Abstract
Purpose:
Hypoglycemia is a frequent side effect induced by insulin treatment of type 1 (T1DM) and type 2 diabetes (T2DM). Limited data exist on the associated healthcare resource use and patient impact of hypoglycemia, particularly at a country-specific level. This study investigated the effects of self-reported non-severe hypoglycemic events (NSHE) on use of healthcare resources and patient wellbeing.
Methods:
Patients with T1DM or insulin-treated T2DM diabetes from seven European countries were invited to complete four weekly questionnaires. Data were collected on patient demographics, NSHE occurrence in the last 7 days, hypoglycemia-related resource use, and patient impact. NSHE were defined as events with hypoglycemia symptoms, with or without blood glucose measurement, or low blood glucose measurement without symptoms, which the patient could manage without third-party assistance.
Results:
Three thousand, nine hundred and fifty-nine respondents completed at least one wave of the survey, with 57% completing all four questionnaires; 3827 respondents were used for data analyses. Overall, 2.3% and 8.9% of NSHE in patients with T1DM and T2DM, respectively, resulted in healthcare professional contact. Across countries, there was a mean increase in blood glucose test use of 3.0 tests in the week following a NSHE. Among respondents who were employed (48%), loss of work-time after the last hypoglycemic event was reported for 9.7% of NSHE. Overall, 10.2% (daytime) and 8.0% (nocturnal) NSHE led to work-time loss, with a mean loss of 84.3 (daytime) and 169.6 (nocturnal) minutes among patients reporting work-time loss. Additionally, patients reported feeling tired, irritable, and having negative feelings following hypoglycemia.
Limitations:
Direct comparisons between studies must be interpreted with caution because of different definitions of hypoglycemia severity, duration of the studies, and methods of data collection.
Conclusions:
NSHE were associated with use of extra healthcare resources and work-time loss in all countries studied, suggesting that NSHE have considerable impact on patients/society.
Background
The burden of diabetes is one of the greatest challenges of the 21st century, accounting for 11% of total healthcare expenditure worldwide in adults in 2011 ($465 billion)Citation1, largely due to the cost of diabetes-related complications. Whilst the long-term benefits of tight glycemic control are well recognized, intensive treatment of diabetes increases the frequency of hypoglycaemiaCitation2–5. Frequent experience of hypoglycemia may lead to hypoglycemia unawareness which in turn may further increase the risk of hypoglycemia, in particular severe episodesCitation6,Citation7. Therefore, many physicians and patients are reluctant to initiate insulin therapy, due to the fear and perceived burden of hypoglycemiaCitation8, which may lead to sub-optimal glycemic control; hence, reducing the risk of hypoglycemia may enable patients to achieve better glycemic control safelyCitation7. Hypoglycemia occurs most frequently in patients with type 1 diabetes mellitus (T1DM) due to the intensive insulin therapy regimen and the impaired counter-regulatory defense mechanisms, but is also common in patients with insulin-treated type 2 diabetes mellitus (T2DM)Citation7,Citation9–11. Severe hypoglycemia is the most commonly studied form of hypoglycemia and has a considerable economic impact; for example, glucose-lowering therapies account for 94.6% of all endocrine-related emergency hospitalizations in older patientsCitation12.
Non-severe hypoglycemia may be symptomatic (usually characterized by a pounding heart, trembling, hunger, and/or sweating) or asymptomatic. A study by Brod et al.Citation13 investigated the economic consequences of non-severe hypoglycemia for patients and their employers in the US, UK, Germany, and France. Non-severe hypoglycemia was associated with a substantial economic burden, due to its high frequency and the associated lost productivity and increased healthcare resource costsCitation13. Similarly, a recent study showed the considerable impact of nocturnal non-severe hypoglycemic events (NSHE) on patients across nine countriesCitation14. Moreover, hypoglycemia reduces patient wellbeing where both severity and frequency of hypoglycemia are associated with reduced quality-of-lifeCitation13,Citation15–19. Hypoglycemia can also trigger patient fear and anxiety, disrupting sleep, domestic, and social life, and leading to patients maintaining a higher-than-optimal glucose levelCitation13,Citation19,Citation20. The frequency of hypoglycemic events may be under-reported because many patients do not inform their healthcare professional about their hypoglycaemiaCitation21, and also because clinical trials often exclude patients who experience recurrent severe hypoglycemia or experience hypoglycemia unawareness, which are both predictors of risk of hypoglycemiaCitation9.
