Abstract
Objective:
Selective internal radiation therapy (SIRT) using SIR-Spheres® 90Y-labeled resin microspheres has been shown to be a well-tolerated, effective treatment in patients with inoperable liver-dominant chemotherapy–refractory metastatic colorectal cancer (mCRC). This study estimated the cost-effectiveness of 90Y-resin microspheres compared to best supportive care (BSC) from a UK perspective.
Methods:
Survival data from a comparative retrospective cohort study was analyzed and used in a state-transition cost-effectiveness model, using quality-adjusted life years (QALYs) gained as the measure of effectiveness. The model incorporated costs for the SIRT procedure, monitoring, further treatment, adverse events, and death. Utility values, reflecting patient quality-of-life, were taken from a published source.
Results:
SIRT using 90Y-resin microspheres compared to BSC improved overall survival by a mean of 1.12 life years and resulted in a cost per QALY gained of £28,216. In sensitivity analysis, this varied between £25,015–£28,817.
Conclusion:
In an area of large unmet need, treatment with 90Y-resin microspheres offers a clinically effective and cost-effective treatment option.
Introduction
Chemotherapy–refractory metastatic colorectal cancer (mCRC) is an area of unmet need with a poor prognosis. The median survival estimates for patients who received placebo and an active biological treatment (regorafenib) in a recent clinical trial were 5.0 and 6.4 months, respectivelyCitation1. In the UK, treatment options are limited. None of the currently-licensed pharmacological therapies (cetuximab, panitumumab, and bevacizumab) are recommended by the National Institute for Health and Care Excellence (NICE)Citation2.
Selective internal radiation therapy (SIRT) delivers targeted radiation therapy to tumors in the liver. Millions of radioactive yttrium-90 (90Y) resin microspheres (SIR-Spheres; Sirtex Medical, North Sydney, Australia) are delivered directly into the hepatic artery through a microcatheter. The microspheres are then carried by the bloodstream into the microvasculature that supplies the tumors, where the microspheres become lodged and deliver radiation that destroys the tumor cells. SIRT using 90Y-resin microspheres has been demonstrated to be well tolerated and effective in reducing tumor burden and increasing survival in chemotherapy–refractory mCRC patientsCitation3–6.
This study aimed to calculate the cost-effectiveness of SIRT using 90Y-resin microspheres compared to best supportive care (BSC) in patients with inoperable chemotherapy–refractory colorectal liver metastases in the UK.
Methods
Source of efficacy data
Four potential sources of efficacy data have been identified through a targeted literature review:
A Phase III trial comparing protracted intravenous 5-fluorouracil (5FU) infusion alone or with 90Y-resin microspheres for liver-limited mCRC refractory to standard chemotherapyCitation3;
A Phase II trial of 90Y-resin microspheres alone in inoperable, chemotherapy-refractory colorectal liver-dominant metastasesCitation4;
A matched-pair comparison of 90Y-resin microspheres plus BSC vs BSC alone for chemotherapy-refractory liver-dominant colorectal metastasesCitation5; and
A comparative retrospective cohort study of 90Y-resin microspheres vs BSC of chemotherapy-refractory liver-dominant mCRCCitation6.
These studies were selected because they are either prospective, comparative, or both (many other retrospective single-arm studies exist).
The data-set from the comparative retrospective cohort studyCitation6, which recorded overall survival, was considered to be the most appropriate source of data for modeling the cost-effectiveness of 90Y-resin microspheres. The observational study design allowed for flexibility in the definition of BSC, which potentially included chemotherapy, biological agents, and further interventional procedures. The study authors believed treatment was similar in both arms, except for the addition of SIRT using 90Y-resin microspheres. The patient-level data from the study was available for analysis for all 29 patients receiving BSC and for 223 of the 224 patients treated with 90Y-resin microspheres. The baseline patient characteristics are shown in .
Table 1. Patient characteristics.
Model settings
The cost-effectiveness model compared SIRT using 90Y-resin microspheres with BSC from the perspective of the National Health Service (NHS) in England, following NICE guidance on good modeling practiceCitation7. The outcomes from the analysis were costs, life years, quality-adjusted life years (QALYs), cost per life year gained, and cost per QALY gained. The model had a daily cycle length to accurately model the relatively short survival. A lifetime time horizon was used.
