Abstract
Mounting evidence indicates that inflammation may play a significant role in the development of depression. Patients with depression exhibit increased inflammatory markers, and administration of cytokines and other inflammatory stimuli can induce depressive symptoms. Mechanisms by which cytokines access the brain and influence neurotransmitter systems relevant to depression have also been described, as have preliminary findings indicating that antagonizing inflammatory pathways may improve depressive symptoms. One primary source of inflammation in depression appears to be adiposity. Adipose tissue is a rich source of inflammatory factors including adipokines, chemokines, and cytokines, and a bidirectional relationship between adiposity and depression has been revealed. Adiposity is associated with the development of depression, and depression is associated with adiposity, reflecting a potentional vicious cycle between these two conditions which appears to center around inflammation. Treatments targeting this vicious cycle may be especially relevant for the treatment and prevention of depression as well as its multiple comorbid disorders such as cardiovascular disease, diabetes, and cancer, all of which have also been associated with both depression and inflammation.
Existe una evidencia creciente que señala que la inflamación puede jugar un papel significativo en el desarrollo de la depresión. Los pacientes con depresión muestran aumentados marcadores inflamatorios, y la administración de citoquinas y otros estímulos inflamatorios pueden inducir síntomas depresivos. También se han descrito mecanismos a través de los cuales las citoquinas tienen acceso al cerebro y afectan los sistemas de neurotransmisión importantes en la depresión, y se cuenta con hallazgos preliminares que indican que el antagonizar las vías inflamatorias puede mejorar los síntomas depresivos. Una fuente primaria de inflamación en la depresión parece ser la adiposidad. El tejido adiposo es una rica fuente de factores inflamatorios que incluyen las adipoquinas, las quemoquinas y las citoquinas, y también se ha revelado una relación bidireccional entre adiposidad y depresión. La adiposidad está asociada con el desarrollo de la depresión y la depresión está asociada con la adiposidad, lo que refleja un potencial círculo vicioso entre estas dos condiciones que parece estar centrado en la inflamación. Los tratamientos que se enfocan en este círculo vicioso pueden ser especialmente relevantes para el tratamiento y prevención de la depresión como de sus múltiples trastornos comórbidos como la enfermedad cardiovascular, la diabetes y el cáncer, todos los cuales también se han asociado con la depresión y la inflamación.
Un faisceau d'arguments sont en faveur d'un rôle significatif de l'inflammation dans le développement de la dépression. En effet, les patients déprimés présentent une augmentation des marqueurs inflammatoires, et l'administration de cytokines et d'autres stimuli inflammatoires peut induire des symptômes dépressifs. Des mécanismes par lesquels les cytokines ont accès au cerveau et influent sur les systèmes neurotransmetteurs liés à la dépression ont aussi été décrits, des résultats préliminaires ayant indiqué que le fait d'antagoniser des voies inflammatoires pouvait améliorer les symptômes dépressifs. L'adiposité semble une des premières sources d'inflammation dans la dépression. Le tissu adipeux est une source importante de facteurs inflammatoires comme les adipokines, les chémokines et les cytokines et il existe une relation bidirectionnelle entre adiposité et dépression. En effet, l'adiposité est associée au développement de la dépression et la dépression est associée à l'adiposité, traduisant un cercle vicieux potentiel entre ces pathologies centrées autour de l'inflammation. Des traitements visant ce cercle vicieux peuvent être particulièrement pertinents dans le traitement et la prévention de la dépression et de ses multiples comorbidités comme la maladie cardiovasculaire, le diabète et le cancer, qui sont aussi associés à la dépression et à l'inflammation.
Inflammation and depression
An overwhelming amount of evidence indicates that depressed patients exhibit increased markers of innate immune system activation and inflammation.Citation1 For example, in a meta-analysis of over 50 studies, Howren et alCitation2 found that the majority of studies show that depressed patients have elevations in the proinflammatory cytokines, interleukin (IL)-6, and IL-1β as well as the acute phase protein, C-reactive protein (CRP). A recent meta-analysis has revealed that the proinflammatory cytokine, tumor necrosis factor (TNF)-α, is also increased in patients with major depression.
In addition to the simple association between depression and inflammatory markers, the administration of inflammatory cytokines such as the innate immune cytokine, interferon (IFN)-α, can induce depression in a high proportion of treated patients.Citation3 In many ways this is parallel to what is referred to as sickness behavior in animals, which represents an adaptive response to acute infection and other sources of inflammation such as wounding.Citation4- Citation6 The sickness response can be induced in laboratory animals by the acute administration of proinflammatory cytokines such as IL-1β or TNF-αCitation7-Citation11 or indirectly via the induction of peripheral immune activation by stimuli such as bacterial endotoxin.Citation12,Citation13 Acute administration of endotoxin as well as other immune stimuli including typhoid vaccination causes a similar sickness syndrome in humans that includes depressed mood, decreased social interaction, sleep disturbance, and anhedonia.Citation14,Citation15 This constellation of symptoms, which parallels that found in major depression, has also been consistently observed during chronic administration of cytokines such as IFN-α and β for illnesses including hepatitis C, multiple sclerosis, and several types of cancers, including malignant melanoma.Citation3 To explore the degree to which cytokine-induced depression parallels depression in ostensibly medically healthy individuals, Capuron et alCitation8 compared 20 patients who were being treated with INFα for malignant melanoma with 28 medically healthy subjects with major depression using the Hamilton Rating Scale for Depression (HAM-D).Citation16 Forty-five percent of the IFN-α-treated patients developed major depression during the 12-week follow-up period. There were minimal differences in the severity of individual depressive symptoms between patients who became depressed during IFN-α treatment versus medically healthy depressed individuals, although IFN-α-treated depressed patients did exhibit more psychomotor retardation and weight loss, and the medically healthy depressed group experienced greater feelings of guilt and thoughts of suicide.Citation8 These results suggest that the depression induced by cytokines is remarkably similar to depression seen in medically healthy depressed patients.
Of note, the link between inflammation and depression may explain the frequent association between medical illnesses and depression.Citation17 As shown in Table I, while there are many medical conditions associated with increased rates of depression, the majority of these illnesses are also associated with increased inflammation, including not only infectious diseases and cancer but also cardiovascular disease and diabetes, both of which are now recognized to have an inflammatory component.Citation18 Of note, when depression occurs in the context of medical illness, it has been associated with increased concentrations of inflammatory cytokines. For example, several studies have shown that depressed patients with cancerCitation19-Citation22 or cardiovascular diseaseCitation23 have higher peripheral blood concentrations of IL6 and CRP. Moreover, depression scores have been shown to be strongly correlated with blood cytokine concentrations in these patients.Citation24
Table I. Inflammatory and noninflammatory diseases associated with elevated rates of depression. *Particularly in the context of combined chemoradiation
How do cytokines cause depression?
Access to the brain
Peripheral immune activation, such as that seen with local infection, wounding and/or psychological stress, induces release of IL-1α, IL-1β, IL-6, and TNF-α.Citation5,Citation25-Citation27 However, these cytokines are too large to freely pass through the blood-brain barrier, which raises the question of how a centrally mediated behavioral effect is achieved. Several pathways by which cytokine signals can access the brain have been identified. Local release of cytokines can stimulate peripheral afferent nerve fibers such as the vagus that innervate peripheral tissues, ultimately leading to activation of microglia, which can produce cytokines in the brain. In addition, “leaky” regions in the blood brain barrier such as the circumventricular organsCitation6,Citation28 allow access of peripheral inflammatory mediators to the brain. Cytokines in the peripheral circulation can also cross the blood-brain barrier via saturable active transport molecules expressed on brain endothelial cells.Citation29 Finally, in the context of chronic immune stimulation, microglia activated by peripheral TNF-α can produce the chemokine, monocyte chemoattractant protein (MCP)-1, which in turn, can attract monocytes into the brain parenchyma.Citation30
Impact on neurotransmitter metabolism
Once cytokine signals reach the brain, there is a rich literature indicating that they can interact with virtually every pathophysiologic domain relevant to depression, including marked effects on brain monoamines, which are the target of conventional antidepressant medications. Indeed, cytokines have been shown to influence central monoamine synthesis, release, and synaptic reuptake.
Serotonin
Serotonin is synthesized from tryptophan by tryptophan hydroxylase (TH) and aromatic amino acid decarboxylase (AAAD), and the amount of serotonin in brain is highly dependent on tryptophan availability.Citation31 Specifically, depletion of tryptophan rapidly leads to reduced brain serotonin levels, which in turn can precipitate depressive symptoms in vulnerable individuals.Citation31 Activation of the enzyme idoleamine 2,3-dioxygenase - IDO (and the related liver enzyme tryptophan 2,3dioxygenase) is an alternative pathway for tryptophan metabolism yielding kynurenine (KYN) and leading to tryptophan depletion and ultimately decreased serotonin in brain.Citation32,Citation33 Several cytokines and their signaling pathways have been shown to activate IDOCitation34,Citation35 (for a review see Shelton and Miller14). Interestingly, peripheral administration of the cytokine-inducer, lipopolysaccharide (LPS) to mice activates IDO and is associated with depressive-like behavior.Citation36 These LPS-induced behavioral changes can be reversed by IDO inhibition using the IDO antagonist 1-methyltryptophan.
