Abstract
Neurodevelopmental changes over the lifespan, from childhood through adulthood into old age, have important implications for the onset, presentation, course, and treatment of anxiety disorders. This article presents data on anxiety disorders as they appear in older adults, as compared with earlier in life. In this article, we focus on aging-related changes in the epidemiology, presentation, and treatment of anxiety disorders. Also, this article describes some of the gaps and limitations in our understanding and suggests research directions that may elucidate the mechanisms of anxiety disorder development later in life. Finally we describe optimal management of anxiety disorders across the lifespan, in “eight simple steps” for practitioners.
Los cambios en el neurodesarrollo durante el curso de la vida, desde la niñez pasando por la adultez y hasta la vejez, tienen importantes repercusiones para la instalación, presentación, curso y tratamiento de los trastornos ansiosos. Este artículo presenta datos acerca de los trastornos ansiosos en la forma cómo ellos aparecen en los adultos mayores en comparación con los más jóvenes. Este artículo se centra en los cambios relacionados con la edad en la epidemiología, presentación y tratamiento de los trastornos ansiosos. Además, este articulo describe algunas de las brechas y limitaciones en nuestra comprensión del trastorno ansioso y sugiere directrices de la investigación que puedan aclarar los mecanismos de aquellos cuadros que se desarrollan más tardíamente en la vida. Finalmente se describe el manejo óptimo para los clínicos de los trastornos ansiosos a lo largo de la vida en “ocho pasos simples”.
Les modifications neurodéveloppementales survenant tout au long de la vie, de l'enfance à l'âge adulte jusqu'à la vieillesse, ont des implications importantes sur la survenue, le cours et le traitement des troubles anxieux. Cet article présente des données sur les troubles anxieux tels qu'ils apparaissent chez les adultes plus âgés, comparés à ceux moins avancés en âge. Nous nous intéressons ici aux modifications liées au vieillissement dans l'épidémiologie, la présentation et le traitement des troubles anxieux. Cet article décrit aussi les lacunes et les limites de notre compréhension et suggère des directions de recherche pouvant élucider les mécanismes du développement du trouble anxieux plus tard dans la vie. Enfin, nous décrivons la prise en charge optimale des troubles anxieux au cours de la vie, en « huit étapes simples » pour le médecin.
Introduction
Picture the world in 2050. A demographic shift towards older age that began generations ago will have reached its peak, and 2 billion individuals will be aged 60 and older.Citation1 In the United States and much of Europe, one in three persons will be in this old-age demographic (compared with one in five today). It is increasingly clear that the common mental disorders of emotion—anxiety disorders and unipolar depression—are a terrible scourge across the lifespan: they not only induce significant misery and suffering for the patient and his/her whole family, but with increasing age they become increasingly deleterious to health and cognition, even increasing mortality risk in older adults. Given such deleterious effects, understanding the common mental disorders in this large and growing demographic would seem to be a question of some importance.
The last decade has seen several advances in our knowledge of the epidemiology, course, and treatment of anxiety disorders, and how this changes into old age. Yet, even though anxiety disorders are the most common mental disorders in older adults, there has been scant attention paid to some major issues regarding anxiety disorders in older adults.
In this review, we present a lifespan view of anxiety disorders, primarily from an aging perspective, but also with an examination of the changing picture of anxiety disorders and their treatment throughout the lifespan from childhood to old age. This review will focus on three aspects of anxiety disorders: epidemiology, presentation, and treatment. One of the major arguments that will be advanced is that anxiety disorders are common in older adults and cause considerable distress and functional impairment, and that, absent improvements in detection and management, geriatric anxiety disorders will become an increasing human and economic burden. We will also argue that much is known already about the optimal management of anxiety disorders across the lifespan into old age, such that practitioners could greatly improve outcomes of their patients with these common problems even now, if they follow eight simple management steps which are outlined.
Additionally, it will be obvious from reading this review that significant gaps remain in our understanding of many aspects of anxiety disorders, particularly in older adults. Throughout the review, we will point out these gaps in our knowledge, and we will finish with a brief prospectus on research that could begin to fill these gaps.
Epidemiology of anxiety disorders throughout the lifespan
Table I shows prevalence estimates from several large epidemiologic studies that focused on elderly persons. As a whole, the studies suggest that generalized anxiety disorder (GAD) is the most common anxiety disorder and is as common, or more common, in older as in younger adults; other anxiety disorders are less common. Several excellent reviews of the epidemiology of late -life anxiety disorders existCitation2-Citation4 and we will not recapitulate them, but will note two key and related points from them. First, epidemiologic studies have produced wide variations in prevalence estimates of anxiety disorders in elderly persons. One systematic review found 28 epidemiological studies of anxiety symptoms, or disorders, in older adults: 19 in community samples, and nine in clinical samples. The range of anxiety disorder prevalence estimates in those studies varied markedly, ranging from 1.2% to 15% in community samples and from 1% to 28% in medical settings. The prevalence of clinically significant anxiety symptoms ranges from 15% to 52% in community samples and 15% to 56% in medical settings.Citation2 Second, anxiety disorders (and symptoms), already difficult to measure accurately in young adults, are more difficult to assess in older adults. In a section below, we will discuss difficulties in the assessment and diagnosis of anxiety disorders and symptoms in older adults and how these might affect prevalence estimates.
Table I Prevalence estimates for anxiety disorders in older adults from five community studies. GAD, generalized anxiety disorder; OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder; *prevalence estimate of GAD in EGA is from one site only; **prevalence estimate from NMHWS is for panic disorder and/or agoraphobia; ***prevalence estimate from NCS-R is for specific phobia
Presentation of anxiety disorders across the lifespan
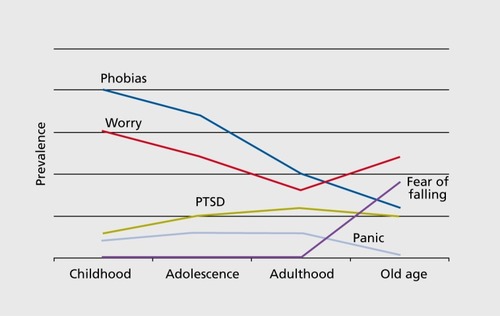
portrays our current understanding of how different forms of anxiety disorders may predominate at different stages of the lifespan. Phobias (particularly social and specific phobias) may predominate in childhood; panic disorder and post-traumatic stress disorder (PTSD) may be at their highest prevalence in adulthood; while worry disorders (ie, GAD) may be most common in old age. Anxiety disorders with a strong autonomic nervous system component (eg, resulting in panic attacks or panic-like symptoms) are usually considered to be more common in childhood or early adulthood than later in life, particularly with respect to social phobia and panic disorder. Age-related changes in brain structure or function or peripheral physiology likely reduce the propensity for autonomic responses.Citation5 Here we note the caveat that specific disorders “may” peak at different times in the lifespan because these data are largely based on epidemiological studies. The difficulty of retrospective evaluation of age of onset of mental disorders is a limitation to this assertion,Citation6 as is the difficulty of detecting late-onset anxiety disorders using standardized assessment tools that were developed for young adults..Citation2 Additionally, fear of falling (FOF) is a common and uniquely geriatric syndromeCitation7 marked by fear and avoidance. High rates of older adults in the community report a FOF,Citation8 and in its more severe forms the consequences of this fear are very serious, including a curtailing of activitiesCitation9; thus the problem is akin to agoraphobia in the more severe manifestation. However, it appears difficult to diagnose FOF as an anxiety disorder, due in large part to issues with insight and goodness of fit with existing DSM-IV nosology.Citation10 The one anxiety disorder that seems to be more commonly present in late life is GAD.Citation11
Why might anxiety disorders develop late in life?
Although anxiety disorders are properly thought of as neurodevelopmental conditions (ie, they develop in the context of brain changes which occur characteristically at various points in the lifespan), this does not mean that they are of childhood onset only. In fact, anxiety can develop in old age: one study found new-onset anxietydisorders in 11 % of older women and 2% of older men.Citation12
Up to one half of older patients with GAD have onset later in life.Citation13-Citation15 A review of European epidemiological studies found that the incidence of agoraphobia may increase over the lifespan in women.Citation16 While older adults may develop PTSD less frequently after traumatic events than younger adults do,Citation17 late-onset PTSD is not uncommon.Citation18-Citation20 Even panic disorder, thought to have a particularly low late-life incidence, has been documented in some studies,Citation21 particularly in patients with medical illness.Citation22
There are potential neurobiological risks for late-onset anxiety disorders (although these have not been subjected to empirical testing). We conceptualize pathological anxiety as potentially due to a functional disconnect between amygdala (and possibly insula) and frontal areas (including anterior cingulate cortex, dorsolateral and ventromedial prefrontal cortex), impairing natural fear extinction and thus converting fears or worries into chronic pathological conditions.Citation23 This process could be exaggerated in elderly persons, in whom aging and neurodegenerative changes may lead to reduced functional connectivity.Citation24,Citation25 Late-onset anxiety may thus be conceptualized as a consequence of neurobiological changes in aging involving pathways which are suspects in the onset and chronicity of anxiety disorders.
