Abstract
Objectives:
To assess factors associated with adherence to phosphodiesterase type 5 inhibitors (PDE5Is) in the management of pulmonary arterial hypertension (PAH).
Methods:
This study analyzed pharmacy benefit claims of naïve Adcirca and Revatio users between January 1, 2008 and December 31, 2010. Patients were considered adherent if their proportion of days covered (PDC) was ≥ 80% over a 6-month period. Logistic regressions were estimated to assess the factors associated with adherence. Analyses were stratified by use of a specialty pharmacy or retail pharmacy. A sensitivity analysis was performed by excluding individuals with 90-day supply.
Results:
Of the total of 2143 patients included, 46.8% were adherent. Adherence was higher among 930 specialty pharmacy users (65.6%) than 1213 retail pharmacy users (32.3%, p < 0.001). Adherence was higher among Adcirca users (60.7%; approved dose 40 mg once-daily) than Revatio users (44.3%, p < 0.001; approved dose 20 mg thrice-daily). Among retail pharmacy users, adherence was higher in patients using Adcirca (OR = 2.59; 95% CI = 1.60–4.22) and patients with an index prescription given by pulmonologists (OR = 1.70; 95% CI = 1.15–2.50), while lower in patients with higher copayment ($51–$250: OR = 0.61, 95% CI = 0.42–0.90; $251+: OR = 0.57, 95% CI = 0.39–0.83). Among specialty pharmacy users, only high copayment ($251+: OR = 0.56, 95% CI = 0.35–0.90) was found to be a significant factor for non-adherence. After excluding individuals with 90-day supply, adherence rate was 29.6% in retail pharmacy and 57.9% in specialty pharmacy (p < 0.001), and regression results were similar.
Limitations:
Diagnosis of PAH was not confirmed without access to medical claims. Pharmacy refill records might not reflect actual consumption. Adherence evaluated for 6 months might not be generalizable to longer periods.
Conclusion:
Adherence to PDE5Is for PAH is sub-optimal. The findings suggest that adherence to PDE5Is in patients with PAH is associated with the use of specialty pharmacy, simpler dosing frequency, a lower financial barrier, and a prescription given by pulmonologists.
Introduction
Pulmonary arterial hypertension (PAH) is a rare disease characterized by an elevation of pulmonary artery pressure and pulmonary vascular resistance resulting from vasoconstriction of small-to-medium sized pulmonary arteries, as well as progressive fibrotic and proliferative changesCitation1. Common symptoms of the disease include shortness of breath, chest tightness and pain, fatigue, and limited exercise tolerance which can often be attributed to various other conditions, making it challenging to diagnose PAH at an early stageCitation2. Although PAH is a rare disease with only 2.4 new cases per million people per yearCitation3, delays in diagnosis and referral to expert centers mean that patients often are already progressing toward right heart failure and death by the time PAH-specific treatment is institutedCitation4. Prior to the development of approved treatments for PAH, patients were expected to live on average less than 3 years after diagnosisCitation5. However, due to the increase in disease awareness and new medicines approved for PAH, studies indicate improved overall survival as compared to the ‘pre-treatment era’Citation6,Citation7.
With the exception of lung transplants where possible, there is no known cure for PAH; however, a proliferation of treatment options has improved the outlook for patients suffering from this condition. Management of PAH is targeted at improving symptoms, exercise tolerance, long-term outcomes, and quality-of-lifeCitation8,Citation9. Pharmacologic therapies for PAH generally include three classes of medication: phosphodiesterase type 5 inhibitors (PDE5Is), endothelin receptor antagonists (ERAs), and prostacyclin analogsCitation10,Citation11. The choice of drug depends on a variety of factors. Oral administration has the advantage of avoiding some complications associated with parenteral therapies (e.g., central venous catheter-related sepsis or thrombosis associated with intravenous infusion and pain associated with subcutaneous infusion) and intermittent inhaled therapies (e.g., faulty administration technique, inconsistent dose timing)Citation11. PDE5Is and ERAs are both available for oral administration, but PDE5Is are the most frequently used due to their improved safety profile vs ERAs and lower wholesale cost for 1 year of treatmentCitation11,Citation12. The prognosis of patients with PAH has improved in the past decade with the development of these treatmentsCitation5,Citation13, although it remains unsatisfactory.
