Abstract
Introduction:
Diabetic peripheral neuropathy (DPN) is a debilitating complication of diabetes and accounts for significant morbidity by pre-disposing the foot to ulceration and lower extremity amputation. Using a large US commercial claims database, this study analyzes the drug class usage and co-morbidities associated with DPN as well as estimates the associated economic burden.
Methods:
Patients older than 18 and diagnosed with DPN were followed longitudinally for 2 years pre- and post-diagnosis date. Patients were analyzed for age, gender, hospital visits, ER and doctor’s office visits, pharmacy claims, co-morbidities, and drug classes prescribed pre- and post-DPN diagnosis. The economic impact post-diagnosis of DPN was compared to the patients’ pre-diagnosis resource use.
Results:
In total, 10,982 incident DPN patients were identified, with a median age of 61 years, and an equal gender distribution. Post-DPN diagnosis, there was a 20% increase in the number of patients visiting hospitals and a 46% increase in the number of visits to hospitals. Further, there was a 46% increase in the annual cost per patient associated with visits to the hospitals, emergency room (ER), doctor’s office, and pharmacy claims. As per the analysis presented in this study, increase in the number of visits, cost per visit, and number of patients visiting hospitals, ER and doctor’s offices added up to a 46% increase in aggregated cost associated with Medical Resource Utilization (MRU) owing to DPN, with the highest increase (60%) in costs associated with hospitalization of patients with DPN.
Conclusion:
This study highlights the high economic burden associated with DPN. The results indicate that resource use significantly increases post-diagnosis of DPN, which leads to an increase in costs for payers. A noticeable proportion of patients with DPN had a pain co-diagnosis signifying the need for treatments that can effectively manage painful DPN.
Introduction
Diabetic peripheral neuropathy, or peripheral neuropathic pain in patients suffering from diabetes, is defined by the International Association for the Study of Pain as ‘pain arising as a direct consequence of abnormalities in the peripheral somatosensory system in people with diabetes’ (Ref. 1: p. 1630, Ref. 2: p. 2286).Citation1,Citation2 Peripheral neuropathy is the most common co-morbidity associated with diabetes mellitusCitation3. Up to 50% of patients suffering from diabetes have peripheral neuropathy associated with the conditionCitation4–10. DPN affects the lower limbs first and then moves up to the upper limbs in a ‘stocking and glove’ pattern of distributionCitation9. In some patients, occurrence of hypoesthesia is symptomatic of DPN; however, in half the cases, DPN is asymptomatic and such patients are at risk of injury to their feet and developing foot ulcersCitation4,Citation11, making DPN a major factor associated with foot ulceration, amputation, and deathCitation4,Citation5,Citation12,Citation13. In symptomatic patients, symptoms of DPN can be positive (prickling, pain) or negative (loss of sensation and strength)Citation14,Citation15.
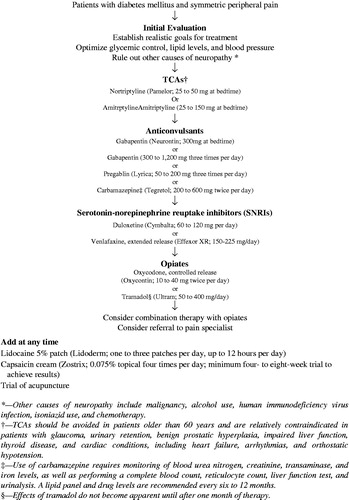
The American Academy of Family Physicians algorithm for management of DPN is shown in Citation16. On top of analgesic treatment and treatments for management of diabetes, therapies for DPN management include tri-cyclic antidepressants (TCAs), serotonin norepinephrine re-uptake inhibitors (SNRIs) such as duloxetine, and anticonvulsants such as pregabalin and gabapentin, the use of which in painful DPN is supported by clinical evidenceCitation17,Citation18. Although there are a number of treatment options available for patients with symptomatic DPN, pain management is often inadequateCitation8, either due to lack of efficacy or due to adverse events associated with the use of such medications, the latter leading to curtailment of dose and, thereby, limiting their effectiveness.
