the event that PD efficiency decreased. Fifth, one cycle was set to 1 year. The total period of analysis was 15 years.
Costs
Medical costs were calculated assuming that, except for the introductory period of dialysis, patients received chronic dialysis (HD or PD) as an outpatient treatment. Furthermore, medical costs were calculated based on administrative fees for treatment, therapeutic agents, examinations, and outpatient care. The costs involved for a new ESKD patient requiring RRT and for each of PD, PD + HD, HD, and resumption of HD (after transplant) were obtained from doctor’s certificates. The costs of living donor transplant and deceased donor transplant for EKSD were estimated from studies by Higashiyama et al.Citation20 and Nakatani et al.Citation21. For kidney transplant (living, pre-emptive living, and deceased donor transplants), the transplant year and subsequent years were assigned two different costs. The equation for living donor transplant costs also included the medical costs associated with living donors.
For medical costs, only direct costs, not indirect costs such as labour costs, were calculated. All costs were converted into US dollars using the 2010 exchange rates as reported by the Organization for Economic Co-operation and Development (1 US$ = 87.761 Japanese Yen)Citation23. Costs and QALY were discounted using a rate of 3% per annumCitation24.
Cost-utility analysis
Health effects are expressed as quality-adjusted survival, calculated by integrating utility values over each simulated patient’s lifetime and expressed in terms of QALY. The utility values represent QoL on a standard 0–1 scale, where 1 is equal to perfect health and 0 represents death. The scored QoL (utility) needed in the calculation of QALY was determined either from scales based on preference or from investigation results of measured utility of RRT patients. The QoL scores were obtained from studies in the medical literature that had used the Health Utilities Index (details of 66 deceased transplant patients were examined)Citation17, the EQ-5D (details of 416 ESKD patients who were receiving HD, PD, living donor transplant, or pre-dialysis were examined)Citation18, or the standard gamble method (details of 66 deceased transplant patients were examined)Citation19 as a measure of health outcome. Utilities for health states were obtained from previously published studiesCitation17–19.
Results are reported as an incremental cost-effectiveness ratio (ICER: expressed as cost per QALY), calculated by dividing the mean difference in costs between two strategies by the mean difference in effectiveness. The ICER represents the incremental cost for each additional QALY gained when patients are treated with either further PD or kidney transplant. ICERs are considered favourable when the estimates are lower than the amount decision-makers would be willing to pay for an additional QALY gain: in the US, treatment is judged to be cost-effective when the ICER is $50,000 or lessCitation25.
Statistical analysis
Base composition of RRT denotes the current composition of RRT in regard to treatment modality. Alternatives for the composition of RRT represent a change of the RRT modality. To consider cost-effectiveness, we compared a base case with four alternatives.
For Alternative 1, the likelihood of starting with PD was increased by 2.3-times. This value was determined from the fact that PD accounted for 7.0% of all RRT in the US in 2008Citation2Citation6, while in Japan the figure was 3.1%Citation1; that is, the rate of PD in the US was 2.3-times that of Japan.
For Alternative 2, the likelihood of having a pre-emptive living donor transplant before some form of dialysis was increased by 2.4-times. As for Alternative 3, the likelihood of having a living donor transplant after some form of dialysis was increased by 2.4-times. Finally, for Alternative 4, after starting some form of dialysis, the likelihood of having a deceased donor transplant was increased by 22-times. These values were decided given the following. By the end of 2008, there were 991 living donor transplant patients and 210 deceased donor transplant patients in JapanCitation2, with corresponding numbers of 5584 and 10,820 in the USCitation26. Since Japan’s population is 127,704,000 and that of the US is 304,060,000Citation27, the number of deceased donor transplant patients in the US is 22.3-times that of Japan, and the number of living donor transplants, 2.4-times that of Japan.
Alternatives were tested over a range of plausible values to assess the robustness of uncertainties in the model’s parameter estimates in the one-way sensitivity analyses. The sensitivity ranges for each parameter tested are shown in . For the sensitivity analysis, 95% confidence intervals of utilities, and costs were used. Because 95% confidence intervals could not be obtained, transplant costs were changed between −50% and 50% of the average. All analyses were performed using the TreeAge Pro 2009 software program (TreeAge Software, Williamstown, MA).