Medication use is a daily commitment, especially with diseases in which the symptoms may not be noticeable on a daily basis. Past research has stressed the importance and challenge of adherence to medication for chronic diseases in the real-world settingCitation14. Currently, limited data are available regarding adherence to PDE5Is for the management of PAH in clinical practice. The objectives of this study were to examine adherence to PDE5Is for management of PAH and to identify potential factors associated with better adherence to PDE5Is. Published literature suggests that patients with chronic diseases are more adherent to once-daily than twice-daily or thrice-daily treatment regimensCitation14–16. We attempted to confirm this finding in PAH by examining if patients treated with Adcirca (indicated to be taken once-daily) are more likely to be adherent than patients treated with Revatio (indicated to be taken 3-times daily)Citation17,Citation18.
PAH medication frequently is delivered via a specialty pharmacy services channel, given the rarity of the disease and the historical complexity of treatment (intravenous infusion, subcutaneous infusion, inhalation) and associated therapy costsCitation19. In addition to its implication on the benefit design from plan perspectives, use of a specialty pharmacy may also influence patient adherence and outcomes through education programs, co-ordinated care and closer follow-up, or disease management; however, there is a lack of published studies to demonstrate these influencesCitation20. Therefore, we evaluated if the use of specialty pharmacy had an impact on medication adherence rates for PAH patients.
Methods
Data source
This study utilized pharmacy claims dated between January 1, 2008 and December 31, 2010 from Medco Health Solutions, Inc. Medco is one of the largest pharmacy benefit management companies in the US, with over 60 million covered individuals and pharmacy claims data for one-in-five Americans. Pharmacy claims contain information about National Drug Codes (NDC), medication name, co-payment amounts, fill dates, quantity dispensed, days of supply, strength, and prescribing physician type. Refill history can be tracked by encrypted unique identifiers. Patient demographic characteristics are also available including birth year, gender, and region of residence.
Sample selection
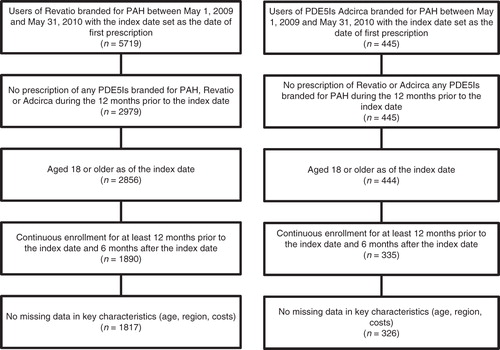
Patients were first selected if they had pharmacy claims of Adcirca or Revatio, based on NDC numbers, between May 1, 2009 and May 31, 2010. Since we did not have the medical claims to confirm the diagnosis of PAH, we only selected the FDA-approved PAH-indicated brands of PDE5Is (i.e., Adcirca and Revatio)Citation17,Citation18. The date of the first prescription identified during this period was denoted as the index date. To select naïve users, we excluded patients who had any prescription of Adcirca or Revatio during the 12 months prior to the index date. Additional inclusion criteria were being 18 years or older as of the index date, having continuous enrollment in the insurance plan during the 12 months prior to and 6 months following the index date, and without missing data in any key characteristics (i.e., age, region, costs).
The final selected patients were stratified into two cohorts based on whether they had any PDE5Is during the 6-month follow-up period from a specialty pharmacy. Within specialty pharmacy and retail pharmacy cohorts, patients were further categorized into two cohorts based on adherence. Adherence to the initiated therapies (Adcirca or Revatio) was measured by the proportion of days covered (PDC), which is calculated as the number of days with medication available over the 6 months following the index date divided by 180 daysCitation21. Patients were considered as adherent if the PDC was greater than or equal to 80%. For patients who switched from one PDE5I to another, only the first PDE5I was considered, as we were interested in the impact of dosing frequency on adherence.
Study measures
Patient demographic characteristics were assessed on the index date including age, gender, and geographic region. From the pharmacy claims, we also assessed characteristics of the index prescription including index medication (Adcirca or Revatio), co-payment amount standardized to a 30-day supply (i.e., co-payment for a 90-day supply was divided by 3), and specialty of prescribing physician based on the specialty coded on the index prescription (i.e., pulmonologist, cardiologist, primary care provider, rheumatologist, other specialist, or unknown). We examined whether patients had any prescription of index PDE5I with 90-day supply or more. We also examined index prescription characteristics. Average daily dose and mean daily consumption (number of pills) were estimated over 6 months for Adcirca and Revatio, respectively. In addition, we estimated RxRisk score, a risk adjustment algorithm to predict healthcare costs based on automated pharmacy claims developed by Fishman et al.Citation22 We categorized patients into four levels based on quartiles (RxRisk level 1–4) of the score, with the lowest quartile representing the lowest predicted costs.