Figure 1. Algorithm for management of symptomatic DPNCitation16. Reproduced from Lindsay TJ, et al. Treating diabetic peripheral neuropathic pain. American Family Physician 2010;82(2):151–158, with permission of the American Academy of Family Physicians.
Untreated or under-treated chronic painful DPN has been shown to have a debilitating impact on quality-of-lifeCitation8,Citation19,Citation20, as it results in sleep disturbance, anxiety, and depressionCitation8,Citation21–24. Gore et al.Citation8 assessed the burden associated with DPN and published a study based on patients with DPN recruited by community-based physicians. In this study, patients with DPN were found to be suffering from co-morbidities such as depression (27.8%), anxiety (26.7%), and peripheral vascular disease (24.3%), at rates greater than the normal population (National Comorbidity Survey Replication study reported 12 month period prevalence of any mood disorder including depression at 9.5%, and any anxiety at 18.1%, while Hiatt et al.Citation25 have reported peripheral arterial disease to be affecting 12–14% of the general population). Additionally, other co-morbidities such as microvascular complications of diabetes including retinopathy (13.7%) and nephropathy (17.3%), and chronic musculoskeletal pain conditions such as osteoarthritis (33.7%) and nociceptive low back pain (26.7%) were found to be common among patients with DPN, along with other chronic neuropathic pain conditions such as carpal tunnel syndrome (13.7%) and low back pain with neuropathic involvement (13.3%).
These co-morbidities associated with DPN, along with polypharmacy and medical resource utilization, generate a considerable economic burden. Annual cost associated with DPN in the US alone was estimated to be $10.3 billion in 2003Citation4. Direct medical costs associated with patients with DPN are 5-times higher than the for patients suffering from diabetes mellitus aloneCitation10, and DPN contributes 27% to direct medical cost of diabetesCitation4.
The objective of this study was to use real world data to characterize patients with DPN, specifically their demographics, co-morbidities, and treatment patterns, and define medical resource utilization (MRU) before and after diagnosis of DPN, and, thus, contribute to existing literature by confirming and quantifying the unmet need and high burden associated with DPN.
Methods
Data source
This retrospective study is based on a large US commercial database, the LifeLink (formerly PharMetrics) Health Plan Claims Database (IMS, Inc., Watertown, MA). The LifeLink database contains adjudicated medical and pharmaceutical claims data from more than 98 managed care organizations throughout the US (Midwest 34%, Northeast 22%, South 29%, West 15%). The database consists of more than 61 million patients and ∼16 million covered lives per year and includes information on inpatient and outpatient diagnoses (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] format) and procedures (Current Procedure Terminology, 4th Edition and Healthcare Common Procedural Coding System formats), as well as demographic variables, provider specialty, prescription records, National Drug Code numbers, days’ supply of prescriptions, and quantity dispensed of prescriptions. The database also provides costs of Medical Services such as hospitalization, emergency room (ER) visits, physician visits, procedures, home care, and medical testsCitation26.
Study sample
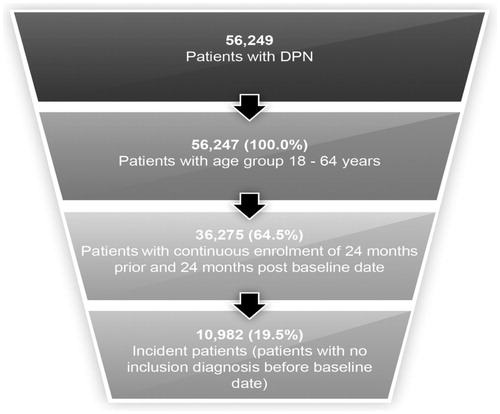
All patients with one or more healthcare encounters with an associated diagnosis of DPN (ICD-9-CM code 250.6x and 357.2) starting January 1, 2009 through December 31, 2009 were identified. A patient’s first DPN diagnosis in 2009 was used as the baseline date (‘Baseline Date’) for each patient. Each patient was then historically evaluated to check for any previous diagnosis of DPN, for at least a period of 2 years, or where data was available for longer, for the entire history of that patient. Patients with no prior diagnosis of DPN were termed ‘incident DPN’ patients. Additional eligibility conditions that were considered before patients were included in the study were that the year of birth for the patient should have been 1992 or earlier (at least 18 years old), and that the patient had continuous enrolment of at least 24 months prior and 24 months post-baseline date (n = 10,982, ).