Psychological and social risk factors also play a role in the development of late-onset anxiety disorders. Some risk factors for geriatric anxiety and depression are shared, eg, female gender, cognitive impairment, chronic health conditions, poor self-rated health, functional limitations, personality traits such as neuroticism, and poor coping skills.Citation26,Citation27 Additional risk factors for anxiety specifically are being childless, having lower income, and experiencing traumatic events.
These psychosocial and neurobiological changes in aging interact with each other and with predisposition (eg, genetic or early-life adversity) to produce late-onset anxiety disorders. Additionally, age-related protective factors may include social support, religiosity, physical activity, cognitive stimulation, and effective coping skills learned throughout a lifetime, As in childhood disorders, such protective factors may buffer the effects of genetic and other risk factors.
Prospective studies are needed to study these risk and protective factors and their interactions. One option is to conduct a preventive intervention study for late-life anxiety disorders.Citation28 A preventive intervention study could enroll subjects with one or more of these risk factors, probably those with subsyndromal depressive or anxiety symptoms, and manage them with a stepped-care approach to prevent the onset of an anxiety disorder.Citation29 Such a preventive study could gather biological and behavioral data to elucidate biological, psychological, and social variables associated with increased likelihood of developing chronic anxiety. Elucidation of such risk signatures could then lead to a second generation of more robust preventive interventions that could target individuals most likely to benefit from prevention and intervene directly on the modifiable risk.Citation30 Such research would be consistent with the National Institute of Mental Health's vision of “pre-emptive” and “personalized” mechanistic-based novel intervention development.Citation31
Course
Anxiety disorders are among the most persistent mental health syndromes. The few longitudinal studies that have been carried out in older adults with anxiety suggest that they tend to be persistent in this age group.Citation32 Anxious older adults in epidemiological and treatment-seeking samples retrospectively report an average duration of 20 years or more, at least in the case of GAD.Citation13,Citation14,Citation33,Citation34
Anxiety's association with disability is greater with increasing age and it is bidirectional.Citation35 Anxiety increases disabilityCitation36 and appears in some studies to be associated with increased mortality risk.Citation37-Citation40 Additionally, significant quality of life impairment and increased burden of health care cost has been noted in GAD in older adults, on a par with that seen in late-life depression.Citation41,Citation42
Perhaps more uniquely in older adults, data suggest that chronic pathological anxiety is toxic to brain health. Anxiety symptoms or disorders in elderly are associated with accelerated cognitive decline.Citation43-Citation45 Below are some putative mechanisms based on an examination of recent mechanistic research.
Chronic psychological distress in older adults results in impairments in cognitionCitation46-Citation49 and it is thought that a keymechanism for this relationship involves changes in the hypothalamic-pituitary-adrenal (HPA) axis.Citation50 The HPA axis is a neuroendocrine mediator of stress and its central nervous system (CMS) effects .
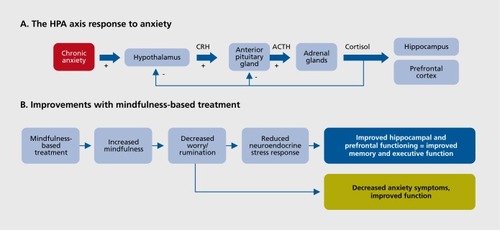
The aging brain is less able to downregulate the HPA axisCitation51-Citation56 and is more vulnerable to physiological insults.Citation57,Citation58 As a result, in older adults, chronic anxiety can cause IIPA axis hyperactivity,Citation59-Citation64 with deleterious effects on memory and executive function.Citation48,Citation53,Citation61,Citation65-Citation75 The putative mechanism is an effect of high Cortisol on brain structures (eg, hippocampus and prefrontal cortex) involved in neurocognitionCitation76-Citation77: Chronically elevated Cortisol desensitizes CNS glucocorticoid receptors,Citation78 altering glutamatergic N-methyl-D-aspartate receptor activityCitation79 with consequent synaptic and morphological changes in these structures.Citation69,Citation80,Citation81
Some of these changes appear to be reversible.Citation69,Citation82 For example, memory and hippocampal volumes in depression and anxiety disorders appear to be dynamic, increasing with successful treatment,Citation75,Citation83,Citation84 including in the elderly.Citation85 Thus, treatments for late-life mental disorders that reduce HPA axis hyperactivity ought to improve cognition. In a series of articles examining cortisol in late-life GAD, we found support for this hypothesis. We found that older adults with GAD had HPA axis hyperactivity, with 40% to 60% higher cortisol levels than comparisons.Citation61,Citation86 We also found a neuroendocrine effect of treatment: subjects who received escitalopram had a 12% to 15% reduction in peak and total cortisol with escitalopram (vs no change with placebo).Citation86 The neuroendocrine effect was correlated with reduced anxiety. This indicated that HPA dysfunction in late-life anxiety is modifiable with treatment. Finally, we found that cortisol changes during treatment predicted memoryimprovement; that is, we found significant improvements in immediate and delayed memory in escitalopramtreated subjects whose cortisol levels decreased.Citation87 In all, this research suggests that reducing the biological stress response might be one treatment target for cognitive improvement in late-life anxiety disorders, which we discuss further later in this review.
A chronically elevated stress response seen in late-life anxiety may cause cognitive decline by other mechanisms. Some studies have found increases in β-amyloid-42 peptide (Aβ42) production and tau hyperphosphorylation attributable to excessive HPA activation (mediated via corticotropin releasing factor-1 [CRF1]), showing a link between chronic stress in aging, increased CRF production, and the putative pathogenic steps in Alzheimer's diseaseCitation88-Citation90; this provides other putative mechanisms for cognitive decline in the context of chronic anxiety, mediated by excessive or altered HPA axis activation. Late-life depression is associated with immune activation, so this relationship might also be true in late-life anxiety.Citation91,Citation92,Citation93 Cardiovascular disease is the main cause of premature mortality in mental illness,Citation94 and some research has elucidated mechanisms between anxiety in elderly and cardiovascular disease - insulin resistance, endothelial reactivity, and altered autonomic function.Citation95 Research in chronic psychosocial stress and reduced telomere lengthCitation96,Citation97 has given rise to the hypothesis that chronic affective disorders lead to telomere shrinkingCitation98; hence chronic anxiety may be accelerating aging at a cellular level. Finally, altering serotonin function in an aging model appears to affect stress responsitivity as well as longevity and age-related neurodegeneration.Citation99
An apt summary of these myriad findings would be that stress research and aging research are intersecting: accelerated aging and stress hyperreactivity (as seen in anxiety disorders) are overlapping concepts. Thus, for late-life anxiety disorders, agents that affect aging pathways (such as rapamycin or calorie restriction mime tics) may be among the novel treatments that benefit health and cognition. Unfortunately, despite the wealth of research in the stress, immunology, and aging fields that could be applied to elucidate these connections, no longitudinal research, to our knowledge, has been done or is underway to elucidate the long-term consequences of chronic pathological anxiety in late life, their mechanisms, and/or novel treatments to reverse this “accelerated aging” process.
Comorbidity of anxiety with depression in the elderly
Depressed individuals at all ages, including older adults, commonly have comorbid anxiety symptoms or disorders. Longitudinally, anxiety symptoms appear to lead to depressive symptoms, more likely than is the case vice versa.Citation100 Anxiety disorders could therefore be a risk factor for late-life depression as well as a predictor of persistence and relapse, as in young adults.Citation14,Citation101,Citation102-Citation106 Some research disputes this assertion.Citation107 On the whole, though, studies support the conceptualization of anxious depression as a severe, treatment-relevant subtype of depression throughout the lifespan. It remains unknown whether anxious depression reflects diagnostic or dimensional phenotypic overlap, a common neurobiological, behavioral, and/or psychological underpinning, or some additional heterogeneity. Anxious depression might be particularly relevant in older adults, in whom it predicts more cognitive declineCitation44 and greater suicide riskCitation108 than nonanxious depression.
Treatment
Pharmacological treatments for anxiety disorders do not always have the same benefits or risks across the lifespan. Additionally, in the case of psychotherapy, treatments typically need to be adapted for older adults.Citation30,Citation109
This section summarizes treatment literature in geriatric anxiety disorders, discusses new directions in treatment development for older adults, and then provides a set of management guidelines for clinicians.