IDO activation also has other effects that may be relevant to depression. For example, KYN is metabolized to kynurenic acid (KYNA), which antagonizes α7 nicotinic acetylcholine receptorsCitation32 and can reduce striatal dopamine release (see below)Citation37,Citation38 KYN is also metabolized to quinolinic acid (QUIN); QUIN leads to the generation of toxic lipid peroxides and activates N-methylD-aspartic acid (NMDA) receptors and the release of glutamate, all of which can contribute to neurotoxicity.Citation39 The impact of QUIN on neuronal integrity has been implicated in the pathophysiology of several degenerative neurological conditions including Alzheimer's, Huntington's, and Parkinson's diseases, amyotrophic lateral sclerosis, and human immunodeficiency virusrelated dementia.Citation40-Citation47 Of note, IFN-α therapy has also been shown to increase KYN/tryptophan ratios in humans, and KYN has been found to access the brain in IFN-α-treated patients where it is associated with increased cerebrospinal fluid (CSF) concentrations of both QUIN and KYNA.Citation48,Citation49 CSF KYN and QUIN were in turn correlated with depression in during IFN-α treatment.
Aside from its impact on tryptophan and serotonin synthesis, immune activation can also affect serotonin availability by acting on synaptic reuptake via the high-affinity serotonin transporter (5HTT).Citation50 Activation of p38 mitogen activated protein kinase (MAPK) by both IL-1β- and TNF-α leads to phosphorylation of 5HTT and increased neuronal uptake of serotonin.Citation51 ExpressionCitation52 and trafficking of 5HTT to the cell surfaceCitation53 is also increased by the activation of p38 MAPK. These effects of cytokines on 5HTT expression and function have been observed both in vitro and in vivo. Of note, polymorphisms in the 5HTT gene have also been associated with the development of depression during cytokine (IFN-α) administration.Citation54,Citation55
The relevance of immune-serotonin interactions is further supported by the observation that serotonin reuptake inhibitors can block the development of depressive symptoms in the context of immune activation. For example, one studyCitation56 randomly assigned 40 patients undergoing IFN-α therapy for malignant melanoma to treatment with the selective serotonin reuptake inhibitor (SSRI) paroxetine or placebo for 12 weeks. Eleven percent of the patients treated with paroxetine developed depression as compared to 45% of the placebo group. Almost all studies of SSRIsCitation57-Citation67 in the context of immune activation have demonstrated benefit in reversing or preventing immunotherapy-induced depressive symptoms.
Dopamine
In addition to serotonin, cytokine effects on dopamine metabolism may also be important in the pathophysiology of inflammation-induced depression. Reduced prefrontal and striatal dopamine activity is thought to be associated with symptoms of depression such as decreased motivation, psychomotor slowing, fatigue, and lack of response to rewarding stimuli.Citation68,Citation69 Positron emission tomography imaging studies in humans undergoing IFN-α therapy show increased striatal resting state glucose metabolism,Citation70,Citation71 which is believed to represent increased ocillatory burst activity in neurons normally under tonic inhibition by dopamine. Increased striatal resting state glucose metabolism is also found in other dopamine depletion states including Parkinson's disease.Citation72,Citation73 Animal studies show that immune stimulation by TNF-α and IFN-α reduce brain and CSF dopamine and its metabolites.Citation74,Citation75 In addition, prodopaminergic agents such as levodopa or psychostimulants improve fatigue and depression symptoms in patients undergoing IFN-α therapy as well as a variety of other conditions associated with inflammation including cancer and systemic HIV infection.Citation76-Citation78
There are several mechanisms by which dopamine may be depleted in the CNS during immune activation, aside from decreased dopamine release secondary to the α7 nicotinic acetylcholine receptor mechanism described above.Citation32 For example, IFN-αCitation79 administration to rodents has been associated with depletion of tetrahydrobiopterin (BH4), a cofactor for tyrosine hydroxylase, the rate-limiting enzyme in dopamine synthesis. Also, in a mechanism similar to the effects of immune activation on 5HTT, phosphorylation of the dopamine transporter (DAT) by MAPK kinase (MEK) has been shown to increase cell surface expression of DAT and uptake of dopamine.Citation80 Therefore, relative depletion of synaptic dopamine (via reduced synthesis and release and increased reuptake) may underlie some of the neurovegetative symptoms of sickness behavior and depression, such as low energy, reduced motivation, and reduced response to rewarding stimuli.Citation69,Citation81
The anti-inflammatory effects of antidepressant treatments and the antidepressant effects of anti-inflammatories
There have been a number of in vitro and in vivo studies of antidepressant medicationsCitation82-Citation98 and other antidepressant treatments such as electroconvulsive therapyCitation99
indicating that antidepressant treatments can reduce proinflammatory factors including IL2, IL-6, TNF-α, and IFN-γ.Citation1 In fact, the available evidence indicates that many antidepressant therapies induce a shift from a Th1 (proinflammatory) to a TH2/TH3 (anti-inflammatory) pattern.Citation82,Citation87,Citation88,Citation100,Citation101 The IFN-α to IL10 or IL4 ratio is a measure of relative TH1 to TH2-3 activity, and a number of studies indicate that antidepressants decrease this ratio.Citation82,Citation87,Citation88 Because these effects have been observed both in vitro and in vivo, they do not appear to be dependent on the actions of these drugs on monoamines such as norepinephrine or serotonin, suggesting a direct impact of antidepressant medications on cytokines.Citation95 Therefore, the mechanism of antidepressant action in the context of inflammation-induced depression may be a direct effect on inflammatory factors themselves.
There is also a small but significant literature indicating that anti-inflammatory drugs may produce antidepressant effects. Cyclooxygenase 2 (COX-2) activity is increased by proinflammatory cytokines, particularly IL-6, and it, in turn, activates the release of IL-1β and TNF-αCitation100 as well as prostaglandin E2 (PGE2), a central mediator of sickness behavior.Citation6 COX-2 inhibitors have been shown to reverse depression-like behaviors in animal models.Citation102-Citation104 In addition, the COX-2 rofecoxib has been shown to reduce depressive symptoms in patients with osteoarthritis.Citation105 Adjunctive treatment, the nonselective COX-1 and -2 antagonist acetylsalicylic acid (aspirin), increased remission rates in one open-label study of depressed patients previously nonresponsive to fluoxetine alone.Citation106 A prospective, double-blind, placebocontrolled trial of the COX-2 antagonist celecoxib (400 mg. per day) added to the norepinephrine reuptake inhibitor antidepressant reboxetine (4-10 mg per day) for 6 weeks showed greater effects of the combination treatment than reboxetine alone.Citation107
TNF receptor antagonists such as infliximab, adalimumab, golimumab, and certolizumab pegol, and the TNF receptor fusion protein etanercept have been developed in recent years to treat inflammatory and autoimmune diseases such as psoriasis, rheumatoid arthritis, and Crohn's disease. Direct actions in depressed patients have not yet been reported. However, one study of etanercept treatment of psoriasis did examine antidepressant effects.Citation108 Six hundred and eighteen patients with moderate to severe psoriasis received double-blind treatment with placebo or 50 mg twice weekly infusion treatment with etanercept for 12 weeks. Patients on etanercept had greater improvements on measures of depression (as measured by Beck Depression Inventory) than those on placebo. Notably, these improvements were not associated with reduction in psoriatic plaques or joint pain, which indicates a primary effect of TNF antagonism on depression, not simply a cosmetic or analgesic effect.Citation108 These effects were confirmed in subsequent longer term studies in psoriasis patientsCitation109,Citation110 and in patients with rheumatoid arthritis.Citation111 A similar effect has been shown with the TNF-α monoclonal antibody infliximab.Citation112,Citation113
Adiposity as a possible causal pathway to depression
In considering possible sources of inflammation leading to depression, there has been increasing interest in the role of obesity. Rates of overweight and obesity have increased tremendously in recent years in both adults and children.Citation114-Citation119 Along with this has been an epidemic of related metabolic conditions like type 2 diabetes, dyslipidemias, cardiovascular and fatty liver disease, and certain forms of cancer.Citation120-Citation122 The bulk of evidence links obesity and its attendant complications to inflammation.Citation123-Citation125 The possible relationship between depression and obesity appears to be bidirectional, as evidence indicates that being depressed also increases the risk for the subsequent development of obesity, probably mediated, in part, by inactivity.Citation126
Obesity as an inflammatory state
Adipose tissue is now understood as being a very complex organ system.Citation127 White adipose tissue (WAT) is the main location for long-term fat storage in the body. WAT, particularly in the abdomen, is the main contributor to metabolic diseases.Citation122,Citation128,Citation129 Adipocytes in WAT secrete a variety of hormones, inflammatory factors including cytokines (referred to as adipocytokines or adipokines).Citation130,Citation131 These factors include hormones traditionally associated with adipose tissue such as leptin, adiponectin, resistin, and visfatin; however, adipocytes can also secrete IL-6 and TNF-α.Citation130,Citation130 Nevertheless, one of the primary mechanisms for the induction of inflammation in adipose tissue is the secretion of chemokines, particularly MCP-1. MCP-1 attracts leukocytes such as macrophages, T lymphocytes, and dendritic cells to adipose tissue, which in turn secrete cytokines including IL1, IL6, and TNF-α.Citation132,Citation133 Thus, chemokines and cytokines produced by WAT may contribute to widespread immune activation, potentially causing or exacerbating diseases associated with inflammation such as type 2 diabetes, cardiovascular disease, cancer, and depression.Citation130
Leptin is another important peptide produced by adipocytes that regulates dietary intake. It regulates appetite by acting on leptin receptors in brain, particularly the hypothalamus.Citation134 In the case of obesity, a state of leptin resistance develops in which circulating levels are actually increased but responsiveness is reduced. Excess calories in the diet lead to leptin resistance; however, high-fructose feeding is a major contributor.Citation135,Citation136 Leptin is a member of the type I cytokine superfamily;Citation137,Citation138 it is involved in the modulation of white blood cell response, including T-cell activation and a shift to Th1 cytokine production.Citation137,Citation138 Resistin is another proinflammatory adipocytokine produced by both WAT and monocytes.Citation130 It sets up a positive inflammatory feedback system in which the secretion of resistin is increased by proinflammatory cytokines such as IL-1, IL-6, and TNF-α, but it also increases the production of these same cytokines by macrophages. Citation130,Citation139 By contrast, adiponectin increases fatty acid oxidation and reduces the synthesis of glucose in the liver.Citation137,Citation138 Adiponectin, whose levels are reduced in obese persons,Citation137 has a predominantly inhibitory role in Th1 immune responses, including the inhibition of IL-6 and TNF-α production and an increase in the anti-inflammatory cytokine IL10.Citation130 Therefore, dietary excess, leading to expansion of WAT, produces a shift in the pro- and anti-inflammatory mediators such as leptin, resistin, adiponectin, and other adipocytokines, leading to a general proinflammatory state.Citation14 This, then, contributes to metabolic derangements and disease such as dyslipidemias, cardiovascular disease, and type 2 diabetes.Citation123,Citation130,Citation140,Citation141
The activation of inflammatory factors related to obesity also appears to induce the IDO-KYN pathway. Plasma tryptophan concentrations are reducedCitation142 and the KYN/tryptophan ratio is increased in obese relative to lean individuals, indicating IDO activationCitation142,Citation143 Weight reduction by dietCitation142 or bariatric surgeryCitation143 restores a normal KYN/tryptophan balance. This is likely to be the result of a reduction in the proinflammatory state after weight loss.Citation143 It, then, appears that, like other inflammatory diseases, the immune activation found in obesity may shift metabolism from tryptophan to KYN, which may contribute to depression.