Pain co-morbidities and medical resource utilization (MRU)
Pain co-morbidities, specifically post-herpetic neuralgia, back and neck pain, and osteoarthritis, along with co-morbidities associated with pain such as depression, sleep disorder, and other relevant pain co-morbidities (including atypical facial pain, phantom limb pain, trigeminal neuralgia, reflex sympathetic dystrophy, nerve root and plexus disorders, other disorders of soft tissues, and inflammatory and toxic neuropathy) were analyzed at the patient level to determine if patients after a diagnosis of DPN had a greater occurrence of these co-morbidities.
Analyses were also conducted to examine MRU both in terms of costs (on the basis of the ‘Allowed’ field in the LifeLink data) and number of visits, including hospitalizations, ER visits, office visits and prescription filling, to determine whether DPN diagnosis was associated with greater healthcare utilization and costs. Hospital, ER, and office visit costs and pharmacy costs were added to derive and compare total costs associated with incident patients pre- and post-DPN diagnosis. Percentage (%) class possession days for a drug was calculated as number of days a drug was prescribed out of 730 study days (2 years) pre- and post-DPN diagnosis.
Statistical analysis
The t-test (two-tailed) was used to analyze the difference in parameters before and after being diagnosed with DPN. The parameters that were compared are mean occurrences of co-morbidities, cost per patient, cost per visit, and number of visits per patient across different MRU categories. The Z-test was used to compare occurrence of different co-morbidities and drug/drug class usage, between pre- and post-DPN diagnosis. The level of significance was fixed at 5%. The Bonferroni correction was applied to adjust for multiple comparisons and only values less than 0.00156 (p < 0.05/n, n = 32) were considered statistically significant
Results
Characteristics of patients with DPN
The included study sample of 10,982 patients () comprised similar proportions of males (49.7%) and females (50.3%). Their mean age was 62 years (median 61 years), with the mean age of male patients being 62 years (median = 61 years) and female patients 61 years (median age = 60 years). While 54.7% of these incident patients were between 45–64 years old, 27.9% were between 65–80 years old (). Out of 10,982 incident patients, only 57.2% of patients were being treated with any one of the following classes: opioids, anti-convulsants, anti-depressants, and NSAIDs in the baseline month (the calendar month of the Baseline Date), which went up to 68% over the 2-year follow-up period post-DPN diagnosis.
Table 1. Characteristics of incident patients with DPN included in the analysis.
Medical resource utilization (MRU) and associated costs
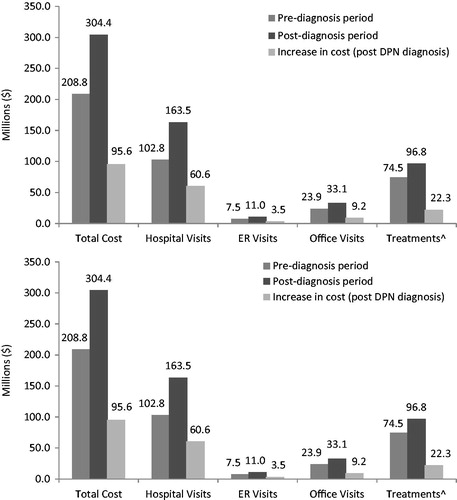
The number of patients visiting the hospitals and ER was 20% and 8% higher, respectively, after their DPN diagnosis compared to pre-diagnosis (). A similar trend was seen in office visits and pharmacy claims. The number of office visits was 24% higher () and number of pharmacy claims 20% higher () post-DPN diagnosis. The mean number of hospital visits per patient increased significantly from 1.8 to 2.2 post-DPN diagnosis, and the mean number of ER visits per patient from 2.3 to 2.5, resulting in an overall increase in the number of hospital visits of these patients by 45.6% and ER visits by 20.3% post-DPN diagnosis (). This increase in number of visits, as well as an increase in cost per visit of 9.2% for hospital visits and 21.5% for ER visits (), contribute to an increase in total costs associated with hospitalization (59% increase) and ER (47% increase) (). Similarly, an ∼20% increase in number of office visits and number of pharmacy claims, along with an 11.6% increase in the cost per office visit and 8.3% increase in the cost per pharmacy claim () post-DPN diagnosis, contribute to an increase in the total direct cost of office visits and pharmacy claims by 39% and 30%, respectively (). Combined cost of hospital visits, ER visits, office visits, and treatments lead to a 46% increase in the aggregated costs associated with MRU post-DPN diagnosis ().
