Abstract
Objective:
Patients with persistent or longstanding atrial fibrillation have modest success achieving sinus rhythm with catheter ablation or rhythm control medications. Their high risk of stroke, bleed, and heart failure leads to significant morbidity and health care costs. The convergent procedure has been shown to be successful in this population, with 80% of patients in sinus rhythm after 1 year. This study evaluated the cost-effectiveness of the convergent procedure, catheter ablation, and medical management for non-paroxysmal AF patients.
Methods:
A Markov micro-simulation model was used to estimate costs and effectiveness from a payer perspective. Parameter estimates were from the literature. Three patient cohorts were simulated, representing lower, medium, and higher risks of stroke, bleed, heart failure, and hospitalization. Effects were estimated by quality-adjusted life-years (QALYs). Single-variable sensitivity analysis was performed.
Results:
After 5 years, convergent procedure patients averaged 1.10 procedures, with 75% of survivors in sinus rhythm; catheter ablation patients had 1.65 procedures, with 49% in sinus rhythm. Compared to medical management, catheter ablation and the convergent procedure were cost-effective for the lower risk (ICER <$35,000) and medium risk (ICER <$15,000) cohorts. The procedures dominated medical management for the higher risk cohort (lower cost and higher QALYs). The convergent procedure dominated catheter ablation for all risk cohorts. Results were subject to simplifying assumptions and limited by uncertain factors such as long-term maintenance of sinus rhythm after successful procedure and incremental AF-associated event rates for AF patients relative to patients in sinus rhythm. In the absence of clinical trial data, convergent procedure efficacy was estimated with observational evidence. Limitations were addressed with sensitivity analyses and a moderate 5 year time horizon.
Conclusion:
The convergent procedure results in superior maintenance of post-ablation sinus rhythm with fewer repeat ablation procedures compared to catheter ablation, leading to lower cost and higher QALYs after 5 years.
Introduction
An estimated 5.2 million people in the US have been diagnosed with atrial fibrillation (AF), and over one million new cases are added each yearCitation1. By 2030, the prevalence of AF could reach 9.3 to 12.1 million. In addition to decreased quality of life, patients face increased risk of stroke, heart failure, and premature deathCitation2. AF also imposes a significant national cost burden, with the cost of AF and associated complications estimated to be $26 billion in 2010Citation3. Management strategies are needed to ease the heavy burden of AF for patients and societyCitation4.
AF can be categorized as either idiopathic (lone), paroxysmal (intermittent) or continuous (persistent). In this paper, ‘non-paroxysmal’ is used to include the following terms: persistent (AF that does not terminate spontaneously within 7 days of onset), permanent or longstanding AF (continuous AF for greater than 1 year).
Endocardial catheter ablation is an established treatment for restoration of sinus rhythm, which can relieve patient symptoms, reduce morbidity risk, and lead to health care expenditure savingsCitation5–7. Multiyear outcomes of catheter ablation have now been established at a number of centersCitation8–10. In general, freedom from AF falls linearly after approximately 1 year in most studies, with a larger and earlier decline in the non-paroxysmal AF cohorts. Minimally invasive surgical procedures have been developed to improve catheter ablation outcomes, the most studied being the convergent procedure. The closed-chest convergent procedure is a technique that places pericardioscopic, epicardial lesions immediately preceding standard percutaneous catheter ablation. This approach enables pulmonary vein isolation with shortened catheter ablation time, as well as the comprehensive epicardial ablation of the posterior left atrium. Posterior left atrial ablation is important, particularly in patients with non-paroxysmal AF, yet difficult to achieve with catheter ablation aloneCitation11. The convergent procedure is enabled by the Numeris and EPi-Sense Coagulation System.
Studies have estimated the cost-effectiveness of catheter ablation for patients with paroxysmal AFCitation12–14. Studies for the non-paroxysmal AF population and for the convergent procedure are needed. This study develops cost-effectiveness estimates for catheter ablation and the convergent procedure, compared to medical management, for non-paroxysmal AF patients with three levels of risk for AF-associated events. Clinically relevant outcome data such as AF recurrence, AF associated events, and quality-adjusted life-years are also estimated.
Methods
A Markov model was developed to estimate costs, health outcomes, and incremental cost-effectiveness comparing the convergent procedure, catheter ablation, and medical management for patients with symptomatic non-paroxysmal AF refractory to anti-arrhythmic medications. The target population was assumed to be 80% male and age 60 at the start of the simulation. Cohorts of patients were defined to represent patients at three risk levels for stroke, bleed, heart failure, and cardiovascular-related hospitalization and emergency department (ED) visits. Data from the literature was used to populate the model. The outcome measure was quality-adjusted life-years (QALYs). Single-variable sensitivity analysis was used to identify influential variables and test model robustness. A payer perspective was taken, and costs and outcomes were discounted at 3% per year. All costs were in 2013 US dollars.