Limited data exist on the use of healthcare resources due to hypoglycemia induced by glucose-lowering treatment in many countries. This study was undertaken to collect country-specific data on the rate of NSHE among patients with insulin-treated diabetes, and to assess the health-economic and patient-impact consequences of non-severe hypoglycemia in seven European countries. Results from the first part of the study have been published elsewhereCitation21. The aim of the second part of the study, reported here, was to investigate the impact on healthcare resource use and patient outcomes of self-reported NSHE in patients with T1DM and insulin-treated T2DM.
Methods/design
Study design
Patients with insulin-treated diabetes were invited to complete on-line questionnaires to investigate the frequency and impact of hypoglycemia in real-life settings in seven European countries (Austria, Denmark, Finland, the Netherlands, Norway, Sweden, and Switzerland). Patients were invited to participate if they met the screening criteria of a confirmed diagnosis of diabetes, were >15 years of age, and were currently being treated with any insulin regimen. Inclusion criteria were kept to a minimum in order to obtain data that were representative for a broad patient population.
Patients completed the questionnaire on four occasions at weekly intervals, to obtain data on frequency of NSHE in the previous 7 days and hypoglycemia-related resource use following patients’ last NSHE. The first questionnaire was also used to collect data on patient demographics and patient experience and knowledge of hypoglycemia. All respondents completed the questionnaires anonymously, in line with the industry regulations (European Pharmaceutical Marketing Research Association [EphMRA] and European Society for Opinion and Marketing Research [ESOMAR]). A minimum incentive was offered (€5–25) for the time taken to complete the entire survey (35 min in total for the four questionnaires), to ensure that respondents participated for non-monetary reasons.
A NSHE was defined as an event with symptoms of hypoglycemia, with or without blood glucose measurement, or asymptomatic with a low blood glucose measurement (<3.1 mmol/L), which the patient could manage without assistance. Patients were categorized according to whether they had been diagnosed with T1DM or T2DM, and patients with T2DM were further grouped according to the type of insulin therapy they received: BOT—basal-only therapy, BB—basal--bolus therapy, or O—patients on ‘other’ insulin regimens; this included those on pre-mixed insulin, using an insulin pump or on bolus-only insulinCitation21.
Recruitment methodologies
Patients were primarily recruited via existing large online panels deemed to reflect a representative sample of local populations based on age, gender, and other demographic characteristics. This accounted for 82% of respondents and was the only method of recruitment used in the Netherlands. Where an insufficient number of respondents could be identified via online panels, other methods of recruitment were initiated, including the use of advertisements on diabetes-related websites and patient association websites, face-to-face recruitment, telephone recruitment, and subsequent referrals from friends and family. Additionally, some patients were directly recruited by nurses at general practitioner (GP) clinics who had been asked to identify patients and seek consent for participation before providing contact details for those that were eligible to take part in the survey. A target of 600 patients per country was set with an expectation that the probability of a hypoglycemic event occurring in the last 7 days would have a 95% confidence interval of ±4%.
