Abstract
Background:
Large institutional analyses demonstrating outcomes of right anterior mini-thoracotomy (RAT) for isolated aortic valve replacement (isoAVR) do not exist. In this study, a group of cardiac surgeons who routinely perform minimally invasive isoAVR analyzed a cross-section of US hospital records in order to analyze outcomes of RAT as compared to sternotomy.
Methods:
The Premier database was queried from 2007–2011 for clinical and cost data for patients undergoing isoAVR. This de-identified database contains billing, hospital cost, and coding data from >600 US facilities with information from >25 million inpatient discharges. Expert rules were developed to identify patients with RAT and those with any sternal incision (aStern). Propensity matching created groups adjusted for patient differences. The impact of surgical approach on outcomes and costs was modeled using regression analysis and, where indicated, adjusting for hospital size and geographical differences.
Results:
AVR was performed in 27,051 patients. Analysis identified isoAVR by RAT (n = 1572) and by aStern (n = 3962). Propensity matching created two groups of 921 patients. RAT was more likely performed in southern hospitals (63% vs 36%; p < 0.01), teaching hospitals (66% vs 58%; p < 0.01) and larger hospitals (47% vs 30%; p < 0.01). There was significantly less blood product cost associated with RAT ($1381 vs $1912; p < 0.001). After adjusting for hospital differences, RAT was associated with lower cost than aStern ($38,769 vs $42,656; p < 0.01).
Conclusions:
Outcomes analyses can be performed from hospital administrative collective databases. This real world analysis demonstrates comparable outcomes and less cost and ICU time with RAT for AVR.
Introduction
The first valvular procedure via a right thoracotomy was reported by Lillehei et al.Citation1 in 1957 when they performed an annuloplasty to correct mitral insufficiency. However, a full sternotomy became the preferred incision for valvular surgery for decades to come. It was not until 1993 that the first aortic valve replacement via a right anterior thoracotomy (RAT) approach was performedCitation2. While several national champions of RAT for isolated aortic valve replacement (isoAVR) have presented their outcomes, no large multi-institutional analyses exist. Isolated series have exhibited equivalent results to sternotomy isoAVR while demonstrating less blood transfusion and decreased hospitalizations for RAT groupsCitation3–5. However, a major criticism of the RAT approach is that it increases the procedural costs due to the added equipment and longer operating timesCitation6,Citation7. To this point, a group of experienced cardiac surgeons who routinely perform alternative incision AVR (Supplementary Appendix A) analyzed a cross-section of US hospital records in order to better understand ‘real world’ clinical and economic outcomes of RAT as compared to sternotomy approaches for isoAVR.
Materials and methods
Data source
The Premier hospital database, a highly regarded hospital database that is used extensively and cited regularly in these types of analyses, was used as the data source for this studyCitation8. This database contains complete patient billing, hospital cost, and coding histories from more than 600 healthcare facilities throughout the US. The data from which this study was derived was extracted from more than 25 million inpatient discharges and 175 million hospital outpatient visits from acute care facilities, ambulatory surgery centers, and clinics across the nation.
A protocol describing the analysis objectives, criteria for patient selection, data elements of interest, and statistical methods was submitted to the New England Institutional Review Board (NEIRB) and exemption was obtained (NEIRB # 13–203).
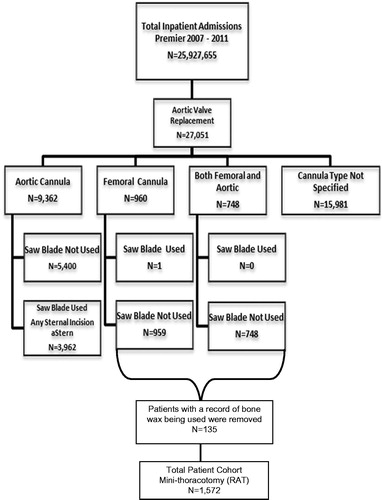
Eligible patients were 18 years of age or older and had undergone either a right anterior mini-thoracotomy (RAT) or any sternal incision (aStern) during the time period 2007–2011, for which isolated aortic valve replacement (isoAVR) was the primary reason for surgery. IsoAVR was identified for visits having the following primary ICD-9 procedure code classification: 35.21 and 35.22. Patients having either a record of Coronary Artery Bypass Grafting (CABG) in conjunction with isoAVR or procedures utilizing robotic technology were excluded. A set of expert rules were developed by authors ER, SCM, JRM, AS, GA, and EAG based on surgical experience to text mine the charge master billing files of the Premier database in order to identify a surgical approach as either RAT or aStern. displays rules for procedure identification and attrition.
