Abstract
Objectives:
The ATHENA study showed that use of dronedarone reduced rates of first cardiovascular (CV) hospitalization in atrial fibrillation/flutter (AF/AFL) patients. AF is associated with high costs to payers, which are driven by high rates of hospitalization. This retrospective cohort study examined readmission patterns and costs to US payers in real-world AF/AFL patients with ≥1 additional risk factor (ARF).
Methods:
Patients hospitalized (January 2005–March 2008) with AF/AFL as primary diagnosis and having ≥1 year of health coverage, before and after their first (index) admission, were identified in the PharMetrics Patient-Centric database. As in the ATHENA study, patients had to be ≥75 years of age or ≥70 years, with ≥1 ARF. Rehospitalization patterns (all-cause, all CV-related [including AF/AFL] and AF/AFL-related alone) were examined over 1 year post-index, and costs of index vs later AF/AFL admissions compared.
Results:
The study included 3498 patients (mean 80 [SD 7.6] years; 42.4% men). Over 1 year, 1389 patients (39.7%) were rehospitalized for any cause (mean 1.7 [SD 1.3] events/patient), with 1223 patients (35.0%) undergoing CV-related (mean 1.6 [SD 1.0] events/patient) and 935 (26.7%) undergoing AF-related rehospitalization (mean 1.4 [SD 0.8] events/patient). Common causes of CV-related readmissions (primary diagnosis) were AF/AFL (47.5%), congestive heart failure (CHF) (9.9%), coronary artery disease (7.4%), and stroke/transient ischemic attack (6.2%). Readmission rates at 3 months were 16.2% (all-cause), 14.3% (all CV-related including AF/AFL), and 10.5% (AF/AFL-related alone). AF/AFL readmissions (primary diagnosis) were longer than initial hospitalizations (mean total 6.9 [SD 12.9] vs 4.3 [SD 5.1] days, p < 0.0001) and more costly (median $1819 [25th percentile $1066, 75th percentile $5623] vs $1707 [25th percentile $1102, 75th percentile $4749]).
Limitations:
This study excluded patients with pre-existing CHF, did not require electrocardiogram confirmation of AF/AFL diagnosis, and did not distinguish between paroxysmal, persistent, and permanent AF.
Conclusions:
AF/AFL patients with ≥1 ARF have high readmission rates. AF/AFL-related readmissions incur higher costs than the initial AF/AFL admissions.
Introduction
Atrial fibrillation (AF) and atrial flutter (AFL) affect ∼3.3 million individuals in the US, and are associated with increased cardiovascular (CV) and cerebrovascular riskCitation1. Patients with AF and/or AFL are significantly more likely than age-matched non-AF/AFL patients to have co-morbidities such as ischemic stroke, congestive heart failure (CHF), valvular heart disease, coronary artery disease, peripheral vascular disease, pulmonary disease, thyroid disease, diabetes mellitus, or hypertensionCitation1. Moreover, the presence of AF and/or AFL puts patients at increased risk of hospitalization or deathCitation2,Citation3.
AF and AFL are associated with high healthcare costs, driven in particular by high rates of CV-related hospitalizationCitation4–8. For example, the incremental cost of AF in the US was projected to reach $26.0 billion in 2010, of which $16.4 billion (63%) represented inpatient costsCitation8. A retrospective, cohort study of 4174 patients hospitalized with primary AF found that 12.5% and 10.1% of chronic AF and newly-diagnosed AF patients, respectively, were rehospitalized within 1 year of their index hospitalization with an AF-related diagnosis. The majority of these patients were readmitted within the first 6 monthsCitation5.