Psychotherapy
Cognitive behavioral therapy (CBT) is the mainstay for anxiety disorder treatment. In younger adults, it is a treatment of choice, particularly when exposure-based, for most anxiety disorders (although it is by no means the only effective approach in these cases). It remains unclear whether CBT is superior to other psychotherapy approaches in late-life anxiety disorders; however, this is presently the dominant and most widely available formal psychotherapy for anxiety disorders. CBT might be particularly effective for anxiety disorders in cognitively intact, motivated older adults who are able to learn new skills in CBT and use them effectively.Citation110
CBT for late-life anxiety typically involves psychoeducation, relaxation, cognitive therapy, problem-solving skills training, exposure and habituation to anxiogenic situations, and sleep hygiene when necessary for insomnia, similar to treatment in younger adults.Citation111 In older adults, the most effective ingredient of CBT may be relaxation training, which is fairly simple for providers.Citation112 With respect to long-term management of this chronic disorder, naturalistic follow-up studies of older GAD patients treated with CBT have demonstrated maintenance of gains for up to 1 year following discontinuation of treatment.Citation113
There are some limitations to CBT for older adults with anxiety disorders. First, both a meta-analysis and a small direct randomized comparison of pharmacotherapy and psychotherapy found medications to be more effective than CBT in the acute phase of treatment.Citation114,Citation115 Additionally, although CBT has been shown to be effective in the primary care setting,Citation116 the lack of CBT therapists with experience in late-life anxiety is a barrier to widespread implementation.
Adaptations for older adults include a slower pace with increased repetition, less abstract cognitive restructuring techniques and correspondingly more focus on behavioral change, more focus on health concerns, and engagement of the family in the treatment. In addition to in-session discussion and a written summary of material, it is useful to audiotape sessions for participants to increase the learning of new material. Another possible adaptation is the integration of religion into CBT, particularly in older adults who often have more of a spiritual view of their lives.Citation117
Modular treatment reflects a novel approach in psychotherapy research in which the patient's presenting problems or symptoms are used to choose the specific components of treatment.Citation118,Citation119 This patient-centered process appears to increase engagement and reduce attritionCitation120,Citation121 and may be more cost-effective.
Some other psychotherapy treatment modalities are worth mentioning. First, bibliotherapy, or guided selfhelp, has long been a low-cost and widely available alternative (or addition) to a full-scale psychotherapy protocol.Citation122 Such self-help guides exist using CBT, Acceptance and Commitment Therapy, or mindfulness models; they can be used as a first step in, or complement to, formal psychotherapy (or pharmacotherapy) approaches. A recent study of late-life anxiety and depression prevention used a stepped-care approach, in which the first intervention was bibliotherapy, was effective at preventing anxiety and depressive episodes.Citation29 Many self-help workbooks exist for anxiety disorders, though none to our knowledge are focused on older adults. There is increasing indication that many patients are using the Internet as a guide for treatment, although it is unknown to what extent this is the case for older adults. As such, Internet-based self-help may be another increasingly available, low-cost psychotherapy option that is little studied in this age group. Organizations such as the Anxiety Disorders Association of America and the Geriatric Mental Health Foundation offer psychoeducational help for late-life anxiety disorders on-line.
Novel treatment directions for psychotherapy in late-life anxiety disorders
Worry and rumination are important driving forces in late-life mental disorders.Citation123-Citation125 Poorer executive function, which is associated with aging, is associated with decreased ability to inhibit rumination and worry.Citation126-Citation130 Recent studies demonstrate that putative neuroimaging markers for ruminationCitation131,Citation132 increase with aging.Citation25,Citation133-Citation136 Worry and rumination are associated with HPA axis hyperactivity in late-life mental disorders; for example, we found that excessive worry robustly predicted cortisol levels in late-life generalized anxiety disorder (GAD) patients,Citation61 and that reduction of worry predicted cortisol reduction during treatment.Citation86
These data generate the hypothesis that interventions that reduce pathological worry and rumination will reduce HPA axis hyperactivity and thereby improve cognition as well as clinical symptoms in late-life anxiety disorders and depression. Unfortunately, standard treatments for these disorders in older adults are of modest efficacy for pathological worry and rumination. Citation116,Citation137,Citation138 Thus, new and effective psychosocial interventions are needed.Citation139
Hyperactive stress response due to pathological worry and rumination may be an ideal target for mindfulness meditation. Mindfulness meditation emphasizes focused, nonjudgmental awareness of present moment experiences as an alternative to dwelling on the past (eg, ruminating)Citation140 or future (eg, worrying).Citation141 One mindfulness-based intervention, Mindfulness-Based Stress Reduction (MBSR) has been shown to improve anxietyCitation142-Citation144 and other psychological outcomes in clinical trials. It is already practiced in every major city in the US and in over 250 clinics, hospitals, and HMOs in the US and abroad.Citation145 Mindfulness meditation programs have seen an explosion of interest and acceptability among older adults.Citation146-Citation150 MBSR appears to increase mindfulness,Citation151 a state of present-centeredness that is the converse of worry about the future and rumination about the past.Citation152 Accordingly, several studies have demonstrated a rumination- and worry-reducing effect of MBSR.Citation140,Citation153,Citation154
Accordingly, multiple studies of MBSR have demonstrated potent cortisol-lowering effects, suggesting that increasing mindfulness reduces excessive HPA axis responses.Citation155,Citation156 Thus, MBSR appears promising, conceptually- and empirically, as a treatment for the factors that underlie neurocognitive impairment and clinical outcomes in late-life anxiety disorders, as shown in the model in Figure 2b.
Pharmacotherapy
Benzodiazepines are still commonly used for geriatric anxiety.Citation157 However, the risk:benefit ratio of these medications is poorer in older adults than in younger adults. In older adults, these medications are associated with falls,Citation158 disability,Citation159 and cognitive impairment and decline.Citation160 The risks occur at doses lower than the usual efficacious dose of these medications for anxiety disorders. Thus, these medications do not just have a tight therapeutic index, they have a reverse index (dose for harms lower than dose for benefits) with increasing aging. For this reason, they should be considered short-term adjuncts to treatment, with long-term use only as a last resort.
Two small RCTsCitation115,Citation161 provided important feasibility data and preliminary evidence of the efficacy of selective serotonin reuptake inhibitors (SSRIs) in the acute treatment of older adults with anxiety disorders, predominantly GAD. As a result, one of us (EJL) led the first and, to our knowledge, only full-scale RCT of an SSRI for acute treatment of late-life anxiety disorders.Citation137 We randomized 177 older adults with GAD to the SSRI escitalopram, flexibly dosed at 10 to 20 mg daily, or placebo for 12 weeks. Escitalopram was shown to be efficacious, with greater cumulative response (69% vs 51%,P=0.03) and greater improvements in worry severity and role function. The effect size for most clinical outcome measures was in the low-medium range. A reasonable conclusion from this full-scale study, together with the pilot studies, is that SSRIs are efficacious but show the same disappointing effect sizes as in studies of young adults (or older adults with depression).Citation162
There are caveats to this conclusion: first, a single relatively small full-scale study is unlikely to be adequate for clarifying the extent of benefits for any treatment (although, as mentioned previously, we are unaware of any current efforts for another); perhaps the effect size of SSRIs is higher, or lower, than we found in that study. Second, all of these studies suffer the limitations of the measures used in anxiety trials, such as the Hamilton Anxiety ScaleCitation163 and Penn State Worry Questionnaire. Finally, clinical symptomatology is not the only important outcome of late-life anxiety disorder treatment. In fact, it may be the least important, as patients are typically more concerned about their quality of life and their systemic and (in particular) cognitive health, such as memory decline. In that study, we measured quality of life (which improved, albeit modestly, more with escitalopram than placebo) and also cognitive health, using neuropsychological testing as a proxy.Citation164 We found that improvement in late-life GAD was associated with significant improvements in a variety of cognitive measures; however, patients randomized to escitalopram showed greater improvement than those randomized to placebo in only one neuropsychological testing - a sorting task that is a proxy for some aspects of executive function. Thus, although, as noted previously, in some individuals (namely those with reduction in cortisol during treatment) there were some cognitive improvements, in the aggregate the SSRI treatment was disappointing for its acute benefits for cognitive function and quality of life. The SSRIs may be too nonspecific and “broadspectrum” to hope for significant cognitive benefits in late-life anxiety treatment.
