Abstract
Objective:
To assess the economic burden in direct healthcare utilization and costs for refractory epileptic patients with partial onset seizures (POS) and assess the antiepileptic drug (AED) treatment patterns among these patients.
Methods:
This retrospective database study analyzed administrative claims of commercially-insured patients with POS from 2004–2008. Healthcare costs and utilization were compared between refractory (defined as ≥3 AEDs) and non-refractory patients by calendar year and AED treatment patterns were described for refractory patients.
Results:
Of the 79,149 patients identified (mean age 33 years; 54.8% female), 8714 (11%) were classified as refractory. In 2008, average annual healthcare costs for refractory patients were significantly higher than non-refractory patients ($33,613 vs $19,085), also by settings for inpatient ($11,780 vs $6076), outpatient ($13,431 vs $8637), and pharmacy costs ($8402 vs $4372) (all p < 0.001). Among refractory patients, close to one-third of total costs were for POS-related services. Similar trends were observed when assessing POS-related utilization and costs. The differences were consistent across all calendar years examined. Among refractory patients, 80.5% were on monotherapy at the beginning of the follow-up period. Levetiracetam is the common AED in mono/combination therapy as well as add-on/switch-to.
Limitations:
The onset of seizure cannot be identified, and the indication of each AED could not be confirmed from the pharmacy claims. Only direct medical costs were assessed.
Conclusions:
Pattern of use was very dynamic, suggesting seizures are not well-controlled. Improving seizure control and reducing economic burden of refractory epilepsy remain important unmet medical needs in this population.
Introduction
Epilepsy is a neurological disorder affecting ∼2 million Americans and 50 million people worldwideCitation1,Citation2. It was estimated that the annual cost of prevalent cases in the US was $12.5 billion in 1995, with indirect costs accounting for 85% of the total costCitation3. A more recent review suggested an estimated total cost of epilepsy of €15.5 billion in Europe in 2004, with indirect costs being the most dominant cost category (55.5%)Citation4. Close to 60% of patients with epilepsy have partial onset seizures (POS)Citation5.
Anti-epileptic drugs (AEDs) are the most common therapeutic intervention to prevent recurrent seizures. Although AEDs are highly effective when taken regularly, ∼30% of patients still have inadequate seizure controlCitation6,Citation7. Patients are considered to have refractory epilepsy when there is inadequate control of seizures, despite being adherent to AEDs for 1–2 yearsCitation8. Refractory epilepsy is clinically defined based on the number of AEDs previously taken, frequency of seizures, and duration of non-controlled epilepsyCitation8. Uncontrolled seizures are associated with a lower quality-of-life as well as higher morbidity and mortalityCitation9–11. The annual total cost incurred by prevalent refractory epilepsy patients was estimated to be close to $4 billion in the US, with indirect costs accounting for two-thirds of total costCitation12.
There is abundant literature examining the association between healthcare costs and epilepsy. Several published studies reported total healthcare costs and costs associated with managing epilepsy for epileptic patients in the USCitation3,Citation13–15. One study focused specifically on estimating the direct and indirect costs associated with POSCitation16, and two other studies conducted economic evaluations on POS patients who failed their initial treatmentCitation17,Citation18. One study conducted a decade ago reported the direct and indirect costs associated with refractory epilepsyCitation12. However, information on the incremental costs between refractory patients with POS and non-refractory patients is limited. In addition, even though there have been several retrospective studies that used real-world data to examine AED treatment patternsCitation19,Citation20, resource utilization in refractory patients has yet to be evaluated extensively.
The objectives of this study were to assess the economic burden in direct healthcare utilization and costs for refractory epileptic patients with POS and assess the AED treatment patterns among these patients. Findings from this study about treatment patterns, resource utilization, and healthcare costs using real-world data would be useful in bridging the gap in currently published literature.