Until recently, anti-arrhythmic drug therapy had not been demonstrated to reduce the risk of hospitalization in AF or AFL. ATHENA (A placebo-controlled, double-blind, parallel arm Trial to assess the efficacy of dronedarone 400 mg bid for the prevention of cardiovascular Hospitalization or death from any cause in patiENts with Atrial fibrillation/atrial flutter) was the first randomized controlled study to demonstrate that anti-arrhythmic drug therapy (dronedarone) could reduce the risk of CV-related hospitalization and death in AF/AFL patients. This study demonstrated significant reductions in the incidence of first CV hospitalization (−26%), CV death (−29%), and arrhythmic death (−45%) with use of dronedarone compared with placebo over a 12–30-month follow-up periodCitation9. However, the ATHENA study adopted the end-point of first hospitalization, and did not examine subsequent rehospitalization events.
Hospital readmission has become the focus of much attention in the current healthcare debate in the US, with healthcare reformers proposing to cut spending and improve quality of care by penalizing institutions with high readmission rates. This has been prompted by the very high costs of unplanned rehospitalizations, with one estimate suggesting a cost of ∼$17.4 billion per year to Medicare aloneCitation10, of which ∼$12.0 billion for patients readmitted within 30 days is potentially preventableCitation11. The recent ‘Hospital to Home’ national quality improvement initiative of the American College of Cardiology and Institute for Healthcare Improvement aims to reduce all-cause readmission rates among patients hospitalized with heart failure and acute myocardial infarction. This initiative may be expanded to cover other CV conditions that are also characterized by high rates of hospital readmission.
An important question regarding chronic conditions associated with multiple hospitalizations, such as AF, is whether the patient’s condition is worsening over time. One way of assessing this would be to compare the initial hospitalization with subsequent readmissions: if each readmission requires a longer stay in hospital and a greater level of intervention, then this would suggest that the patient’s condition was worsening. The aim of the present analysis was to determine the temporal pattern and cost of rehospitalization (relative to the initial hospitalization) among a cohort of hospitalized AF/AFL patients, with ≥1 additional risk factor (ARF), in the real-world setting.
Patients and methods
Study design
This was a retrospective cohort study using data from the PharMetrics Patient-Centric database (IMS Health, Danbury, CT) covering the period between January 1, 2004 and March 31, 2009. This database contains fully adjudicated medical and pharmaceutical claims from commercial health plan information collected from >94 different managed care organizations in addition to Medicare. The database includes information on outpatient pharmacy claims and medical hospitalization claims with discharge diagnoses as well as health plan costs from the third-party payer’s perspective. Data from this database have been used in several previous health outcome studiesCitation12–16.
Patient selection
Adult patients hospitalized (index hospitalization identification period January 2005–March 2008) with AF/AFL as the primary diagnosis (International Classification of Diseases, ninth revision, Clinical Modification [ICD-9-CM] codes 427.31 and 427.32, respectively) were identified. In accordance with the published patient selection criteria of the ATHENA trialCitation9, the AF/AFL patients included in this analyses (i.e., with ≥1 ARF) were required to be: (1) aged ≥75 years regardless of co-morbidities (as advanced age was considered an ARF); or (2) aged 70–74 years with ≥1 of the following additional CV risk factors: arterial hypertension, diabetes, arterial/pulmonary embolism, or stroke/transient ischemic attack (TIA). Patients were also required to have ≥12 months of continuous medical and prescription drug coverage both prior to and following their first hospitalization with a primary diagnosis of AF/AFL (the index event). As in the ATHENA study, patients were excluded from the analysis if they had a diagnosis of acute myocarditis or end-stage renal disease during the 12-month period preceding the index AF/AFL event. Patients in the ATHENA trial were not automatically excluded if they had a diagnosis of CHF. Patients with New York Heart Association (NYHA) Class I, II, and III CHF were included in the ATHENA trial and those with Class IV CHF were excluded. In our study, it was not possible to identify NYHA CHF class; therefore we took the conservative approach of excluding all patients with CHF.
Study end-points
Information was collected on gender, age, geographic region, health plan type, co-morbidities, Charlson co-morbidity index (CCI), and CHADS2 index. The CCI was used as a composite measure of co-morbidity burdenCitation17, and the CHADS2 score was used as a measure of stroke riskCitation18,Citation19.