There have been no prospective studies of serotonin norepinephrine reuptake inhibitors (SNRIs) specifically in late-life anxiety as there have in late-life depression. A retrospective examination of phase 3 venlafaxine XR data found the drug to be efficacious in adults aged 60+, with an effect size (drug-placebo difference) and side-effect profile similar to younger adults.Citation165 Similar findings have been reported with duloxetine.Citation166
These studies in SSRIs and SNRIs have found similar side effects in elderly persons as in younger adults, but importantly they were not designed to determine the recently reported potential risks of SSRIs specific to the elderly population: gait impairment increasing risk for falls,Citation167 and bone loss.Citation168 Other risks that are greater in older adults are impaired clotting leading to non-GI and GI bleedingCitation169 and SIADII leading to hyponatremia.Citation170 Such reports suggest that the risk:benefit ratio for longterm SSRI/SNRI use is not the same as in younger adults. These concerns have yet to be addressed in a properly constructed longitudinal study (ie, a randomized controlled trial with an adequate safety evaluation). In terms of non-SSRI/SNRI treatments, a large-scale study with pregabalin in geriatric GAD showed efficacy.Citation171 Pregabalin is not FDA-approved to treat anxietydisorders; its mechanism of action for anxiety is unknown - it binds to an auxiliary subunit voltage-gated calcium channels and is thought to reduce the synaptic release of several neurotransmitters. Mirtazapine is another non-SSRI/SNRI treatment with efficacy in anxiety, with some evidence specifically in late-life anxiety disorders.Citation172
Most geriatric anxiety pharmacotherapy research has focused on GAD. There has been one promising study of the SSRI citalopram in older adults with PTSD,Citation173 and also evidence that the α-adrenergic antagonist prazosin is efficacious for sleep-related concerns in PTSD, although not for other PTSD symptoms.Citation174 There are two small studies in late-life panic disorder: Rampello et alCitation175 found superiority of escitalopram over citalopram in time to response, and a small open-label study found promising signals with sertraline.Citation176 Finally, in GAD in the context of stroke, one analysis found efficacy of nortriptyline in a merged dataset of several RCTs of post-stroke depression, in which patients with comorbid GAD were analyzed.Citation177
The only published augmentation study in late-life anxiety disorders is a small study with risperidone.Citation178 While the atypical antipsychotic was promising, there have been concerns with atypicals in older adults, given evidence of higher mortality with antipsychotics in older patients with dementia, and metabolic effects including weight gain, elevated lipids, and insulin resistance. It is unclear whether the mortality risk applies to nondemented older adults, but the metabolic risks certainly do. Finally, long-term or maintenance treatment of late-life anxiety with medication has not been studied (although we are currently carrying out a study of maintenance effects of SSRI treatment in late-life GAD), and no augmentation strategies can be recommended with confidence.
Combining medication and psychotherapy for late-life anxiety disorders
The inadequacy of monotherapy is well known in mood and anxiety disorders, and combination treatments may be more effective.Citation179 Antidepressants and CBT have different mechanisms and may be able to treat different components of the illness.Citation180,Citation181 Combination treatment in older adults might best be carried out sequentially, rather than simultaneously initiated, to maximize costeffectiveness and allow the patient and provider to focus sequentially on different aspects of treatment, rather than divide focus among multiple treatments and components of illness at once.Citation182 The hope is that, with two treatments targeting the different facets of the illness, persistent residual features and relapse are less likely. Supporting this assertion, a recent review of meta-analyses concluded that psychotherapies involving cognitive and behavioral strategies for GAD are superior to nondirective therapy and pill placebo, and equivalent to pharmacotherapy in the acute phase of treatment, with robust effects extending as far as 10 years following discontinuation of treatment.Citation183 In one study of anxious older adults, benefits of CBT were increased at 1-year follow-up in patients who had been treated for at least 3 months with medications prior to receiving CBT, suggesting that sustained or increasing gains are possible for older adults receiving CBT for anxiety following an acute course of pharmacotherapy.Citation184
The strategy of sequencing medication with CBT is controversial in the anxiety disorders.Citation185,Citation186 Pharmacotherapy might interfere with the challenging of catastrophic beliefs during psychotherapy, individuals treated with medications may be less motivated to engage in psychotherapy, and psychotherapy in the context of medications may result in state-dependent learning that does not persist after the medication is discontinued.Citation187,Citation188
Because of this, we are currently testing the strategy of sequenced medication and CBT within a controlled study design.
Future directions in treatment development: new targets and one large barrier
The preceding sections raise several avenues for novel treatment development. Our findings with cortisol in late-life GAD are summed up as such: elevated cortisol is associated with GAD, is reducible with treatment, and when reduced during treatment is associated with neuropsychological improvements (in memory). Thus, the biological stress response (for which cortisol is a mediator or proxy) may be a prime target for novel pharmacological (ie, cortisol-blocking) or behavioral (ie, worry-reducing) strategies, with the effect of improving not only clinical but also cognitive functioning. Conversely, researchers also need to consider how to improve anxiety in cognitively-impaired older adults, particularly those whose impairment has evolved into dementia, realizing that for many if not most, such a level of cognitive impairment is not likely to improve with any treatment (anxiety or otherwise).
The biological stress response may also be a target in improving systemic health in late-life anxiety disorders. The dramatic health impact not only of late-life anxiety disorders but also in other chronic stress models, such as is seen in spousal caregivers of AD patients, suggests that more mechanistic work is needed to delineate the pathways from psychosocial stress as seen in chronic anxiety/worry to adverse health. Fortunately, new tools (such as genome-wide expression or proteomic analysis, or novel imaging techniques to measure CNS or peripheral inflammation) should make this research more feasible. Less mechanistic than a specific biological pathway but at least as important is the concept of function as a target. Anxiety disorders are disabling, just as is depression in older adults. For example, fear of falling is in some patients a highly disabling condition akin to severe agoraphobia. New methods are needed to measure and improve function in older adults that is relevant to anxiety disorders.
In terms of one major barrier to progress in late-life anxiety research, we turn again to the issue of measurement. Progress in measurement techniques is a prerequisite for scientific advances, yet in the area of late-life anxiety disorders our measurements are antiquated and demonstrably inadequate, hampering research progress. This is true across the lifespan but may be particularly pressing in geriatrics. We have previously reviewed this issue of inadequate measurement in some depthCitation30 but will summarize key concerns here.
Variability in diagnostic criteria and tools leads to discrepant epidemiological findings: as reviewed in-depth elsewhere,Citation2 epidemiologic studies have found dramatically different prevalence and incidence estimates. Numerous issues hamper our ability to accurately diagnose or characterize anxiety disorders in older adults,Citation189 and a recent review has suggested ways to improve diagnosis so that DSM-5 might be more sensitive to late-life anxiety disorders.Citation4 Additionally, it has been suggested that the problems described above reflect the limitation of using diagnostic categories, and the solution is to move towards dimensional assessments of illness.Citation190 Yet, the challenge of measuring geriatric anxiety goes beyond diagnosis. The problems of symptom assessment in geriatric mental health are complex and not necessarily ones that can be resolved with existing or adapted symptomatic assessments. Instead, technological advances could develop novel ways of monitoring the severity and phenomenology of anxiety and its response to treatment. These advances include: (i) improved subjective symptom measurement via electronic daily or momentary assessment; (ii) improved measurement of function via actigraphy and other assessments; and (iii) assessment of the physiological and cognitive benefits of treatment via biomarkers. These are described in more detail below.
Electronic assessment of symptoms
Anxiety symptomatology has traditionally been assessed using retrospective self-report.Citation191-Citation197 Such measures require participants to recall, average, and summarize their experiences and are subject to bias and error; for example, disproportionate weight may be given to highly significant past instances relative to current or ongoing events.Citation198-Citation207 Current state assessment seems critical for anxiety, often a moment-to-moment waxing and waning experience.
Ecological momentary assessment (EMA) involves repeated measurement of momentary experiences naturalistically and in real time.Citation208 It has been used to assess stress, behavior, and other physical and mental healthrelated constructs.Citation209-Citation214 The key features of EMA are that it samples: (i) present moment experience (ie, as opposed to recalled, averaged, or summarized experience); (ii) in its natural context (ie, outside of a laboratory); (iii) repeatedly over time (often up to eight times per day). The availability of electronic means of data capture, such as mobile devices, has greatly facilitated the use of EMA. For example, participants can be prompted at random intervals by a device to respond to a brief series of questions about the present moment; responses are input immediately by the participants, with data transmitted wirelessly to the investigator.Citation215-Citation217
Given its capability of evaluating momentary experience, EMA appears well suited to examine anxiety symptomatology. EMA avoids reporting biases such as recency and severity effects, ”telescoping,“ and difficulties with estimation. These biases are particularly relevant for elderly. These types of assessments can also capture diurnal variations in symptoms. Yet even these assessments require a fair degree of insight by the user; we may need assessments of anxiety severity that do not require subjective assessment by the patient.
Novel measures
Novel measures may also improve our measurement of disability (or behavior change) stemming from anxiety. Actigraphy findings have been used to measure depression severity and treatment response.Citation218-Citation220 Actigraphy is particularly useful in examining sleep, activity, and circadian rhythm, so these patterns could potentially provide an objective measure of response that could complement self-report. A similar use of objective assessment technology might be the use of global positioning (GPS/GIS) to gather extensive data on activity and therefore on function.