Model structure and base-case assumptions
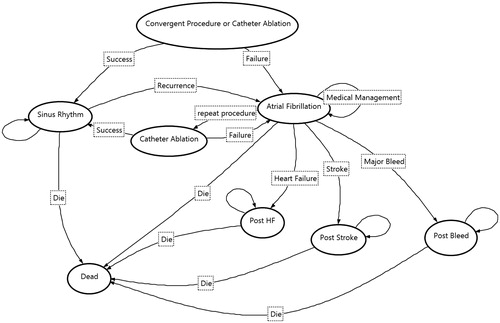
The Markov process for the convergent procedure and catheter ablation had eight states (). Patients underwent the procedure in the first cycle. If the procedure was successful without complications, the patient moved to the Sinus Rhythm state. If the procedure was unsuccessful without complications, the patient had a probabilistic chance for a repeat procedure in the next cycle or moved to the Atrial Fibrillation state. Patients with complications incurred additional cost and possible death. If the patient survived complications and the procedure was successful, he or she moved to the Sinus Rhythm state; otherwise the patient moved to the Atrial Fibrillation state.
In the Sinus Rhythm state, patients survived or died based on general mortality risk. If they survived, they returned to the Sinus Rhythm state in the next cycle or experienced recurrence of AF. If AF recurred, they had a probabilistic chance for a repeat procedure or moved to the Atrial Fibrillation state. In the Sinus Rhythm state, a portion of patients were treated with anti-arrhythmic medications.
The repeat procedure was catheter ablation regardless of the initial procedure. The possibility of repeat procedure was at the time of procedure failure or AF recurrence, with the repeat procedure occurring in the following cycle. If the repeat option was not taken and the patient moved to the AF recurrence arm, no repeat ablations were available for the patient.
In the Atrial Fibrillation state, patients were treated with rate or rhythm control medications, antithrombotic medications, and were exposed to risks for stroke, bleed, heart failure, or hospitalization and ED visit as described for medical management.
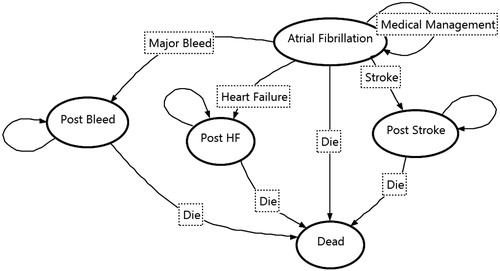
The Markov process for medical management had five states (). Patients were assumed to remain in non-paroxysmal AF and continue treatment with rhythm control or rate control, and anticoagulant medications. During each model cycle, patients were at risk for a cardiovascular (CV) related hospitalization or emergency department (ED) visit; for developing heart failure, stroke, intracranial hemorrhage or major bleed; or death. If patients developed heart failure or experienced a bleed or stroke, they incurred the costs of treating both the event and the related ongoing post-event costs, and a higher risk of death.
Costs included the cost of procedures, medication and management, hospitalization, and AF-associated events. Quality of life was adjusted for procedure, AF, hospitalization, heart failure, bleed, and stroke.
Model inputs
Estimates of procedure efficacy, rates and costs of AF-associated events, and utilities were from the literature. Procedure and medical management costs were based on Medicare National Allowances. Death rates were from National Health Statistics. A summary of base-case inputs is shown in . Additional description of the base-case estimates and data sources is provided in the Supplemental material.
Table 1. Summary of model inputs: rates and costs.
Procedure efficacy, repeat procedures, and AF recurrence
Procedure success was defined as sinus rhythm, on or off anti-arrhythmic medications. Three tiers of procedure efficacy were estimated: the first for quarters one and two post-procedure; the second for quarters three through eight post-procedure; the third for late recurrence of AF in quarters nine and later. All available convergent procedure studies were included, except those reporting previously published results or using a procedure that is no longer current. Catheter ablation studies were included if the patient population was less than 50% paroxysmal. When studies reported success for non-paroxysmal patients separately from paroxysmal patients, the rate for non-paroxysmal patients was used.
Recent catheter ablation studies have reported maintenance of sinus rhythm up to 6 years post-catheter ablation, although evidence past 2 years was limitedCitation8–10. Those studies, along with others of shorter duration, were used to estimate the success rates used in the model up to two years post procedureCitation24–26. Most studies of the convergent procedure had 1 year post-procedure follow-up availableCitation15–19. Four studies provided success rates at 18 or 24 months and were used to estimate the success rate up to 2 yearsCitation20–23. Although longer-term evidence for the convergent procedure success was modest, evidence from catheter ablation suggests that if a procedure remains successful after two quarters, sinus rhythm maintenance continues at a rate with significantly reduced linearized drop-offCitation8–10.