Ethical considerations
When collecting information on general medical examinations from nephrologists to calculate the medical costs, the data obtained already had all personal information deleted. This study was approved by the Ethics Committee of Niigata University Faculty of Medicine.
Results
Base-case analysis ()
The results of the cost-effectiveness analysis are shown in . For the base composition of RRT, total costs 15 years later were $349,152 and total QALY was 4.099. Alternatives 2 (likelihood of a pre-emptive living donor transplant increased by 2.4-times), 3 (likelihood of a living donor transplant increased by 2.4-times), and 4 (likelihood of a deceased donor transplant increased by 22-times) were dominant (i.e., were more effective and less costly). Overall, Alternative 3 (likelihood of a living donor transplant increased by 2.4-times) was most effective and least costly, with total costs of $341,002 and total QALY of 4.871. Alternative 1 (likelihood of starting with PD increased by 2.3-times) was more effective: the ICER of Alternative 1 was $3059/QALY, which is much less than the $50,000/QALY deemed to be cost-effective in the US.
Table 2. Base-case analysis (no discount).
Discounted cost-effectiveness ()
As a result of discounting medical costs by 3%, the base composition of RRT was $84,008/QALY, with total costs 15 years later of $297,723 and total QALY of 3.544. Alternatives 2 (likelihood of a pre-emptive living donor transplant increased by 2.4-times), 3 (likelihood of a living donor transplant increased by 2.4-times), and 4 (likelihood of a deceased donor transplant increased by 22-times) were dominant. Overall, Alternative 3 (likelihood of a living donor transplant increased by 2.4-times) was most effective and least costly at $70,581/QALY, with total costs of $291,358 and total QALY of 4.128.
Table 3. Base-case analysis: discounted at 3%.
The marginally higher value for QALY at marginally higher cost translated into an ICER of $5,645 for Alternative 1 in comparison to the base composition of RRT.
Sensitivity analysis ()
shows the results of the sensitivity analysis. In the parameters of utilities, Alternatives 2 (likelihood of a pre-emptive living donor transplant increased by 2.4-times), 3 (likelihood of a living donor transplant increased by 2.4-times), and 4 (likelihood of a deceased donor transplant increased by 22-times) resulted in more QALY and reduced lifetime costs in comparison with the base composition of RRT. When the cost of HD in subsequent years was lower, total costs rose above the base composition of RRT for Alternatives 2, 3, and 4 and ICERs ranged from $4942–$16,457. A similar case was seen for the cost of a living donor transplant in subsequent years: ICERs ranged from $26,182–$40,476 for Alternatives 2, 3, and 4. ICERs were all less than $50,000/QALY, except in the case of a living donor transplant in subsequent years for Alternative 1 (likelihood of starting with PD increased by 2.3-times).
Table 4. One-way sensitivity analysis.
Discussion
By using a Markov model utilizing transition probabilities data as input parameters, this study assessed how the cost-effectiveness of the composition of RRT changed over time in Japan. As a result, the current composition of RRT carried the highest total costs and at the same time had low total QALY. The most cost-effective RRT was when the likelihood of a living donor transplant was increased by 2.4-times, followed in order by when the likelihood of a deceased donor transplant was increased by 22-times, a pre-emptive living donor transplant was increased by 2.4-times, and starting with PD was increased by 2.3-times. These findings concur with the results of previous studies showing that an increase in the rate of kidney transplant reduces RRT costs and increases patient survival in most developed countriesCitation8,Citation28. Although the cost data used in the present study is unique to RRT provided in Japan, similar to all high-income countries, the cost-effectiveness of transplant is better than that of the other modalities. From the viewpoint of cost-effectiveness of RRT, there appears to be a need to correct the composition of RRT in Japan, where chronic HD accounts for 96.8%Citation1. While it will be difficult, within a short time frame, to increase the number of kidney transplants conducted nationally as well as internationally, the results of this study do suggest that kidney transplant should be promoted, and ways to do this will now be examined.