Biomarkers
Finally, measurement of biomarkers may be able to characterize one aspect of anxiety disorders most notable in older adults: their deleterious effects on cognitive and physiological health. Neuropsychological testing has long existed (though rarely examined in treatments of anxiety disorders). Newer biomarkers could evaluate treatment response in older adults in whom anxiety is most likely to have long-term adverse health or cognitive consequences. These may include HPA axis functioning through cortisol sampling, or genome-wide expression analysis, a powerful high-throughput technology that provides a systems approach for examining complex clinical disease in terms of dynamic changes in gene expression.Citation221 Genome-wide expression analysis assays the current activity level of all transcripts known in humans. Thus, for example, a researcher can determine whether stress results in higher or lower levels of RNA transcripts in peripheral immunological cells.Citation222 Such data, combined with bioinformatic techniques, allow researchers to infer the functioning of all of the intracellular pathways at a given point in time (ie, at baseline and then after a treatment), as well as their interactions.Citation223,Citation224 Additionally, as we previously noted, chronic stress hyperactivity (as seen in anxiety disorders) may cause accelerated aging; thus, telomere length measurement, during the course of a treatment study, might provide a precise and quantitative estimate of benefits of treatment for health and cognition of older adults. Finally, novel neuroimaging markers might include neurogenesis, functional connectivity, and peripheral and central inflammation. In all, recent advances in technology in studies of anxiety could increase our precision for measurement, a need most pressing in geriatrics.
What we do know: eight rules for managing anxiety disorders from a lifespan perspective
In this last section, we provide a blueprint for managing older (and equally so, younger) adults with anxiety disorders, based on empirical findings and our own clinical experience.
1. Assessment should measure severity and provide objective criteria for assessing response, and should assess comorbidity, prior treatment, cognitive status, and need for a medical workup
Assessment of anxiety is often overlooked by mental health providers. A helpful introduction to the topic is to ask about stress; eg, “older adults often deal with stress; how do you feel in times of stress?“ Patients who describe symptoms suggestive of anxiety or worry can then be further queried. Use nondirective questioning to determine the severity of anxiety symptoms, by: (i) level of distress (asking how much the anxiety symptoms bother the patient, what strategies they are trying in order to control or avoid it, and what somatic symptoms they are having); (ii) how much of their time it takes; and (iii) avoidance. Avoidance is a key component of all anxiety disorders yet often is not recognized. For example, older adults may rationalize changes in behavior patterns to perceived poor health or environmental limitations. Inquire about behavioral changes including activities given up or, conversely, intrusive overinvolvement with family members. Talk to the family for corroboration.
We are often asked about differentiating anxiety from depression. In our experience, some patients (and some neurobiologists!) fail to appreciate the importance we place on this diagnostic distinction. Clinically, the clinician will often have to deal with anxiety as well as depression in a patient.
The medical differentiation of late-onset anxiety is long but should chiefly consider: (i) depression; (ii) cognitive impairment (dementia, delirium); (iii) anxiety-inducing medications (or recent discontinuation or inconsistent use of sedatives); and (iv) common and rare medical conditions that could masquerade as an anxiety disorder. Regarding the latter, consider thyroid disease, B12 deficiency, hypoxia, ischemia, or metabolic changes (eg, hypercalcemia or hypoglycemia).
2. Think twice about a benzodiazepine prescription
As previously noted, benzodiazepines, like any sedatives, have a poorer risk:benefit ratio in elderly persons than in young adults. Therefore, long-term use of benzodiazepines appears unfavorable in this age group. Patients should be warned about the potential risks associated with these medications.
Benzodiazepines provide a fast anxiolytic action, so a common recommendation is to use these medications at low dose as a short-term adjunct, in which case they may provide some early relief and improve adherence to the treatment regimen. Even this adjunctive use of benzodiazepines is typically unnecessary and can reinforce an inappropriate message to patients that anxiety must be immediately relieved, which is akin to an avoidance response.
3. Psychoeducation about anxiety and treatment, including potential health benefits
Psychoeducation may be the most important management step. Providers should inform patients that they have a treatable condition and should address stigma, misinformation, and other common and surmountable barriers to treatment. Emphasize the importance of treating anxiety for improving quality of life, health, and brain health. Include the family in these discussions.
4 First-line treatment according to patient's preference, provider preference and competence, and treatment availability
First-line options include one or more of the following: SSRI, SNRI, relaxation training, and CBT. Bibliotherapy can and should be recommended alongside any of these options. Often these options will need to be started along with, or after, discontinuation of harmful or inappropriate confusogenic medications such as sedatives, anticholinergics, and antihistaminergics.
Table II Features of anxiety disorders across the lifespan.
5. Frequent follow-up, particularly within the first month of treatment or dose change, to encourage adherence and monitor treatment response
Most anxious adults will receive a pharmacological trial as first-line treatment. Older adults vary from young adults in terms of increased comorbid medical conditions, pharmacokinetic changes, frailty, and drug interactions. Yet, anxious older adults' reports that they are sensitive or intolerant of antidepressant medications appears to result less from actual side effects than from their anticipatory concern, vigilance towards interoceptive stimuli, and tendency to catastrophize about any interoceptive sensations they detect.
Overcoming such fears related to the medication's potentially negative effects is not an easy task. This task is made more difficult by the standard list of potential side effects with any medication, many of which sound frightening or are symptoms that the patient already has (eg, fatigue, insomnia). To combat these fears proactively, describe how such antidepressant medications have established efficacy and high tolerability. Also, a health care provider should describe their experience in prescribing this medication and state that, while side effects are possible, no particular side effect is inevitable: most patients taking the medication will either have no side effects or will have brief, self-limited side effects which subside in a few weeks. Emphasize that the medication is unlikely to be incapacitating. When patients mention that “I already have that symptom,” they are not more likely to have that as a side effect as a result; in contrast, physical symptoms tend to decrease with pharmacological treatment.Citation225
Family involvement can help with adherence. Nevertheless, most patients will have additional concerns after the medication is prescribed, especially before and just after they take the first dose. Address this in several ways, stating to patients/families that it is natural to have questions, and encouraging them to call, providing 24-hour contact information (typically patients do not, but benefit from the knowledge that they can). Ideally, as in clinical trials, we would provide weekly visits, or biweekly visits with interim telephone contacts, for the first month of treatment and the month subsequent to a dose increase, since this is when patients are most likely to develop concerns about side effects.
Follow-up includes interviewing patients closely for any concerns about perceived side effects. Patients often seem to perceive as side effects symptoms that predate the start of medication and are clearly a component of the disorder. In anxiety, adherence issues stem from vigilance to perceived side effects and subsequent catastrophizing. If such an issue is noted, an immediate contact will reassure the patient that they are being monitored closely by experts and that the medication is not causing some sort of severe or worsening problem. This brief but timely intervention reduces premature discontinuation of pharmacotherapy.
Geriatric anxiety disorder patients usually get better, but given the fluctuating nature of the disorders and the issues with insight, they often do not realize they are improving. Repeated assessment of frequency and severity of anxiety is important not just for assessing success of treatment but also demonstrating improvement to the patient.
6. With medications, start low, go slow, but go - as aggressively as required to treat symptoms to remission
After psychoeducation and clean-up of inappropriate medications, the proximal goal of acute care is to get the patient a treatment trial of sufficient intensity and duration to improve symptoms. This requires dose optimization, often at high doses that do not vary across the lifespan in the case of SSRIs/SNRIs.
Table III Key points from a lifespan view of anxiety disorders.
7. Consider augmentation treatment and refer to experts if necessary
Monotherapy is usually inadequate, and if a good trial is only partially effective, add another. Providers should not “run out of options” but then should refer a patient to someone with additional expertise in (eg, a geriatric psychiatrist or a psychotherapist skilled at treating anxiety disorders).
8. Provide maintenance treatment; evaluate the need for such if treatment is discontinued
Since anxiety is chronic, treatment will usually need to be long-term, ie, maintenance medication and/or booster psychotherapy sessions. As the patient has already overcome any fears or initial side effects, maintenance pharmacotherapy requires less frequent oversight though continued monitoring of clinical changes, side effects, and changes in coprescribed medications is necessary. If a patient chooses to taper off a medication, they should be informed that they may need to resume treatment in the event of relapse. A taper should be very gradual (ie, over several weeks) to avoid rebound anxiety symptoms. Management does not have an end point, even when the patient is no longer receiving active pharmacotherapy. In the case of psychotherapy benefits, booster sessions provide important reminders to continue to use effective new coping skills.
Summary
Anxiety disorders are neurodevelopmental disorders, and as neurodevelopment continues and changes throughout the lifespan, even into old age, there are new, unique issues with anxiety disorder and presentation at each point in aging. Just as childhood offers unique perspectives such as the need to target parental influenceCitation226 and the possibility for prevention, in older adults there are new presentations (such as FOF) and new effects of anxiety (on brain and physiological health).