The temporal pattern of rehospitalization (categorized as all-cause, all CV-related [including AF/AFL], and AF/AFL-related alone) was assessed over the 12-month post-index period. CV-related rehospitalizations encompassed admissions with a primary or secondary diagnosis of circulatory system disease (ICD-9-CM codes 390–459.9) and included AF-related rehospitalizations, which were defined as admissions with a primary or secondary diagnosis of AF/AFL (ICD-9-CM codes 427.31 and 427.32, respectively). CV- and AF/AFL-related rehospitalizations were further sub-classified into those with a CV or AF/AFL primary diagnosis at hospital discharge. CV causes were further categorized based on the pre-specified main causes for CV hospitalization in the ATHENA studyCitation20, which are as follows: AF/AFL, CHF, coronary atherosclerosis, TIA/stroke, blood pressure-related, acute myocardial infarction/intermediate coronary syndrome, ventricular arrhythmia, major bleeding, supraventricular rhythm disorder, venous thromboembolism, angina pectoris/chest pain, and other CV events.
Rehospitalization parameters included time to readmission (number of days between the index hospitalization and the first readmission during the 12-month post-index period), frequency of readmission, and reason for rehospitalization (e.g., all-cause, CV-associated [including AF/AFL-related], or AF/AFL-related alone). For the sub-set of AF/AFL patients with ≥1 ARF who underwent hospital readmission with AF/AFL as the primary discharge diagnosis, the cost of the first post-index rehospitalization (hospital and physician payments) was compared with the cost of the index AF/AFL hospitalization. The length of stay of the first post-index rehospitalization was also compared with that of the index hospitalization within this sub-set. These comparisons used the same patients for initial hospitalization and rehospitalization; therefore, demographics and co-morbidities were self-matched, with each patient serving as their own control.
Statistical analyses
Patient demographics, clinical characteristics, resource use, and cost data were summarized using descriptive statistics. Comparisons of rehospitalization duration and costs between index AF/AFL hospitalizations and subsequent rehospitalizations for AF/AFL were performed using the Chi-square test for discrete variables and Student’s t-test for continuous variables. Logistic regression analysis, with a maximum likelihood, binary response method, and Fisher scoring algorithm, was used to assess potential predictors of rehospitalization (age, gender, US Census Bureau region, healthplan type, and CCI). Odds ratio estimates with Wald 95% confidence limits were reported for each regression parameter. A separate analysis was performed to analyze cardiovascular-related co-morbidities (hypertension, stroke, diabetes, peripheral vascular disease, coronary artery diseases, thyroid diseases, pulmonary diseases, valvular heart disease, and cardiomyopathy) in concert with the predictors. Statistical significance was considered to be a p-value of ≤0.05. All statistical analyses were performed using SAS 9.2.
Results
Patient population
A total of 38,258 hospitalized AF/AFL patients were identified in the database, of whom 3498 met the study inclusion criteria and were classified as having ≥1 ARF (). The AF/AFL patients with ≥1 ARF had a mean age of 80.0 years (SD = 7.6 years), 42.4% were male, and they had high levels of co-morbidity and stroke risk (mean baseline CCI 1.7 [SD 1.8] and CHADS2 score 2.2 [SD 1.0]) ().
Figure 1. Patient identification and selection. AF, atrial fibrillation; AFL, atrial flutter; ARF, additional risk factor(s); ESRD, end-stage renal disease; HF, heart failure.
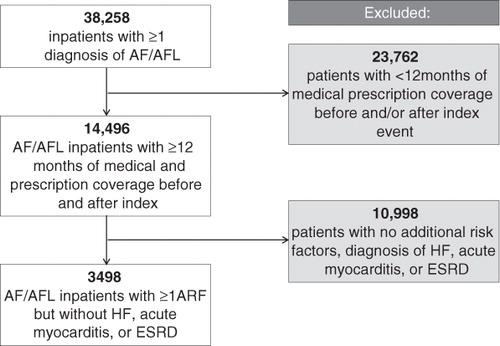
Table 1. Baseline demographic and clinical characteristics of AF/AFL patients with ≥1 ARF.