In Japan, only 600 or so kidney transplants were performed annually up to the mid-1990s, but this had climbed to more than 1000 cases in FY2008 due to the increased number of living donor transplants carried out. Currently, living donor transplants account for 80% of all kidney transplants, and there has been no increase in deceased donor transplants in recent yearsCitation29. Since more than 50% of kidney transplants in the US involve a deceased donorCitation26, the high rate of living donor transplants is characteristic of the situation in Japan. In this study, the likelihood of a patient receiving a deceased donor transplant was increased by 22-times. However, such rapid growth in deceased donor transplants is difficult to realize, because ethnographic research has identified that Japan departs radically from the traditional notion still prevalent in Western Europe that organ donation is the ultimate altruistic giftCitation30. Nevertheless, it is inevitable that living donors will suffer pain and possible morbidity, so it is desirable to increase the rate of deceased donor transplants in the future.
Compared to kidney donation from donors after cardiac death, the outcome of transplant is better for donation from a donor after brain deathCitation31. Moreover, even for deceased donor transplant, it has been reported that, with careful selection of the donor and with organ preservation, success rates can be improvedCitation32. Between 1997 (when the Act on Organ Transplant was enforced in Japan) and as of October 11, 2011, 181 cases of kidney transplant after brain death were performed nationallyCitation33. Since it is difficult to increase the number of donations from deceased persons and, thus, deceased donor transplants over the short-term, further improvement in kidney transplant techniques is urgently needed. In Japan, amendment of the Act on Organ Transplantation in 2010 now permits the removal of organs for donation with the consent of family membersCitation34, and this measure is expected to increase the number of kidney transplants performed after brain death.
Little difference was found between the costs when the likelihood of deceased donor transplant was increased by 22-times, and those when the likelihood of pre-emptive living donor transplant was increased by 2.4-times. According to an Australian study, living donor transplant before introducing chronic dialysis was better in terms of both success rate of transplant and survival rate compared to living donor transplant after chronic dialysisCitation35. In 2008, only 15.1% of living donor transplants in Japan were carried out before introducing chronic dialysisCitation2, so there is yet room for improvement. Pre-emptive living donor transplants are certainly not the norm, and it is important to disseminate information about their existence. Appropriate distribution is also necessary for living donor transplants, pre-emptive living donor transplants, and HD, in parallel with examining how best to increase the rate of kidney transplants after brain death.
The results of the sensitivity analysis revealed that HD costs were an important parameter affecting cost-effectiveness. This is because HD accounts for most RRT received in Japan. Although the medical costs for chronic HD are high, HD is considered to be a therapy of an advanced-nation levelCitation36,Citation37. As for the medical fees for chronic HD, according to the recent Research and Report on Actual Conditions of Dialysis Medical CostsCitation38, a single HD treatment cost $396 in 2001, but had reduced to $351 in 2009. This is attributable to Japan’s clear cost reduction efforts for medical fees, such as abolition of fees for every hour of hemodialysis provided in 2002 (restored in 2008), adoption of the Diagnosis Procedure Combination payment system for erythropoietin (epo) treatment costs in 2006, and a major drop in the cost of dialyzers in 2008. In addition, Japan’s health insurance system has instituted a bundling policy that now includes epo in outpatient HD therapyCitation39. In research conducted at 14 university hospitals in Japan, epo treatment costs have been reduced for formulations of erythropoietin-alpha and -beta, although they have increased for formulations of darbepoetin, making it possible overall to cut costs for the duration of action. As epo is covered under the Diagnosis Procedure Combination system, there is the possibility that using epo as part of outpatient hemodialysis therapy may increase the costs of dialysis facilities. Despite implementing a drastic cost-cutting policy, Japanese HD care has retained healthcare outcomes for ESKD patients that are considered some of the best in the worldCitation40. In actuality, the number of patients receiving dialysis for more than 25 years in Japan reached 10,017 in 2008, while one patient who had been on dialysis for 40 years is worthy of special mentionCitation1. However, the drive for further reduction in the medical costs of chronic HD may yet deteriorate its quality.