There have been many strides in our understanding of anxiety disorders across the lifespan, but also many gaps in our knowledge remain. The field has adequately clarified the benefits of treatments developed for young adults, as equally efficacious in older adults in the case of pharmacotherapy, or in the case of cognitive-behavioral therapy, needing adaptation in order to be efficacious. What is lacking are new treatments for older adults and the understanding of the mechanisms for onset and maintenance of anxiety disorders and how they exert such deleterious effects on the brain and physiologic health of older adults.
New treatments, both behavioral and somatic, need to be developed and tested across the lifespan. In older adults, treatment development ought to consider the barriers posed by cognitive impairment and even develop treatments that target cognition as well as clinical symptoms. Research needs to consider and address the gaps raised in this review, most fundamentally our limitations in the diagnosis and measurement of anxiety disorders in older adults. The great public health importance of this research is highlighted by the graying of the world population, the high human and economic cost of anxiety disorders in all age groups, and the potential for existing and new treatments to reduce much of this burden.
This publication was supported by NIH grants R01 MH083648, R34 MH080151, and R34 MH086668.
Conflict of interest statement: Dr Lenze discloses that he has received research funding from Forest Laboratories, Johnson & Johnson, and Roche. He has been a consultant for Fox Learning Systems; Dr Wetherell discloses that she has received research funding from Forest Laboratories.
REFERENCES
- Secretariat of the UN. World Population Prospects: The 2008 Revision. Available at: http://esa.un.org/unpp. Accessed January 7. 2011
- BryantC.JacksonH.AmesD.The prevalence of anxiety in older adults: methodological issues and a review of the literature.J Affect Disord.200810923325018155775
- Wolitzky-TaylorKB.CastriottaN.LenzeEJ.StanleyMA.CraskeMG.Anxiety disorders in older adults: a comprehensive review.Depress Anxiety.20102719021120099273
- MohlmanJ.BryantC.LenzeEJ.et al.Improving recognition of late life anxiety disorders in DSM-V: observations and recommendations of the Advisory Committee to the Lifespan Disorders Work Group.Int J Geriatr Psychiatry. In press.
- FlintA.BradwejnJ.VaccarinoF.GutkowskaJ.PalmourR.KoszyckiD.Aging and panicogenic response to cholecystokinin tetrapeptide: an examination of the cholecystokinin system.Neuropsychopharrnacology.200227663671
- WienerP.AlexopoulosGS.KakumaT.MeyersBS.RosenthalE.ChesterJ.The limits of history-taking in geriatric depression.Am J Geriatr Psychiatry .199751161259106375
- RowlandJ.PetersonEW.LevinWC.FriedL.PordonD.BakS.Fear of falling among the community-dwelling elderly.J Aging Health.1993522924310125446
- ZijlstraGA.van HaastregtJC.van RossumE.van EijkJT.YardleyL.KempenGl.Interventions to reduce fear of falling in community-living older people: a systematic review.J Am Geriatr Soc.20075560361517397441
- WilsonMM.MillerDK.AndresenEM.MalmstromTK.MillerJP.WolinskyFD.Fear of falling and related activity restriction among middle-aged African Americans.J Gerontol. Series A, Biol Sci Med Sci.200560355360
- GagnonN.FlintAJ.NaglieG.DevinsGM.Affective correlates of fear of falling in elderly persons.Am J Geriatr Psychiatry.20051371415653935
- BeekmanAT.BremmerMA.DeegDJ.et al.Anxiety disorders in later life: a report from the Longitudinal Aging Study Amsterdam.Int J Geriatr Psychiatry.1998137177269818308
- SamuelssonG.McCamish-SvenssonC.HagbergB.SundstromG.DehlinO.Incidence and risk factors for depression and anxiety disorders: results from a 34-year longitudinal Swedish cohort study.Aging Mental Health.2005957157516214705
- Le RouxH.GatzM.WetherellJL.Age at onset of generalized anxiety disorder in older adults.Am J Geriatr Psychiatry.200513233015653937
- LenzeEJ.MulsantBH.MohlmanJ.et al.Generalized anxiety disorder in late life: lifetime course and comorbidity with major depressive disorder.Am J Geriatr Psychiatry.200513778015653943
- ChouKL.Age at onset of generalized anxiety disorder in older adults.Am J Geriatr Psychiatry.20091745546419472431
- Riedel-HellerSG.BusseA.AngermeyerMC.The state of mental health in old-age across the'old' European Union- a systematic review.Acta Psychiatr Scandinav.200611338840116603030
- AciernoR.RuggieroKJ.KilpatrickDG.ResnickHS.GaleaS.Risk and protective factors for psychopathology among older versus younger adults after the 2004 Florida hurricanes.Am J Geriatr Psychiatry.2006141051105917035356
- AndrewsB.BrewinCR.PhilpottR.StewartL.Delayed-onset posttraumatic stress disorder: a systematic review of the evidence.Am J Psychiatry.20071641319132617728415
- MittalD.TorresR.AbashidzeA.JimersonN.Worsening of post-traumatic stress disorder symptoms with cognitive decline: case series.J Geriatr Psychiatry Neurol.200114172011281311
- RuzichMJ.LooiJC.RobertsonMD.Delayed onset of posttraumatic stress disorder among male combat veterans: a case series.Am J Geriatr Psychiatry.20051342442715879593
- SheikhJI.SwalesPJ.CarlsonEB.LindleySE.Aging and panic disorder: phenomenology, comorbidity, and risk factors.Am J Geriatr Psychiatry.20041210210914729565
- TodaroJF.ShenBJ.RaffaSD.TilkemeierPL.NiauraR.Prevalence of anxiety disorders in men and women with established coronary heart disease.J Cardiopulm Rehabil Prev.200727869117558244
- AupperleRL.PaulusMP.Neural systems underlying approach and avoidance in anxiety disorders.Dialogues Clin Neurosci.20101251753121319496
- Andrews-HannaJR.SnyderAZ.VincentJL.et al.Disruption of large-scale brain systems in advanced aging.Neuron.20075692493518054866
- ShelineYl.RaichleME.SnyderAZ.et al.Amyloid plaques disrupt resting state default mode network connectivity in cognitively normal elderly.Biol Psychiatry.20106758458719833321
- SchoeversRA.BeekmanAT.DeegDJ.JonkerC.van TilburgW.Comorbidity and risk-patterns of depression, generalised anxiety disorder and mixed anxiety-depression in later life: results from the AMSTEL study.Int J Geriatr Psychiatry.200318994100114618550
- VinkD.AartsenMJ.SchoeversRA.Risk factors for anxiety and depression in the elderly: a review.J Affect Disord.2008106294417707515
- SmitF.ComijsH.SchoeversR.CuijpersP.DeegD.BeekmanA.Target groups for the prevention of late-life anxiety.Br J Psychiatry.200719042843417470958
- van't Veer-TazelaarPJ.van MarwijkHW.van OppenP.et al.Steppedcare prevention of anxiety and depression in late life: a randomized controlled trial.Arch Gen Psychiatry.20096629730419255379
- LenzeEJ.WetherellJL.Bringing the bedside to the bench, and then to the community: a prospectus for intervention research in late-life anxiety disorders,int J Geriatr Psychiatry.20092411418613267
- InselTR.Translating scientific opportunity into public health impact: a strategic plan for research on mental illness.Arch Gen Psychiatry.20096612813319188534
- SchuurmansJ.ComijsHC.BeekmanAT.et al.The outcome of anxiety disorders in older people at 6-year follow-up: results from the Longitudinal Aging Study Amsterdam.Acta Psychiatr Scand.200511142042815877708
- BlazerD.GeorgeKL.HughesD.The epidemiology of anxiety disorders: an age comparison. In: Salzman C LB, ed.Anxiety in the Elderly: Treatment and Research. New York, NY: Springer. 19911730
- SheikhJl.KingRJ.TaylorCB.Comparative phenomenology of early-onset versus late-onset panic attacks: a pilot survey.Am J Psychiatry.1991148123112331883003
- BrenesGA.PenninxBW.JuddPH.RockwellE.SewellDD.WetherellJL.Anxiety, depression and disability across the lifespan.Aging Ment Health.20081215816318297491
- BrenesGA.GuralnikJM.WilliamsonJD.et al.The influence of anxiety on the progression of disability.J Am Geriatr Soc.200553343915667373
- BrenesGA.KritchevskySB.MehtaKM.et al.Scared to death: results from the Health, Aging, and Body Composition study.Am J Geriatr Psychiatry.20071526226517322138
- MartensEJ.de JongeP.NaB.CohenBE.LettH.WhooleyMA.Scared to death? Generalized anxiety disorder and cardiovascular events in patients with stable coronary heart disease: The Heart and Soul Study.Arch Gen Psychiatry.20106775075820603456
- TullyPJ.BakerRA.KnightJL.Anxiety and depression as risk factors for mortality after coronary artery bypass surgery.J Psychosom Res.20086428529018291243
- van HoutHP.BeekmanAT.de BeursE.et al.Anxiety and the risk of death in older men and women.Br J Psychiatry.200418539940415516548
