Abstract
Background:
The Timing of Intervention in Acute Coronary Syndromes (TIMACS) trial demonstrated that early invasive intervention (within 24 hours) was similar to a delayed approach (after 36 hours) overall but improved outcomes were seen in patients at high risk. However, the cost implications of an early versus delayed invasive strategy are unknown.
Methods and results:
A third-party perspective of direct cost was chosen and United States Medicare costs were calculated using average diagnosis related grouping (DRG) units. Direct medical costs included those of the index hospitalization (including clinical, procedural and hospital stay costs) as well as major adverse cardiac events during 6 months of follow-up. Sensitivity and sub-group analyses were performed. The average total cost per patient in the early intervention group was lower compared with the delayed intervention group (−$1170; 95% CI −$2542 to $202). From the bootstrap analysis (5000 replications), the early invasive approach was associated with both lower costs and better clinical outcomes regarding death/myocardial infarction (MI)/stroke in 95.1% of the cases (dominant strategy). In high-risk patients (GRACE score ≥141), the net reduction in cost was greatest (−$3720; 95% CI −$6270 to −$1170). Bootstrap analysis revealed 99.8% of cases were associated with both lower costs and better clinical outcomes (death/MI/stroke).
Limitations:
We were unable to evaluate the effect of community care and investigations without hospitalization (office visits, non-invasive testing, etc). Medication costs were not captured. Indirect costs such as loss of productivity and family care were not included.
Conclusions:
An early invasive management strategy is as effective as a delayed approach and is likely to be less costly in most patients with acute coronary syndromes.
Introduction
Although an invasive management strategy for acute coronary syndromes (ACS) without ST-segment elevation is superior to conservative managementCitation1,Citation2, the optimal timing of such therapy has been a matter of debate. This question was recently evaluated in the multinational Timing of Intervention in Acute Coronary Syndromes (TIMACS) study, where an early invasive strategy did not differ greatly from a delayed approach in preventing the primary outcome of death from any cause, myocardial infarction (MI), or stroke at 6 monthsCitation3. However, an early invasive strategy appeared to be superior in higher-risk patients (GRACE risk score ≥141)Citation3.
Given these data, the cost implications of an early versus delayed invasive management strategy is important to evaluate. Efficient use of scarce healthcare resources has become vital in maintaining affordable medical care. It is possible that there are lower costs associated with the early invasive strategy, due to a shorter duration of hospitalization and fewer cases of refractory ischemia. On the other hand, an early invasive strategy may lead to a greater number of procedures performed given the higher thrombotic burden of plaque which may offset its cost advantage in favor of the delayed approach. Accordingly, we performed a cost analysis of early versus delayed coronary angiography in ACS based on the results from the TIMACS study to determine if one strategy favors the other when costs are considered in the context of the results of the clinical trial.
Methods
Clinical trial
The TIMACS trial was a randomized, parallel-group, multicenter study performed from April 2003 through June 2008 with 650 patients from North America, 442 patients from South America, 1065 patients from Europe, 846 patients from Asia and 28 patients from Australia. The design and main results of the TIMACS study have been publishedCitation3. Eligible patients presenting to the hospital with unstable angina or myocardial infarction without ST-segment elevation within 24 hours from symptom onset had to have two of the three following high-risk criteria: age 60 years or older, elevated cardiac biomarkers above the upper limit of normal, or electrocardiogram changes consistent with ischemia (ST-segment depression of ≥1 mm or transient ST-segment elevation or T-wave inversion of >3 mm). Patients not eligible for an invasive strategy were excluded. Of the 3031 patients enrolled, 1593 were randomized to the early invasive group on whom coronary angiography was performed within 24 hours (median time of 14 hours). The remaining 1438 patients were randomized to the delayed invasive group on whom coronary angiography was performed at a minimum of 36 hours (median time 50 hours).
Revascularization was attempted in the two groups if at least one coronary stenosis considered hemodynamically significant was suitable for intervention. Clinical follow-up occurred over 6 months. All patients received conventional therapy regardless of treatment allocation. Treatments included aspirin, ADP-receptor antagonists, beta blockers, angiotensin converting enzyme (ACE) inhibitors and statin therapy. All cost comparisons are based solely on an early versus delayed invasive strategy. Results of the TIMACS study are shown in .
Table 1. Summary of the TIMACS trial at 6 months.
Study perspective
This analysis is from the perspective of a third party payer, where all direct costs are recorded and indirect costs were not evaluated.