Pattern of rehospitalization
In total, 1389 (39.7%) of the 3498 AF/AFL patients with ≥1 ARF were rehospitalized (all causes) over the 12-month post-index period (mean 1.7 [SD 1.3] readmissions per rehospitalized patient) ( and ). Of these, 1223 patients (35.0% of the study cohort) underwent a CV-related rehospitalization (mean 1.6 [SD 1.0] readmissions per rehospitalized patient), which included AF/AFL-related readmissions. When AF/AFL-related rehospitalizations were assessed alone, 935 patients (26.7% of the study cohort) were rehospitalized (mean 1.4 [SD 0.8] readmissions per rehospitalized patient). Rehospitalization with a CV or AF/AFL primary diagnosis occurred in 804 (23.0%) patients (mean 1.4 [SD 0.7] readmissions per rehospitalized patient) and 426 (12.2%) patients (mean 1.2 [SD 0.5] readmissions per rehospitalized patient), respectively. The most frequent causes of readmission with a CV primary diagnosis were AF/AFL (521/1097 total primary CV readmissions, 47.5%), CHF (109/1097, 9.9%), coronary artery disease (81/1097, 7.4%), and stroke/TIA (68/1097, 6.2%) ().
Figure 2. Rehospitalization rates (percentage of patients) for all-cause rehospitalizations, among all AF/AFL patients with ≥1 ARF (n = 3498). AF, atrial fibrillation; AFL, atrial flutter; CV, cardiovascular. *Includes AF/AFL-related rehospitalizations.
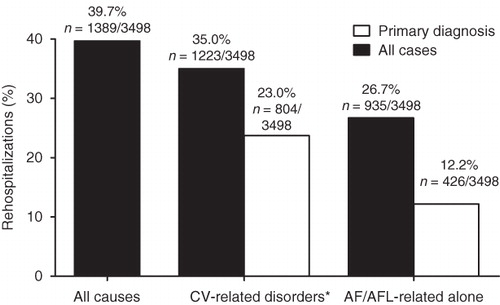
Figure 3. Mean (± SD) number of readmissions per patient among the sub-group of rehospitalized AF/AFL patients with ≥1 ARF (n = 1389). AF, atrial fibrillation; AFL, atrial flutter; CV, cardiovascular. *Includes AF/AFL-related rehospitalizations.
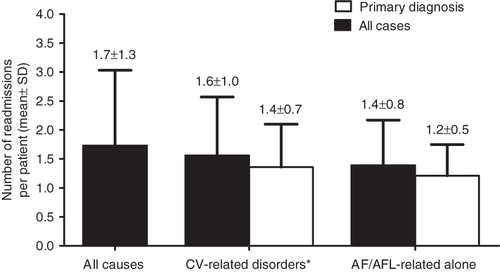
Table 2. Specific causes of readmission with a CV-related primary diagnosis among AF/AFL patients with ≥1 ARF.
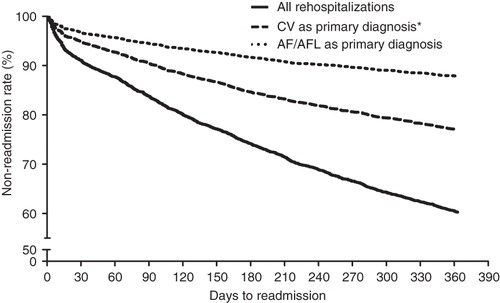
Cumulative readmission rates over the 12-month post-index follow-up period are summarized graphically (). Cumulative all-cause rehospitalization rates at 1, 3, and 6 months’ follow-up were 9.0%, 16.2%, and 25.9%, respectively. Cumulative rehospitalization rates with a CV (including AF/AFL) or AF/AFL primary diagnosis alone, respectively, were 5.1% and 3.3% at 1 month, 9.5% and 5.6% at 3 months, and 15.4% and 8.4% at 6 months. For those AF/AFL patients with ≥1 ARF who were readmitted with a primary diagnosis of AF/AFL (n = 426), 26.8%, 45.5%, and 68.5% of all such readmissions recorded over the 12-month follow-up period occurred within 1, 3, and 6 months, respectively, of the index event. Corresponding figures for readmissions with a CV primary diagnosis (n = 804) at 1, 3, and 6 months were 22.3%, 41.4%, and 66.8%, respectively.