Evidence for long-term recurrence of AF in patients successfully restored to sinus rhythm after catheter ablation and convergent procedures was limited. In a 2006 cost-effectiveness study, Chan et al. assumed an annual recurrence rate of 2% after catheter ablationCitation12. In a more recent cost-effectiveness study, McKenna et al. assumed an annual rate of 3.35% after catheter ablationCitation14. Long term recurrence rates of 6.4% and 7.6% per year after catheter ablation have also been reportedCitation51,Citation52. Without compelling evidence for recurrent AF after catheter ablation and no evidence after the convergent procedure, we assumed an annual recurrence rate of 4% for patients who remained in sinus rhythm 2 years after a procedure.
Evidence from catheter ablation studies suggests that patients become less likely to accept the second, third, and fourth proceduresCitation8–10,Citation24. We assumed that 70% of patients would accept the second procedure, 40% the third, and 35% the fourth. Although limited, data suggested that patients with recurrent AF after the convergent procedure were less likely to have a repeat procedure. We assumed that 30% of patients would accept a repeat procedure. Repeat procedures after initial catheter ablation were assumed to have the same success rates as initial procedures. Repeat catheter ablation after initial convergent procedure was assumed to have 90% success 1 year post-ablation.
Procedure complications were estimated by re-hospitalizations within 30 days of the initial procedure. Re-hospitalizations represent adverse events or new arrhythmias that were generated by the initial procedure. Two large studies of catheter ablation outcomes provided estimates that were used for both proceduresCitation27,Citation28.
AF-associated events
Patients in AF have higher rates of AF-associated stroke, bleed, heart failure, and CV-related hospitalization and ED visits. Incremental event rates for AF patients compared to patients in sinus rhythm were used to estimate incremental costs for patients with recurrent AF or those in medical management. Three cohorts of patients were defined as those with lower, medium, or higher event rate risk, corresponding to CHADS2 scores of 0, 1, and 2 or aboveCitation29.
Incremental rates of events were estimated from various sources. Stroke rates were estimated for AF patients without anticoagulation therapy, adjusted by their relative risk compared to non-AF patientsCitation29,Citation30. We assumed that 50% of patients in the AF state would receive anticoagulation therapy, which would reduce their risk of stroke by 50%Citation31,Citation53,Citation54. Bleed rates combined rates of major bleed and intracranial hemorrhageCitation31–33. Heart failure rates were for new onset or worsening of existing heart failure. The rate of CV-related hospitalizations included stroke, bleed, and heart failure events. To avoid double-counting, the hospitalization rate used in the model was reduced by the total of those events. ED visits that did not result in hospitalization were also modeled.
Medication management
Twenty-one percent (21%) of convergent procedure patients and 16% of catheter ablation patients were assumed to continue with anti-arrhythmic medications after a successful procedureCitation10,Citation16,Citation19,Citation21–23,Citation25,Citation26. Thirty-five percent (35%) of patients in the AF state were assumed to receive anti-arrhythmic medications and 65% received rate control medicationsCitation55,Citation56. Patients in a post-event state were assumed to continue rate control medication.
Costs
Costs of procedures and medical management were based on 2013 Medicare National Allowances. Costs of AF-associated events were estimated from the literature and adjusted to 2013 US dollars. Procedure costs included pre-procedure tests, hospital and physician reimbursement. Medical management costs included cost of medication and periodic routine management office visit costs. Costs for stroke, bleed, and heart failure were estimated for the quarter of the event and follow-up in the post-event state.
Quality-adjusted life-years
Utilities were estimated for patients in sinus rhythm, AF, AF-associated event, and post-event states. Estimates for sinus rhythm and AF states were based on Gula et al. for patients with symptomatic non-paroxysmal AF refractory to anti-arrhythmic medicationsCitation49. Following the Institute for Clinical and Economic Review and Chan et al., we applied decrements to estimate utility in the quarter of an AF-associated event and post-eventCitation12,Citation50. Post-event utility decrements were applied until death. Utility during a procedure, heart failure event, or CV hospitalization was assumed to be the same as utility during the AF state.
Analysis
All analyses were performed using TreeAge Pro Suite 2013 (TreeAge Software, Williamstown, MA, USA). We performed a Monte Carlo simulation of 10,000 patients for each of the three risk cohorts. The simulation had a 5 year time horizon, in quarterly cycles. The quarterly cycle was long enough to be clinically meaningful and short enough to capture known patterns of AF-recurrence after a procedure. Transitions occurred at the start of each cycle. Each simulated patient accumulated costs and health outcomes, which were discounted at 3% per year. Results were presented as mean costs, QALYs, and incremental cost–effectiveness ratios (ICERS). Single-variable sensitivity analysis was performed for the medium risk cohort, unless otherwise described. In sensitivity analyses, procedure efficacies at the lower bound of the 95% confidence interval were tested. To recognize the uncertainty of long-term AF-recurrence rates, rates of 8% per year and 16% per year were tested. Using the lower and medium risk cohort rates of hospitalization and ED visits, we tested the possibility of no difference of AF-associated event rates between patients in sinus rhythm and those in AF. Higher procedure costs (+25%) and lower AF-associated event costs (-25%) were each tested. To estimate the influence of utility values on outcomes, several utility scenarios were tested: (1) a 0.10 decrement for patients in AF compared to patients in sinus rhythm, (2) a 0.065 decrement for patients in AF compared to patients in sinus rhythm, (3) a post-stroke decrement of 0.02 based on an assumption of no severe strokes, and (4) an assumption of no post-event decrement after stroke, bleed, and heart failure. Annual cumulative costs were estimated over a 10 year time horizon to evaluate cost patterns for the three treatment strategies.