Adiposity and depression
Both depression and obesity, then, are associated with Th1 activation. However, is there evidence of a causal link in either direction - ie, from depression to obesity of viceversa? Some larger-scale epidemiological studies have failed to find a strong association between obesity and depression.Citation144,Citation145 Nevertheless, while cross-sectional studies do not show strong correlations between depression and obesity, longitudinal studies tell a very different storyCitation146-Citation149 A recent meta-analysis of 15 longitudinal studies showed a bidirectional association between depression and obesity (especially abdominal adiposity) in which prior obesity increases the risk for depression and depression increases the likelihood of subsequent obesityCitation150
To further investigate this bidirectional relationship especially as it pertains to inflammation, Miller et alCitation151 conducted a mediational analysisCitation152 evaluating the relationship between serum inflammatory markers (including IL-1β, IL-6, TNF-α, CRP, and MCP-1) in 50 physically healthy young adults with depression and 50 matched controls. IL-6, CRP, and BMI were elevated in the depressed sample compared with controls. When the relationship between depression and both IL-6 and CRP (but not IL-1β) were adjusted for BMI, the results became nonsignificant, indicating a mediational role for adiposity in the relationship between depression and IL-6 and CRP elevation.Citation151 A separate analysis of the same datasetCitation153 using structural equation modeling (SEM) estimated the relationship among depression, adiposity, leptin, and inflammation (IL-6 and CRP). The best fit model indicated that the primary causal pathway was from depression to adiposity to inflammation. This was interpreted as indicating that depression leads to increased adiposity (possibly through inactivity) which, in turn, leads to an increase in inflammatory markers.
Diet and depression
Diets in much of the world have shifted to high carbohydrates and a reduction in omega-3 (n-3) (unsaturated) compared with omega-6 (n-6) (saturated) fatty acids.Citation154 The intake of fish and other sources of n-3 fatty acids appear to be somewhat protective from certain metabolic conditions,Citation155-Citation163 and epidemiological studies have associated an increased relative intake of fish with a reduced risk for depression.Citation164 However, it does not seem to be primarily intake of fish per se, but so-called fatty fish with high n-3 concentration (eg, anchovy, sea bass, carp, dogfish, eel, halibut, herring, mackerel, mullet, fish, roe, salmon, sardine, trout, and tuna) that lend protection against both metabolic diseases and depression.Citation162,Citation163,Citation165,Citation166
The benefits of the Mediterranean diet pattern
Recent studies have found particular health benefits, including reduction in risk of depression, associated with the so-called Mediterranean Diet Pattern (MDP).Citation167 As noted in the seminal work by Willett et al,Citation167 this pattern of eating has been associated historically with good general health and longer life expectancy. This method “is based on food patterns typical of Crete, much of the rest of Greece, and southern Italy in the early 1960s” and “included regular physical activity... abundant plant foods (fruit, vegetables, breads, other forms of cereals, potatoes, beans, nuts, and seeds), fresh fruit as the typical daily dessert, olive oil as the principal source of fat, dairy products (principally cheese and yogurt), and fish and poultry consumed in low to moderate amounts, zero to four eggs consumed weekly, red meat consumed in low amounts, and wine consumed in low to moderate amounts, normally with meals.” This pattern of eating is characterized by lower saturated and total fat content. This manner of eating was shown recently to be associated with reduced risk for depression in a prospective study of the relationship between the MDP and health.Citation168,Citation169 A sample of 10 094 healthy persons in Spain were assessed using a validated 136-item item food frequency questionnaire to determine the relative adherence to the MDP, and followed for 4.4 years. Using the lowest adherence to the MDP as the reference condition, adjusted hazard ratios for depression for the higher categories of adherence ranged from 0.74 for modest adherence to 0.49. These results indicate a strong prospective protective effect for the MDP. Of relevance, earlier research found a strong inverse relationship between adherence to the MDP and serum IL-6 with a trend for CRP.Citation170
These data indicate that diet is an important contributor to inflammatory load and risk for depression. In addition to the n-3 to n-6 fatty acid ratio in the diet is the relative intake of carbohydrates, particular simple sugars. Carbohydrates in Western diets have also increased substantially in recent years. While the intake of certain refined sugars such as cane sugar has declined over the last 40 years, the total caloric load from sweeteners has increased; this has primarily been in the form of fructose, particularly in the form of high-fructose corn syrup (also known as “corn sugar”).Citation171 A high level of fructose intake is associated with obesity and metabolic diseases.Citation172-Citation177 Although the specific role of fructose intake, as opposed to increased total calories, has been questioned,Citation178 it is increasingly clear that high intake of fructose contributes uniquely to problems of obesityCitation179 and metabolic diseases such as cardiovascular disease, dyslipidemia, and type 2 diabetes.Citation180-Citation182 Fructose has a very high extraction ratio by the liver,Citation183 and does not contribute significantly to increases in insulinCitation184 or satiety signaling.Citation185 High levels of fructose loading in the liver leads to the synthesis of triglycerides, which contribute to liver and abdominal fat.Citation181,Citation184,Citation186 The shift in intake from proteins and “healthy” fats to saturated fats and carbohydrates, particularly fructose, has contributed to the worldwide epidemic of obesity.
Does n-3 fatty acid supplementation reduce depression?