Cost analysis and healthcare utilization
Costs were estimated by multiplying counts of resource use by price weights derived from a similar population of patients in the United States. Costs are reported in United States dollars (USD 2008). No annual discount rate was required given the 6 month duration of the study.
Detailed hospitalization data were prospectively collected on the study case report forms for all patients enrolled in the study. Information regarding indication for hospitalization, in-hospital events, diagnostic/therapeutic procedures and length of stay were reported. During the initial hospitalization, a diagnosis-related group (DRG) was assigned based on each diagnosis or procedure noted on the case report forms. Costs were assigned based on the Medicare reimbursement rates per DRG code using national averages from the schedule of benefits for the Medicare system (MEDPAR 2008Citation4). Physician costs were estimated according to the DRG-specific ratio of physician reimbursement to hospital costs and were included in the unit cost estimateCitation5–7 ().
Table 2. Unit costs per DRG code.
Hospital costs primarily consisted of three components: clinical event, procedural and hospital stay costsCitation8. While DRG-based costs are valuable estimates of clinical event costs (medical conditions and procedures), they are insensitive to hospital stay costs during hospitalization. Since the ‘hotel portion’ of hospital stay costs are broadly constant over the length of stayCitation8 separate costs were assigned to reflect the hospital stay costs per day (). These hospital stay costs were based on prior published cost analysis of similar United States patients (Duke Transition One cost-accounting system) which report room and monitoring costs of $624 per day in hospital, assuming the lowest ratio of nurses to patients (1:6) and providing a conservative estimateCitation9. These costs were adjusted to year 2008 values using the medical care proportion of the consumer price index resulting in $869 per day.
The primary economic endpoint was to evaluate the cost implication of an early versus delayed invasive strategy over a 6 month interval, which included the index hospitalization and repeat hospitalization events. Community care and outpatient investigations, non-invasive procedures and medications were not collected in the trial and were not used in this study. The study was approved by the local institutional review board. Informed written consent was obtained from each patient and the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Statistical analysis
Descriptive statistics were summarized as medians with 25th and 75th percentiles for continuous variables and the Mann–Whitney U test or Kruskal–Wallis H test was used for group comparisons where appropriate. For categorical variables, the data were summarized in percentages and chi-square or Fisher’s exact test was used to assess group differences where appropriate. Unit costs were applied to cost hospital utilization data of each patient enrolled in the study. Thereafter, averages were taken between each of the treatment groups. Differences in mean costs between early versus delayed coronary angiography groups were compared on an intention-to-treat basis. As cost data are unlikely to be normally distributed, the bootstrap method was used to obtain confidence intervals (CIs)Citation10. The bias corrected and accelerated method was used for confidence intervalsCitation11. Heterogeneity differences in costs by treatment group in different pre-specified subgroups analyzed in the original trial were tested using an interaction term in an analysis of variance (ANOVA), using Generalized Linear Models (GLM). Since the total cost was skewed on inspection, transformation using the logarithm of the inverse of the cost was used before using the GLM procedure.
Results
Costs
The average costs for treatment of clinical events were lower in patients treated with an early invasive strategy compared with a delayed strategy (−$196; 95% CI −$430 to $38) (). Lower average costs of refractory ischemia were seen in the early invasive group (−$52). The average costs for cardiovascular procedures (coronary angiography, PCI [percutaneous coronary intervention], CABG [coronary artery bypass grafting]) over 6 months were greater for an early invasive strategy compared with a delayed approach ($346; 95% CI $-440 to $1132) (). Higher average cost differences of PCI ($541) and CABG ($232) were noted per patient with the early invasive approach. As shown, patients in the early invasive arm had a shorter 6 month hospital stay compared to the delayed invasive strategy (median 7.0 versus 9.0 days respectively). Given shorter time in hospital, the hospital stay costs for the early invasive patients were lower compared to the delayed invasive group (−$1320; 95% CI −$2074 to −$566) (). There was no difference in the frequency of off-hour procedures between early intervention and a delayed approach (14.2% versus 12.5%, p = 0.46 respectively). The total cost for 6 month follow-up includes clinical, procedural and hospital stay costs. The total cost for the early invasive group tended to be lower compared to the delayed invasive group (−$1170; 95% CI −$2542 to $202) ().
Table 3. Average costs (US$) per patient.