Predictors of rehospitalization
Linear regression analysis indicated that co-morbidity identified by a CCI score of ≥5 (vs a CCI score of 0)—and specifically hypertension, peripheral vascular disease, coronary artery disease and valvular heart disease—were significant predictors of all-cause and CV rehospitalization. Age over 80 years vs age 70–74 years and female gender compared with male gender were also significant predictors of all-cause and CV rehospitalization. This analysis also identified some geographic variation in the risk of rehospitalization.
Rehospitalization costs and resource utilization
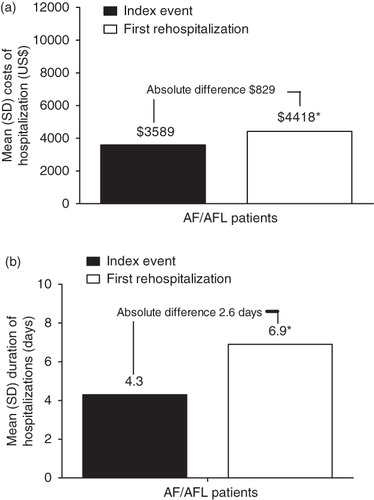
For the sub-set of AF/AFL patients with ≥1 ARF who underwent an AF/AFL-related rehospitalization, the cost of the first rehospitalization with a primary diagnosis of AF/AFL was significantly higher than the cost of the corresponding index hospitalization (mean US$4418 [SD $6294] vs $3589 [SD $4194], p = 0.0036) (). The median costs of rehospitalization compared with index hospitalization were $1819 [25th percentile $1066, 75th percentile $5623] vs $1707 [25th percentile $1102, 75th percentile $4749]). In addition, the duration of hospital stay was on average 2.6 days longer on readmission compared with the index event (mean 6.9 [SD 12.9] vs 4.3 [SD 5.1 days], p < 0.0001) ().
Discussion
According to this analysis of the PharMetrics Patient-Centric database, almost two out of five (39.7%) AF/AFL patients with ≥1 ARF were rehospitalized (all causes) during the 12-month period following their initial (index) AF/AFL-related hospitalization. Each of these patients underwent, on average, 1.7 rehospitalizations (all-cause) over this 12-month follow-up period. In the great majority of cases (88%), the cause of readmission was a CV-related disorder (including AF/AFL) and, more specifically, an AF/AFL-related disorder alone (67.3%). AF/AFL accounted for nearly half (47.5%) of all rehospitalizations with a CV-related primary diagnosis among AF/AFL patients with ≥1 ARF, making it the most common reason for readmission in these patients. As may be anticipated, clinical characteristics and demographics found to significantly predict CV and all-cause rehospitalization included advanced age and increased co-morbidity.
In this cohort of AF/AFL patients with ≥1 ARF, the rate of readmission with AF/AFL as the primary discharge diagnosis (12.2% over 12 months) was similar to that reported in an earlier retrospective cohort analysis, using the Integrated Health Care Information Services, Inc. (IHCIS) National Managed Care Benchmark database, of 4174 patients with newly diagnosed and chronic AF (10.1% and 12.5%, respectively, over 12 months)Citation5. In addition, the temporal patterns of readmission were similar in the two analyses. For example, in the present study, 26.8%, 45.5%, and 68.5% of first readmissions with primary AF/AFL occurred within 1, 3, and 6 months, respectively, of the index event compared with 17.6%, 43.4%, and 65.8% (chronic AF patients), and 22.7%, 44.5%, and 67.2% (newly diagnosed AF patients) of corresponding first readmissions in the earlier studyCitation5. However, in comparison with the former study, patients in the present analysis were older (mean age 80.0 vs 62.4–64.0 years) and had higher baseline levels of co-morbidity (mean CCI score 1.7 vs 0.8–1.0). This might explain why a higher percentage of AF/AFL readmissions occurred within 1 month in the AF/AFL patients identified in this study, with ≥1 ARF, as compared with a wider AF patient population assessed in the earlier study.