A recent study indicates that not all n-3 fatty acids reduce inflammation; this study actually showed that docosahexanoic acid, one constituent of fish oil, may actually increased the ratio of interferon gamma to IL-10, indicating a proinflammatory effect. However, eicospentaenoic acid (EPA) did not show this effect; EPA has shown to reduce depressive symptoms in a few, smallerscale studies. One studyCitation187 randomized 70 persons with major depression not responsive to antidepressants to ethyl-eicosapentaenoic acid (e-EPA) (a specific n-3 fatty acid) 1, 2, or 4 g per day or placebo as add-on therapy.Citation187 Curiously, the 1 mg per day, but not 2 or 4 mg./day doses was significantly better than placebo. Subsequent studies have supported these results.Citation188-Citation190 Of note, a polymorphism in the gene for phospholipase A2, a key enzyme in the metabolism of polyunsaturated fatty acids, was associated with a 3-fold increase in the likelihood of developing major depression during IFN-α treatment as well as lower blood concentrations of EPA.Citation191
Diet, adiposity, and risk for depression in children
The increase in obesity in adults has been paralleled in children and adolescents,Citation119 along with an increase in inflammationCitation192,Citation193 and inflammatory diseases previously thought to occur mostly in adults: type 2 diabetes, fatty liver disease, cardiovascular disease, and dyslipidemia.Citation121,Citation194-Citation200 As described earlier for adults, the current evidence suggests a bidirectional relationship between obesity and depression in children.Citation201 Prior depression in childhood is a relatively strong predictor of the subsequent development of obesity, metabolic syndrome, and related diseases in adult life.Citation202-Citation204 Depression may increase risk by changes in diet, eating behavior, and inactivity.Citation126 Alternatively, baseline obesity may increase risk for depression via increases in inflammation as well as cultural aspects of beauty.Citation205 Obesity negatively impacts self-esteem based on cultural aspects of beauty and desirability.Citation205 Obesity also may contribute to risk for depression via effects on physical activity, sleep, and eating behavior.Citation205
Summary and conclusions
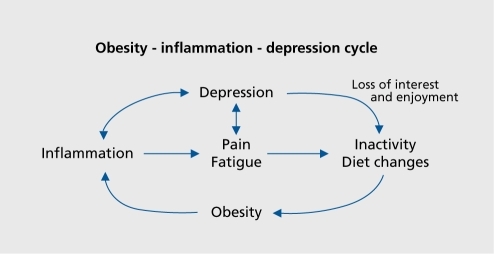
It seems clear at this point that inflammatory mediators, whether they are generated by specific diseases or administered exogenously (as with IFN therapy) can lead to depression. It also appears that a significant subset of depressed patients without known inflammatory disease have inherent upregulation of inflammatory factors, particularly IL-6, TNF-α, and CRP, without other known inflammatory disease.Citation1,Citation3,Citation14 As posited in this paper, one causal pathway for this increased inflammation may be overweight and obesity. Therefore, depression (and the inactivity and diet changes associated with it), obesity, and inflammation may represent a “vicious cycle” (). A person may enter this cycle at any pointobesity may lead to inflammation which leads to depression; depression may lead to inactivity and dietary changes, which lead to obesity leading to inflammation; inflammatory diseases may lead to both depression and inactivity, resulting in obesity. Western high-fat, high-carbohydrate diets and inactivity may lead to obesity inflammation, and depression. This cycle may also explain the common association between inflammatory diseases such as lupus or fibromyalgia and both depression and obesityCitation206-Citation218 Therefore, multiple, interacting factors may lead to a general decline in mental and physical health.
However, this cycle also provides multiple nodal points for both treatment and prevention. For example, children and adolescents at risk for depression (ie, with positive family history or those who have been traumatizedCitation219) may represent a group for whom targeted diet and exercise programs would be beneficial to help to prevent or reduce risk for depression. In addition, recent data indicate that overweight and obese patients have reduced response to antidepressant treatments.Citation220-Citation222 For example, a recent combined analysis of outcomes in three clinical trials of marketed antidepressants divided participants into normal weight (BMI<25), overweight (BMI 25-<30), and obese (BMI > 30).Citation221 The results indicated progressive resistance to antidepressant therapies from normal weight to obesity. Future interventions could target overweight and obesity as a possible remediable cause of treatment resistance. Depression is a complex condition with many potential causal pathways; two, possibly interrelated mechanisms, diet-associated overweight and obesity and inflammation have been reviewed. Although these mechanisms represent only two among many causal paths, they potentially explain many features, such as the common association between inflammatory diseases and depression risk. Nevertheless, there is cause for optimism for possible intervention strategies given the evidence for success of lifestyle modifications such as exercise, diet, and other weight loss approaches to inflammatory diseases a nd obesity.Citation116,Citation167,Citation207,Citation216,Citation223-Citation225
Selected abbreviations and acronyms
| 5HTT | = | serotonin transporter |
| CRP | = | C-reactive protein |
| IFN | = | interferon |
| IL | = | interleukin |
| KYN | = | kynurenine |
| TNF | = | tumor necrosis factor |
REFERENCES
- MillerAHMaleticVRaisonCL.Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression.Biol Psychiatry.20096573274119150053
- HowrenMBLamkinDMSulsJ.Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis.Psychosom Med.20097117118619188531
- RaisonCLCapuronLMillerAH.Cytokines sing the blues: inflammation and the pathogenesis of depression.Trends Immunol.200627243116316783
- HartBL.Biological basis of the behavior of sick animals.Neurosci Biobehav Rev.1988121231373050629
- DantzerRO'ConnorJCFreundGGJohnsonRWKelleyKW.From inflammation to sickness and depression: when the immune system subjugates the brain.Nat Rev Neurosci.20089465618073775
- DantzerR.Cytokine, sickness behavior, and depression.Immunol Allergy Clin North Am.20092924726419389580
- FelgerJCAlagbeOHuFet al.Effects of interferon-alpha on rhesus monkeys: a nonhuman primate model of cytokine-induced depression.Biol Psychiatry.2007621324133317678633
- CapuronLFornwaltFBKnightBTHarveyPDNinanPTMillerAH.Does cytokine-induced depression differ from idiopathic major depression in medically healthy individuals?J Affect Disord.200911918118519269036
- CapuronLMillerAH.Cytokines and psychopathology: lessons from interferon-alpha.Biol Psychiatry.20045681982415576057
- CapuronLGumnickJFMusselmanDLet al.Neurobehavioral effects of interferon-alpha in cancer patients: phenomenology and paroxetine responsiveness of symptom dimensions.Neuropsychopharmacology.20022664365211927189
- MatriscianoFBonaccorsoSRicciardiAet al.Changes in BDNF serum levels in patients with major depression disorder (MDD) after 6 months treatment with sertraline, escitalopram, or venlafaxine.J Psychiatr Res.20094324725418511076
- BlutheRMLayeSMichaudBCombeCDantzerRParnetP.Role of interleukin-1beta and tumour necrosis factor-alpha in lipopolysaccharideinduced sickness behaviour: a study with interleukin-1 type I receptor-deficient mice.Eur J Neurosci.2000124447445611122355
- DantzerR.Cytokine-induced sickness behavior: mechanisms and implications.Ann N Y Acad Sci.200193322223412000023
- SheltonRCMillerAH.Eating ourselves to death (and despair): The contribution of adiposity and inflammation to depression.Progr Neurobiol.201091275299
- DantzerRKelleyKW.Twenty years of research on cytokine-induced sickness behavior.Brain Behav Immun.20072115316017088043
- HamiltonM.A rating scale for depression.J Neurol Neurosurg Psychiatry.196023566214399272
- BentonTStaabJEvansDL.Medical co-morbidity in depressive disorders.Ann Clin Psychiatry.20071928930318058286
- HevenerALFebbraioMA.The 2009 Stock Conference Report: Inflammation, Obesity and Metabolic Disease.Obes Rev.20101163564420002885
- MusselmanDLMillerAHPorterMRet al.Higher than normal plasma interleukin-6 concentrations in cancer patients with depression: preliminary findings.Am J Psychiatry.20011581252125711481159
- SoygurHPalaogluOAkarsuESet al.Interleukin-6 levels and HPA axis activation in breast cancer patients with major depressive disorder.Prog Neuropsychopharmacol Biol Psychiatry.2007311242124717587477
- LutgendorfSKWeinribAZPenedoFet al.Interleukin-6, cortisol, and depressive symptoms in ovarian cancer patients.J Clin Oncol.2008264820482718779606
- JehnCFKuehnhardtDBartholomaeAet al.Biomarkers of depression in cancer patients.Cancer.20061072723272917036362