Conclusions
The current composition of RRT carried the highest total costs and at the same time had low total QALY. The most cost-effective treatment was when the likelihood of a living donor transplant was increased by 2.4-times. Compared with the base composition of RRT, the dominant treatments with respect to cost-effectiveness were when the likelihood of a deceased donor transplant was increased by 22-times and when the likelihood of a pre-emptive living donor transplant was increased by 2.4-times. Little difference was found between these two treatments. Appropriate distribution of all transplant options and HD are necessary to achieve the most cost-effective solution.
Transparency
Declaration of funding
This study was provided data from the Association of Platform for Clinical Information Statistical Analysis (NTT DATA Co., Tokyo, Japan).
Declaration of financial/other relationships
None of the authors have any other financial relationships pertaining to this study to disclose.
References
- Nakai S, Suzuki K, Masakane I, et al. Overview of regular dialysis treatment in Japan (as of 31 December 2008). Ther Apher Dial 2010;14:505‐40
- The Japanese Society for Clinical Renal Transplantation. Annual Progress Report from the Japanese Renal Transplant Registry: number of renal transplantation in 2008, part 2. Jpn J Transplant 2009;44:548‐58 [Japanese]
- Organisation for Economic Co-operation and Development Advisory. OECD statistical profile for Japan – 2006. OECD Statistics v.4.3, 2006. http://stats.oecd.org/wbos/viewhtml.aspx?query name=321&querytype=view&lang=en. Accessed March 30, 2011
- Imai E, Horio M, Watanabe T, et al. Prevalence of chronic kidney disease in the Japanese general population. Clin Exp Nephrol 2009;13:621-30
- Foley RN, Parfrey PS, Sarnak MJ. Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis 1998;32:112-9
- Vestergaard P, Løkkegaard H. Predicting future trends in the number of patients on renal replacement therapy in Denmark. Nephrol Dial Transplant 1997;12:2117-23
- Schaubel DE, Morrison HI, Desmeules M, et al. End-stage renal disease in Canada: prevalence projections to 2005. CMAJ 1999;160:1557--63
- Howard K, Salkeld G, White S, et al. The cost-effectiveness of increasing kidney transplantation and home-based dialysis. Nephrology (Carlton) 2009;14:123-32
- Haller M, Gutjahr G, Kramar R, et al. Cost-effectiveness analysis of renal replacement therapy in Austria. Nephrol Dial Transplant 2011;26:2988-95
- Inaguma D, Tatematsu M, Shinjo H, et al. Effect of an educational program on the predialysis period for patients with chronic renal failure. Clin Exp Nephrol 2006;10:274-8
- Beck JR, Pauker SG. Markov models in medical process in Medical prognosis. Med Decis Making 1983;3:419-58
- Sonnenberg FA, Beak JR. Markov models in medical decision making: a practical guide. Med Decis Making 1993;13:322-38
- The Japanese Society for Dialysis Therapy. An overview of regular dialysis treatment in Japan as of December 31, 2008 (CD-R version), 2009 [Japanese]
- Mitome J, Yamamoto H, Kato N, et al. Dialysis as bridge therapy for renal transplantation: single center experience, a comparison of hemodialysis and continuous ambulatory peritoneal dialysis. Jpn J Nephrol 2005;47:813-20 [Japanese]
- Matsuo N, Maruyama Y, Terawaki H, et al. Risk factors for death in patients starting PD for their first renal replacement therapy. Jpn J Nephrol 2009;51:38-43 [Japanese]
- The Japanese Society for Clinical Renal Transplantation, The Japanese Society for Transplantation. Annual progress report from the Japanese Renal Transplant Registry, 2007: part III: results from 2006 follow-up survey. Jpn J Transplant 2007;6:545-57 [Japanese]
- Gorodetskaya I, Zenios S, McCulloch CE, et al. Health-related quality of life and estimates of utility in chronic kidney disease. Kidney Int 2005;68:2801-8