Results
Base-case analysis
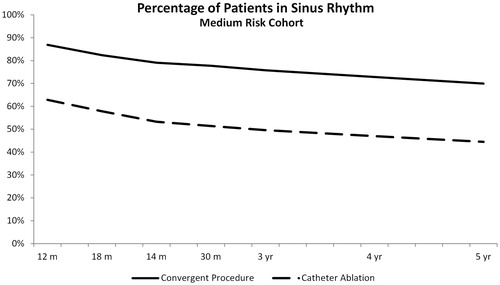
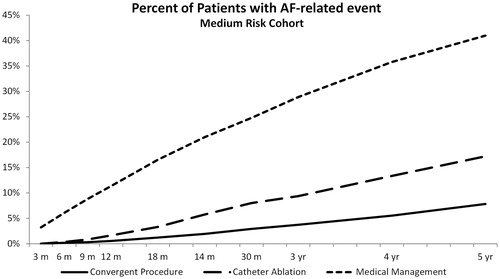
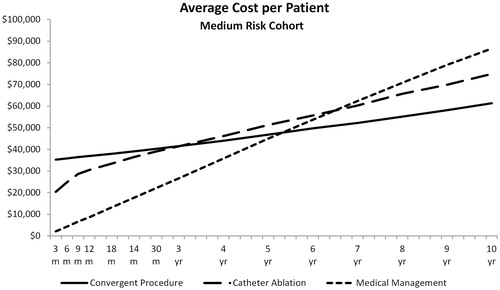
After 5 years, convergent procedure patients averaged 1.10 procedures, with 75% of survivors remaining in sinus rhythm. Most (90%) patients had only one procedure, 9% had two, and less than 1% had three procedures. Catheter ablation patients averaged 1.65 procedures, with 49% ending in sinus rhythm. About half (50%) of catheter ablation patients had only one procedure, 36% had two, 10% had three, and about 3% received four procedures. For both procedures, the percentage of patients in sinus rhythm declined steadily as illustrated for the medium risk cohort (). For the lower risk cohort, total average cost was $44,231 for convergent procedure patients, $44,588 for catheter ablation, and $28,779 for medical management (). Patients in medical management incurred an average $5900 per life year in costs associated with AF. The convergent procedure (ICER = $20,640) and catheter ablation (ICER = $30,596) were cost-effective compared to medical management. The convergent procedure and catheter ablation procedures had similar average cost per patient, but the convergent procedure produced higher QALYs.
Table 2. Quality-adjusted life-years, cost, and incremental cost–effectiveness ratios.
For the medium risk cohort, total average cost was $46,795 for convergent procedure patients, $51,270 for catheter ablation, and $44,970 for medical management (). Patients in medical management incurred $9500 per life year in costs associated with AF. Compared to medical management, both procedures were cost-effective. The convergent procedure had lower cost and higher QALYs, therefore it dominated catheter ablation. For the higher risk cohort, total average cost was $49,817 for Convergent Procedure patients, $58,154 for catheter ablation, and $64,490 for medical management. Patients in medical management incurred $13,600 per life year in costs associated with AF. The procedures dominated medical management, and the convergent procedure dominated catheter ablation.
For all risk cohorts, convergent procedure patients had 80% fewer AF-associated events, including hospitalizations, than medical management patients and catheter ablation patients had 60% fewer AF-associated events than medical management patients. The percentage of patients ending in the post-stroke, post-bleed, or post-HF state at every cycle of the simulation was lowest after the convergent procedure ().
Sensitivity analysis
In all scenarios, the convergent procedure was cost-effective (ICER <$30,000) compared to medical management, and dominated catheter ablation in all but one scenario (). Catheter ablation ICERs relative to medical management were 1.5 to 5.0 times those of the convergent procedure.
In most scenarios, the average AF-associated cost for patients in medical management was $9500 per life year. Costs were lower when the assumed treatment costs were lower ($7100 per life year), and when the incremental rate of strokes, bleeds, and heart failure was assumed to be zero with medium risk hospitalization rate ($7300) or lower risk hospitalization rate ($4600). Even at the lowest cost assumption for medical management patients, the procedures were cost-effective at generally accepted levels.