- MillerGEFreedlandKEDuntleySCarneyRM.Relation of depressive symptoms to C-reactive protein and pathogen burden (cytomegalovirus, herpes simplex virus, Epstein-Barr virus) in patients with earlier acute coronary syndromes.Am J Cardiol.20059531732115670537
- JacobsonCMRosenfeldBPessinHBreitbartW.Depression and IL-6 blood plasma concentrations in advanced cancer patients.Psychosomatics.200849646618212178
- DantzerRKelleyKW.Twenty years of research on cytokine-induced sickness behavior.Brain Behav Immun.20072115316017088043
- BierhausAWolfJAndrassyMet al.A mechanism converting psychosocial stress into mononuclear cell activation.Proc Natl Acad Sci U S A.20031001920192512578963
- PaceTWMletzkoTCAlagbeOet al.Increased stress-induced inflammatory responses in male patients with major depression and increased early life stress.Am J Psychiatry.20061631630163316946190
- ErmischARuhleHJLandgrafRHessJ.Blood-brain barrier and peptides.J Cereb Blood Flow Metab.198553503573897253
- QuanNBanksWA.Brain-immune communication pathways. BrainBehav Immunity.200721727735
- D'MelloCLeTSwainMG.Cerebral microglia recruit monocytes into the brain in response to tumor necrosis factoralpha signaling during peripheral organ inflammation.J Neurosci.2009292089210219228962
- DelgadoPLCharneyDSPriceLHAghajanianGKLandisHHeningerGR.Serotonin function and the mechanism of antidepressant action. Reversal of antidepressant-induced remission by rapid depletion of plasma tryptophan.Arch Gen Psychiatry.1990474114182184795
- SchwarczRPellicciariR.Manipulation of brain kynurenines: glial targets, neuronal effects, and clinical opportunities.J Pharmacol Exp Ther.200230311012235226
- SchrocksnadelKWirleitnerBWinklerCFuchsD.Monitoring tryptophan metabolism in chronic immune activation.Clin Chim Acta.2006364829016139256
- PopovAAbdullahZWickenhauserCet al.Indoleamine 2,3-dioxygenase-expressing dendritic cells form suppurative granulomas following Listeria monocytogenes infection.J Clin Invest.20061163160317017111046
- TakikawaOTagawaYIwakuraYYoshidaRTruscottRJ.Interferongamma-dependent/independent expression of indoleamine 2,3-dioxygenase. Studies with interferon-gamma-knockout mice.Adv Exp Med Biol.199946755355710721099
- O'ConnorJCLawsonMAAndreCet al.Lipopolysaccharide-induced depressive-like behavior is mediated by indoleamine 2,3-dioxygenase activation in mice.Mol Psychiatry.20091451152218195714
- RassoulpourAWuHQFerreSSchwarczR.Nanomolar concentrations of kynurenic acid reduce extracellular dopamine levels in the striatum.J Neurochem.20059376276515836634
- AmoriLWuHQMarinozziMPellicciariRGuidettiPSchwarczR.Specific inhibition of kynurenate synthesis enhances extracellular dopamine levels in the rodent striatum.Neuroscience.200915919620319138730
- JangSJeongHSParkJSet al.Neuroprotective effects of (-)-epigallocatechin-3-gallate against quinolinic acid-induced excitotoxicity via pi3k pathway and NO inhibition.Brain Res.201011313C253320025854
- Owe-YoungRWebsterNLMukhtarMet al.Kynurenine pathway metabolism in human blood-brain-barrier cells: implications for immune tolerance and neurotoxicity.J Neurochem.20081051346135718221377
- KwidzinskiEBechmannI.IDO expression in the brain: a double-edged sword.J Mol Med.2007851351135917594069
- BrewBJHalmanMCatalanJet al.Factors in AIDS dementia complex trial design: results and lessons from the abacavir trial.PLoS Clin Trials.20072e1317401456
- GuilleminGJKerrSJBrewBJ.Involvement of quinolinic acid in AIDS dementia complex.Neurotox Res.2005710312315639803
- ZadoriDKlivenyiPVamosEFulopFToldiJVecseiL.Kynurenines in chronic neurodegenerative disorders: future therapeutic strategies.J Neural Transm.20091161403140919618107
- VamosEPardutzAKlivenyiPToldiJVecseiL.The role of kynurenines in disorders of the central nervous system: possibilities for neuroprotection.J Neurol Sci.2009283212719268309
- MosleyRLBennerEJKadiuIet al.Neuroinflammation, oxidative stress and the pathogenesis of parkinson's disease.Clin Neurosci Res.2006626128118060039
- SasKRobotkaHToldiJVecseiL.Mitochondria, metabolic disturbances, oxidative stress and the kynurenine system, with focus on neurodegenerative disorders.J Neurol Sci.200725722123917462670
- WichersMCKoekGHRobaeysGVerkerkRScharpeSMaesM.IDO and interferon-alpha-induced depressive symptoms: a shift in hypothesis from tryptophan depletion to neurotoxicity.Mol Psychiatry.20051053854415494706
- RaisonCLDantzerRKelleyKWet al.CSF concentrations of brain tryptophan and kynurenines during immune stimulation with IFN-alpha: relationship to CNS immune responses and depression.Mol Psychiatry. In press.
- BlakelyRDBersonHE.Molecular biology of serotonin receptors and transporters.Clin Neuropharmacol.199215(suppl 1 Pt A)351A352A
- ZhuCBCarneiroAMDostmannWRHewlettWABlakelyRD.p38 MAPK activation elevates serotonin transport activity via a trafficking-independent, protein phosphatase 2A-dependent processJ Biol Chem.2005280156491565815728187
- TsaoCWLinYSChengJTet al.Interferon-alpha-induced serotonin uptake in Jurkat T cells via mitogen-activated protein kinase and transcriptional regulation of the serotonin transporter.J Psychopharmacol.20082275376018308792
- SamuvelDJJayanthiLDBhatNRRamamoorthyS.A role for p38 mitogen-activated protein kinase in the regulation of the serotonin transporter: evidence for distinct cellular mechanisms involved in transporter surface expression.J Neurosci.2005252941 15634764
- LotrichFEFerrellRERabinovitzMPollockBG.Risk for depression during interferon-alpha treatment is affected by the serotonin transporter polymorphism.Biol Psychiatry.20096534434818801474
- BullSJHuezo-DiazPBinderEBet al.Functional polymorphisms in the interleukin-6 and serotonin transporter genes, and depression and fatigue induced by interferon-alpha and ribavirin treatment.Mol Psychiatry.2009141095110418458677
- MusselmanDLLawsonDHGumnickJFet al.Paroxetine for the prevention of depression induced by high-dose interferon alfa.N Engl J Med.200134496196611274622
- RaisonCLWoolwineBJDemetrashviliMFet al.Paroxetine for prevention of depressive symptoms induced by interferon-alpha and ribavirin for hepatitis C.Aliment Pharmacol Ther.2007251163117417451562
- MorascoBJRifaiMALoftisJMIndestDWMolesJKHauserP.A randomized trial of paroxetine to prevent interferon-alpha-induced depression in patients with hepatitis C.J Affect Disord.2007103839017292481
- SchrammTMLawfordBRMacdonaldGACooksleyWG.Sertraline treatment of interferon-alfa-induced depressive disorder.Med J Aust.200017335936111062791
- SammutSBethusIGoodallGMuscatR.Antidepressant reversal of interferon-alpha-induced anhedonia.Physiol Behav.20027576577212020742
- LevensonJLFallonHJ.Fluoxetine treatment of depression caused by interferon-alpha.Am J Gastroenterol.1993887607618480744
- KrausMRSchaferASchottkerKet al.Therapy of interferon-induced depression in chronic hepatitis C with citalopram: a randomised, doubleblind, placebo-controlled study.Gut.20085753153618079286
- GleasonOCFucciJCYatesWRPhilipsenMA.Preventing relapse of major depression during interferon-alpha therapy for hepatitis C--A pilot study.Dig Dis Sci.2007522557256317436092
- SchaeferMSchwaigerMGarkischASet al.Prevention of interferonalpha associated depression in psychiatric risk patients with chronic hepatitis C.J Hepatol.20054279379815885349
- LagunoMBlanchJMurillasJet al.Depressive symptoms after initiation of interferon therapy in human immunodeficiency virus-infected patients with chronic hepatitis C.Antivir Ther.2004990590915651749
- LoftisJMSochermanREHowellCDet al.Association of interferonalpha-induced depression and improved treatment response in patients with hepatitis C.Neurosci Lett.2004365879115245784
- HauserPKhoslaJAuroraHet al.A prospective study of the incidence and open-label treatment of interferon-induced major depressive disorder in patients with hepatitis C.Mol Psychiatry.2002794294712399946
- SalamoneJDCorreaM.Dopamine/adenosine interactions involved in effort-related aspects of food motivation.Appetite.20095342242519635514
- DunlopBWNemeroffCB.The role of dopamine in the pathophysiology of depression.Arch Gen Psychiatry.20076432733717339521
- CapuronLPagnoniGDemetrashviliMFet al.Basal ganglia hypermetabolism and symptoms of fatigue during interferon-alpha therapy.Neuropsychopharmacology.2007322384239217327884
- JuenglingFDEbertDGutOet al.Prefrontal cortical hypometabolism during low-dose interferon alpha treatment.Psychopharmacology.200015238338911140330
- SpetsierisPGMoellerJRDhawanVIshikawaTEidelbergD.Visualizing the evolution of abnormal metabolic networks in the brain using PET.Computerized Medical Imaging and Graphics.2005192953067641174
- FeiginAFukudaMDhawanVet al.Metabolic correlates of levodopa response in Parkinson's disease.Neurology.2001572083208811739830