Outcomes
The questionnaires were used to collect data on the frequency of daytime and nocturnal NSHE during the preceding 7 days (as reported by Östenson et al.Citation21). Data were also collected on healthcare resource use following a NSHE, e.g., contact made with healthcare professionals and the number of extra blood glucose strips used. Loss of work-time following a NSHE was assessed by asking patients to report time off work and lost productivity, i.e., where patients were at work but were not as effective as usual (e.g., rescheduling work, postponing appointments, struggling to focus). Patient wellbeing was examined using questions relating to negative feelings following a NSHE, duration of negative feelings following hypoglycemia, and how hypoglycemia affected a patient’s day. Patients were only asked to provide information relating to their last NSHE, in order to reduce the burden to respondents. It was assumed that the behavior following the last NSHE was representative of the average across all the reported NSHEs.
Data cleaning was performed to remove unrealistic or extreme outliers, as described in more detail in Östenson et al.Citation21. Where applicable, the questions requiring values as entries had pre-programmed minimum and maximum values. In order to exclude non-serious responders, patients were omitted if they provided erroneous answers to simple demographic questions or inconsistent answers, such as a disease duration greater than their age. Patients who did not know whether they had T1DM or T2DM were also excluded.
Results
Baseline characteristics and demographics
In total, 3959 respondents completed at least one wave of the survey, with 76%, 66%, and 57% completing waves two, three, or four, respectively. Following data cleaning, 132 (3.3%) responses were excluded. From the remaining 3827 respondents, 11,440 patient-week records were collected and used for the analyses.
The demographic characteristics of the overall patient population, and by country and diabetes type, are summarized in . Patients with T1DM and T2DM had mean glycosylated hemoglobin (HbA1c) values of 7.7% (61 mmol/mol) and 7.6% (60 mmol/mol), respectively. The overall employment rate was 48%, which was similar between the countries investigated, ranging from ∼40% in the Netherlands and Austria to 60% in Switzerland. The mean duration of insulin treatment was 19.9, 5.3, 8.9, and 7.1 years for patients with T1DM, T2DM-BOT, T2DM-BB, and T2DM-O, respectively.
Table 1. Patient demographics.
Mean frequencies of NSHE/patient-week for all patients were 1.8 (T1DM), 0.4 (T2DM-BOT), 0.7 (T2DM-BB), and 0.5 (T2DM-O), corresponding to annual event rates of 91.0, 20.3, 35.4, and 27.0 NSHE, respectivelyCitation21. The proportion of NSHE occurring at night was 28% for the overall population and 22%, 32%, 22%, and 27% in patients with T1DM, T2DM-BOT, T2DM-BB, and T2DM-O, respectively.
Healthcare resource use
Following a NSHE, contact with a healthcare professional was reported by 2.3%, 8.9%, 7.0%, and 9.7% of patients with T1DM, T2DM-BOT, T2DM-BB, and T2DM-O, respectively (). Across countries, there was a mean increase in blood glucose test use in the week following a NSHE of 3.0 overall and 2.9, 2.7, 3.1, and 3.8 in patients with T1DM, T2DM-BOT, T2DM-BB, and T2DM-O, respectively (). Across all seven countries, 13.6% [95% confidence interval (CI): 12.2; 14.9] of NSHE led to patients reducing their insulin dose (). This was similar across countries, except for Norway, where only 4.0% [95% CI: 1.7; 6.4] of NSHE led to a reduction in insulin dose ().
Table 2. Increased resource use and work-time lost due to NSHE.
Work-time loss
Among those who were employed, loss of work-time was reported following 9.7% of NSHE (). Overall, 10.2% and 8.1% of NSHE led to work-time loss after a daytime or a nocturnal NSHE, respectively. Across countries the mean (SD) work-time lost among patients who reported work-time loss (n = 282) was 84.3 (144.5) for a daytime and 169.6 (241.0) min for a nocturnal event ().
Overall, 10% of NSHE led to patients rescheduling their working day, 3% to postponing appointments, 27% to reporting that they had difficulty in focusing at work, and 12% feeling that their colleagues noticed that they were experiencing the effects of a hypoglycemic event. The time spent doing something about a NSHE (for example monitoring your blood sugar, going to get something to eat or drink and then eating or drinking it) was similar following a daytime and a nocturnal event and did not vary greatly between countries (). The overall mean (SD) time taken to return to normal functioning was 50.4 (357.6) min following a daytime NSHE and 80.5 (267.6) min following a nocturnal NSHE. The time taken to return to normal functioning was higher following a nocturnal NSHE compared with a daytime NSHE ().