Bootstrap analysis
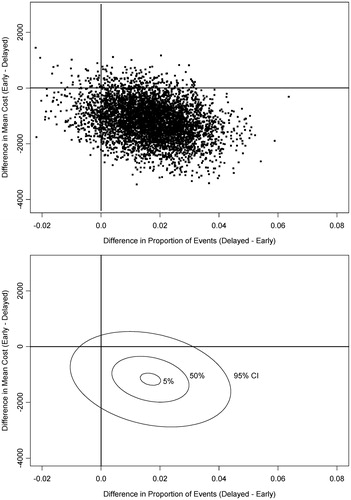
illustrates the relationship between the differences in mean cost and clinical events in the bootstrap analysis (5000 iterations). Overall, 95.1% of cases had lower costs and improved clinical outcomes favoring an early invasive approach (dominant strategy).
Sensitivity analysis
A sensitivity analysis was performed to assess total costs for 6 month follow-up of cardiac services in Canada using a detailed micro-costing system developed at McMaster University. Canadian costs were applied to all enrolled patients in the trial (n = 3031). Costs were reported in Canadian dollars (CAD 2008). All components of healthcare consumption including hospital stay (coronary care unit or intensive care unit, step-down unit, regular ward) pharmacy costs (main pharmacy and ward stock), all blood work, radiology tests, nuclear medicine investigations and procedures (coronary angiogram, PCI and CABG) were recorded and calculatedCitation12. The total cost for the early invasive group was significantly lower compared to the delayed invasive group (−$1390; 95% CI −$2464 to −$316). The lower overall costs were attributed to reduced hospital stay costs with an early invasive approach (−$1381; 95% CI −$2216 to −$546).
Subgroups results
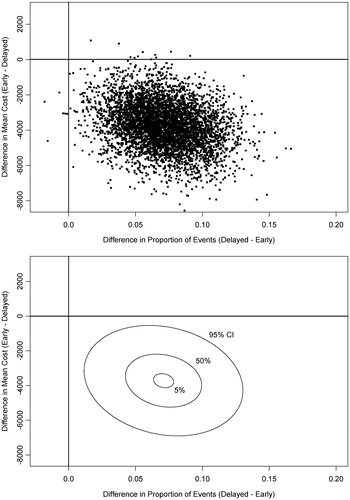
As pre-specified subgroups were including in the TIMACS study, total costs for each subgroup were analyzed using an interaction test. As shown in , we found no significant interaction, with the exception of high-risk patients (GRACE risk score ≥141) where there was a net decrease in costs of $3720 (95% CI −$6270 to −$1170) per patient. As age may be unduly emphasized in the GRACE risk score for high-risk patients, we compared patients ≥65 years receiving coronary angiography with an early invasive versus a delayed approach and found no difference (14.7% versus 11.2%, p = 0.23 respectively). A bootstrap analysis of patients with a GRACE risk score ≥141 revealed 99.8% of cases had lower costs and better clinical outcomes (), a clear dominant strategy.
Table 4. Subgroup analysis of average cost (US$) per patient.
Discussion
The results of the Timing of Intervention in Acute Coronary Syndromes (TIMACS) trial economic analysis demonstrate that an early invasive strategy in acute coronary syndromes without ST-segment elevation saves costs compared with a delayed strategy. The greatest savings appears to be in the high-risk patients receiving early coronary angiography. Moreover, the early invasive approach was dominant and associated with both lower costs and better clinical outcomes in 95.1% of 5000 bootstrap iterations. The lower overall costs were primarily due to reduced length of stay in hospital in patients managed with an early invasive strategy.
It is well recognized that healthcare resources are scarce. To achieve maximum health gains we should use them efficiently. It is no wonder that it has become a national mandate to evaluate alternate clinical approaches and policy reform to improve efficiencyCitation13. When it is possible to find approaches to reduce hospital costs without affecting quality of care or patient safety, these strategies should be promoted as they free up resources for use in other interventions. Similar to patients with ST-segment elevation myocardial infarctionCitation14,Citation15, routine coronary angiography is also beneficial in patients with non-ST-segment elevation ACS. The randomized trials evaluating invasive versus conservative treatment were associated with large variations in timing of early coronary angiography ranging from 6–96 hoursCitation16–20. TIMACS was the first randomized study to address optimal timing of coronary angiography with intended intervention and found an early approach (<24 hours) did not differ greatly from delayed treatment (≥36 hours) in preventing death, MI or stroke at 6 months, with similar safety outcomes between the strategiesCitation3.