Results of utility value sensitivity testing showed little impact from post-event utility decrement changes and no change in overall conclusions from the base-case scenario. In all cases, the convergent procedure ICER compared to medical management was under $6000 per QALY and the catheter ablation ICER compared to medical management was $12,200 to $31,500 per QALY. As expected, the greatest impact was an AF decrement of 0.065, where the convergent procedure and catheter ablation ICERs neared $6000 and $31,500, respectively. That decrement had been used in previous cost-effectiveness studies, but because it represented the change from baseline to 12 month follow-up after catheter ablation without regard to sinus rhythm in patients with paroxysmal and persistent patients, it was not an appropriate base-case assumption for our modelCitation13,Citation50.
The 10 year time horizon projection showed that the average cost per patient with medical management approached the cost of the procedures in years six and seven, and exceeded procedure cost thereafter (). The cost of catheter ablation exceeded the cost of the convergent procedure after year three.
Discussion
We developed a Markov micro-simulation model to estimate the cost-effectiveness of catheter ablation and the convergent procedure compared to medical management for patients with non-paroxysmal AF. Successful procedures restore sinus rhythm and reduce the risk of AF-associated events. However, catheter ablation has modest success and often requires repeat procedures. The convergent procedure has higher success than catheter ablation; however, the cost per procedure is also higher. The cost–effectiveness model evaluated the average cost per patient over 5 years, recognizing procedure costs and costs for AF-associated events.
Our simulated procedure success and repeat procedure rates were similar to what has been reported for catheter ablation proceduresCitation8–10,Citation25,Citation26. After 5 years, about half of patients remained in sinus rhythm and patients averaged 1.65 procedures.
Our simulated costs of low, medium and high risk patients compared favorably with those reported in the literature. The average annual patient cost was $5900, $9500, and $13,600 for medical management patients. The costs included medical management and event and follow-up care for stroke, bleed, heart failure, and CV-associated hospitalizations and ED visits. Several studies have estimated the cost burden of AF in the United States. Wu et al. compared the costs of AF patients to matched controls and estimated the annual incremental direct health care costs in a privately insured population to be $12,349 (2002 US$)Citation57. The average age of the AF cohort was 55 and 69% were male. Nearly 50% of AF patients had at least one inpatient hospital claim and nearly 40% had at least one ED visit during the 1 year follow-up. In a more recent study, Kim et al. compared a cohort of AF patients with matched controls. They estimated the annual incremental cost of AF patients as $8705, 60% from inpatient costs (2008 US$)Citation3. The majority (75%) of patients were Medicare beneficiaries with an average age of 71 years.
Amin et al. estimated incremental utilization and costs for AF patients with additional risk factors compared to non-AF controls using 2007 to 2008 claims data for Medicare beneficiaries with Medicare Supplement insurance. Compared to controls, the AF patients had higher CV-related health care costs of $9213, 76% from inpatient hospitalizationsCitation39. The AF patients averaged 0.51 more CV-related hospitalizations per patient per year with additional 2.77 days length of stay compared to controls. Patients in the study were average age 80 and 51% male. Lee et al. analyzed 2002 to 2004 Medicare databases to estimate the incremental cost of AF patients compared to matched controls. The patients were older, with 69% aged 75 or over, and 46% male. After adjusting for demographics, co-morbidities, and baseline health care cost, the incremental AF total treatment costs were $14,199Citation34. Compared to controls, a significantly higher percentage of the AF patients had three or more hospitalizations, outpatient visits, and physician visits.
Most studies of incremental AF costs included paroxysmal and non-paroxysmal patients and reported sizable cost burden to payers. Our simulated cohorts were within the range of reported cost for patients with AF. In sensitivity analysis, we tested incremental costs of $7300 per patient in medical management. Using that modest estimate, both procedures were cost-effective (ICER <$30,000) and the convergent procedure dominated catheter ablation. However, for the lowest cost AF patients, with incremental costs of $4600 per year, the ICER for the convergent procedure was over $30,000 and the ICER for catheter ablation approached $50,000.
Previous cost–effectiveness studies have compared catheter ablation to anti-arrhythmic medications, usually for paroxysmal patients. The higher initial cost of the procedure was offset by savings by the avoidance of stroke and medication-associated hospitalization. Our study expands on previous work by incorporating savings from avoided bleeds, heart failures, and CV-related hospitalizations, which have been associated with AF. In addition, we compare two procedures to medical management for patients with non-paroxysmal AF at three levels of risk for AF-associated events.
Although the cost of the convergent procedure is higher than catheter ablation, the convergent procedure was more cost-effective, especially for the medium and higher risk cohorts. In those cohorts, the higher initial cost was offset by savings from avoided repeat ablation procedures and AF-associated events. Convergent procedure patients were more frequently restored to sinus rhythm and had fewer recurrences within the first 2 years post-procedure, therefore reducing their risk of AF-associated events. The convergent procedure is more successful at restoring sinus rhythm in part because it produces a more complete posterior left atrial ablationCitation22.