Patient wellbeing
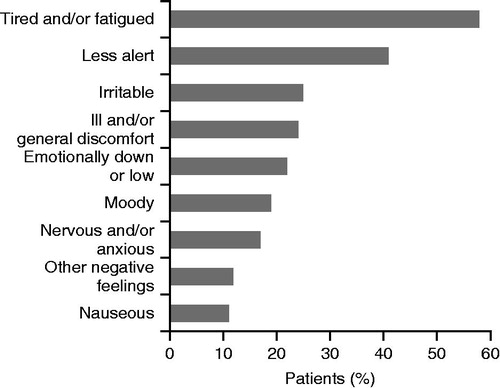
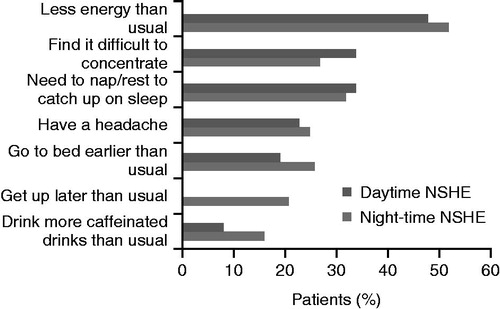
NSHE impacted on patient wellbeing, with the most frequent complaints being tiredness/fatigue (58%), feeling less alert (40%), and feeling irritable (24%) (). On average the negative feelings following hypoglycemia lasted for a mean of 5.4 h following a daytime event and 12.2 h following a nocturnal event. Experiencing a nocturnal NSHE had a substantial impact on patient behavior the following day: 52% of NSHE led to patients reporting less energy than usual, 32% needed to rest during the day, and 27% found it difficult to concentrate (). Similar effects were reported following a daytime NSHE (). Following 51% of NSHE, patients felt that they were not able to complete their work tasks in a timely manner ().
Discussion
The results of this large-scale survey of patients with T1DM and insulin-treated T2DM show that non-severe hypoglycemia leads to an increase in healthcare resource use and to a loss of productivity. Furthermore, a substantial proportion (28%) of patient-reported non-severe hypoglycemia occurred nocturnally; in general this had a greater effect on productivity and patient wellbeing than daytime hypoglycemia.
In terms of direct healthcare resource use, patients increased the number of blood glucose tests used by 3.0 in the week following the NSHE. This compares with an overall increase of 5.6 per week and 3.6 per week for nocturnal NSHE reported by Brod et al.Citation13,Citation14 in two different studies. Even greater increases in blood glucose test use of 71% and 80% following a NSHE in T1DM and T2DM, respectively, have been reportedCitation19.
A number of patients contacted a healthcare professional following a NSHE in the current study. The proportion was highest in Switzerland (9.4%) and lowest in Denmark and Sweden (both 2.9%). Furthermore, across countries, patients with T2DM-BOT were the most likely to contact their healthcare professional, whereas those with T1DM were least likely. This may be because patients with T1DM frequently had a longer disease duration and a higher frequency of NSHE, and were therefore more familiar with hypoglycemia or more confident at managing it themselves. In contrast, patients on BOT were likely to have been using insulin therapy for a shorter period of time. Overall the proportion of patients contacting their healthcare professional (4.8%) was lower than the 25% reported by Brod et al.Citation13 for the UK, Germany, France, and the US, and the 14.8% reported across nine countries following a nocturnal NSHECitation14. The proportion contacting a healthcare professional in the Netherlands (5.6% vs 9.5%) and Sweden (2.9% vs 6.2%) were similar between this study and Brod et al.Citation14. Differences between studies may reflect inter-country differences; for example there may be cultural differences in how frequently patients contact their doctors, and/or differences in the quality of patient education that could be influential, especially considering the high proportion of patients on complex insulin regimens. The latter usually receive more detailed instructions on insulin use and are more experienced in self-management of hypoglycemic events. It has also been shown that many patients do not communicate effectively with their healthcare professionals regarding their NHSE, with the lowest level of communication reported during routine appointments in the Netherlands, with 86% of T1DM, 64% of T2DM-BOT, 77% of T2DM-BB, and 79% of T2DM-O rarely or never informing their healthcare professionals about hypoglycemic eventsCitation21.