- FelgerJCAlagbeOHuFet al.Effects of interferon-alpha on rhesus monkeys: a nonhuman primate model of cytokine-induced depression.Biol Psychiatry.2007621324133317678633
- ShutoHKataokaYHorikawaTFujiharaNOishiR.Repeated interferon-[alpha] administration inhibits dopaminergic neural activity in the mouse brain.Brain Research.19977473483519046014
- LouJSKearnsGBeniceTOkenBSextonGNuttJ.Levodopa improves physical fatigue in Parkinson's disease: a double-blind, placebocontrolled, crossover study.Mov Disord.2003181108111414534913
- SchwartzALThompsonJAMasoodN.Interferon-induced fatigue in patients with melanoma: a pilot study of exercise and methylphenidate.Oncol Nurs Forum.200229E85E9012183762
- BreitbartWRosenfeldBKaimMFunesti-EschJ.A randomized, double-blind, placebo-controlled trial of psychostimulants for the treatment of fatigue in ambulatory patients with human immunodeficiency virus disease.Arch Intern Med.200116141142011176767
- KitagamiTYamadaKMiuraHHashimotoRNabeshimaTOhtaT.Mechanism of systemically injected interferon-alpha impeding monoamine biosynthesis in rats: role of nitric oxide as a signal crossing the blood-brain barrier.Brain Research.200397810411412834904
- MoronJAZakharovaIFerrerJVet al.Mitogen-activated protein kinase regulates dopamine transporter surface expression and dopamine transport capacity.J Neurosci.2003238480848813679416
- BrustolimDRibeiro-dos-SantosRKastREAltschulerELSoaresMB.A new chapter opens in anti-inflammatory treatments: the antidepressant bupropion lowers production of tumor necrosis factor-alpha and interferongamma in mice.Int Immunopharmacol.2006690390716644475
- Szuster-CiesielskaATustanowska-StachuraASlotwinskaMMarmurowska-MichalowskaHKandefer-SzerszenM.In vitro immunoregulatory effects of antidepressants in healthy volunteers.Pol J Pharmacol.20035535336214506314
- BengtssonBOZhuJThorellLHOlssonTLinkHWalinderJ.Effects of zimeldine and its metabolites, clomipramine, imipramine and maprotiline in experimental allergic neuritis in Lewis rats.J Neuroimmunol.1992391091221535634
- SongCDinanTLeonardBE.Changes in immunoglobulin, complement and acute phase protein levels in the depressed patients and normal controls.J Affect Disord.1994302832887516941
- ZhuJBengtssonBOMixEet al.Clomipramine and imipramine suppress clinical signs and T and B cell response to myelin proteins in experimental autoimmune neuritis in Lewis rats.J Autoimmun.1998113193279776709
- ZhuJBengtssonBOMixEThorellLHOlssonTLinkH.Effect of monoamine reuptake inhibiting antidepressants on major histocompatibility complex expression on macrophages in normal rats and rats with experimental allergic neuritis (EAN).Immunopharmacology.1994272252448071062
- MaesMSongCLinAHet al.Negative immunoregulatory effects of antidepressants: inhibition of interferon-gamma and stimulation of interleukin-10 secretion.Neuropsychopharmacology.19992037037910088138
- KuberaMLinAHKenisGBosmansEvan BDMaesM.AntiInflammatory effects of antidepressants through suppression of the interferon-gamma/interleukin-10 production ratio.J Clin Psychopharmacol.20012119920611270917
- KuberaMKenisGBosmansEet al.Suppressive effect of TRH and imipramine on human interferon-gamma and interleukin-10 production in vitro.Pol J Pharmacol.20005248148611334244
- KuberaMMaesMHolanVBasta-KaimARomanAShaniJ.Prolonged desipramine treatment increases the production of interleukin10, an anti-inflammatory cytokine, in C57BL/6 mice subjected to the chronic mild stress model of depression.J Affect Disord.20016317117811246093
- KuberaMSimbirtsevAMathisonRMaesM.Effects of repeated fluoxetine and citalopram administration on cytokine release in C57BL/6 mice.Psychiatry Res.200020;96255266
- KuberaMKenisGBosmansEet al.Plasma levels of interleukin-6, interleukin-10, and interleukin-1 receptor antagonist in depression: comparison between the acute state and after remission.Pol J Pharmacol.20005223724111055582
- MohrDCGoodkinDEIslarJHauserSLGenainCP.Treatment of depression is associated with suppression of nonspecific and antigen-specific T(H)1 responses in multiple sclerosis.Arch Neurol.2001581081108611448297
- SeidelAAroltVHunstigerMRinkLBehnischAKirchnerH.Cytokine production and serum proteins in depression.Scand J Immunol.1995415345387539545
- ObuchowiczEKowalskiJLabuzekKKrysiakRPendzichJHermanZS.Amitriptyline and nortriptyline inhibit interleukin-1 release by rat mixed glial and microglial cell cultures.Int J Neuropsychopharmacol.20069273515963243
- LanquillonSKriegJCBening-Abu-ShachUVedderH.Cytokine production and treatment response in major depressive disorder.Neuropsychopharmacology.20002237037910700656
- SluzewskaARybakowskiJKLaciakMMackiewiczASobieskaMWiktorowiczK.Interleukin-6 serum levels in depressed patients before and after treatment with fluoxetine.Ann N Y Acad Sci.19957624744767668562
- BasterziADAydemirCKisaCet al.IL-6 levels decrease with SSRI treatment in patients with major depression.Hum Psychopharmacol.20052047347616158446
- HestadKATonsethSStoenCDUelandTAukrustP.Raised plasma levels of tumor necrosis factor alpha in patients with depression: normalization during electroconvulsive therapy.J ECT.20031918318814657769
- MullerNSchwarzMJ.The immune-mediated alteration of serotonin and glutamate: towards an integrated view of depression.Mol Psychiatry.200712988100017457312
- MyintAMLeonardBESteinbuschHWKimYK.Th1, Th2, and Th3 cytokine alterations in major depression.J Affect Disord.20058816717316126278
- MyintAMSteinbuschHWGoegheganLLuchtmanDKimYKLeonardBE.Effect of the COX-2 inhibitor celecoxib on behavioural and immune changes in an olfactory bulbectomised rat model of depression.Neuroimmunomodulation.200714657117713352
- GuoJYLiCYRuanYPet al.Chronic treatment with celecoxib reverses chronic unpredictable stress-induced depressive-like behavior via reducing cyclooxygenase-2 expression in rat brain.Eur J Pharmacol.2009612546019356723
- KumariBKumarADhirA.Protective effect of non-selective and selective COX-2-inhibitors in acute immobilization stress-induced behavioral and biochemical alterations.Pharmacol Rep.20075969970718195459
- Collantes-EstevezEFernandez-PerezC.Improved control of osteoarthritis pain and self-reported health status in non-responders to celecoxib switched to rofecoxib: results of PAVIA, an open-label post-marketing survey in Spain.Curr Med Res Opin.20031940241013678477
- MendlewiczJKriwinPOswaldPSoueryDAlboniSBrunelloN.Shortened onset of action of antidepressants in major depression using acetylsalicylic acid augmentation: a pilot open-label study.Int Clin Psychopharmacol.200621227231 16687994
- MullerNSchwarzMJDehningSet al.The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a doubleblind, randomized, placebo controlled, add-on pilot study to reboxetine.Mol Psychiatry.20061168068416491133
- TyringSGottliebAPappKet al.Etanercept and clinical outcomes, fatigue, and depression in psoriasis: double-blind placebo-controlled randomised phase III trial.Lancet.2006367293516399150
- DaudenEGriffithsCOrtonneJPet al.Improvements in patientreported outcomes in moderate-to-severe psoriasis patients receiving continuous or paused etanercept treatment over 54 weeks: the CRYSTEL study.J Eur Acad Dermatol Venereol.2009231374138219563497
- KrishnanRCellaDLeonardiCet al.Effects of etanercept therapy on fatigue and symptoms of depression in subjects treated for moderate to severe plaque psoriasis for up to 96 weeks.Br J Dermatol.20071571275127717916204
- KekowJMootsRJEmeryPet al.Patient-reported outcomes improve with etanercept plus methotrexate in active early rheumatoid arthritis and the improvement is strongly associated with remission: the COMET trial.Ann Rheum Dis.20106922222519293160
- FeldmanSRGottliebABBalaMet al.Infliximab improves healthrelated quality of life in the presence of comorbidities among patients with moderate-to-severe psoriasis.Br J Dermatol.200815970471018627375
- LichtensteinGRBalaMHanCDeWoodyKSchaibleT.Infliximab improves quality of life in patients with Crohn's disease.Inflamm Bowel Dis2002823724312131606
- BornsteinSREhrhart-BornsteinMWongMLLicinioJ.Is the worldwide epidemic of obesity a communicable feature of globalization?Exp Clin Endocrinol Diabetes.2008116 (suppl 1)S30S3218777450
- CumurcuBEOzyurtHEtikanIDemirSKarlidagRTotal antioxidant capacity and total oxidant status in patients with major depression: impact of antidepressant treatment.Psychiatry Clin Neurosci.20096363964519674383
- WilbornCBeckhamJCampbellBet al.Obesity: prevalence, theories, medical consequences, management, and research directions.J Int Soc Sports Nutr.2005243118500955
- WangYLobsteinT.Worldwide trends in childhood overweight and obesity.Int J Pediatr Obes.20061112517902211
- MacPheeM.Global childhood obesity: how to curb an epidemic.J Pediatr Nurs.2008231418207042