Table 2. Number and percentage of patients that make hospital, ER, and office visits.
Table 3. Count, mean, median, and standard deviation of hospital, ER, and office visits.
Table 4. Cost per visit and annual cost per patient.
Increase in the number of visits and cost per visit also contributed to a significant increase (46%) in the average annual cost per patient post-DPN diagnosis ($13,874) ().
Pain co-morbidity analysis
Pain co-morbidities and pain-associated co-morbidities were analyzed post-DPN diagnosis. There was a 6% increase () in the number of patients suffering from various co-morbidities analyzed. In particular, there was a 37% increase in patients suffering from other pain co-morbidities such as atypical facial pain, phantom limb pain, trigeminal neuralgia, reflex sympathetic dystrophy, and nerve root and plexus disorders. There was also a 23% increase in patients suffering from depression and a 16% increase in patients suffering from osteoarthritis in the post-diagnosis period ().
Table 5. Number and pecentage of patients suffering from co-morbidities.
Drug usage in patients with DPN
In the analysis of various drug classes, viz. opioids, anti-convulsants, anti-depressants, and NSAIDs before and after DPN diagnosis, it emerged that NSAIDs were the most used drugs in analyzed patients irrespective of DPN diagnosis. The number of patients using NSAIDs stayed approximately the same pre- (31%) and post-DPN (30%) diagnosis. However, usage of other drug classes increased post DPN diagnosis (). The increase in usage was highest for anti-convulsants, especially gabapentin (56%), followed by long acting opioids, duloxetine, and short acting opioids (37%, 36%, and 26%, respectively) (). Additionally, there was an increase in the percentage of class possession days (as described in the Methods) for all treatments analyzed post-DPN diagnosis, with the highest absolute increase in the class possession days for the two anti-convulsants, pregabalin (10%) and gabapentin (6%).
Table 6. Drug/class usage by number of patients, percentage of patients, and percentage of class possession days.
Discussion
Neuropathy associated with diabetes is a growing healthcare priority due to its impact on patients’ quality-of-life and the additional resource burden as a result of the conditionCitation5. This study is an attempt to quantify the burden associated with DPN.
In this study, the mean age of identified DPN cohort was 61 years, which is similar to several other published studiesCitation27–30, but is higher than the mean age of 51 years reported by another study by Le et al.Citation10 based on the same database. This difference is likely due to exclusion of all patients co-diagnosed with depression in the study by Le et al.Citation10
Various factors which contribute to costs associated with MRU and, hence, economic burden of DPN such as treatment cost, cost per visit, and total cost associated with visits to the hospitals/ER/doctor’s office were analyzed. This study shows that diagnosis of DPN is associated with a 60% (∼$60 million) increase in the hospitalization costs; of this, $11 million was found to be directly associated with pain owing to DPN diagnosis and $49 million was associated with diagnosis of other pain co-morbidities analyzed. This increase in hospitalization costs is contributed to by an increase in the number of patients visiting hospitals and a higher rate of hospital visits post-DPN diagnosis. In further analysis of 3884 patients who visited hospitals post-DPN diagnosis, it was found that 1148 patients visited hospitals owing to pain associated with DPN and 2545 visited hospitals owing to a pain diagnosis associated with the co-morbidities analyzed (). Similarly, out of 8470 hospital visits post-DPN diagnosis, 1486 visits were found to have a DPN claim associated with the visit and 4651 had a claim associated with the pain co-morbidities analyzed, contributing to a 46% increase in the number of hospital visits and a 60% increase in the costs associated with hospitalization post-DPN diagnosis. In this study, annual cost per patient post-DPN diagnosis was calculated to be $13,874, which was 46% more than the annual cost per patient pre-DPN diagnosis ($9498). This cost ($13,874) is in agreement with the previously reported cost of $14,062 for patients with DPNCitation31, and is 3–5-fold higher than the annual cost per patient reported for pain conditions such as OA ($2600–$4833)Citation32,Citation33. These results underscore the chronic nature of pain in DPN and its contribution towards a heavy patient burden associated with the condition. While we cannot attribute causation (i.e. the increase in resource use post-diagnosis was solely due to pain), the only major change in all of these patients was the fact that they had a DPN diagnosis leading us to believe that most of the increased resource usage is attributed to the DPN diagnosis.