Statistical analysis
Descriptive analyses were used to compare the study measures between adherent and non-adherent users. Tests used include the Student’s t-test for continuous variables and the Chi-square test for categorical variables. Logistic regressions were run to assess the factors associated with adherence including index PDE5Is medication (Adcirca vs Revatio), age, gender, specialty of prescriber, and average 30-day co-payment of the index prescription. Since patients who filled a prescription with a 90-day supply would have their 6-month follow-up covered with relatively fewer prescriptions, we controlled for the possession of such prescriptions in our regression model. To further test whether our findings were robust, we conducted a sensitivity analysis by excluding patients who possessed a prescription with more than a 90-day supply. Since we did not have medical claims to ascertain PAH diagnosis, we also conducted another sensitivity analysis by excluding any patients who filled Viagra or Cialis. All analyses were performed separately for specialty and retail pharmacy users.
The review from Institutional Review Broad was exempted since the data were encrypted and in compliance to the Health Insurance Portability and Accountability Act requirements.
Results
The study included 2143 PDE5Is users (326 Adcirca users and 1817 Revatio users) meeting the selection criteria (). In the study population, 930 had their PDE5Is filled at a specialty pharmacy and 1212 filled at a retail pharmacy (). A higher proportion of patients with their prescription dispensed through specialty pharmacy were adherent (65.6%) than those through retail pharmacy (32.3%) (p < 0.001). The study population had a mean age of ∼ 65 years old, and ∼ 65% were female. The majority of patients were from the South region (40%). While demographic characteristics were similar between adherent and non-adherent cohorts, a higher proportion of adherent patients possessed a 90-day or greater supply of medication. RxRisk score distribution was similar between cohorts.
Table 1. Baseline demographic characteristics by adherence and use of specialty pharmacy.
Adherence to and characteristics of PDE5I
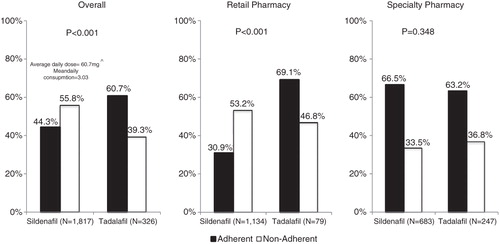
Overall, a higher proportion of patients receiving Adcirca were adherent than those receiving Revatio (60.7% vs 44.3%, p < 0.001) (). For Adcirca users, the average daily dose over the 6-month follow-up period was 37.9 mg and the mean daily consumption was 1.89 tablets per day. The average daily dose for Revatio users was 60.7 mg, with a mean daily consumption of 3.03 tablets per day. Among retail pharmacy users, the rate of adherence was higher for Adcirca users than Revatio users (69.1% vs 30.9%, p < 0.001). Among specialty pharmacy users, on the other hand, the rates of adherence were similar between the two groups (66.5% vs 63.2%, p = 0.348).
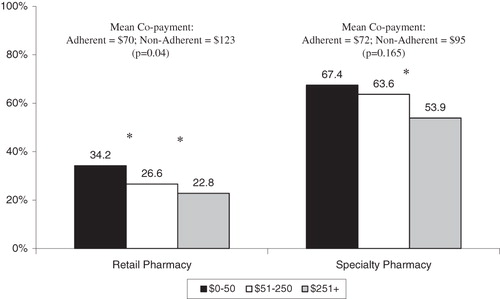
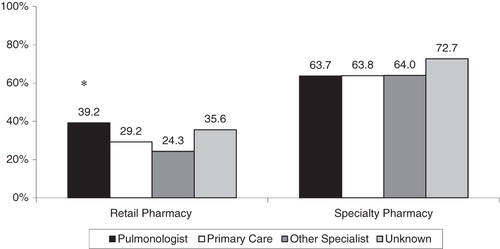
We observed a higher mean co-payment amount for non-adherent patients ($136.7 vs $103.7, p = 0.04) among retail pharmacy users, although it was not statistically different among specialty pharmacy users ($94.9 vs $78.3, p = 0.165) (). When comparing the rate of high adherence between patients paying different levels of out-of-pocket co-payment, we found a significantly lower rate in the higher co-payment group (34.2% vs 26.6% vs 22.8% for $0–$50, $51–$250, and $251+, respectively; all p < 0.05) among retail pharmacy users, and a lower rate on the $251+ group compared with the $0–$50 group (53.9% vs 67.4%; p < 0.05) among specialty pharmacy users. Of the known prescriber specialists, we found the adherence rate to be higher among patients who had their prescription from a pulmonologist compared with those from a primary care provider (39.2% vs 29.2%) among retail pharmacy users, and we did not observe any differences in adherence rates by prescriber specialty among specialty pharmacy users ().