Our results are subject to several limitations. As with all modeling studies, several simplifying assumptions were made. In particular, the long term maintenance of sinus rhythm after a successful procedure is unknown. We used the most recent and longest follow-up studies of catheter ablation efficacy, but results after 2 years are uncertain. To address the longer term, we tested AF recurrence rates in sensitivity analysis. We attempted to measure the incremental rates of AF-associated events for AF patients relative to patients in sinus rhythm; however, they are estimates. Our three risk cohorts provide a sensitivity analysis of those incremental rates. Evidence that restoration to sinus rhythm after ablation reduces utilization has been provided by Piccini et al., who reported that catheter ablation reduced the rate of CV-related hospitalization compared to medical management of AF (14 vs. 93 per 100 person-years)Citation58. In a working population, Kleinman et al. found AF patients had lower costs after ablation compared to AF patients that didn’t have ablationCitation59. However, our incremental rate for bleed may be overstated as newer anticoagulation medications which reduce the risk of bleed and stroke become more commonly used. The methods used during catheter ablation vary and the estimates used may not be representative of all centers. Finally, our rates of the convergent procedure efficacy were from currently available observational evidence, which allowed us to present interim cost–effectiveness results in the absence of clinical trial data. A clinical trial of the convergent procedure and catheter ablation is underway, and those results will provide a more reliable conclusion. In addition, the rates of procedure efficacy used in our study may not be representative of procedures performed outside of academic centers, where surgeons and electrophysiologists are highly experienced.
Conclusion
Non-paroxysmal AF patients present with highly variable states of complications and comorbidities. The emergence of the convergent procedure presents cardiothoracic surgeons and electrophysiologists with a new combined technique that has demonstrated successful clinical outcomes in these complex cases. This economic analysis demonstrates that the initial higher costs associated with the convergent procedure can be justified in non-paroxysmal AF patients when compared to medical management or catheter ablation over a 5 year time horizon. This is due to the superior maintenance of post-ablation sinus rhythm, with fewer repeat ablations, and higher quality of life metrics.
Supplementary material available online at
http://informahealthcare.com/doi/abs/10.3111/13696998.2014.911185
Supplementary Material
Download PDF (110.4 KB)Transparency
Declaration of funding
This study was funded in part by nContact Inc., Morrisville, NC, USA.
Declaration of financial/other relationships
E.J.B., L.H.A., and M.S.M. have disclosed that they have consulting arrangements with nContact Inc. K.C.C. has disclosed that he has teaching honoraria and research grants with nContact Inc. D.C.K. has disclosed that he has no significant relationships with or financial interests in any commercial companies related to this study or article.
JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Notes
*Numeris and EPi-Sense are trade names of nContact Inc., Morrisville, NC, USA
References
- Colilla S, Crow A, Petkun W, et al. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. Am J Cardiol 2013;112:1142-7
- Stewart S, Hart CL, Hole DJ, et al. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med 2002;113:359-64
- Kim MH, Johnston SS, Chu B-C, et al. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes 2011;4:313-20
- Reynolds MR, Essebag V. Economic burden of atrial fibrillation: implications for intervention. Am J Pharm Benefits 2012;4:58-65
- Goldberg A, Menen M, Mickelsen S, et al. Atrial fibrillation ablation leads to long-term improvement of quality of life and reduced utilization of healthcare resources. J Interv Card Electrophysiol Int J Arrhythm Pacing 2003;8:59-64
- Ladapo JA, David G, Gunnarsson CL, et al. Healthcare utilization and expenditures in patients with atrial fibrillation treated with catheter ablation. J Cardiovasc Electrophysiol 2012;23:1-8
- Bunch TJ, May HT, Bair TL, et al. Atrial fibrillation ablation patients have long-term stroke rates similar to patients without atrial fibrillation regardless of CHADS2 score. Heart Rhythm Off J Heart Rhythm Soc 2013;10:1272-7
- Chao T-F, Tsao H-M, Lin Y-J, et al. Clinical outcome of catheter ablation in patients with nonparoxysmal atrial fibrillation: results of 3-year follow-up. Circ Arrhythm Electrophysiol 2012;5:514-20
- Sorgente A, Tung P, Wylie J, et al. Six year follow-up after catheter ablation of atrial fibrillation: a palliation more than a true cure. Am J Cardiol 2012;109:1179-86