In comparison with the initial (index) hospitalization for primary AF/AFL, each subsequent rehospitalization for primary AF/AFL proved to be more protracted (mean 6.9 vs 4.5 days) and more costly (mean $4418 vs $3589; median costs $1819 vs $1707). The increased length of stay and cost of rehospitalization for primary AF/AFL may possibly be a reflection of disease progression and the need for more intensive inpatient care. It should be noted that regression analyses were not used to adjust for co-morbidity within resource utilization and costs associated with rehospitalization for primary AF/AFL, since this comparison was conducted within the same group of patients. Proportionately, the increase in mean hospital costs (23%) was substantially less than the increase in length of hospital stay (53%). This may be due to the use of a diagnosis-related group (DRG) or modified DRG payment system whereby hospital reimbursement might be capped or limited, regardless of the length of hospital stay. In this case, rehospitalization is likely to impose a financial burden on the hospital in addition to the payer. Based on the reported study average of 1.2 primary AF/AFL readmissions per rehospitalized patient, the estimated mean costs of the primary hospitalization and subsequent primary AF/AFL rehospitalizations over the 12-month post-index period amount to $8935 ($3589 +[1.2 × $4418]) per patient; based on median costs this value is $3890 ($1707 +[1.2 × $1819]). It should be emphasized, however, that these costs are applicable only to the small minority (12.2%) of the study population undergoing rehospitalization for primary AF during the post-index period. The costs for patients requiring rehospitalization due to other causes were not determined in this study.
Set against the background of the recent ‘Hospital to Home’ national quality improvement initiative and studies that have demonstrated the high cost burden of unscheduled hospital readmissionsCitation10,Citation11, the high rate of rehospitalization among AF/AFL patients highlights the need for renewed efforts to reduce hospitalizations and improve post-discharge transition of care across the spectrum of CV disease.
This study has several limitations. First, in contrast to the ATHENA study, which included patients with mild-to-moderate CHF (NYHA class II–III; who accounted for ∼20% of the study population) and excluded those with severe CHF (NYHA class IV), the present study excluded all patients with pre-existing CHF, since the claims data did not allow determination of CHF severity. Accordingly, this study is likely to have under-estimated the actual readmission rate among the real-world AF/AFL population with ≥1 ARF. Secondly, in contrast to the ATHENA study, which was confined to patients with paroxysmal or persistent AF, this analysis may have included patients with permanent AF, since the ICD-9-CM diagnostic codes do not differentiate between AF sub-types. Furthermore, in the present study, the diagnosis of AF/AFL was not required to be confirmed by electrocardiogram and the use of ICD-9-CM diagnostic codes on non-diagnostic claims introduces the potential for coding error. Another limitation is that the PharMetrics Patient-Centric database may be under-represented in certain geographic regions in the US (e.g., the West) and, therefore, these findings may not be fully representative of AF/AFL patients with ≥1 ARF nationwide.
Conclusion
In the real-world setting, AF/AFL patients with ≥1 ARF experience a high rate of rehospitalization after their initial admission. Subsequent AF/AFL-related readmissions incur higher medical costs to payers and longer inpatient stays compared with the initial AF/AFL admission. This increased resource utilization represents an economic burden on the healthcare system and is also likely to have a negative impact on patient wellbeing.
Transparency
Declaration of funding
Financial support for the research and manuscript development was provided by Sanofi-Aventis Inc.
Declaration of financial/other relationships
The authors received no financial support or other form of compensation related to the development of this paper. ANA has received funding for research and speaking from Sanofi-Aventis Inc. and Boehringer Ingelheim. MJ is an employee of Sanofi-Aventis Inc. JL is an employee of Novosys Health, which has a research consulting agreement with Sanofi-Aventis Inc.