Factors associated with adherence
The regression model among retail pharmacy users showed several factors associated with adherence to the drugs studied (). Patients receiving Adcirca were more likely to be adherent than Revatio users (odds ratio [OR] = 2.59, 95% CI = 1.60–4.22). Compared with patients receiving their prescription from primary care providers, those having their prescription from a pulmonologist had an increased likelihood of being adherent (OR = 1.70; 95% CI = 1.15–2.50). Patients with a higher 30-day co-payment on their initial payment were less likely to be adherent ($51–$250: OR = 0.61, 95% CI = 0.42–0.90; $251+: OR = 0.57, 95% CI = 0.39–0.83; reference group: ≤ $50). Patients who had possession of a prescription with a 90-day or greater supply were also more likely to be adherent (OR = 5.81, 95% CI = 3.39–9.95). Among specialty pharmacy users, only co-payment ($250+: OR = 0.56, 95% CI = 0.35–0.90; reference group ≤ $50), possession of a prescription with a 90-day or greater supply (OR = 1.75, 95% CI = 1.32–2.33), and being in the highest quartile of RxRisk score (OR = 0.66; 95% CI = 0.44–0.99) were significant factors. In the sensitivity analysis, 898 patients who had possession of a prescription with a 90-day or greater supply were excluded. The overall adherence rate decreased from 32.3% to 29.6% in retail pharmacy and from 65.6% to 57.9% in specialty pharmacy (). However, the adherence rate was significantly higher in specialty pharmacy than retail pharmacy both before and after this exclusion. The findings from regression analyses were similar. The sensitivity analysis excluding users of Viagra or Cialis (n = 78; 3.64%) also yielded similar results (data not shown).
Table 2. Primary and sensitivity analyses to assess factors associated with adherence to PAH treatment by use of specialty pharmacy.
Discussion
Non-adherence to medication is one of the issues that many practitioners are facing in actual practiceCitation23,Citation24. Adherence to medication plays an important role, especially for maintenance medications in chronic illnessesCitation16. To our knowledge, no published studies have examined the issue of adherence for patients suffering from PAH. This study analyzed a large pharmacy database to understand the adherence to two specific PDE5Is and associated factors in the treatment of PAH in the real-world setting. During the 6 months after treatment initiation, we found that, overall, only half of the patients were adherent to their medication based on prescription refill records. Our study is the first to show that, like other chronic diseases, adherence to two PDE5Is indicated for PAH is poor in actual practice. Future research is needed to understand barriers that PAH patients face in order to design interventions to improve their adherence.
With these two PDE5Is being commonly distributed through specialty pharmacy for PAH, we also assessed patient adherence between users of specialty and retail pharmacy. We found that specialty pharmacy users were more likely to be adherent to their PDE5Is. This is consistent with a prior study which found greater refill adherence to adalimumab, a tumor necrosis factor antagonist injection, among specialty pharmacy usersCitation25. However, we could not assess what the unique features of specialty pharmacy are that differ from retail pharmacy, leading to this difference in patient adherence.
Our results suggest several factors associated with adherence among retail pharmacy users. First, users of Adcirca, which has a simpler frequency of administration than Revatio, had better adherence rates. This is consistent with past studies investigating this question in other chronic conditionsCitation14–16. Our findings are similar to what has been reported in the literature that the average adherence rate of a once-daily regimen was close to 75%, while the adherence rate of 4-times a day was ∼ 45%Citation26,Citation27, and a range of 22–41% more adherent days was reported for the patients receiving the once-daily than the thrice-daily regimenCitation16.