The frequency of NSHE also impacts indirectly on the economy due to lost productivity, e.g., due to lost work-time and missed appointments. In the current study, 10.2% and 8.0% of NSHE led to respondents missing work-time following a daytime or a nocturnal event, compared with 18.3% and 22.7% missing work if their NSHE occurred during or outside working hours (including nocturnal) found by Brod et al.Citation13. The estimated mean loss in working time in this study was 84.3 min (1.4 h) after a daytime NSHE and 169.6 min (2.8 h) after a nocturnal event among patients reporting work-time loss, with considerable differences between countries. This is considerably lower than the values observed in the study by Brod et al.Citation13, where the mean work-time loss after a nocturnal NSHE was 14.7 h among patients reporting work-time loss. A smaller UK-based study, evaluating mostly patients with T1DM who experienced a low rate of NSHE compared to the current study, showed that a mean of only 12.8 min work-time was lost following non-severe hypoglycemia occurring at any time of dayCitation22.
The overall annual direct medical costs of patients with T2DM in eight European countries were estimated as €2834 in 2002Citation23, indicating a substantial economic burden of diabetes. The present study estimates the resource use, but not the direct costs, associated with a NSHE. Studies that have included costs related to hypoglycemia include one performed in patients with T2DM in Sweden, which estimated the direct and indirect costs of all severe and non-severe hypoglycemia to be US$12.9 and $14.1 per patient per month, respectivelyCitation24. The annual cost of productivity loss following non-severe hypoglycemia per patient has been estimated at ∼$2300 across the US, UK, Germany, and FranceCitation13. However, it should be noted that this was based on an average of more than 14 h work-time loss among patients in employment reporting work-time loss. It is also recognized that the costs arising due to severe hypoglycemia are higher than those for non-severe hypoglycemia. Furthermore, asymptomatic non-severe hypoglycemia is likely to be common and may result in lost productivity, but by its nature is difficult to quantify.
Respondents reported tiredness/fatigue and negative feelings following a NSHE, indicating that non-severe hypoglycemia significantly impacts on patient wellbeing. This study and the study by Brod et al.Citation14 show that the time needed to return to normal functioning or recovery phase after a nocturnal NSHE lasted considerably longer than the acute symptoms of hypoglycemia. The results of this survey are in line with previous studies showing that hypoglycemia negatively affects patient quality of lifeCitation13,Citation15. Hypoglycemia may lead to anxiety/worry about future episodes, or to patients maintaining a higher than optimal blood glucose level, by reducing insulin dose or through deliberate over-eating, to avoid hypoglycemia.
To date, studies of hypoglycemia have focused on T1DM more than T2DM and often on severe hypoglycemia rather than non-severe hypoglycemia. Whilst the frequency of hypoglycemia is greater in T1DM than T2DM, the lower occurrence in T2DM is not inconsequential, becoming more frequent with disease durationCitation9 and more stringent treatment goals. Furthermore, due to the high frequency of non-severe hypoglycemia and the proportion of patients with diabetes that it affects, the impact and economic consequences may be substantial. This is the first study, to our knowledge, to examine healthcare resource use specifically following NSHEs in all of these seven European countries and supports the data reported on nocturnal NSHE for the Netherlands and Sweden by Brod et al.Citation14. It provides a valuable insight into the impact of non-severe hypoglycemia, and highlights the fact that reducing NSHEs could have economic benefits and improve patient wellbeing. As hypoglycemia is a major barrier to achieving good glycemic control in patients with T1DM and insulin-treated T2DMCitation7, measures to reduce the incidence of severe and non-severe hypoglycemia could help lessen the burden on patients and the economic burden on society. Furthermore, data from a large observational study showed that patients who experience NSHE are significantly more likely to experience severe hypoglycemia, further supporting the rationale for reducing the occurrence of NSHECitation25.