- PorenskyEK.DewMA.KarpJF.et al.The burden of late life generalized anxiety disorder: effects on disability, health-related quality of life, and health care utilization.Am J Geriatr Psychiatry.20091747348219472438
- WetherellJL.ThorpSR.PattersonTL.GolshanS.JesteDV.GatzM.Quality of life in geriatric generalized anxiety disorder: a preliminary investigation.J Psychiatr Res.20043830531215003436
- PalmerK.BergerAK.MonasteroR.WinbladB.BackmanL.FratiglioniL.Predictors of progression from mild cognitive impairment to Alzheimer disease.Neurology.2007681596160217485646
- DeLucaAK.LenzeEJ.MulsantBH.et al.Comorbid anxiety disorder in late life depression: association with memory decline over four years.Int J Geriatr Psychiatry.20052084885416116585
- SinoffG.WernerP.Anxiety disorder and accompanying subjective memory loss in the elderly as a predictor of future cognitive decline.Int J Geriatr Psychiatry.20031895195914533128
- LupienSJ.GaudreauS.TchiteyaBM.et al.Stress-induced declarative memory impairment in healthy elderly subjects: relationship to cortisol reactivity.J Clin Endocrinol Metab.199782207020759215274
- LupienSJ.NairNP.BriereS.et al.Increased cortisol levels and impaired cognition in human aging: implication for depression and dementia in later life.Rev Neurosci.19991011713910658955
- PeavyGM.LangeKL.SalmonDP.et al.The effects of prolonged stress and APOE genotype on memory and cortisol in older adults.Biol Psychiatry.20076247247817544378
- MackenzieCS.WiprzyckaUJ.HasherL.GoldsteinD.Associations between psychological distress, learning, and memory in spouse caregivers of older adults.J Gerontol B Psychol Sci Soc Sci.20096474274619762451
- LupienSJ.MaheuF.TuM.FioccoA.SchramekTE.The effects of stress and stress hormones on human cognition: implications for the field of brain and cognition.Brain Cogn.20076520923717466428
- UrryHL.van ReekumCM.JohnstoneT.et al.Amygdala and ventromedial prefrontal cortex are inversely coupled during regulation of negative affect and predict the diurnal pattern of cortisol secretion among older adults.J Neurosci.2006264415442516624961
- VanCauter E.LeproultR.KupferDJ.Effects of gender and age on the levels and circadian rhythm icity of plasma cortisol.J Clin Endocrinol Metab.199681246824738675562
- LupienS.LecoursAR.LussierI.SchwartzG.NairNP.MeaneyMJ.Basal cortisol levels and cognitive deficits in human aging.J Neurosci.199414289329038182446
- FerrariE.MagriF.DoriD.et al.Neuroendocrine correlates of the aging brain in humans.Neuroendocrinology.1995614644707783860
- DeuschleM.GotthardtU.SchweigerU.et al.With aging in humans the activity of the hypothalamus-pituitary-adrenal system increases and its diurnal amplitude flattens.Life Sci.199761223922469393943
- KernS.OakesTR.StoneCK.McAuliffEM.KirschbaumC.DavidsonRJ.Glucose metabolic changes in the prefrontal cortex are associated with HPA axis response to a psychosocial stressor.Psychoneuroendocrinology.20083351752918337016
- McEwenBS.Protective and damaging effects of stress mediators.N Engl J Med.19983381711799428819
- YaoYY.LiuDM.XuDF.LiWP.Memory and learning impairment induced by dexamethasone in senescent but not young mice.Eur J Pharmacol.2007574202817884039
- BelucheI.ChaudieuI.NortonJ.et al.Persistence of abnormal cortisol levels in elderly persons after recovery from major depression.J Psychiatr Res.20094377778319054531
- ChaudieuI.BelucheI.NortonJ.BoulengerJP.RitchieK.AncelinML.Abnormal reactions to environmental stress in elderly persons with anxiety disorders: evidence from a population study of diurnal cortisol changes.J Affect Disord.200810630731317727959
- MantellaRC.ButtersMA.AmicoJA.et al.Salivary cortisol is associated with diagnosis and severity of late-life generalized anxiety disorder.Psychoneuroendocrinology.20083377378118407426
- BremmerMA.DeegDJ.BeekmanAT.PenninxBW.LipsP.HoogendijkWJ.Major depression in late life is associated with both hypo- and hyper-cortisolemia.Biol Psychiatry.20076247948617481591
- FioccoAJ.WanN.WeekesN.PirnH.LupienSJ.Diurnal cycle of salivary cortisol in older adult men and women with subjective complaints of memory deficits and/or depressive symptoms: relation to cognitive functioning.Stress.2006914315217060048
- O'BrienJT.LloydA.McKeithI.GholkarA.FerrierN.A longitudinal study of hippocampal volume, cortisol levels, and cognition in older depressed subjects.Am J Psychiatry.20041612081209015514410
- LeeBK.GlassTA.McAteeMJ.et al.Associations of salivary cortisol with cognitive function in the Baltimore memory study.Arch Gen Psychiatry.20076481081817606815
- LiG.CherrierMM.TsuangDW.et al.Salivary cortisol and memory function in human aging.Neurobiol Aging.2006271705171416274857
- ComijsHC.GerritsenL.PenninxBW.BremmerMA.DeegDJ.GeerlingsMl.The association between serum cortisol and cognitive decline in older persons.Am J Geriatr Psychiatry.201018425020094017
- BelucheI.CarrièreI.RitchieK.AncelinML.A prospective study of diurnal cortisol and cognitive function in community-dwelling elderly people.Psychol Med.2010401039104919814852
- ConradCD.Chronic stress-induced hippocampal vulnerability: the glucocorticoid vulnerability hypothesis.Rev Neurosci.20081939541119317179
- RothmanSM.MattsonMP.Adverse stress, hippocampal networks, and Alzheimer's disease.Neuromolecular Med.201012567019943124
- ShelineYl.Hippocampal atrophy in major depression: a result of depression-induced neurotoxicity?Mol Psychiatry.199612982999118352
- ShelineYl.GadoMH.KraemerHC.Untreated depression and hippocampal volume loss.Am J Psychiatry.20031601516151812900317
- NeumeisterA.WoodS.BonneO.et al.Reduced hippocampal volume in unmedicated, remitted patients with major depression versus control subjects.Biol Psychiatry.20055793593715820716
- BremnerJD.VythilingamM.VermettenE.AndersonG.NewcomerJW.CharneyDS.Effects of glucocorticoids on declarative memory function in major depression.Biol Psychiatry.20045581181515050862
- VythilingamM.VermettenE.AndersonGM.et al.Hippocampal volume, memory, and cortisol status in major depressive disorder: effects of treatment.Biol Psychiatry.20045610111215231442
- NewcomerJW.SelkeG.MelsonAK.et al.Decreased memory performance in healthy humans induced by stress-level cortisol treatment.Arch Gen Psychiatry.19995652753310359467
- HetS.RamlowG.WolfOT.A meta-analytic review of the effects of acute cortisol administration on human memory.Psychoneuroendocrinology.20053077178415919583
- SapolskyRM.RomeroLM.MunckAU.How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions.Endocr Rev.200021558910696570
- WeilandNG.OrchinikM.TanapatP.Chronic corticosterone treatment induces parallel changes in N-methyl-D-aspartate receptor subunit messenger RNA levels and antagonist binding sites in the hippocampus.Neuroscience.1997786536629153648
- TataDA.AndersonBJ.The effects of chronic glucocorticoid exposure on dendritic length, synapse numbers and glial volume in animal models: implications for hippocampal volume reductions in depression.Physiol Behav.20109918619319786041
- McLaughlinKJ.BaranSE.ConradCD.Chronic stress- and sex-specific neuromorphological and functional changes in limbic structures.Mol Neurobiol.20094016618219653136
- McEwenBS.Central effects of stress hormones in health and disease: Understanding the protective and damaging effects of stress and stress mediators.Eur J Pharmacol.200858317418518282566
- FrodlTS.KoutsoulerisN.BottlenderR.et al.Depression-related variation in brain morphology over 3 years: effects of stress?Arch Gen Psychiatry.2008651156116518838632
- VermettenE.VythilingamM.SouthwickSM.CharneyDS.BremnerJD.Long-term treatment with paroxetine increases verbal declarative memory and hippocampal volume in posttraumatic stress disorder.Biol Psychiatry.20035469370214512209
- RaskinJ.WiltseCG.SiegalA.et al.Efficacy of duloxetine on cognition, depression, and pain in elderly patients with major depressive disorder: an 8-week, double-blind, placebo-controlled trial.Am J Psychiatry.200716490090917541049
- LenzeEJ.MantellaRC.ShiP.et al.Elevated cortisol in older adults with generalized anxiety disorder is reduced by treatment: a placebo-controlled evaluation of escitalopram. AmJ Geriatr Psychiatry.201119482490
- LenzeEJ.DixonD.MantellaRC.et al.Treatment-related alteration of cortisol predicts change in neuropsychological function during acute treatment of late-life anxiety disorder.Int J Geriatr Psychiatry. In press.