Among retail pharmacy users, we also found that receiving a prescription from a pulmonologist, compared with a primary care provider, was associated with a higher likelihood of adherence. However, what characteristics associated with prescriber specialty, whether it is the pulmonology specialty or being managed in PAH centric medical practices, could not be determined from our data source and, while intriguing, remains to be confirmed. The association observed from this retrospective study could be helpful to generate a hypothesis about care from PAH centric medical practices for a future prospective study to better understand the influence of care setting on treatment adherence. Findings from some studies have suggested patient out-of-pocket co-payment is associated with adherence in several chronic diseasesCitation28–32, and our findings broaden the previous observations to include PAH patients who demonstrated poor adherence associated with a higher co-payment. Our findings further extend limited published data on the assessment of out-of-pocket cost share on adherence to high-cost specialty pharmacy medicationsCitation33.
Interestingly, many of these factors that we found were associated with adherence among retail pharmacy users were not significant among specialty pharmacy users. Only high co-payment remained significant. It is possible that, since the distinguishing features of specialty pharmacy users are accounted for in the stratified analysis demonstrating a higher adherence than retail pharmacy users, other factors became less influential when patients already have a high level of adherence.
As anticipated, possession of prescriptions with a 90-day or greater supply was associated with high adherence (from an analytical perspective based on how PDC was derived). To confirm that our findings were robust, we excluded the patients with such prescriptions and performed a sensitivity analysis, and found that our results were consistent. Performing this sensitivity analysis to address this potential methodological limitation strengthened our study findings. Future studies using a combination of pharmacy and medical claims should aim to assess whether better adherence to a prescribed treatment is associated with improved long-term outcomes and reduced healthcare utilization for PAH patients.
Several limitations must be noted when interpreting the results of this study. First, this study only used pharmacy claims without access to the medical claims. The diagnosis of PAH was not confirmed via medical claims or chart records. Although we identified patients who used the branded products indicated for PAH, it is possible that we inadvertently included in this analysis patients who used these two drugs for reasons other than PAH. Second, pharmacy refill records might not reflect actual consumption. Third, at the time of this analysis being conducted, the available data only allowed adherence to be evaluated for 6 months and might not be generalizable to longer periods. For example, using up to 3 years of data available, we found the mean daily consumption for Revatio was 3.30 tablets per day. A shorter evaluation time frame here could not capture the dose escalation that occurred after patients were on a treatment for extended periods. Future studies should attempt to confirm the findings using a longer evaluation period. Also, other unknown confounders may exist which could result in biased estimates. Due to the retrospective design of this study, the findings can only be interpreted as associative rather than causative.
Conclusions
In clinical practice, overall adherence to two PDE5Is indicated for PAH is sub-optimal. Our findings suggest that the use of a specialty pharmacy, a simpler frequency of administration, a lower co-payment, and having a prescription prescribed by certain physician types were associated with better adherence to the two PDE5Is. These factors could be considered when designing interventions to improve the quality-of-care for patients with PAH. Future research should aim at understanding the impact of adherence on clinical and economic outcomes.
Transparency
Declaration of funding
This study was funded by United Therapeutics Corporation.
Declaration of financial/other relationships
GG and JW are employed by United Therapeutics Corporation (whose wholly owned subsidiary, Lung LLC, markets Adcirca in the US). SC and LB are employees of United BioSource Corporation, an independent health outcomes research firm contracted by United Therapeutics Corporation to conduct this analysis. AW serves as a consultant for United Therapeutics Corporation.
Acknowledgments
The authors would like to extend sincere thanks to Prakash Sista and Folger Tuggle from United Therapeutics Corporation for their valuable assistance in formulating this study as well as preparation of the manuscript.