Acknowledgments
Editorial/writing support was provided by Jon Edwards, PhD, and Andrew Fitton, PhD, of UBC-Envision Group and funded by Sanofi-Aventis Inc. Drs ANA, JL, and MJ were fully responsible for all content and editorial decisions.
Previous presentation
This study was presented as an oral presentation at the Heart Rhythm Society 32nd Annual Scientific Sessions, San Francisco, CA, USA, May 5, 2011 and the abstract was published in Heart Rhythm 2011;8 (5, Supplement):S212–213.
References
- Naccarelli GV, Varker H, Lin J, et al. Increasing prevalence of atrial fibrillation and flutter in the United States. Am J Cardiol 2009;104:1534-9
- Kannel WB, Wolf PA, Benjamin EJ, et al. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol 1998;82:2N-9N
- Stewart S, Hart CL, Hole DJ, et al. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med 2002;113:359-64
- Reynolds MR, Essebag V, Zimetbaum P, et al. Healthcare resource utilization and costs associated with recurrent episodes of atrial fibrillation: the FRACTAL registry. J Cardiovasc Electrophysiol 2007;18:628-33
- Kim MH, Lin J, Hussein M, et al. Incidence and temporal pattern of hospital readmissions for patients with atrial fibrillation. Curr Med Res Opin 2009;25:1215-20
- Kim MH, Lin J, Hussein M, et al. Cost of atrial fibrillation in United States managed care organizations. Adv Ther 2009;26:847-57
- Naccarelli GV, Johnston SS, Lin J, et al. Cost burden of cardiovascular hospitalization and mortality in ATHENA-like patients with atrial fibrillation/atrial flutter in the United States. Clin Cardiol 2010;33:270-9
- Kim MH, Johnston SS, Chu B-C, et al. Estimation of total incremental health care cost in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes 2011;4:313-20
- Hohnloser SH, Crijns HJ, van Eickels M, et al. Effect of dronedarone on cardiovascular events in atrial fibrillation. N Engl J Med 2009;360:668-78
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360:1418-28
- Medicare Payment Advisory Commission. Report to Congress: promoting greater efficiency in medicare. Washington, DC: 2007. http://www.medpac.gov/documents/jun07_entirereport.pdf. Accessed October 10, 2011
- Spyropoulos AC, Hussein M, Lin J, et al. Rates of symptomatic venous thromboembolism in US surgical patients: a retrospective administrative database study. J Thromb Thrombolysis 2009;28:458-64
- Prescott JD, Factor S, Pill M, et al. Descriptive analysis of the direct medical costs of multiple sclerosis in 2004 using administrative claims in a large nationwide database. J Manag Care Pharm 2007;13:44-52
- Gore M, Sadosky A, Zlateva G, et al. Initial use of pregabalin, patterns of pain-related pharmacotherapy, and healthcare resource use among older patients with fibromyalgia. Am J Manag Care 2010;16:S144-53
- Lang K, Sussman M, Friedman M, et al. Incidence and costs of treatment-related complications among patients with advanced squamous cell carcinoma of the head and neck. Arch Otolaryngol Head Neck Surg 2009;135:582-8
- Kim MH, Klingman D, Lin J, et al. Patterns and predictors of discontinuation of rhythm-control drug therapy in patients with newly diagnosed atrial fibrillation. Pharmacotherapy 2009;29:1417-26
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83
- Gage BF, Waterman AD, Shannon W, et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 2001;285:2864-70
- Hughes M, Lip GY. Stroke and thromboembolism in atrial fibrillation: a systematic review of stroke risk factors, risk stratification schema and cost effectiveness data. Thromb Haemost 2008;99:295-304
- Hohnloser SH, Connolly SJ, Crijns HJ, et al. Rationale and design of ATHENA: a placebo-controlled, double-blind, parallel arm Trial to assess the efficacy of dronedarone 400 mg bid for the prevention of cardiovascular Hospitalization or death from any cause in patiENts with Atrial fibrillation/atrial flutter. J Cardiovasc Electrophysiol 2008;19:69-73