Inadequate pain management could be one of the reasons that contribute to recurrent visits by patients to the hospital. A high number of patients with DPN (42%) were found to be untreated with any of the following classes: opioids, anti-convulsants, anti-depressants, and NSAIDs at the baseline month which decreases to 32% over the 2-year follow-up period. For treatment, NSAIDs was found to be the most prescribed drug class, but there was no increase in its usage post-DPN diagnosis. This is consistent with the fact that NSAIDs are largely ineffective in the treatment of DPNCitation8. The database only captures prescription drug use, so it is difficult to say if the patients were using other over-the-counter NSAIDs to manage their pain, unlike other classes of drugs which are mostly prescription-based and, hence, allowed a more accurate analysis of their usage.
Gabapentin, an anticonvulsant which is an emerging first line treatment for DPNCitation5, showed the highest increase in usage (56%) post-DPN diagnosis. However, in terms of total usage, only 18% of patients with DPN were prescribed gabapentin compared to NSAIDs (30%). Among opioids, Schedule III/IV opioids were the most prescribed (46%), followed by Schedule II short acting opioids (18%) and Schedule II long acting opioids (4%). Although several clinical trials have established a role for opioids in the treatment of different types of neuropathic painCitation34–37, it is interesting to note that tapentadol extended release, a centrally acting analgesic which is a mu-opioid agonist and norepinephrine re-uptake inhibitor, is the only opioid that has been approved in the US by the Food and Drug Administration for the management of neuropathic pain associated with DPN. This analysis shows a high use of opioids in patients with DPN, which suggests that a majority of patients with DPN are perhaps refractory to first line treatmentsCitation34 such as NSAIDs and anti-depressants and, hence, were subsequently prescribed opioids for palliation or symptom relief. High use of opioids in patients with DPN may also be attributed to a large number of such patients suffering from pain co-morbidities such as osteoarthritis (33%) and low back pain (32%), which require opioids for pain management.
Analysis of pain co-morbidities associated with DPN showed that co-morbidities such as post-herpetic neuralgia, osteoarthritis, and back and neck back pain, showed an upward trend post-DPN diagnosis, and contributed to the economic burden associated with DPN, as they affect daily functioning of patients and impair their quality-of-life. A recent study showed that one out of four patients with DPN had anxiety, depression, and sleep disturbanceCitation8. While there was no significant increase in the number of patients suffering from sleep disorder post-DPN diagnosis (p-value = 0.26), there was a significant increase in the number of patients suffering from depression post-DPN diagnosis (p-value <0.001) (). This insignificant increase in the number of patients suffering from sleep disorder post-DPN diagnosis could be due to multiple reasons: (1) other co-morbidities associated with DPN overshadow sleep disorder and, hence, are being overlooked by physicians, (2) direct and indirect effect of prescribed medicinesCitation17, and/or (3) sedatives prescribed to treat sleep disorder prior to DPN diagnosis.