Methods
Data source and sample selection
Thomson Medstat MarketScan Commercial Insurance Database with administrative claims dated between January 1, 2004 and December 31, 2008 were used to conduct the analysis. This database includes ∼30 million commercially insured individuals (i.e. working age adults and their dependents) from ∼100 US payers. This database is built for research purposes from the administrative claims of these payers, which has been widely used for health economics, epidemiology, and health services research and is geographically diverse and representative of the US commercially-insured population. The retrospective billing records of medical services and prescriptions covered and reimbursed by the payers were de-identified and can be tracked longitudinally via encrypted enrollee identifiers to assess the patterns of healthcare utilization. The medical service claims record detailed information for inpatient and outpatient healthcare encounters, including date and place of service, provider type, plan- and patient-paid amounts, International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes, and CPT-4 procedure codes. Pharmacy claims include information on dispensed medications including National Drug Code (NDC), dispense date, quantity, days supplied, and plan- and patient-paid amounts. The enrollment file contains information on age, gender, US census region, health insurance payer type, and monthly enrollment status. These files are linkable based on an encrypted patient identification number.
Prevalent patients with POS aged less than 65 years were first selected if they had any medical claim with the associated diagnosis (ICD-9-CM diagnosis codes: 345.4, 345.5). We chose to focus on localization-related epilepsies with partial seizures because we would like to define the unmet needs in this specific target population and the results of this analysis could be used as inputs to economic models for treatment interventions targeting this population. ICD-9-CM codes were used since that was still the coding scheme used in the US in the period that this study examined. Unlike the ICD-10-CM system where specific codes for those known to cause symptomatic epilepsy are available, the ICD-9-CM system does not have those codes separately. Hence, using the codes of 345.4 and 345.5 should be sufficient to identify the patients and would not lead to under-estimation of healthcare costs and utilization. In the past investigational studies, an operational definition of the absence of response to two AEDs tolerated at reasonable doses was used to define refractorinessCitation8. Since we were not able to identify onset of seizures in administrative claims, we defined refractoriness based on having three lifetime AEDs observed in the claims data. The AEDs considered in the study were levetiracetam, felbamate, clobazam, clonazepam, diazepam, midazolam, acetazolamide, gapabentin, phenobarbital, primidone, pregabalin, topiramate, zonisamide, vigabatrin, tiagabine, carbamazepine, eslicarbazepine, fosphenytoin, lamotrigine, oxcarbazepine, phenytoin, rufinamide, and valproic acid. Vagus nerve simulation (VNS) was counted as one AED. Once POS patients received their third AED, they were classified into the refractory cohort for that calendar year and the years afterward. The non-refractory cohort consists of patients who were never or had not yet been classified as refractory during the study period.
Economic burden analysis
Analysis was conducted to compare economic burden between refractory and non-refractory cohorts by each calendar year. Patients were included in the comparison for a particular calendar year only if they were continuously enrolled in the health plan for the entire year. Patients could be included in multiple years and on different cohorts (refractory and non-refractory) depending on when they reached the refractory status. We reported baseline demographic characteristics for the study population including age, gender, region, co-morbid conditions such as depression, anxiety, migraine, multiple sclerosis, fracture, dislocation, sprains and strains, open wounds, burns, and Charlson comorbidity index (CCI) in the first continuously enrolled yearCitation21. Healthcare resource utilization measures including inpatient admission, emergency room (ER) visits, head computed tomography (CT), and head magnetic resonance imaging (MRI) were compared by each calendar year. All-cause and POS-related (medical services with POS diagnosis and costs for AED prescriptions) healthcare costs by setting (total, inpatient, outpatient, pharmacy) were examined. All costs estimated were adjusted to 2008 dollars based on the consumer price index for medical careCitation22. Descriptive analyses performed included Chi-square test for categorical variables and non-parametric Wilcoxon rank-sum tests for mean age, CCI, and cost variables.