For all eligible patients, elements describing adverse events, hospital cost, surgery time, length of stay and re-admissions were obtained from the data. Cost analysis reflected the cost of the procedure to the hospital. The pre-operative All Patient Refined Diagnosis Related Groups (APR-DRG) severity level was used as an index of comorbidity. The 3 M APR DRG Classification System is a widely adopted proprietary risk adjustment classification tool, which uses information from routine claims data to produce valid and reliable severity measurement and risk adjustment scoresCitation9. It is used to account for differences related to an individual’s severity-of-illness or risk-of-mortality in large datasets. Comorbid conditions that might influence procedure selection or outcomes of interest, such as previous organ transplantation, the presence of pulmonary disease or diabetes mellitus, were obtained using ICD-9 diagnosis and procedure codes. Supplementary Appendix B provides a detailed listing of all ICD-9 codes for each condition included in the study. Information on socio-demographic characteristics and health insurance status was also included, as were descriptors of the care setting, namely census region, urban or rural setting, teaching hospital status, and facility bed count. Adverse events (identified by ICD-9 codes) that occurred intra-operatively were flagged and included in the analysis. A detailed list of each event and the corresponding ICD-9 code is found in Supplementary Appendix C.
Statistical analyses
The objective of this study was to use the Premier hospital database to compare clinical and economic outcomes in patients undergoing isoAVR with RAT vs aStern. Outcomes of interest included adverse events, hospital costs, length of stay, and re-admission rates. Propensity scoring was utilized to create well-matched groups for comparison. Comorbid conditions before and after matching are contained in Supplemental Tables 1 & 2. Since hospital costs have been found to be positively skewed, a generalized linear model (GLM) with a gamma distribution and a log link function was used to adjust for differences in hospital characteristics (teaching vs non-teaching, urban vs rural, and bed count) and to calculate the corresponding least square means of overall cost for the hospital stay within each matched cohort. Extensive details of the statistical methodology are contained in Supplementary Appendix D.
Results
Data analysis identified 27,501 patients undergoing AVR. Expert rule analysis positively identified isoAVR by RAT in 1572 patients and by aStern in 3962 patients. Propensity matching created two balanced groups of 921 patients each ( & ). RAT was more likely performed in southern hospitals (63% vs 36%; p < 0.01), teaching hospitals (66% vs 58%; p < 0.01), and larger hospitals (47% vs 30%; p < 0.01) ( & ). There were no statistically significant differences in adverse events between the two groups (). After adjusting for hospital differences, hospital lengths of stay and re-admission rates, up to 30–60 days, were not different between groups (). Cost analysis revealed that RAT was associated with lower hospitalization cost than aStern () ($38,769 vs $42,656; p < 0.0001). Further examination revealed that RAT was associated with lower mean room and board costs, including ICU, compared to aStern ($11,283.56 vs $9890.77, p < 0.01). Finally, mean blood bank associated costs were lower for RAT group than aStern group ($1381 vs $1912, p < 0.001).
Table 1. Patient demographics before matching.
Table 2. Patient demographics after matching.
Table 3. Hospital characteristics before matching.
Table 4. Hospital characteristics after matching.
Table 5. Adverse events after matching.
Table 6. Healthcare utilization and costs after matching.
Table 7. Least square means for total hospital costs.