- Ben-SeferEBen-NatanMEhrenfeldM.Childhood obesity: current literature, policy and implications for practice.Int Nurs Rev.20095616617319646165
- BellentaniSMarinoM.Epidemiology and natural history of non-alcoholic fatty liver disease (NAFLD).Ann Hepatol.20098(suppl 1)S48S4S819381118
- GoldenSHRobinsonKASaldanhaIAntonBLadensonPW.Clinical review: prevalence and incidence of endocrine and metabolic disorders in the United States: a comprehensive review.J Clin Endocrinol Metab.2009941853187819494161
- HevenerALFebbraioMA.The 2009 Stock Conference Report: Inflammation, Obesity and Metabolic Disease.Obes Rev.20101163564420002885
- ShoelsonSEHerreroLNaazA.Obesity, inflammation, and insulin resistance.Gastroenterology.20071322169218017498510
- SutherlandJPMcKinleyBEckelRH.The metabolic syndrome and inflammation.Metab Syndr Relat Disord.200428210418370640
- DandonaPAljadaAChaudhuriAMohantyPGargR.Metabolic syndrome: a comprehensive perspective based on interactions between obesity, diabetes, and inflammation.Circulation.20051111448145415781756
- MillerGEFreedlandKECarneyRMStetlerCABanksWA.Pathways linking depression, adiposity, and inflammatory markers in healthy young adults.Brain Behav Immun.20031727628512831830
- MathieuPPoirierPPibarotPLemieuxIDespresJP.Visceral obesity: the link among inflammation, hypertension, and cardiovascular disease.Hypertension.20095357758419237685
- CalabroPYehET.Intra-abdominal adiposity, inflammation, and cardiovascular risk: new insight into global cardiometabolic risk.Curr Hypertens Rep.200810323818367024
- DespresJPArsenaultBJCoteMCartierALemieuxI.Abdominal obesity: the cholesterol of the 21st century?Can J Cardiol.200824 (suppl D)7D12D
- TilgHMoschenAR.Adipocytokines: mediators linking adipose tissue, inflammation and immunity.Nat Rev Immunol.2006677278316998510
- TilgHMoschenAR.Inflammatory mechanisms in the regulation of insulin resistance.Mol Med.20081422223118235842
- CarrMWRothSJLutherERoseSSSpringerTA.Monocyte chemoattractant protein 1 acts as a T-lymphocyte chemoattractant.Proc Natl Acad Sci U S A.199491365236568170963
- XuLLWarrenMKRoseWLGongWWangJM.Human recombinant monocyte chemotactic protein and other C-C chemokines bind and induce directional migration of dendritic cells in vitro.J Leukoc Biol.1996603653718830793
- BrennanAMMantzorosCS.Drug insight: the role of leptin in human physiology and pathophysiology - emerging clinical applications.Nat Clin Pract End Met.20062318327
- ShapiroAMuWRoncalCChengKYJohnsonRJScarpacePJ.Fructose-induced leptin resistance exacerbates weight gain in response to subsequent high-fat feeding.Am J Physiol Regul Integr Comp Physiol.2008295R1370R137518703413
- VasselliJR.Fructose-induced leptin resistance: discovery of an unsuspected form of the phenomenon and its significance. Focus on “Fructoseinduced leptin resistance exacerbates weight gain in response to subsequent high-fat feeding,” by Shapiro, et al.Am J Physiol Regul Integr Comp Physiol.2008295R1365R136918784330
- LagoFDieguezCGomez-ReinoJGualilloO.Adipokines as emerging mediators of immune response and inflammation.Nat Clin Pract Rheumatol.2007371672418037931
- LagoFGomezRGomez-ReinoJJDieguezCGualilloO.Adipokines as novel modulators of lipid metabolism.Trends Biochem Sci.20093450051019729309
- SilswalNSinghAKArunaBMukhopadhyaySGhoshSEhteshamNZ.Human resistin stimulates the pro-inflammatory cytokines TNF-[alpha] and IL-12 in macrophages by NF-[kappa]B-dependent pathway.Biochem Biophys Res Comm.20053341092110116039994
- BaysHEGonzalez-CampoyJMBrayGAet al.Pathogenic potential of adipose tissue and metabolic consequences of adipocyte hypertrophy and increased visceral adiposity.Exp Rev Cardiovasc Ther.20086343368
- GustafsonB.Adipose tissue, inflammation and atherosclerosis.J Atheroscler Thromb.20101733234120124732
- BreumLRasmussenMHHilstedJFernstromJD.Twenty-four-hour plasma tryptophan concentrations and ratios are below normal in obese subjects and are not normalized by substantial weight reduction.Am J Clin Nutr.2003771112111812716660
- BrandacherGWinklerCAignerFet al.Bariatric surgery cannot prevent tryptophan depletion due to chronic immune activation in morbidly obese patients.Obes Surg.20061654154816687019
- MurphyJMHortonNJBurkeJDJr.et al.Obesity and weight gain in relation to depression: findings from the Stirling County Study.Int J Obes (Lond).20093333534119139752
- AtlantisEBakerM.Obesity effects on depression: systematic review of epidemiological studies.Int J Obes (Lond).20083288189118414420
- VogelzangsNKritchevskySBBeekmanATet al.Obesity and onset of significant depressive symptoms: results from a prospective communitybased cohort study of older men and women.J Clin Psychiatry.20107139139920021992
- VogelzangsNKritchevskySBBeekmanATet al.Depressive symptoms and change in abdominal obesity in older persons.Arch Gen Psychiatry.2008651386139319047525
- VogelzangsNKritchevskySBBeekmanATFet al.Depressive symptoms and change in abdominal obesity in older persons.Arch Gen Psychiatry.2008651386139319047525
- RivenesACHarveySBMykletunA.The relationship between abdominal fat, obesity, and common mental disorders: Results from the HUNT Study.J Psychosom Res.20096626927519302883
- LuppinoFSde WitLMBouvyPFet al.Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies.Arch Gen Psychiatry.20106722022920194822
- MillerGEStetlerCACarneyRMFreedlandKEBanksWA.Clinical depression and inflammatory risk markers for coronary heart disease.Am J Cardiol.2002901279128312480034
- BaronRMKennyDA.The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations.J Pers Soc Psychol.198651117311823806354
- MillerGEFreedlandKECarneyRMStetlerCABanksWA.Pathways linking depression, adiposity, and inflammatory markers in healthy young adults.Brain Behav Immun.20031727628512831830
- ZimmermannMBAeberliI.Dietary determinants of subclinical inflammation, dyslipidemia and components of the metabolic syndrome in overweight children: a review.Int J Obes (Lond).200832(suppl 6)S11S1819079275
- Rodriguez-LeyvaDDupasquierCMcCulloughRPierceGN.The cardiovascular effects of flaxseed and its omega-3 fatty acid, alpha-linolenic acid.Can J Cardiol.20102648949621076723
- Bushkin-BedientSCarpenterDO.Benefits versus risks associated with consumption of fish and other seafood.Rev Environ Health.20102516119121038755
- ChangCLSeoTDuCBAcciliDDeckelbaumRJ.n-3 Fatty acids decrease arterial low-density lipoprotein cholesterol delivery and lipoprotein lipase levels in insulin-resistant mice.Arterioscler Thromb Vasc Biol.2010302510251720930167
- HassanKSHassanSKHijaziEGKhazimKO.Effects of omega-3 on lipid profile and inflammation markers in peritoneal dialysis patients.Ren Fail.2010321031103520863205
- DefilippisAPBlahaMJJacobsonTA.Omega-3 fatty acids for cardiovascular disease prevention.Curr Treat Options Cardiovasc Med.20101236538020842560
- HarrisWS.The omega-3 index: clinical utility for therapeutic intervention.Curr Cardiol Rep.20101250350820809235
- MazzaMPomponiMJaniriLBriaPMazzaS.Omega-3 fatty acids and antioxidants in neurological and psychiatric diseases: an overview.Prog Neuropsychopharmacol Biol Psychiatry.200731122616938373
- JuturuV.Omega-3 fatty acids and the cardiometabolic syndrome.J Cardiometab Syndr.2008324425319040594
- RuxtonCHReedSCSimpsonMJMillingtonKJ.The health benefits of omega-3 polyunsaturated fatty acids: a review of the evidence.J Hum Nutr Diet.20041744945915357699
- KraguljacNVMontoriVMPavuluriMChaiHSWilsonBSUnalSS.Efficacy of omega-3 Fatty acids in mood disorders - a systematic review and metaanalysis.Psychopharmacol Bull.200942395419752840
- AstorgPCouthouisABertraisSet al.Association of fish and longchain n-3 polyunsaturated fatty acid intakes with the occurrence of depressive episodes in middle-aged French men and women.Prostaglandins, Leukotrienes Essential Fatty Acids.200878 171182
- MalhotraAKGoldmanDMazzantiCCliftonABreierAPickarD.A functional serotonin transporter (5-HTT) polymorphism is associated with psychosis in neuroleptic-free schizophrenics.Molecular Psychiatry.199833283329702741
- WillettWCSacksFTrichopoulouAet al.Mediterranean diet pyramid: a cultural model for healthy eating.Am J Clin Nutr.1995611402S1406S7754995
- TortosaABes-RastrolloMSanchez-VillegasAet al.Mediterranean diet inversely associated with the incidence of metabolic syndrome.Diabetes Care.2007302957295917712023
- Sanchez-VillegasADelgado-RodriguezMAlonsoAet al.Association of the Mediterranean dietary pattern with the incidence of depression: the Seguimiento Universidad de Navarra/University of Navarra Follow-up (SUN) Cohort.Arch Gen Psychiatry.2009661090109819805699
- DaiJMillerAHBremnerJDet al.Adherence to the Mediterranean diet is inversely associated with circulating interleukin-6 among middleaged men: a twin study.Circulation.200811716917518086924
- MarriottBPColeNLeeE.National estimates of dietary fructose intake increased from. 1977 to 2004 in the United States.J Nutr.20091391228S1235S19403716