Model structure
mCRC was modeled using health states to represent pre-progression disease, post-progression disease, and death. Such a model structure appropriately reflects the disease and is commonly used in oncology.
Generally, transitions between health states are driven by parametric curves fitted to overall and progression-free survival. However, while the overall survival curve was used to derive the probability of moving to the death health state in each cycle, progression-free survival was not recorded in the studyCitation6. Therefore, it was assumed that, at any time point, 50% of the cohort were in each of the pre- and post-progression health states, based on the proportion of time spent in the health states in other models in a similar indicationCitation8.
Inputs
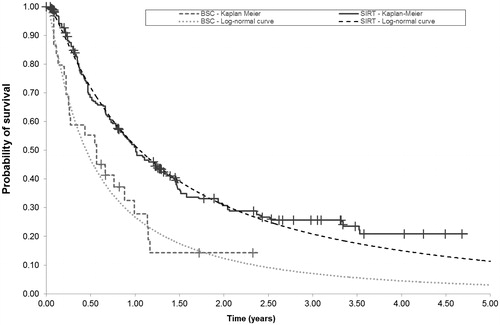
Some patients in the comparative retrospective cohort study were still alive at the end of the study (Kaplan-Meier estimates: 30/224 in the 90Y-resin microspheres arm and 7/29 in the BSC arm), and, therefore, it was necessary to extrapolate the survival data to predict the proportion of patients surviving at each time point until the last patient had died. This was done by fitting parametric curves to the Kaplan-Meier survival data. Nine distributions were tested for goodness-of-fit using the Akaike Information Criterion (AIC)Citation9. The AIC is appropriate for testing the goodness-of-fit in this analysis because the data is mature. The log-normal curve had the lowest AIC score and was, therefore, considered the best-fitting curve, and the stratified log-normal was the second best-fitting curve (see ).
Figure 1. Overall survival curves for best supportive care and selective internal radiation therapy. BSC, best supportive care; SIRT, selective internal radiation therapy.
Quality-of-life was incorporated into the model using utility values from a recent economic evaluation of treatments for mCRC after first-line chemotherapy. Utility values are a measure of HRQoL, with a utility value of 1 representing full health and 0 representing death. A utility value of 0.75 was used for patients who had not progressed, and 0.69 for patients whose disease had progressedCitation8. The reduction in HRQoL following progression is relatively small because radiological markers are not expected to dramatically affect patients’ wellbeing. However, clinicians advised that patients do experience a distinct reduction in HRQoL shortly before death, which was reflected in the model through a utility decrement of 0.1 for the 28 days prior to death. Published data quantifying this decrement could not be found; therefore, this value is an assumption that is tested in the sensitivity analysis.
The model considered costs for SIRT, BSC, monitoring, further treatment, adverse events, and death. The work-up and procedure for SIRT were micro-costed using NHS reference costs and equipment cost data provided by a UK hospitalCitation10. The total cost of the procedure and work-up, including treatment acquisition, equipment and hospital care, was £14,248.
Patients were assumed to have a monthly outpatient appointment with an oncologist. This was costed at £125 according to NHS reference costsCitation11.
Unfortunately, chemotherapy regimens and dosing were not recorded in the retrospective cohort study and, therefore, could not be used to calculate the costs of treatment after SIRT or in the BSC arm. However, these data were available from another studyCitation5. This was considered appropriate because, although overall survival is expected to vary dramatically depending on prognosis, treatments for a chemotherapy–refractory population are not expected to differCitation12. These data allowed a daily cost per patient to be calculated as £16.67 in the 90Y-resin microspheres arm and £15.81 in the BSC arm. This cost is applied for the entire patient lifetime.
Adverse events were incorporated in the model using the data for Grade 3 and 4 adverse events reported in the Phase III trialCitation3. The cost per patient for adverse events was £42.55 in the BSC arm and £7.43 in the 90Y-resin microspheres arm. A cost of death was also incorporated into the model to reflect the costs of terminal care in end-stage cancers. The input values are summarized in .
Table 2. Summary of input values.
A range of sensitivity analyses were performed. The one-way sensitivity analysis varied each parameter between its lower and upper bound and investigated the effect on the cost per QALY. The probabilistic analysis simultaneously sampled each parameter from its appropriate distribution (beta for utilities, normal for costs, and multivariate normal for survival curve parameters) for 1000 simulations and investigated the uncertainty around the cost per QALY. The scenario analysis explored alternative parametric curves for overall survival, alternative sources for utility values, and alternative assumptions for the proportion of time spent in the pre- and post-progression health states.