Discussion
This study used a conservative ‘real world’ analysis (grouping full and partial sternotomies) and demonstrated comparable outcomes as well as less total cost, room and board cost, as well as blood bank related cost with RAT for isoAVR. While others have published single center series comparing minimally invasive AVR (RAT or hemi-sternotomy vs sternotomy), this is the first large multi-center/multi-regional study comparing RAT to any sternotomy approach for isolated AVR.
After propensity matching, we did not appreciate significant differences in mortality or complication rates between groups. This study corroborates the findings of several other studies demonstrating that RAT for AVR is safe, with complications rates similar to those using a sternotomy approachCitation3,Citation4,Citation10,Citation11. Therefore, based on this study as well as many other single center studies, RAT for isolated AVR appears to be safe.
Multiple series have demonstrated shorter hospital LOS when a less invasive approach (RAT or hemi-sternotomy) is used instead of a full sternotomyCitation3–5,Citation12–17. Our study did not show a difference in hospital LOS. A potential explanation is that the aStern group included both hemi- and full sternotomy patients and, thus, it could have benefited the LOS for the aStern group as hemi-sternotomy has been shown to be associated with shorter LOS compared to full sternotomyCitation15–17. ICU LOS has also been shown to be shorter when less invasive techniques, such as hemi-sternotomy, are used for AVRCitation15,Citation16. We were not able to obtain specific ICU LOS vs total hospital LOS due to limitations in the Premier database. Nonetheless, the mean ICU room and board cost was higher for the aStern group compared to RAT group ($5666 vs $5123). This may suggest a shorter ICU LOS or lower costs due to decrease intensive care needed for the RAT group.
Our study demonstrated roughly a $500 (28%) reduction in blood bank related costs for RAT patients despite there being a few more patients in the RAT group receiving transfusion (n = 871; ). Our analysis confirms less blood product usage for RAT as suggested by other seriesCitation3.
Finally, this study also demonstrates the potential value of developing prospective query methodologies in order to probe large hospital administrative collective databases, which comprise broad geographic and demographic representation of US hospitals, in order to compare different surgical approaches. This approach allows investigators to effectively compare outcomes utilizing relatively recent data for large and broad patient populations representing the real world setting.
Limitations
This study also had some noteworthy limitations. The authors acknowledge that ‘minimally invasive’ cardiac surgery is often recognized as including both partial sternotomy and RAT approaches. Based on expert rules for procedure identification, it was not feasible to clearly segregate partial from full sternotomies and, therefore, both are represented in the aStern cohort. Additionally, due to the de-identified nature of Premier, an audit of an institution’s data to verify the expert rules algorithm was not possible. However, this large multi-institutional comparison of sternal vs non-sternal approach for isoAVR is compelling, filling a gap in the literature. Furthermore, given the demonstrated clinical benefits of partial-sternotomy vs full sternotomyCitation16,Citation18,Citation19, it could be argued that the observed differences between the two cohorts may have been even greater if the partial-sternotomies had been excluded from the control group.
While the data were mined from a sophisticated hospital administrative database, certain data points could not be clearly identified. These limitations are inherent to the data source; however, they could be rationalized to impact both cohorts similarly. Additionally, the analysis was limited to a 30–60 day perioperative period, which restricts analysis of potential long-term complications.
Conclusion
Informative outcomes analyses can be performed from hospital administrative collective databases. This conservative real world analysis (grouping full and partial sternotomies together) demonstrates mostly comparable clinical outcomes but lower costs associated with right anterior mini-thoracotomy for AVR.
Supplementary Material
Download PDF (78.3 KB)Transparency
Declaration of funding
Funding for this project was provided by Edwards Lifesciences. This included funding for access to the Premier database and statistical analysis.