References
- Badesch DB, Champion HC, Sanchez MA, et al. Diagnosis and assessment of pulmonary arterial hypertension. J Am Coll Cardiol 2009;54(1 Suppl):S55-66
- Stringham R, Shah NR. Pulmonary arterial hypertension: an update on diagnosis and treatment. Am Fam Physician 2010;82:370-7
- Humbert M, Sitbon O, Chaouat A, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med 2006;173:1023-30
- Barst RJ. Pulmonary hypertension: past, present and future. Ann Thorac Med 2008;3:1-4
- D’Alonzo GE, Barst RJ, Ayres SM, et al. Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med 1991;115:343-9
- Humbert M, Sitbon O, Chaouat A, et al. Survival in patients with idiopathic, familial, and anorexigen-associated pulmonary arterial hypertension in the modern management era. Circulation 2010;122:156-63
- Benza RL, Miller DP, Gomberg-Maitland M, et al. Predicting survival in pulmonary arterial hypertension: insights from the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL). Circulation 2010;122:164-72
- McLaughlin VV, Archer SL, Badesch DB, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association developed in collaboration with the American College of Chest Physicians; American Thoracic Society, Inc.; and the Pulmonary Hypertension Association. J Am Coll Cardiol 2009;53:1573-619
- Badesch DB, Abman SH, Simonneau G, et al. Medical therapy for pulmonary arterial hypertension: updated ACCP evidence-based clinical practice guidelines. Chest 2007;131:1917-28
- Barst RJ, Gibbs JS, Ghofrani HA, et al. Updated evidence-based treatment algorithm in pulmonary arterial hypertension. J Am Coll Cardiol 2009;54(1 Suppl):S78-84
- Houtchens J, Martin D, Klinger JR. Diagnosis and management of pulmonary arterial hypertension. Pulm Med 2011;2011:845-864
- Archer SL, Michelakis ED. Phosphodiesterase type 5 inhibitors for pulmonary arterial hypertension. N Eng J Med 2009;361:1864-71
- Thenappan T, Shah SJ, Rich S, et al. A USA-based registry for pulmonary arterial hypertension: 1982–2006. Eur Respir J 2007;30:1103-10
- Frishman WH. Importance of medication adherence in cardiovascular disease and the value of once-daily treatment regimens. Cardiol Rev 2007;15:257-63
- Ingersoll KS, Cohen J. The impact of medication regimen factors on adherence to chronic treatment: A review of literature. J Behav Med 2008;31:213-24
- Saini SD, Schoenfeld P, Kaulback K, et al. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care 2009;15:e22-33
- Adcirca®. Once-daily Adcirca (tadalafil) tablets for the treatment of PAH. Indianapolis, IN: United Therapeutics Corporation, 2010. www.adcirca.com. Accessed January 31, 2012
- Revatio®. Revatio Start with Confidence. New York City: Pfizer Inc, 2009. www.revatio.com. Accessed January 31, 2012
- McDonald RC. Managing the intersection of medical and pharmacy benefits. J Manag Care Pharm 2008;14(4 Suppl):S7-11
- Stern D, Reissman D. Specialty pharmacy cost management strategies of private health care payers. J Manag Care Pharm 2006;12:736-44
- Andrade SE, Kahler KH, Frech F, et al. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Safety 2006;15:565-74
- Fishman PA, Goodman MJ, Hornbrook MC, et al. Risk adjustment using automated ambulatory pharmacy data: the RxRisk model. Med Care 2003;41:84-99
- Cramer JA. Effect of partial compliance on cardiovascular medication effectiveness. Heart 2002;88:203-6
- O'Brien MK, Petrie K, Raeburn J. Adherence to medication regimens: updating a complex medical issue. Med Care Rev 1992;49:435-54
- Liu Y, Yang M, Chao J, et al. Greater refill adherence to adalimumab therapy for patients using specialty versus retail pharmacies. Adv Ther 2010;27:523-32
- Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther 2001;23:1296-310
- Iskedjian M, Einarson TR, MacKeigan LD, et al. Relationship between daily dose frequency and adherence to antihypertensive pharmacotherapy: evidence from a meta-analysis. Clin Ther 2002;24:302-16
- Cole JA, Norman H, Weatherby LB, et al. Drug copayment and adherence in chronic heart failure: effect on cost and outcomes. Pharmacotherapy 2006;26:1157-64
- Gibson TB, Mark TL, McGuigan KA, et al. The effects of prescription drug copayments on statin adherence. Am J Manag Care 2006;12:509-17
- Kessler RC, Cantrell CR, Berglund P, et al. The effects of copayments on medication adherence during the first two years of prescription drug treatment. J Occup Environ Med 2007;49:597-609
- Philipson TJ, Mozaffari E, Maclean JR. Pharmacy cost sharing, antiplatelet therapy utilization, and health outcomes for patients with acute coronary syndrome. Am J Manag Care 2010;16:290-7
- Taira DA, Wong KS, Frech-Tamas F, et al. Copayment level and compliance with antihypertensive medication: analysis and policy implications for managed care. Am J Manag Care 2006;12:678-83
- Gleason PP, Starner CI, Gunderson BW, et al. Association of prescription abandonment with cost share for high-cost specialty pharmacy medications. J Manag Care Pharm 2009;15:648-58