Results
The outcomes of the model demonstrate that SIRT using 90Y-resin microspheres can be expected to increase overall survival by 1.12 years (discounted) compared to treatment with BSC. The mean life expectancy is 2.09 years (2.38 undiscounted) for patients treated with 90Y-resin microspheres compared to 0.97 years (1.03 undiscounted) for patients treated with BSC (see ).
Table 3. Base case and scenario analysis results.
Treatment with 90Y-resin microspheres resulted in an increase of 0.81 QALYs compared to BSC (1.50 compared to 0.69). In the 90Y-resin microspheres arm, 0.78 of the QALYs were obtained in the pre-progression state, and 0.72 in the post-progression state. In the BSC arm, these were 0.36 and 0.33, respectively.
More patients in the BSC arm experienced Grade 3–4 adverse events (stomatitis, anorexia, fatigue, hand–foot syndrome, dyspnoea, pulmonary, and allergy) than in the 90Y-resin microspheres arm (45% compared to 5%) because these events were the result of failure by chemotherapy to control the diseaseCitation3.
The total discounted cost was £35,487 in the 90Y-resin microspheres arm and £12,730 in the BSC arm—a difference of £22,757. The costs in the 90Y-resin microspheres arm were higher, partly due to the cost of SIRT using 90Y-resin microspheres, but also due to the additional treatment and monitoring costs resulting from the extended survival. There was a small cost saving (£35) in the 90Y-resin microspheres arm due to the lower rate of adverse events.
The increased cost and improved survival following SIRT result in a cost per life year gained of £20,323 and a cost per QALY gained of £28,216 in the base case.
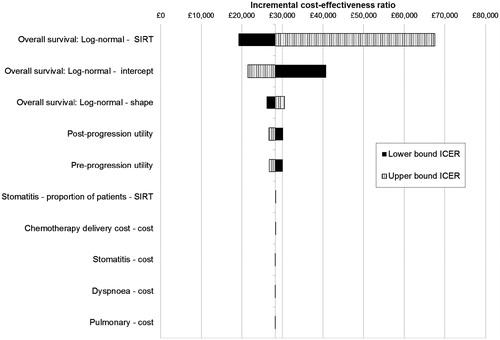
Sensitivity analyses show that the model is robust to changes in parameters. Scenario analysis results demonstrate that the cost per QALY was not sensitive to alternative assumptions for survival curves, utilities, progression, or adverse events, varying between £25,015–£28,817. The one-way sensitivity analysis found that the parameters that had the biggest effect were those relating to the curve used to model overall survival, see .
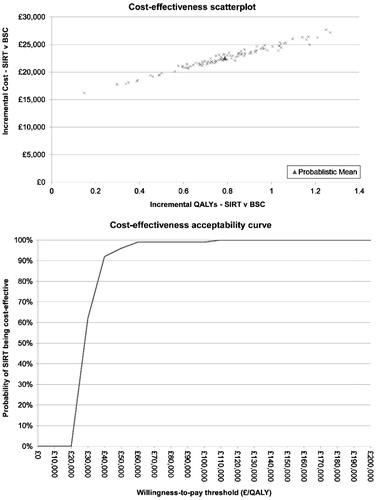
The probabilistic sensitivity analysis found that the probability of 90Y-resin microspheres being cost-effective at a willingness-to-pay threshold of £30,000/QALY is 57% (see ). The cost-effectiveness scatterplot shows a much wider spread in the incremental QALYs than in the incremental cost, which is driven by the uncertainty in the estimation of life years from the overall survival parameters.