- Tilz RR, Rillig A, Thum A-M, et al. Catheter ablation of long-standing persistent atrial fibrillation: 5-year outcomes of the Hamburg Sequential Ablation Strategy. J Am Coll Cardiol 2012;60:1921-9
- Chilukuri K, Scherr D, Dalal D, et al. Conventional pulmonary vein isolation compared with the ‘box isolation’ method: a randomized clinical trial. J Interv Card Electrophysiol Int J Arrhythm Pacing 2011;32:137-46
- Chan PS, Vijan S, Morady F, et al. Cost-effectiveness of radiofrequency catheter ablation for atrial fibrillation. J Am Coll Cardiol 2006;47:2513-20
- Reynolds MR, Zimetbaum P, Josephson ME, et al. Cost-effectiveness of radiofrequency catheter ablation compared with anti-arrhythmic drug therapy for paroxysmal atrial fibrillation. Circ Arrhythm Electrophysiol 2009;2:362-9
- McKenna C, Palmer S, Rodgers M, et al. Cost-effectiveness of radiofrequency catheter ablation for the treatment of atrial fibrillation in the United Kingdom. Heart Br Card Soc 2009;95:542-9
- Civello KC, Smith CA, Boedefeld W. Combined endocardial and epicardial ablation for symptomatic atrial fibrillation: single center experience in 100+ consecutive patients. J Innov Card Rhythm Manag 2013;4:1367-73
- Geršak B, Zembala MO, Müller D, et al. European experience of the convergent atrial fibrillation procedure: multicenter outcomes in consecutive patients. J Thorac Cardiovasc Surg 2013;147:1411-6
- Robinson, MC. Maximizing ablation, limiting invasiveness, and being realistic about atrial fibrillation: the convergent hybrid ablation procedure for advanced AF. EP Lab Dig 2013;13:34-6
- Thosani AJ, Gerczuk P, Liu E, et al. Closed chest convergent epicardial–endocardial ablation of non-paroxysmal atrial fibrillation – a case series and literature review. Arrhythmia Electrophysiol Rev 2013;2:65-8
- Toplisek J, Pernat A, Gersak B, et al. Effect of convergent procedure on left atrial size & ventricular function in patients with persistent atrial fibrillation. J Am Coll Cardiol 2012;59(13 Suppl 1):E594
- Golden K, Olson J, Walts P, et al. Clinical outcomes of a new epicardial/endocardial ablation procedure (convergent) for the treatment of atrial fibrillation. Presentation PO04-67 Heart Rhythm Society Boston. Heart Rhythm 2012;9(5 Suppl):S292-S328
- Gersak B, Pernat A, Robic B, et al. Low rate of atrial fibrillation recurrence verified by implantable loop recorder monitoring following a convergent epicardial and endocardial ablation of atrial fibrillation. J Cardiovasc Electrophysiol 2012;23:1059-66
- Gilligan DM, Joyner CA, Bundy GM. Multidisciplinary collaboration for the treatment of atrial fibrillation: convergent procedure outcomes from a single center. J Innov Card Rhythm Manag 2013;4:1396-403
- Zembala M, Filipiak K, Kowalski O, et al. Minimally invasive hybrid ablation procedure for the treatment of persistent atrial fibrillation: one year results. Kardiol Pol 2012;70:819-28
- Dixit S, Marchlinski FE, Lin D, et al. Randomized ablation strategies for the treatment of persistent atrial fibrillation: RASTA study. Circ Arrhythm Electrophysiol 2012;5:287-94
- Miyazaki S, Taniguchi H, Komatsu Y, et al. Sequential biatrial linear defragmentation approach for persistent atrial fibrillation. Heart Rhythm Off J Heart Rhythm Soc 2013;10:338-46
- Nademanee K, Schwab MC, Kosar EM, et al. Clinical outcomes of catheter substrate ablation for high-risk patients with atrial fibrillation. J Am Coll Cardiol 2008;51:843-9
- Piccini JP, Sinner MF, Greiner MA, et al. Outcomes of Medicare beneficiaries undergoing catheter ablation for atrial fibrillation. Circulation 2012;126:2200-7
- Shah RU, Freeman JV, Shilane D, et al. Procedural complications, rehospitalizations, and repeat procedures after catheter ablation for atrial fibrillation. J Am Coll Cardiol 2012;59:143-9
- Gage BFWA. Validation of clinical classification schemes for predicting stroke: results from the national registry of atrial fibrillation. JAMA 2001;285:2864-70
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke J Cereb Circ 1991;22:983-8
- Mercaldi CJ, Ciarametaro M, Hahn B, et al. Cost efficiency of anticoagulation with warfarin to prevent stroke in Medicare beneficiaries with nonvalvular atrial fibrillation. Stroke J Cereb Circ 2011;42:112-18
- Meiltz A, Zimmermann M, Urban P, et al, Association of Cardiologists of the Canton of Geneva. Atrial fibrillation management by practice cardiologists: a prospective survey on the adherence to guidelines in the real world. Europace 2008;10:674-80
- Nieuwlaat R, Prins MH, Le Heuzey J-Y, et al. Prognosis, disease progression, and treatment of atrial fibrillation patients during 1 year: follow-up of the Euro Heart Survey on atrial fibrillation. Eur Heart J 2008;29:1181-9