Within this context, we found a total cost advantage of $1170 per patient, largely due to a 2 day reduced hospital stay in patients undergoing early coronary angiography. The impact of these results could have important implications on resource use, given that over 1.5 million patients are admitted to hospital with an ACS each year in the United StatesCitation21. Similar data of decreasing length of stay in acute myocardial infarction that lead to reduced hospital costs have been previously describedCitation9. The results of our analysis favoring an early invasive strategy in non-ST-segment elevation ACS may influence the decision-making process by providing improved quality care at reduced hospital costs. Our results provide clear justification for proceeding, when possible, earlier to coronary angiography given similar safety with overall reduced costs. Shorter hospitalization may also reduce the costs for other unintended events while in hospital (i.e. nosocomial infection), although this was not specifically addressed in our study.
It is noteworthy that high-risk patients (GRACE score ≥141) derived significant clinical benefit along with reduced total cost with an early invasive strategy. In fact, the greatest cost advantage of $3720 per patient was seen in these patients undergoing early invasive management. In this subgroup we feel that every effort should be made to intervene early.
Study limitations
First, the TIMACS trial was a multinational study where unit cost measurements were based on United States DRG estimates. This may not fully account for the potential differences in medical practice and resource use between countries or healthcare systems. However, calculation of costs in different countries would not affect the overall message of the study as shorter hospitalization with an early invasive strategy compared to a delayed approach would still result in a total reduction in cost – albeit the magnitude of benefit may vary as demonstrated in our sensitivity analysis using Canadian cost data from a universal healthcare system. Second, DRG costs assume that all patients are clinically similar and would utilize the same amount of healthcare resources without consideration for off-hour costs. Given the temporal differences between an early invasive approach versus a delayed strategy, we looked at the frequency of off-hour procedures and found no appreciable difference between either strategy. Thus, the cost-savings for an early invasive approach should still be present. Overall, using DRG unit costs makes our analysis intentionally conservative as DRGs are the lowest paid rates. Third, we were unable to evaluate the effect of community care and investigations without hospitalization (office visits, non-invasive testing, etc.) along with medication costs. Non-medical costs such as loss of productivity and family care costs were not included. Despite our hospital stay costs being intentionally conservative, thus biasing against the early intervention, we were still able to show a cost advantage. Fourth, cost analysis was limited to the trial follow-up period of 6 months. It is unlikely that the early invasive strategy would accrue additional costs beyond 6 months. Fifth, the results of this study are limited to non-ST elevation ACS patients receiving an invasive strategy. Sixth, contemporary management of patients may have a shorter length of in-hospital stay with improved clinical outcomes limiting the cost savings with an early invasive approach.
This study provides important new information regarding the cost implications of an early versus delayed invasive strategy for the treatment of acute coronary syndromes without ST-segment elevation. Our results suggest that an early invasive approach with coronary angiography saves costs and should be considered for all patients. Moreover, it should be the standard strategy for patients with high-risk acute coronary syndromes. These results may have implications on future policy decisions regarding cost-saving strategies in acute coronary syndromes.
Transparency
Declaration of funding
Supported by the Canadian Institutes of Health Research; by the sponsors of the OASIS-5 study, which included GlaxoSmithKline, Sanofi-Aventis, and Organon NV; by a New Investigator Award from the Canadian Institutes of Health Research (to S.R.M.); and by the Heart and Stroke Foundation of Ontario. They have not been involved in the design, conduct, interpretation, analysis or writing of this study.
Author contributions: S.R.M., as principal investigator, and K.R.B. as co-principal investigator of this economic study have full access to all the data and attest to the accuracy and validity of the economic analysis.
Declaration of financial/other relationships
P.G.S. has disclosed that he received grant support from Sanofi-Aventis and consulting or lecture fees from Astellas, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Endotis, GlaxoSmithKline, Merck, Nycomed, Sanofi-Aventis, Servier, Takeda, and the Medicines Company. D.P.F. has disclosed that he received consulting fees from Johnson & Johnson and grant support from Boston Scientific. C.B.G. has disclosed that he received grant support from Sanofi-Aventis, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, GlaxoSmithKline, the Medicines Company, Novartis, and Merck, and consulting or speaking fees from Sanofi-Aventis, GlaxoSmithKline, the Medicines Company, Novartis, Fibrex, and AstraZeneca. S.Y. has disclosed that he received grant support from Bristol-Myers Squibb, Sanofi-Aventis, and GlaxoSmithKline and consulting and lecture fees from AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, GlaxoSmithKline, Sanofi-Aventis, and Servier. S.R.M. has disclosed that he received grant support from Bristol-Myers Squibb, GlaxoSmithKline, and Sanofi-Aventis and consulting or lecture fees from Abbott Vascular, Astellas, AstraZeneca, Boston Scientific, Bristol-Myers Squibb, Eli Lilly, GlaxoSmithKline, Pfizer and Sanofi-Aventis. K.R.B., A.G., P.R.-M., W.T. and A.L. have disclosed that they have no significant relationships with or financial interests in any commercial companies related to this study or article.
JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgments
No assistance in the preparation of this article is to be declared.
References
- Mehta SR, Cannon CP, Fox KA, et al. Routine vs selective invasive strategies in patients with acute coronary syndromes: a collaborative meta-analysis of randomized trials. JAMA 2005;293:2908-17
- Bavry AA, Kumbhani DJ, Rassi AN, et al. Benefit of early invasive therapy in acute coronary syndromes: a meta-analysis of contemporary randomized clinical trials. J Am Coll Cardiol 2006;48:1319-25
- Mehta SR, Granger CB, Boden WE, et al. Early versus delayed invasive intervention in acute coronary syndromes. N Engl J Med 2009;360:2165-75
- Centers for Medicare and Medicaid Services. Medicare Fee for Service for Parts A & B. Available at: http://www.cms.gov/MedicareFeeforSvcPartsAB/03_MEDPAR.asp#TopOfPage [Last accessed 18 January 2010]
- Mitchell JBR, Lee A, McCall NT. Per Case Prospective Payment for Episodes of Hospital Care. Springfield, VA: US Department of Commerce National Technical Infromation Service, 1995
- Mahoney EM, Mehta S, Yuan Y, et al. Long-term cost-effectiveness of early and sustained clopidogrel therapy for up to 1 year in patients undergoing percutaneous coronary intervention after presenting with acute coronary syndromes without ST-segment elevation. Am Heart J 2006;151:219-27
- Weintraub WS, Mahoney EM, Lamy A, et al. Long-term cost-effectiveness of clopidogrel given for up to one year in patients with acute coronary syndromes without ST-segment elevation. J Am Coll Cardiol 2005;45:838-45
- Drummond MFSM, Torrance GW, O’Brien BJ, et al. Methods for the Economic Evaluation of Health Care Programmes, 3rd edn. Oxford: Oxford Medical Publication, 2005:67
- Newby LK, Eisenstein EL, Califf RM, et al. Cost effectiveness of early discharge after uncomplicated acute myocardial infarction. N Engl J Med 2000;342:749-55
- Briggs A, Gray A. The distribution of health care costs and their statistical analysis for economic evaluation. J Health Serv Res Policy 1998;3:233-45
- Carpenter J, Bithell J. Bootstrap confidence intervals: when, which, what? A practical guide for medical statisticians. Stat Med 2000;19:1141-64
- Smith KM, Lamy A, Arthur HM, et al. Outcomes and costs of coronary artery bypass grafting: comparison between octogenarians and septuagenarians at a tertiary care centre. Can Med Assoc J 2001;165:759-64
- Hlatky MA, Douglas PS, Cook NL, et al. Future directions for cardiovascular disease comparative effectiveness research: report of a workshop sponsored by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol 2012;60:569-80
- Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 2000;283:2941-7
- Antman EM, Hand M, Armstrong PW, et al. 2007 Focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 writing group to review new evidence and update the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction, writing on behalf of the 2004 writing committee. Circulation 2008;117:296-329
- Neumann FJ, Kastrati A, Pogatsa-Murray G, et al. Evaluation of prolonged antithrombotic pretreatment (‘cooling-off’ strategy) before intervention in patients with unstable coronary syndromes: a randomized controlled trial. JAMA 2003;290:1593-9
- Invasive compared with non-invasive treatment in unstable coronary-artery disease: FRISC II prospective randomised multicentre study. FRagmin and Fast Revascularisation during InStability in Coronary artery disease Investigators. Lancet 1999;354:708-15
- Fox KA, Poole-Wilson PA, Henderson RA, et al. Interventional versus conservative treatment for patients with unstable angina or non-ST-elevation myocardial infarction: the British Heart Foundation RITA 3 randomised trial. Randomized Intervention Trial of unstable Angina. Lancet 2002;360:743-51
- de Winter RJ, Windhausen F, Cornel JH, et al. Early invasive versus selectively invasive management for acute coronary syndromes. N Engl J Med 2005;353:1095-104
- Cannon CP, Weintraub WS, Demopoulos LA, et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med 2001;344:1879-87
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics – 2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2007;115:e69-171