Declaration of financial/other relationships
ER, SCM, AS, GA, EAG are Edwards Lifesciences consultants. MM is an Edwards Lifesciences employee. JRM is on the Edwards Lifesciences medical advisory board. CG is an employee of CTI Clinical Trials and Consulting services which is a paid consultant to Edwards Lifesciences. ER is also a speaker for Medtronic Sorin and is on the Cardionet advisory board. SCM is a Bazter consultant and an Abiomed speaker. GA is an Abbott and Mitralign consultant and an Amcure and St Judes speaker. EAG is a Medtronic consultant and holds Intellectual property with Edwards Lifesciences and Medtronic. JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
References
- Lillehei CW, Gott VL, DeWall RA, et al. Surgical correction of pure mitral insufficiency by annuloplasty under direct vision. J Lancet 1957;77(11):446-9
- Rao PN, Kumar AS. Aortic valve replacement through right thoracotomy. Tex Heart Inst J 1993;20(4):307-8
- Glauber M, Miceli A, Gilmanov D, et al. Right anterior minithoracotomy versus conventional aortic valve replacement: a propensity score matched study. J Thorac Cardiovasc Surg 2013;145(5):1222-6
- Brinkman WT, Hoffman W, Dewey TM, et al. Aortic valve replacement surgery: comparison of outcomes in matched sternotomy and PORT ACCESS groups. Ann Thorac Surg 2010;90(1):131-5
- Sharony R, Grossi EA, Saunders, PC et al. Propensity score analysis of a six-year experience with minimally invasive isolated aortic valve replacement. J Heart Valve Dis 2004;13(6):887-93
- Murtuza B, Pepper JR, Stanbidge, RD et al. Minimal access aortic valve replacement: is it worth it? Ann Thorac Surg 2008;85(3):1121-31
- Cunningham MJ, Berberian CE, Starnes, VA. Is Transthoracic Minimally Invasive Aortic Valve Replacement Too Time-Consuming for the Busy Cardiac Surgeon? Innovations (Phila) 2011;6(1):10-14
- Premier Research Services—Premier Inc. Available at: http://www.premier-inc.com/prs. Accessed December, 2012.
- Averill RF, Goldfield N, Hughes J, et al. What Are APR-DRGs? An Introduction to Severity of Illness and Risk of Mortality Adjustment Methodology. Salt Lake City, UT: 3M Health Information Systems. 2003
- Plass A, Scheffel H, Alkadhi H, et al. Aortic valve replacement through a minimally invasive approach: preoperative planning, surgical technique, and outcome. Ann Thorac Surg 2009;88(6):1851-6
- Glower DD, Lee T, Desai B. Aortic valve replacement through right minithoracotomy in 306 consecutive patients. Innovations (Phila) 2010;5(5):326-30
- Johnston DR, Atik FA, Rajeswaran J, et al. Outcomes of less invasive J-incision approach to aortic valve surgery. J Thorac Cardiovasc Surg 2012;144(4):852-58 e3
- Doll N, Borger MA, Hain J, et al. Minimal access aortic valve replacement: effects on morbidity and resource utilization. Ann Thorac Surg, 2002. 74(4):S1318-22
- Mihaljevic T, Cohn LH, Unic D, et al. One thousand minimally invasive valve operations: early and late results. Ann Surg 2004;240(3):529-34; discussion 534
- Brown ML, McKellar SH, Sundt TM, et al. Ministernotomy versus conventional sternotomy for aortic valve replacement: a systematic review and meta-analysis. J Thorac Cardiovasc Surg 2009;137(3):670-9 e5
- Bakir I, Casselman FP, Wellens F, et al. Minimally invasive versus standard approach aortic valve replacement: a study in 506 patients. Ann Thorac Surg 2006;81(5):1599-604
- Liu J, Sidiropoulos A, Konertz W. Minimally invasive aortic valve replacement (AVR) compared to standard AVR. Eur J Cardiothorac Surg 1999;16 Suppl 2:S80-3
- Bonacchi M, Prifti E, Giunti G, et al. Does ministernotomy improve postoperative outcome in aortic valve operation? A prospective randomized study. Ann Thorac Surg 2002;73(2):460-5; discussion 465-6
- Cohn LH, Adams DH, Couper GS, et al. Minimally invasive cardiac valve surgery improves patient satisfaction while reducing costs of cardiac valve replacement and repair. Ann Surg 1997;226(4):421-6; discussion 427-8