Treatment pattern analysis
AED treatment patterns were evaluated using pharmacy refill records among patients with refractory epilepsy with POS from the first observed AED. Continuous enrollment in the health plan was not required because this was not a comparison analysis. We classified pattern of use for the first observed AED dispensed as monotherapy, combination therapy, or triple/quadruple therapies. Within each therapy group, we assessed their subsequent patterns of use. We defined therapy add-on as the addition of another AED to the initial AED with at least a 30-day overlap in medication supply between the dispensing of these two AEDs. We defined a switch as discontinuing an existing medication and initiating a new medication. We considered it a switch in therapy if patients discontinued their initial AED and started another AED with less than a 30-day overlap in medication supply between dispensing of the two AEDs. We defined it as a partial switch when patients discontinued one of the combination AEDs and started another AED as a replacement. Lastly, we referred to it as a complete switch when patients discontinued their original combination regimen entirely and started a new combination therapy. AED utilization patterns were presented sequentially with the number and proportion of patients of those patterns of use. We also reported the most commonly used AEDs for: (1) first observed monotherapy; (2) first observed combination therapy; (3) add-on AED to a monotherapy; and (4) the AED from which a monotherapy was switched to.
Results
Baseline characteristics
This study included 79,149 patients with POS with continuous enrollment for at least one calendar year between 2004–2008, and 8714 (11%) patients were classified as refractory at some point in time. shows the demographic characteristics and comorbidities based on their first continuously enrolled calendar year of the refractoriness status. The mean age for the study population was 33 years old, and close to one-third of patients were children or adolescents. The refractory cohort had a higher proportion of females (58.3% vs 54.3%, p < 0.001). A large number of patients (44%) lived in the South region.
Table 1. Demographic characteristics and comorbidities by refractory status.
Many POS-related co-morbid conditions were more prevalent in the refractory cohort. Some notable differences were mental illnesses such as depression (14.1% vs 9.6%, p < 0.001) and anxiety (6.7% vs 5.0%, p < 0.001), and injuries such as fractures (6.5% vs 4.9%, p < 0.001), sprains and strains (10.0% vs 8.4%, p < 0.001), and open wounds (7.3% vs 5.0%, p < 0.001). The mean CCI was also higher in the refractory cohort (1.0 vs 0.8, p < 0.001).
Healthcare resource utilization and costs
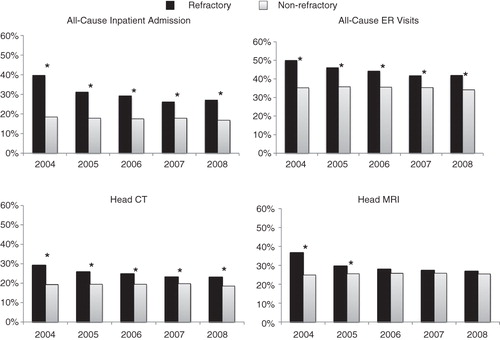
Healthcare utilization by refractory status was presented in for each calendar year. In 2008, a higher proportion of refractory patients had all-cause inpatient admissions (27.2% vs 16.9%, p < 0.001) and all-cause ER visits (42.0% vs 34.3%, p < 0.001) than non-refractory patients. A similar trend was found in prior years examined. We consistently found a higher proportion of patients in the refractory cohort had a head CT scan (22.9% vs 18.6% in 2008, p < 0.001) in these five calendar years. Higher utilization in head MRI for the refractory cohort was observed only in 2004 (36.5% vs 25.0%, p < 0.001) and 2005 (29.5% vs 25.6%, p < 0.001).
In 2008, average annual all-cause healthcare costs for refractory patients were significantly higher than non-refractory patients ($33,613 vs $19,085; p < 0.001) (). We observed a similar trend in costs from inpatient ($11,780 vs $6076; p < 0.001), outpatient ($13,431 vs $8637; p < 0.001), and pharmacy ($8402 vs $4372; p < 0.001) settings. The average annual POS-related healthcare costs were also higher for refractory patients than non-refractory patients ($10,804 vs $4032; p < 0.001), as well as by settings for inpatient ($4621 vs $1384; p < 0.001), outpatient ($904 vs $391; p < 0.001), and pharmacy costs ($5280 vs $2256; p < 0.001). These differences were consistent across all calendar years examined.
Table 2. Annual all-cause and POS-related healthcare costs per patient by refractory status in each calendar year.