- Lee WC, Lamas GA, Balu S, et al. Direct treatment cost of atrial fibrillation in the elderly American population: a Medicare perspective. J Med Econ 2008;11:281-98
- Krahn AD, Manfreda J, Tate RB, et al. The natural history of atrial fibrillation: incidence, risk factors, and prognosis in the Manitoba Follow-Up Study. Am J Med 1995;98:476-84
- Wang TJ, Larson MG, Levy D, et al. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation 2003;107:2920-5
- Le Heuzey J-Y, Paziaud O, Piot O, et al. Cost of care distribution in atrial fibrillation patients: the COCAF study. Am Heart J 2004;147:121-6
- Older Americans & Cardiovascular Diseases. American Heart Association, American Stroke Association, 2013. Available at: http://www.heart.org/idc/groups/heart-public/@wcm/@sop/@smd/documents/downloadable/ucm_319574.pdf [Last accessed 21 July 2013]
- Amin AN, Jhaveri M, Lin J. Incremental cost burden to US healthcare payers of atrial fibrillation/atrial flutter patients with additional risk factors. Adv Ther 2011;28:907-26
- Reynolds MR, Essebag V, Zimetbaum P, et al. Healthcare resource utilization and costs associated with recurrent episodes of atrial fibrillation: the FRACTAL registry. J Cardiovasc Electrophysiol 2007;18:628-33
- Amin AN, Jhaveri M, Lin J. Hospital readmissions in US atrial fibrillation patients: occurrence and costs. Am J Ther 2013;20:143-50
- Casciano JP, Dotiwala ZJ, Martin BC, et al. The costs of warfarin underuse and nonadherence in patients with atrial fibrillation: a commercial insurer perspective. J Manag Care Pharm 2013;19:302-16
- Poulin F, Khairy P, Roy D, et al. Atrial fibrillation and congestive heart failure: a cost analysis of rhythm-control vs rate-control strategies. Can J Cardiol 2013;29:1256-62
- Torp-Pedersen C, Crijns HJGM, Gaudin C, et al. Impact of dronedarone on hospitalization burden in patients with atrial fibrillation: results from the ATHENA study. Europace 2011;13:1118-26
- Mercaldi CJ, Siu K, Sander SD, et al. Long-term costs of ischemic stroke and major bleeding events among Medicare patients with nonvalvular atrial fibrillation. Cardiol Res Pract 2012;2012:645469
- Chen LM, Jha AK, Guterman S, et al. Hospital cost of care, quality of care, and readmission rates: penny wise and pound foolish? Arch Intern Med 2010;170:340-6
- Dunlay SM, Shah ND, Shi Q, et al. Lifetime costs of medical care after heart failure diagnosis. Circ Cardiovasc Qual Outcomes 2011;4:68-75
- Coyne KS, Paramore C, Grandy S, et al. Assessing the direct costs of treating nonvalvular atrial fibrillation in the United States. Value Health J Int Soc Pharmacoeconomics Outcomes Res 2006;9:348-56
- Gula LJ, Massel D, Redfearn DP, et al. Impact of routine transoesophageal echocardiography on safety, outcomes, and cost of pulmonary vein ablation: inferences drawn from a decision analysis model. Europace 2010;12:1550-7
- Ollendorf DA, Silverstein MD, Bobo T, Pearson SD. Rhythm Control and Stroke Prevention Strategies for Patients with Atrial Fibrillation. 2010. Available at: http://www.icer-review.org/index.php/Reports/rhythm-control-and-sroke-prevention-strategies-for-patients-with-atrial-fibrillation-final-appraisal.html [Last accessed 12 June 2013]
- Gaztañaga L, Frankel DS, Kohari M, et al. Time to recurrence of atrial fibrillation influences outcome following catheter ablation. Heart Rhythm Off J Heart Rhythm Soc 2013;10:2-9
- Sotomi Y, Inoue K, Ito N, et al. Incidence and risk factors for very late recurrence of atrial fibrillation after radiofrequency catheter ablation. Europace 2013;15:1581-6
- Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med 1994;154:1449-57
- Kannel W, Benjamin E. Final draft status of the epidemiology of atrial fibrillation. Med Clin North Am 2008;92:17-40, ix
- Camm AJ, Breithardt G, Crijns H, et al. Real-life observations of clinical outcomes with rhythm- and rate-control therapies for atrial fibrillation: RECORDAF (Registry on Cardiac Rhythm Disorders Assessing the Control of Atrial Fibrillation). J Am Coll Cardiol 2011;58:493-501
- Steinberg BA, Holmes DN, Ezekowitz MD, et al. Rate versus rhythm control for management of atrial fibrillation in clinical practice: results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) registry. Am Heart J 2013;165:622-9
- Wu EQ, Birnbaum HG, Mareva M, et al. Economic burden and co-morbidities of atrial fibrillation in a privately insured population. Curr Med Res Opin 2005;21:1693-9
- Piccini JP, Lopes RD, Kong MH, et al. Pulmonary vein isolation for the maintenance of sinus rhythm in patients with atrial fibrillation a meta-analysis of randomized, controlled trials. Circ Arrhythm Electrophysiol 2009;2:626-33
- Kleinman NL, Rohrbacker NJ, White SA, et al. Economic impact to employers of treatment options for cardiac arrhythmias in the US health system. J Occup Environ Med Am Coll Occup Environ Med 2011;53:405-14