Since this study was carried out using a commercial claims database, it does not represent the entire US population and it suffers from the limitations associated with any claims data analysis, including coding accuracies and non-availability of clinical and diagnostic information, including any indicator of severity of pain, or its frequency of occurrence. Further, although the study shows an association of DPN diagnosis with an increase in MRU costs, only a percentage of these costs may actually be related to DPN diagnosis. However, given that the data analyzed is pre–post for the same patients, and the fact that the only common change is the diagnosis of DPN, makes us believe that the DPN diagnosis is a large contributor to the change in resource use. Lastly, costs have not been adjusted for inflation, and thus the comparison of cost between the pre-DPN and post-DPN periods may be viewed and inferred from accordingly.
Conclusion
The study uses data from a large US-based commercial claims database to evaluate drug class use as well as resource use and costs associated with DPN. Results of the analysis indicate that resource use significantly increases post-diagnosis of DPN, which could eventually lead to a significant increase in costs for payers. A noticeable proportion of patients with DPN have a pain co-diagnosis and, with tapentadol being the only approved opioid for treating DPN, there is a significant need for more treatments that can effectively manage DPN as well as other associated pain conditions.
Transparency
Declaration of funding and financial/other relationships
Janssen Global Services is the sponsor of the study, and procured the commercial claims data from IMS, Inc. The data analysis for the study was carried out by SmartAnalyst, Inc, who were financially remunerated by Janssen Global Services for their services.
Acknowledgments
The authors thank Kala Hill, MS, Janssen Global Services, LLC, and Nitesh Garg, BTech, SmartAnalyst, Inc. for providing analytical support for this study
References
- Treede RD, Jensen TS, Campbell JN, et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology 2008;70:1630-5
- Tesfaye S, Boulton AJ, Dyck PJ, et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care 2010;33:2285-93
- Vinik AI, Park TS, Stansberry KB, et al. Diabetic neuropathies. Diabetologia 2000;43:957-73
- Gordois A, Scuffham P, Shearer A, et al. The health care costs of diabetic peripheral neuropathy in the US. Diabetes Care 2003;26:1790-5
- Rathur HM, Boulton AJ. Recent advances in the diagnosis and management of diabetic neuropathy. J Bone Joint Surg Br 2005;87:1605-10
- Dyck PJ, Kratz KM, Karnes JL, et al. The prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: the Rochester Diabetic Neuropathy Study. Neurology 1993;43:817-24
- Tesfaye S, Stevens LK, Stephenson JM, et al. Prevalence of diabetic peripheral neuropathy and its relation to glycaemic control and potential risk factors: the EURODIAB IDDM Complications Study. Diabetologia 1996;39:1377-84
- Gore M, Brandenburg NA, Hoffman DL, et al. Burden of illness in painful diabetic peripheral neuropathy: the patients’ perspectives. J Pain 2006;7:892-900
- Tesfaye S, Selvarajah D. Advances in the epidemiology, pathogenesis and management of diabetic peripheral neuropathy. Diabetes Metab Res Rev 2012;28(1 Suppl):8-14
- Le TK, Able SL, Lage MJ. Resource use among patients with diabetes, diabetic neuropathy, or diabetes with depression. Cost Eff Resour Alloc 2006;4:18
- Boulton AJ, Vinik AI, Arezzo JC, et al. Diabetic neuropathies: a statement by the American Diabetes Association. Diabetes Care 2005;28:956-62
- Boyko EJ, Ahroni JH, Smith DG, et al. Increased mortality associated with diabetic foot ulcer. Diabet Med 1996;13:967-72
- Ding J, Cheung CY, Ikram MK, et al. Early retinal arteriolar changes and peripheral neuropathy in diabetes. Diabetes Care 2012;35:1098-104