AED treatment patterns
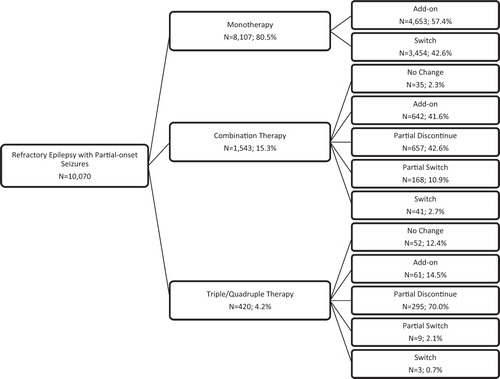
Since continuous enrollment in the health plan was not required in assessing AED treatment patterns, we had more refractory patients (n = 10,070) than in the economic analysis. We examined the AED treatment patterns from the time they entered the cohort, possibly before they reached refractory status. When assessing their first observed AED treatment, we found 80.5% of patients were on monotherapy, 15.3% were on combination therapy, and 4.2% were on triple/quadruple therapy (). Among these refractory patients who were monotherapy users when we first observed them, 57.4% added another AED and 42.6% switched to another AED subsequently. Of the combination therapy users, 41.6% added a third AED, 42.6% discontinued one of the AEDs in combination therapy, 10.9% switched one of the AEDs in combination therapy to another, and 2.7% had the AED combination completely switched. We did not observe subsequent change in AED in 2.3% of these patients because they used VNS instead. Of the few patients who were already on triple/quadruple therapy (n = 420), most of them (70.0%) discontinued one of the existing AEDs.
Figure 2. Anti-epileptic drug treatment patterns among patients with refractory epilepsy with partial onset seizures.
The most frequently prescribed AEDs as the first observed monotherapy in our study population were phenytoin (15.2%), levetiracetam (15.2%), carbamazepine (12.2%), oxcarbazepine (11.3%), and lamotrigine (11.0%) (). Of the refractory patients who were on combination therapy when first selected, the most common combination therapies were levetiracetam with the following AEDs: phenytoin (6.4%), lamotrigine (6.0%), carbamazepine (5.3%), topiramate (4.7%), and oxcarbazepine (4.5%). Among the patients on monotherapy, we found that levetiracetam is the AED that was most commonly added on or switched to (). Of those who were initially on levetiracetam, the most common AEDs added-on or switched-to were lamotrigine, oxcarbazepine, and topiramate.
Figure 3. Most common anti-epileptic monotherapies and combination therapies among patients with refractory epilepsy with partial onset seizures.
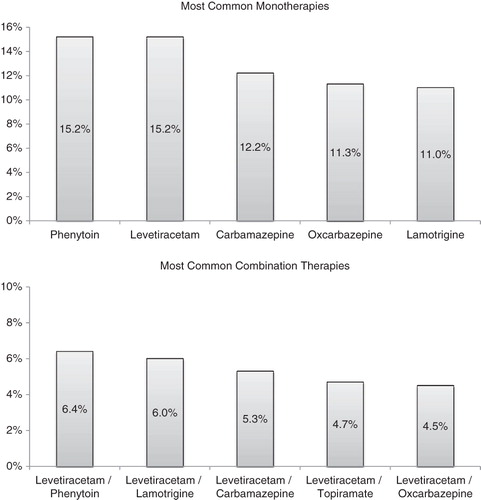
Table 3. Most common therapy add-ons and switches among patients with refractory epilepsy with partial onset seizures.
Discussion
This retrospective database study analyzing administrative claims from a US population reported the treatment patterns among refractory epileptic patients with POS and compared healthcare utilization and costs between patients with POS with and without refractoriness. Findings suggested that patients with refractory epilepsy incurred substantial all-cause healthcare costs, averaging $33,613 per patient in 2008, of which $10,804 was associated with managing POS. The all-cause healthcare costs were 76% more for refractory patients than for non-refractory patients. Although all the individual components of costs were significantly higher in the refractory cohort, the major cost differences were found in inpatient and pharmacy costs, both twice the costs of the non-refractory cohort. Higher inpatient costs might be partially explained by the higher prevalence observed in injuries such as fractures, sprains and strains, and open wounds for refractory patients. Significantly higher costs for prescriptions were anticipated as refractory patients could not achieve satisfactory seizure control by using only one AED.