- JohnsonRJSegalMSSautinYet al.Potential role of sugar (fructose) in the epidemic of hypertension, obesity and the metabolic syndrome, diabetes, kidney disease, and cardiovascular disease.Am J Clin Nutr.20078689990617921363
- StanhopeKLHavelPJ.Endocrine and metabolic effects of consuming beverages sweetened with fructose, glucose, sucrose, or high-fructose corn syrup.Am J Clin Nutr.2008881733S1737S19064538
- SchaeferEJGleasonJADansingerML.Dietary fructose and glucose differentially affect lipid and glucose homeostasis.J Nutr.20091391257S1262S19403705
- StanhopeKLHavelPJ.Fructose consumption: considerations for future research on its effects on adipose distribution, lipid metabolism, and insulin sensitivity in humans.J Nutr.20091391236S1241S19403712
- DolanLCPotterSMBurdockGA.Evidence-based review on the effect of normal dietary consumption of fructose on development of hyperlipidemia and obesity in healthy, normal weight individuals.Crit Rev Food Sci Nutr.201050538420047139
- TappyLLeKA.Metabolic effects of fructose and the worldwide increase in obesity.Physiol Rev.201090234620086073
- WhiteJS.Misconceptions about high-fructose corn syrup: is it uniquely responsible for obesity, reactive dicarbonyl compounds, and advanced glycation endproducts?J Nutr.20091391219S1227S19386820
- BocarslyMEPowellESAvenaNMHoebelBG.High-fructose corn syrup causes characteristics of obesity in rats: Increased body weight, body fat and triglyceride levels.Pharmacol Biochem Behav.20109710110620219526
- TappyLLeKA.Metabolic effects of fructose and the worldwide increase in obesity.Physiol Rev.201090234620086073
- FiglewiczDPIoannouGBennettJJKittlesonSSavardCRothCL.Effect of moderate intake of sweeteners on metabolic health in the rat.Physiol Behav.20099861862419815021
- AngelopoulosTJLowndesJZukleyLet al.The effect of high-fructose corn syrup consumption on triglycerides and uric acid.J Nutr.20091391242S1245S19403709
- SchaeferEJGleasonJADansingerML.Dietary fructose and glucose differentially affect lipid and glucose homeostasis.J Nutr.20091391257S1262S19403705
- BascianoHFedericoLAdeliK.Fructose, insulin resistance, and metabolic dyslipidemia.Nutr Metab (Lond).20052515723702
- MoranTH.Fructose and satiety.J Nutr.20091391253S1256S19403706
- StanhopeKLHavelPJ.Fructose consumption: potential mechanisms for its effects to increase visceral adiposity and induce dyslipidemia and insulin resistance.Curr Opin Lipidol.200819162418196982
- PeetM.Eicosapentaenoic acid in the treatment of schizophrenia and depression: rationale and preliminary double-blind clinical trial results.Prostaglandins Leukot Essent Fatty Acids.20036947748514623502
- FrangouSLewisMMcCroneP.Efficacy of ethyl-eicosapentaenoic acid in bipolar depression: randomised double-blind placebo-controlled study.Br J Psychiatry .2006188465016388069
- MischoulonDPapakostasGIDordingCMet al.A double-blind, randomized controlled trial of ethyl-eicosapentaenoate for major depressive disorder.J Clin Psychiatry.2010701636164419709502
- NemetsBStahlZBelmakerRH.Addition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorder.Am J Psychiatry.200215947747911870016
- SuKP.Mind-body interface: the role of n-3 fatty acids in psychoneuroimmunology, somatic presentation, and medical illness comorbidity of depression.Asia Pac J Clin Nutr.200817 (suppl 1)15115718296325
- TamCSClementKBaurLATordjmanJ.Obesity and low-grade inflammation: a paediatric perspective.Obes Rev.20101111812619845868
- WarnbergJMarcosA.Low-grade inflammation and the metabolic syndrome in children and adolescents.Curr Opin Lipidol.200819111518196981
- MollestonJPWhiteFTeckmanJFitzgeraldJF.Obese children with steatohepatitis can develop cirrhosis in childhood.Am J Gastroenterol.2002972460246212358273
- RobertsEA.Nonalcoholic steatohepatitis in children.Curr Gastroenterol Rep.2003525325912734049
- NandaK.Non-alcoholic steatohepatitis in children.Pediatr Transplant.2004861361815598336
- SemizSRotaSOzdemirOOzdemirAKaptanogluB.Are C-reactive protein and homocysteine cardiovascular risk factors in obese children and adolescents?Pediatr Int.20085041942319143962
- AlisiAMancoMPaneraNNobiliV.Association between type two diabetes and non-alcoholic fatty liver disease in youth.Ann Hepatol.20098 (suppl 1)S44S5019381124
- ChiarelliFMarcovecchioML.Insulin resistance and obesity in childhood.Eur J Endocrinol.2008159 (suppl 1)S67S7418805916
- EyzaguirreFMericqV.Insulin resistance markers in children.Horm Res.200971657419129710
- McElroySLKotwalRMalhotraSNelsonEBKeckPENemeroffCB.Are mood disorders and obesity related? A review for the mental health professional.J Clin Psychiatry.20046563465115163249
- GoodwinRDSouranderADuarteCSet al.Do mental health problems in childhood predict chronic physical conditions among males in early adulthood? Evidence from a community-based prospective study.Psychol Med.20093930131118507873
- HaslerGPineDSGammaAet al.The associations between psychopathology and being overweight: a. 20-year prospective study.Psychol Med.2004341047105715554575
- Pulkki-RabackLElovainioMKivimakiMet al.Depressive symptoms and the metabolic syndrome in childhood and adulthood: a prospective cohort study.Health Psychol.20092810811619210024
- ReevesGMPostolacheTTSnitkerS.Childhood obesity and depression: connection between these growing problems in growing children.Int J Child Health Hum Dev.2008110311418941545
- OkifujiADonaldsonGWBarckLFinePG.Relationship between fibromyalgia and obesity in pain, function, mood, and sleep.J Pain.2010111329133720542742
- ArranzLICanelaMARafecasM.Fibromyalgia and nutrition, what do we know?Rheumatol Int.2010301417142720358204
- WrightLJSchurENoonanCAhumadaSBuchwaldDAfariN.Chronic pain, overweight, and obesity: findings from a community-based twin registry.J Pain.20101162863520338816
- MorkPJVasseljenONilsenTI.Association between physical exercise, body mass index, and risk of fibromyalgia: longitudinal data from the Norwegian Nord-Trondelag Health Study.Arthritis Care Res (Hoboken ).20106261161720191480
- OliverJESilmanAJ.What epidemiology has told us about risk factors and aetiopathogenesis in rheumatic diseases.Arthritis Res Ther.20091122319490599
- OkifujiABradshawDHOlsonC.Evaluating obesity in fibromyalgia: neuroendocrine biomarkers, symptoms, and functions.Clin Rheumatol.20092847547819172342
- TrockD.Tired, achy, and overweight, the inflammatory nature of obesity.J Clin Rheumatol.2009155019131768
- NeumannLLernerEGlazerYBolotinASheferABuskilaD.A crosssectional study of the relationship between body mass index and clinical characteristics, tenderness measures, quality of life, and physical functioning in fibromyalgia patients.Clin Rheumatol.2008271543154718622575
- ZhangZCherryholmesGMaoAet al.High plasma levels of MCP-1 and eotaxin provide evidence for an immunological basis of fibromyalgia.Exp Biol Med (Maywood).20082331171118018535166
- BennettRMJonesJTurkDCRussellIJMatallanaL.An internet survey of 2,596 people with fibromyalgia.BMC Musculoskelet Disord.200782717349056
- JonesKDAdamsDWinters-StoneKBurckhardtCS.A comprehensive review of 46 exercise treatment studies in fibromyalgia (1988-2005).Health Qual Life Outcomes.200646716999856
- KatzPGregorichSYazdanyJet al.Obesity and its measurement in a community-based sample of women with systemic lupus erythematosus.Arthritis Care Res (Hoboken).2010
- HahnBHLourenccoEVMcMahonMet al.Pro-inflammatory highdensity lipoproteins and atherosclerosis are induced in lupus-prone mice by a high-fat diet and leptin.Lupus.20101991391720410156
- ParasMLMuradMHChenLPet al.Sexual abuse and lifetime diagnosis of somatic disorders: a systematic review and meta-analysis.JAMA.200930255056119654389
- PapakostasGIPetersenTIosifescuDVet al.Obesity among outpatients with major depressive disorder.Int J Neuropsychopharmacol.20058596315361263
- OskooilarNWilcoxCSTongMLGroszDE.Body mass index and response to antidepressants in depressed research subjects.J Clin Psychiatry.2009701609161020031110
- MarkowitzSFriedmanFAArentSM.Understanding the relation between obesity and depression: causal mechanisms and implications for treatment.Clin Psychol Sci Pract.200815120
- CiceroAFDerosaGBoveMDiGVGaddiAVBorghiC.Effect of a sequential training programme on inflammatory, prothrombotic and vascular remodelling biomarkers in hypertensive overweight patients with or without metabolic syndrome.Eur J Cardiovasc Prev Rehabil.20091669870419741540
- ForsytheLKWallaceJMLivingstoneMB.Obesity and inflammation: the effects of weight loss. 200821117133
- KelishadiRHashemiMMohammadifardNAsgarySKhavarianN.Association of changes in oxidative and proinflammatory states with changes in vascular function after a lifestyle modification trial among obese children.Clin Chem.20085414715317998270