- Lee AJ, Morgan CL, Conway P, et al. Characterisation and comparison of health-related quality of life for patients with renal failure. Curr Med Res Opin 2005;21:1777-83
- Groome PA, Hutchinson TA, Tousignant P, et al. The repeatability of three methods for measuring prospective patients' values in the context of treatment choice for end-stage renal disease. J Clin Epidemiol 1999;52:849-60
- Higashiyama A, Okamura T, Watanabe M, et al. Effect of chronic kidney disease on individual and population medical expenditures in the Japanese population. Hypertens Res 2009;32:450-4
- Nakatani T, Uchida J, Naganuma T. Health economics of kidney transplant. Jpn J Transplant 2009;44:18-25 [Japanese]
- Kawanishi H, Kawaguchi Y, Fukui H, et al. Encapsulating peritoneal sclerosis in Japan: a prospective, controlled, multicenter study. Am J Kidney Dis 2004;44:729-37
- Organisation for Economic Co-operation and Development Advisory. OECD Economic Outlook No. 89 Annex Tables 36 - Table of Contents, 2010. http://www.oecd.org/document/3/0,3746,en_2649_34573_2483901_1_1_1_1,00.html. Accessed September 3, 2011
- Drummond MF, Sculpher MJ, Torrance GW, et al. Methods for the Economic Evaluation of Health Care Programmes. 3rd edn. New York, NY: Oxford University Press, 2005. p 103-36
- Hirth RA, Chernew ME, Miller E, et al. Willingness to pay for a quality-adjusted life year: in search of a standard. Med Decis Making 2000;20:332-42
- United States Renal Data System. Annual Data Report 2010 Atlas of CKD & ESRD. Transplantation 2010;2:311–24. http://www.usrds.org/atlas.htm. Accessed October 2, 2010
- United Nations. Demographic Yearbook Regular Issues 2008. 2008, p 116–54. http://unstats.un.org/unsd/demographic/products/dyb/2000_round.htm. Accessed March 31, 2011
- Winkelmayer WC, Weinstein MC, Mittleman MA, et al. Health economic evaluations: the special case of end-stage renal disease treatment. Med Decis Making 2002;22:417-30
- The Japan Society for Transplantation. Fact book of organ transplant, 2010. http://www.asas.or.jp/jst/report_top.html. Accessed September 1, 2011 [Japanese]
- Crowley-Matoka M, Lock M. Organ transplantation in a globalised world. Mortality 2006;11:166-81
- Singh RP, Farney AC, Rogers J, et al. Kidney transplantation from donation after cardiac death donors. lack of impact of delayed graft function on post-transplant outcomes. Clin Transplant 2010;25:255-64
- Hoogland ER, Snoeijs MG, van Heurn LW. DCD kidney transplantation: results and measures to improve outcome. Curr Opin Organ Transplant 2010;15:177-82
- Japan Organ Transplant Network. Data about the transplant analysis of brain-dead donor transplant, 2011. http://www.jotnw.or.jp/datafile/offer_brain.html. Accessed October 2, 2010 [Japanese]
- Aita K. New organ transplant policies in Japan, including the family-oriented priority donation clause. Transplantation 2011;91:489-91
- Milton CA, Russ GR, McDonald SP. Pre-emptive renal transplantation from living donors in Australia: effect on allograft and patient survival. Nephrology (Carlton) 2008;13:535-40
- Hidai H. International comparison of dialysis cost -- particularly for health economics of low-income countries. J Jpn Assoc Dial Physicians 2005;20:145-52 [Japanese]
- Takemoto Y, Naganuma T. International comparison of dialysis. J Jpn Assoc Dial Physicians 2007;22:64-8 [Japanese]
- Sugisaki H, Ota Y, Kuma H, et al. The thirteenth report on the fact-finding survey of dialysis cost dialysis cost. J Jpn Assoc Dial Physicians 2010;25:56-86 [Japanese]
- Hasegawa T, Bragg-Gresham JL, Pisoni RL, et al. Changes in anemia management and hemoglobin levels following revision of a bundling policy to incorporate recombinant human erythropoietin. Kidney Int 2011;79:340-6
- Fukuhara S, Yamazaki C, Hayashino Y, et al. The organization and financing of end-stage renal disease treatment in Japan. Int J Health Care Finance Econ 2007;7:217-31