- Davies M, Brophy S, Williams R, et al. The prevalence, severity, and impact of painful diabetic peripheral neuropathy in type 2 diabetes. Diabetes Care 2006;29:1518-22
- Melton LJ III, Dyck PJ. Diabetic polyneuropathy. In: Dyck PJ, Thomas PK, eds. Diabetic neuropathy. 2nd edn. Philadelphia, PA: W.B. Saunders, 1999. pp. 255-78
- Lindsay TJ, Rodgers BC, Savath V, Hettinger K. Treating diabetic peripheral neuropathic pain. Am Fam physician 2010;82:151-8
- Tesfaye S, Vileikyte L, Rayman G, et al. Painful diabetic peripheral neuropathy: consensus recommendations on diagnosis, assessment and management. Diabetes Metab Res Rev 2011;27:629-38
- Finnerup NB, Sindrup SH, Jensen TS. The evidence for pharmacological treatment of neuropathic pain. Pain 2010;150:573-81
- Galer BS, Gianas A, Jensen MP. Painful diabetic polyneuropathy: epidemiology, pain description, and quality of life. Diabetes Res Clin Pract 2000;47:123-8
- Benbow SJ, Wallymahmed ME, MacFarlane IA. Diabetic peripheral neuropathy and quality of life. Qjm 1998;91:733-7
- Backonja M, Beydoun A, Edwards KR, et al. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: a randomized controlled trial. JAMA 1998;280:1831-6
- Dworkin RH. An overview of neuropathic pain: syndromes, symptoms, signs, and several mechanisms. Clin J Pain 2002;18:343-9
- Haythornthwaite JA, Benrud-Larson LM. Psychological aspects of neuropathic pain. Clin J Pain 2000;16(2 Suppl):S101-5
- Rowbotham M, Harden N, Stacey B, et al. Gabapentin for the treatment of postherpetic neuralgia: a randomized controlled trial. JAMA 1998;280:1837-42
- Hiatt WR, Hoag S, Hamman RF. Effect of Diagnostic Criteria on the Prevalence of Peripheral Arterial Disease. Circulation 1995;91:1472-9
- IMS LifeLink. LifeLink Health Plan Claims Database. Overview and Study Design Issues. 2010. American Medical Association, http://www.uams.edu/TRI/hsrcore/Lifelink_Health_Plan_Claims_Data_DesignIssues_wcost_April2010[1].pdf. Accessed February 7, 2014
- Vileikyte L, Peyrot M, Gonzalez JS, et al. Predictors of depressive symptoms in persons with diabetic peripheral neuropathy: a longitudinal study. Diabetologia 2009;52:1265-73
- Sandercock D, Cramer M, Wu J, et al. Gabapentin extended release for the treatment of painful diabetic peripheral neuropathy: efficacy and tolerability in a double-blind, randomized, controlled clinical trial. Diabetes Care 2009;32:e20
- Younger DS. Diabetic neuropathy: a clinical and neuropathological study of 107 patients. Neurol Res Int 2010;2010:140379
- Viala-Danten M, Martin S, Guillemin I, et al. Evaluation of the reliability and validity of the Medical Outcomes Study sleep scale in patients with painful diabetic peripheral neuropathy during an international clinical trial. Health Qual Life Outcomes 2008;6:113
- Wade RL, Cai Q. Impact of L-Methylfolate combination therapy among diabetic peripheral neuropathy patients. American Journal of Pharmacy benefits updated 17 Oct 2012. http://www.ajmc.com/publications/ajpb/2012/AJPB_SepOct2012/Impact-of-L-Methylfolate-Combination-Therapy-Among-Diabetic-Peripheral-Neuropathy-Patients. Accessed February 7, 2014
- News from the Arthritis Foundation. 2008. Arthritis Foundation, Atlanta, GA, http://www.arthritis.org/files/images/newsroom/media-kits/Osteoarthritis_fact_sheet.pdf. Accessed February 7, 2014
- Osteoarthritis Costs U.S. Over $185 Billion a Year. 2009. Health Day, http://health.usnews.com/health-news/family-health/pain/articles/2009/11/30/osteoarthritis-costs-us-over-185-billion-a-year. Accessed February 7, 2014
- Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc 2010;85(3 Suppl):S3-14
- Dworkin RH, O’Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain 2007;132:237-51
- Finnerup NB, Otto M, McQuay HJ, et al. Algorithm for neuropathic pain treatment: an evidence based proposal. Pain 2005;118:289-305
- Wu CL, Agarwal S, Tella PK, et al. Morphine versus mexiletine for treatment of postamputation pain: a randomized, placebo-controlled, crossover trial. Anesthesiology 2008;109:289-96