The study also has some limitations. As the survey was completed via the internet, this made it only available to those who were literate and had computer access, introducing an element of selection bias. However, the rate of literacy and access to the internet is very high in all of the seven European countries included in this studyCitation26. Direct comparisons between studies must be interpreted with caution because of the differing definitions of hypoglycemia severity, different duration of the studies, and different methods of including and/or recruiting patients to studies. The current data are based on patient reports, and the anonymity of the patients completing the questionnaire does not allow for cross-validation of the accuracy of the information. The data are based on patient recall, so there may be an element of recall bias or reporting inaccuracy. Respondents were asked about NSHE experienced in the previous 7 days, so they were not required to recall information over long periods. However, the fact that the results in the different countries were generally consistent strengthens the validity of the data. Overall, the mean HbA1c values of patients included in this study are relatively low; this could suggest a bias in selection of patients with near-normal glycemia, thus being more prone to develop NSHE. Additionally, patients in good control may be keener to participate in studies such as this one or they may be more aware of their HbA1c level, which could also lead to a reporting bias. However, recent data from a randomized disease management study in patients with T2DM treated by GPs in Austria showed a mean HbA1c of 7.4%, suggesting that this average glycemia level may be representative for the typical insulin-treated diabetes populationCitation27.
Conclusions
NSHEs were associated with increased use of healthcare resources and work-time loss in all the countries studied and had a negative impact on wellbeing. It therefore seems that, both from an economic and a patient wellbeing perspective, more attention to prevention of non-severe hypoglycemia is needed.
Transparency
Declaration of funding
Funding for this study was provided by Novo Nordisk. The sponsor was involved in the study design, data collection, data review, and data analysis. All authors had full access to the data and were involved in data interpretation and manuscript writing. P. Geelhoed-Duijvestijn had the final decision to submit the manuscript for publication and takes responsibility for its content.
Declaration of financial/other relationships
P. Geelhoed-Duijvestijn has received honoraria for lectures from Novo Nordisk and as a member of Advisory Boards of Medtronic, Sanofi Aventis, and Eli Lilly. U. Pedersen-Bjergaard has received honoraria for lectures from Novo Nordisk, Sanofi Aventis, and BMS, and has served as a member of Advisory Boards for Novo Nordisk and AstraZeneca. R. Weitgasser has received honoraria for lectures and as a member of Advisory Boards for Novo Nordisk, Eli Lilly, Sanofi Aventis, Novartis, Medtronic, MSD, Takeda, Astra Zeneca/BMS, Boehringer-Ingelheim, and Roche Diagnostics. J. Lahtela has received honoraria for the preparation of educational material and lecture from Novo Nordisk, Sanofi Aventis, Eli Lilly, Novartis, and Merck. M. M. Jensen is an employee at Novo Nordisk Scandinavia. C. Östenson has received honoraria as a symposium speaker for Novo Nordisk Scandinavia. JME Peer Reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgments
The authors take full responsibility for the content of this manuscript. Adele Norman at Watermeadow Medical (supported by Novo Nordisk) provided medical writing support.