Discussion
This analysis shows that treatment with 90Y-resin microspheres offers an extension to survival compared to BSC. We acknowledge the limitations of using cohort studies due to the risk of selection bias and seek to validate our results using other studies. First, we note that the standard care cohort of the study comprised patients who were eligible for SIRT but chose not to undergo the procedure in favor of alternative options, or who would be at risk of lung shunting (radioactive materials from SIRT entering the lung)Citation6, and we have no reason to believe that these patients would have an expected poorer prognosis than patients who received SIRT. The matched-pair analysis reported a significant improvement in survivalCitation5, although the randomized study was not powered to detect a significant difference and is confounded by its cross-over designCitation3. The estimates of survival are consistent with those from other studies: survival in the 90Y-resin microspheres arm was compared to that from the Phase II trialCitation4, and survival in the BSC arm was compared to the overall survival for BSC and biological agents, as modeled in TA242Citation8. The mean survival from the Phase II trial, calculated by fitting a log-normal curve to the overall survival data, was 1.66 years, with a 95% confidence interval of 1.16–2.50 years. The mean survival from the model base case lies within this confidence interval, demonstrating that the mean overall survival for 90Y-resin microspheres is not significantly different between the studies. The mean survival for the BSC arm in TA242 is 0.51 yearsCitation8, but this increases to 1.38 years when patients receive cetuximab and irinotecan. Although this comparison is limited, it suggests that the survival for the BSC arm in this cost-effectiveness analysis is realistic.
In this analysis, treatment with 90Y-resin microspheres has shown a survival advantage, but the high costs of chemotherapy and biological agents in the survival extension increase the cost per QALY. It is worth noting that appropriate patients in this analysis were assumed to receive cetuximab and bevacizumab (as in the data provided from the matched-pair analysisCitation5), but these treatments in themselves may not be considered to be cost-effective (TA242). This analysis assumes that patients keep receiving these treatments until death; however, they may in fact stop earlier, thus reducing the cost, particularly in the 90Y-resin microspheres arm where survival is greater, but with a slight reduction in survival. In those circumstances, the cost per QALY gained of using 90Y-resin microspheres would very likely be reduced.
The strengths of this analysis lie in the mature survival data for a large number of patients treated with 90Y-resin microspheres. It is well understood that mature survival data leads to more reliable estimates of overall survival from parametric curves and only 20% of patients were still alive in the comparative retrospective cohort study after 4 years. Additionally, the sample size (n = 224) is relatively large. Furthermore, although randomized controlled trials are regarded as the gold standard of evidence, the use of an observational data-set allowed the modeling of realistic clinical practice. The choice of BSC as the comparator is reasonable because this analysis examines the cost-effectiveness of SIRT using 90Y-resin microspheres for patients already refractory to chemotherapy. These patients have very limited or no other treatment options.
The analysis is not without limitations, most notably stemming from the limited information available from the study. Progression-free survival, which is frequently used in these analyses to predict health state transitions, was not available. However, progression is measured by surrogate markers, and clinical opinion questions whether radiological markers of progression represent a point where changes are discernible to a patientCitation13. Evidence from the literature suggests that progression does not dramatically impact HRQoLCitation8. Furthermore, quality-of-life data were not collected in the Bester et al.Citation6 study; these data would have helped to inform the patient experience. Equally, if information was available on the treatments patients received instead of or after 90Y-resin microspheres, the costs of chemotherapy could have been more accurately modeled. HRQoL data was not collected in the studyCitation6, and, thus, information was not available to inform the health state utility values or the end-of-life utility decrement. Patients in the 90Y-resin microspheres arm had fewer adverse events, but the effect of these on HRQoL is not captured in the model. An additional HRQoL benefit may exist that has not been captured in the model if patients either receive less toxic chemotherapy following 90Y-resin microspheres or experience prolonged control of liver metastases and thereby avoid the impact of advanced disease symptoms.
Conclusion
This analysis has demonstrated that the use of 90Y-resin microspheres is a cost-effective option in the treatment of patients with chemotherapy–refractory liver-dominant metastases resulting from colorectal cancer in the UK. In an area of large unmet need, treatment with 90Y-resin microspheres offers a clinically effective and cost-effective treatment option.
Transparency
Declaration of funding
The development of the economic model and the manuscript was funded by Sirtex Medical Limited, the manufacturer of SIR-Spheres.
Declaration of financial/other relationships
BP and RA work for BresMed, who were reimbursed by Sirtex Medical Limited for their time on preparing the manuscript. KS is an employee of Sirtex Medical Limited. LB, AK, BS, and HW act as advisors to Sirtex Medical Limited.
Acknowledgments
The authors would like to thank Nic Brereton for aiding in the design of the study and critiquing the manuscript, Baerbel Meteling for her assistance in providing the data, Becca Harvey for performing statistical analysis of the data, and Chris Knight for reviewing the manuscript.