One-third of the all-cause healthcare costs were POS-related in the refractory cohort, whereas 20% of those were POS-related in the non-refractory cohort. POS-related costs for refractory patients were twice as high as POS-related costs for non-refractory patients. Pharmacy costs accounted for half of the POS-related costs, followed by inpatient and outpatient costs for both refractory and non-refractory patients.
Our findings are consistent with the data for patients with POS reported in the literatureCitation16. The rates of healthcare resource utilization reported in our study for the non-refractory cohort are similar to those in a study assessing patients with POS by Ivanova et al.Citation16 in inpatient stay (16.9% vs 17.4%) and ER visits (34.3% vs 32.7%). Their reported average annual all-cause healthcare cost was $11,276 in 2005 dollars. Our findings also mirror their’s regarding the cost distribution by setting. Both studies found outpatient services account for the highest proportion of total healthcare costs, followed by inpatient admissions and drug costs. Although their study had summarized the healthcare costs of utilization for patients with POS, our study adds to the literature by further assessing the economic burden in direct healthcare costs for the refractory patients.
In this cross-sectional comparison, we found that the differences in costs and utilization between refractory and non-refractory cohorts were greater in 2004 than in the subsequent years. To understand what could have resulted in such differences, we conducted an exploratory analysis. Due to our design, refractory patients included in 2004 spent much shorter time to reach their refractory status (less than 1 year) based on our operational definition of at least three AEDs to determine refractoriness. We hypothesized that patients who reached their refractory status with a shorter period of time incurred more healthcare services and costs because they received the most intensive regimen changes during this period. In this exploratory analysis (data not shown), we found that patients who reached their refractory status in less than 6 months had higher annual healthcare costs than those who were considered refractory in more than 6 months. This finding supported our hypothesis to explain the largest differences in all-cause healthcare costs between refractory and non-refractory patients in 2004 and the significant differences in head MRI use in years 2004 and 2005.
This study also assessed the treatment patterns for refractory patients with POS and found it to be very dynamic. Results showed that levetiracetam, phenytoin, carbamazepine, oxcarbazepine, lamotrigine, and topiramate are the six most common AEDs used in the refractory patients with POS in the study population. Levetiracetam is the most common AED used as an add-on or switch-to medication. It is also the most frequently used AED in combination therapy. To the best of our knowledge, this study is the first to describe AED treatment patterns among refractory patients with POS in great detail using real-world data. Our results provided very useful information on the pattern of AED use before patients were classified as refractory, and could be used in future economic evaluation of cost-effectiveness of AEDs in managing refractory patients.
Several limitations must be noted when interpreting the study results. The definition of refractory epilepsy with POS can only be operationally defined based on utilization of three or more AEDs because onset of seizure cannot be identified based on claims data. In addition, we could not determine whether an AED was discontinued due to lack of effectiveness, adverse events, tolerability, or patient compliance. Similarly, the diagnosis of POS from the administrative claims could not be validated without access to medical charts and laboratory or other diagnostic report results. In this study, we selected prevalent patients with POS. It is possible that patients might have received other AEDs prior to the time they entered into this database. This might lead to misclassification of refractory patients as non-refractory which could result in under-estimation of the economic burden we observed. Although all selected patients had a diagnosis of POS, the indication of each AED could not be confirmed from the pharmacy claims. The administrative claims data did not provide us with sufficient information to unfold reasons for the observed dynamic treatment patterns. In addition, treatment patterns were built upon observations of the pharmacy refill records without ascertainment of prescribing data from the medical charts. We were able to assess only direct healthcare costs but not indirect costs such as loss in productivity or intangible costs. Although our study used a combined private insurance payer and patient perspective, only medical services and medications reimbursed by the health plan were captured in the claims database. This did not take into account services or medications paid completely by patient out-of-pocket or by other payers. Hence, our findings might not be generalizable to populations covered by other types of insurance such as Medicaid and Medicare, or healthcare systems outside of the US.