References
- International Diabetes Federation. IDF Diabetes Atlas, 5th edn. Brussels: International Diabetes Federation, 2011
- The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med 1993;329:977–86
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:837–53
- ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–72
- Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129–39
- Chico A, Vidal-Rios P, Subira M, et al. The continuous glucose monitoring system is useful for detecting unrecognized hypoglycemias in patients with type 1 and type 2 diabetes but is not better than frequent capillary glucose measurements for improving metabolic control. Diabetes Care 2003;26:1153–7
- Cryer PE. Hypoglycaemia: the limiting factor in the glycaemic management of type I and type II diabetes. Diabetologia 2002;45:937–48
- Dailey GE, III. Early insulin: an important therapeutic strategy. Diabetes Care 2005;28:220–1
- Donnelly LA, Morris AD, Frier BM, et al. Frequency and predictors of hypoglycaemia in type 1 and insulin-treated type 2 diabetes: a population-based study. Diabet Med 2005;22:749–55
- UK Hypoglycaemia Study Group. Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia 2007;50:1140–7
- Akram K, Pedersen-Bjergaard U, Carstensen B, et al. Frequency and risk factors of severe hypoglycaemia in insulin-treated Type 2 diabetes: a cross-sectional survey. Diabet Med 2006;23:750–6
- Budnitz DS, Lovegrove MC, Shehab N, et al. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 2011;365:2002–12
- Brod M, Christensen T, Thomsen TL, et al. The impact of non-severe hypoglycemic events on work productivity and diabetes management. Value Health 2011;14:665–71
- Brod M, Wolden M, Christensen T, et al. A nine country study of the burden of non-severe nocturnal hypoglycaemic events on diabetes management and daily function. Diabetes Obes Metab 2013;15:546--57
- Vexiau P, Mavros P, Krishnarajah G, et al. Hypoglycaemia in patients with type 2 diabetes treated with a combination of metformin and sulphonylurea therapy in France. Diabetes Obes Metab 2008;10(1 Suppl):16–24
- Levy AR, Christensen TL, Johnson JA. Utility values for symptomatic non-severe hypoglycaemia elicited from persons with and without diabetes in Canada and the United Kingdom. Health Qual Life Outcomes 2008;6:73
- Fidler C, Elmelund CT, Gillard S. Hypoglycemia: an overview of fear of hypoglycemia, quality-of-life, and impact on costs. J Med Econ 2011;14:646–55
- Jonsson L, Bolinder B, Lundkvist J. Cost of hypoglycemia in patients with Type 2 diabetes in Sweden. Value Health 2006;9:193–8
- Leiter LA, Yale JF, Chiasson JL, et al. Assessment of the impact of fear of hypoglycemic episodes on glycemic and hypoglycemic management. Can J Diabetes 2005;29:186–92
- Frier BM. How hypoglycaemia can affect the life of a person with diabetes. Diabetes Metab Res Rev 2008;24:87–92
- Östenson CG, Geelhoed-Duijvestijn P, Lahtela J, et al. Patient-reported non-severe hypoglycaemic events in Europe. Diabet Med 2013; [in press]
- Leckie AM, Graham MK, Grant JB, et al. Frequency, severity, and morbidity of hypoglycemia occurring in the workplace in people with insulin-treated diabetes. Diabetes Care 2005;28:1333–8
- Jönsson B. Revealing the cost of type II diabetes in Europe. Diabetologia 2002;45:S5–12
- Lundkvist J, Berne C, Bolinder B, et al. The economic and quality of life impact of hypoglycemia. Eur J Health Econ 2005;6:197–202
- Sreenan S, Anderson M, Thorsted BL, et al. Increased risk of severe hypoglycaemic events with increasing frequency of non-severe hypoglycaemic events in patients with type 1 and type 2 diabetes. Diabetologia 2012;55(1 Suppl):S258
- US Central Intelligence Agency. The World Factbook. 2013. https://www.cia.gov/library/publications/the-world-factbook/geos/sw.html. Accessed September 2013
- Flamm M, Winkler H, Panisch S, et al. Quality of diabetes care in Austrian diabetic patients willing to participate in a DMP -- at baseline. Wien Klin Wochenschr 2011;123:436–43