References
- Grothey A, Van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013;381:303-12
- NICE. Cetuximab, bevacizumab and panitumumab for the treatment of metastatic colorectal cancer after first-line chemotherapy: Cetuximab (monotherapy or combination chemotherapy), bevacizumab (in combination with non-oxaliplatin chemotherapy) and panitumumab (monotherapy) for the treatment of metastatic colorectal cancer after first-line chemotherapy (review of technology appraisal 150 and part review of technology appraisal guidance 118). London, 2012. http://www.nice.org.uk/guidance/ta242. Accessed May 24, 2013
- Hendlisz A, Van den Eynde M, Peeters M, et al. Phase III trial comparing protracted intravenous fluorouracil infusion alone or with yttrium-90 resin microspheres radioembolization for liver-limited metastatic colorectal cancer refractory to standard chemotherapy. J Clin Oncol 2010;28:3687-94
- Cosimelli M, Golfieri R, Cagol PP, et al. Multi-centre phase II clinical trial of yttrium-90 resin microspheres alone in unresectable, chemotherapy refractory colorectal liver metastases. Br J Cancer 2010;103:324-31
- Seidensticker R, Denecke T, Kraus P, et al. Matched-pair comparison of radioembolization plus best supportive care versus best supportive care alone for chemotherapy refractory liver-dominant colorectal metastases. Cardiovasc Intervent Radiol 2012;35:1066-73
- Bester L, Meteling B, Pocock N, et al. Radioembolization versus standard care of hepatic metastases: comparative retrospective cohort study of survival outcomes and adverse events in salvage patients. J Vasc Interv Radiol 2012;23:96-105
- NICE. Guide to the methods of technology appraisal. London, 2013. http://www.nice.org.uk/article/pmg9/resources/non-guidance-guide-to-the-methods-of-technology-appraisal-2013-pdf. Accessed May 24, 2013
- Hoyle M, Crathorne L, Peters P, et al. The clinical effectiveness and cost-effectiveness of cetuximab (mono- or combination chemotherapy), bevacizumab (combination with non-oxaliplatin chemotherapy) and panitumumab (monotherapy) for the treatment of metastatic colorectal cancer after first-line chemotherapy (review of technology appraisal No.150 and part review of technology appraisal No. 118): a systematic review and economic model. Health Technol Assess 2013;17:1-237
- Akaike H. A new look at the statistical model identification. IEEE Trans Auto Contr 1974;19:716-23
- The Christie NHS Foundation Trust. SIRT equipment costs. Manchester, 2012
- NHS. National schedule of reference costs 2010–2011. London, 2012. https://www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012. Accessed June 12, 2013
- NICE. Colorectal Cancer: the diagnosis and management of colorectal cancer. London, 2011. http://www.nice.org.uk/guidance/cg131/resources/guidance-colorectal-cancer-pdf. Accessed May 24, 2013
- Addicott R, Dewar S. Improving choice at end of life: a descriptive analysis of the impact and costs of the Marie Curie Delivering Choice Programme in Lincolnshire. London: The King's Fund, 2008. http://www.kingsfund.org.uk/sites/files/kf/improving-choice-end-of-life-descriptive-analysis-impact-costs-marie-curie-choice-programme-lincolnshire-rachael-addicot-steve-dewar-april-2008.pdf. Accessed June 12, 2013
- NICE. Erlotinib for the treatment of relapsed non-small cell lung cancer: ERG report. London, 2006. Available at: http://www.nice.org.uk/guidance/ta162/resources/lung-cancer-nonsmallcell-erlotinib-evidence-review-group-report2. Accessed June 12, 2013
- NICE. Trastuzumab for the treatment of HER2 positive metastatic adenocarcinoma of the stomach or gastro-oesophageal junction: ERG report. London, 2010. Available at: http://www.hta.ac.uk/erg/reports/2234.pdf. Accessed June 12, 2013
- Joint Formulary Committee. British National Formulary (online) London: BMJ Group and Pharmaceutical Press, 2012. Available at: http://www.bnf.org/bnf/index.htm Accessed June 12, 2013
- Ramsey S, Andersen M, Etzioni R, et al. Quality of life in survivors of colorectal carcinoma. Cancer 2000;88(6):1294-303