Conclusion
Findings from this study suggest refractoriness in epilepsy patients with POS is associated with high economic burden from the health insurer’s perspective and dynamic treatment patterns. Improving seizure control and reducing the economic burden of refractory epilepsy remain important unmet medical needs in this population.
Transparency
Declaration of funding
The study was funded by Novartis Pharmaceutical Corporation.
Declaration of financial/other relationships
SC, LB, and NW are employees of United BioSource Corporation, a consulting company that has received research grants from Novartis Pharmaceutical Corporation. PS is an employee of Novartis Pharmaceutical Corporation and is a shareholder of Novartis Pharmaceutical Corporation.
Acknowledgments
No assistance in the preparation of this article is to be declared.
References
- Devonshire IM, Papadakis NG, Port M, et al. Neurovascular coupling is brain region-dependent. Neuroimage 2012;59:1997-2006
- Devonshire V, Lapierre Y, Macdonell R, et al. The Global Adherence Project (GAP): a multicenter observational study on adherence to disease-modifying therapies in patients with relapsing-remitting multiple sclerosis. Eur J Neurol 2011;18:69-77
- Begley CE, Famulari M, Annegers JF, et al. The cost of epilepsy in the United States: an estimate from population-based clinical and survey data. Epilepsia 2000;41:342-51
- Pugliatti M, Beghi E, Forsgren L, et al. Estimating the cost of epilepsy in Europe: a review with economic modeling. Epilepsia 2007;48:2224-33
- Semah F, Picot MC, Adam C, et al. Is the underlying cause of epilepsy a major prognostic factor for recurrence? Neurology 1998;51:1256-62
- Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Eng J Med 2000;342:314-9
- Kwan P, Brodie MJ. Epilepsy after the first drug fails: substitution or add-on? Seizure 2000;9:464-8
- Kwan P, Arzimanoglou A, Berg AT, et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 2010;51:1069-77
- Cramer JA. Quality of life for people with epilepsy. Neurol Clin 1994;12:1-13
- Nei M, Bagla R. Seizure-related injury and death. Curr Neurol Neurosci Rep 2007;7:335-41
- Nilsson L, Ahlbom A, Farahmand BY, et al. Risk factors for suicide in epilepsy: a case control study. Epilepsia 2002;43:644-51
- Murray MI, Halpern MT, Leppik IE. Cost of refractory epilepsy in adults in the USA. Epilepsy Res 1996;23:139-48
- Yoon D, Frick KD, Carr DA, et al. Economic impact of epilepsy in the United States. Epilepsia 2009;50:2186-91
- Ivanova JI, Birnbaum HG, Kidolezi Y, et al. Economic burden of epilepsy among the privately insured in the US. Pharmacoeconomics 2010;28:675-85.
- Kurth T, Lewis BE, Walker AM. Health care resource utilization in patients with active epilepsy. Epilepsia 2010;51:874-82
- Ivanova JI, Birnbaum HG, Kidolezi Y, et al. Direct and indirect costs associated with epileptic partial onset seizures among the privately insured in the United States. Epilepsia 2010;51:838-44
- Lee WC, Arcona S, Thomas SK, et al. Effect of comorbidities on medical care use and cost among refractory patients with partial seizure disorder. Epilepsy Behav 2005;7:123-6
- Lee WC, Hoffmann MS, Arcona S, et al. A cost comparison of alternative regimens for treatment-refractory partial seizure disorder: an econometric analysis. Clin Ther 2005;27:1629-38
- Davis KL, Candrilli SD, Edin HM. Prevalence and cost of nonadherence with antiepileptic drugs in an adult managed care population. Epilepsia 2008;49:446-54
- Ettinger AB, Manjunath R, Candrilli SD, et al. Prevalence and cost of nonadherence to antiepileptic drugs in elderly patients with epilepsy. Epilepsy Behav 2009;14:324-9
- Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245-51
- Ross AP. Tolerability, adherence, and patient outcomes. Neurology 2008;71:S21-3