- KangJE.CirritoJR.DongH.CsernanskyJG.HoltzmanDM.Acute stress increases interstitial fluid amyloid-beta via corticotropin-releasing factor and neuronal activity.Proc Natl Acad Sci USA.2007104106731067817551018
- GreenKN.BillingsLM.RoozendaalB.McGaughJL.LaFerlaFM.Glucocorticoids increase amyloid-beta and tau pathology in a mouse model of Alzheimer's disease.J Neurosci.2006269047905616943563
- CsernanskyJG.DongH.FaganAM.et al.Plasma cortisol and progression of dementia in subjects with Alzheimer-type dementia.Am J Psychiatry.20061632164216917151169
- BremmerMA.BeekmanAT.DeegDJ.et al.Inflammatory markers in late-life depression: results from a population-based study.J Affect Disord.200810624925517716746
- SimonNM.McNamaraK.ChowCW.et al.A detailed examination of cytokine abnormalities in Major Depressive Disorder.Eur Neuropsychopharmacol.20081823023317681762
- TiemeierH.HofmanA.van TuijlHR.KiliaanAJ.MeijerJ.BretelerMM.Inflammatory proteins and depression in the elderly.Epidemiology.20031410310712500057
- NewcomerJW.HennekensCH.Severe mental illness and risk of cardiovascular disease.JAMA.20072981794179617940236
- NaritaK.MurataT.HamadaT.et al.Associations between trait anxiety, insulin resistance, and atherosclerosis in the elderly: a pilot cross-sectional study.Psychoneuroendocrinology.20083330531218178323
- EpelES.BlackburnEH.LinJ.et al.Accelerated telomere shortening in response to life stress.Proc Natl Acad Sci USA.2004101173121731515574496
- WolkowitzOM.MellonSH.EpelES.et al.Leukocyte telomere length in major depression: correlations with chronicity, inflammation and oxidative stress-preliminary findings.PLoS One.20116e1783721448457
- SimonNM.SmollerJW.McNamaraKL.et al.Telomere shortening and mood disorders: preliminary support for a chronic stress model of accelerated aging.Biol Psychiatry.20066043243516581033
- SibilleE.SuJ.LemanS.et al.Lack of serotonin 1B receptor expression leads to age-related motor dysfunction, early onset of brain molecular aging and reduced longevity.Mol Psychiatry.2007121042105617420766
- WetherellJL.GatzM.PedersenNL. A longitudinal analysis of anxiety and depressive symptoms. Psychol Aging.20011618719511405307
- HettemaJM.KuhnJW.PrescottCA.KendlerKS.The impact of generalized anxiety disorder and stressful life events on risk for major depressive episodes.Psychol Med.20063678979516515735
- FlintAJ.RifatSL.Two-year outcome of elderly patients with anxious depression.Psychiatry Res.19976623319061801
- DombrovskiAY.MulsantBH.HouckPR.et al.Residual symptoms and recurrence during maintenance treatment of late-life depression.J Affect Disord.2007103778217321595
- AndreescuC.LenzeEJ.DewMA.et al.Effect of comorbid anxiety on treatment response and relapse risk in late-life depression: controlled study.Br J Psychiatry.200719034434917401042
- FlintAJ.RifatSL.Anxious depression in elderly patients. Response to antidepressant treatment.Am J Geriatr Psychiatry.199751071159106374
- SteffensDC.McQuoidDR.Impact of symptoms of generalized anxiety disorder on the course of late-life depression.Am J Geriatr Psychiatry.200513404715653939
- NelsonJC.DelucchiK.SchneiderLS.Anxiety does not predict response to antidepressant treatment in late life depression: results of a metaanalysis.Int J Geriatr Psychiatry.20092453954419334041
- AllgulanderC.LavoriPW.Causes of death among 936 elderly patients with'pure' anxiety neurosis in Stockholm County, Sweden, and in patients with depressive neurosis or both diagnoses.Cornpr Psychiatry.199334299302
- KnightBG.Psychotherapy with Older Adults. Thousand Oaks, CA: Sage.2004
- WetherellJL.HopkoDR.DiefenbachGJ.et al.Cognitive-behavioral therapy for late-life generalized anxiety disorder: who gets better?Behav Ther.200536147156
- StanleyMA.DiefenbachGJ.HopkoDR.Cognitive behavioral treatment for older adults with generalized anxiety disorder. A therapist manual for primary care settings.Behav Modif.2004287311714710708
- ThorpSR.AyersCR.NuevoR.StoddardJA.SorrellJT.WetherellJL.Meta-analysis comparing different behavioral treatments for late-life anxiety.Am J Geriatr Psychiatry.20091710511519155744
- StanleyMA.BeckJG.NovyDM.et al.Cognitive-behavioral treatment of late-life generalized anxiety disorder.J Consult Clin Psychol.20037130931912699025
- PinquartM.DubersteinPR.Treatment of anxiety disorders in older adults: a meta-analytic comparison of behavioral and pharmacological interventions.Am J Geriatr Psychiatry.20071563965117670995
- SchuurmansJ.ComijsH.EmmelkampPM.et al.A randomized, controlled trial of the effectiveness of cognitive-behavioral therapy and sertraline versus a waitlist control group for anxiety disorders in older adults.Am J Geriatr Psychiatry.20061425526316505130
- StanleyMA.WilsonNL.NovyDM.et al.Cognitive behavior therapy for generalized anxiety disorder among older adults in primary care: a randomized clinical trial.JAMA.20093011460146719351943
- PaukertAL.PhillipsL.CullyJA.LoboprabhuSM.LomaxJW.StanleyMA.Integration of religion into cognitive-behavioral therapy for geriatric anxiety and depression.J Psychiatr Pract.20091510311219339844
- ChorpitaBF.DaleidenEL.WeiszJR.Modularity in the design and application of therapeutic interventions.Appi prev Psychol.200511141156
- LangAJ.NormanGJ.CasmarPV.A randomized trial of a brief mental health intervention for primary care patients.J Consult Clin Psychol.2006741173117917154746
- WetherellJL.AyersCR.SorrellJT.et al.Modular psychotherapy for anxiety in older primary care patients.Am J Geriatr Psychiatry. In press.
- WetherellJL.SorrellJT.ThorpSR.PattersonTL.Psychological interventions for late-life anxiety: a review and early lessons from the CALM study.J Geriatr Psychiatry Neurol.200518728215911935
- BrenesGA.McCallWV.WilliamsonJD.StanleyMA.Feasibility and acceptability of bibliotherapy and telephone sessions for the treatment of late-life anxiety disorders.Clin Gerontol.201033626820661315
- SegerstromSC.RoachAR.EvansDR.SchipperLJ.DarvilleAK.The structure and health correlates of trait repetitive thought in older adults.Psychol Aging.20102550551520677888
- D'HudsonG.SalingLL.Worry and rumination in older adults: differentiating the processes.Aging Ment Health.20101452453420480419
- RewstonC.ClarkeC.Moniz-CookE.WaddingtonR.Distinguishing worry from rumination in older people: a preliminary investigation.Aging Ment Health.20071160461117882599
- CroweS.MatthewsC.WalkenhorstE.Relationship between worry, anxiety and thought suppression and the components of working memory in a non-clinical sample.Australian Psychologist.200742170177
- DavisR.Nolen-HoeksemaS.Cognitive inflexibility among ruminators and nonruminators.Cogn Ther Res.200024699711
- von HippelW.VaseyM.GondaT.SternT.Executive function deficits, rumination and late-onset depressive symptoms in older adults.Cogn Ther Res.200832474487
- WhitmerA.BanichM.Trait rumination and inhibitory deficits in long-term memory.Cognition Emotion.201024168179
- WhitmerA.BanichM.Inhibition versus switching deficits in different forms of rumination.Psychol Sci.20071854617576269
- ShelineYl.BarchDM.PriceJL.et al.The default mode network and self-referential processes in depression.Proc Natl Acad Sci USA. 10.200910619421947
- ShelineYl.PriceJL.YanZ.MintunMA.Resting-state functional MRI in depression unmasks increased connectivity between networks via the dorsal nexus.Proc Natl Acad Sci USA. 15.20101071102011025
- PihlajamakiM.SperlingRA.Functional MRI assessment of task-induced deactivation of the default mode network in Alzheimer's disease and at-risk older individuals.Behav Neurol.200921779119847047
- WooSL.PrinceSE.PetrellaJR.HellegersC.DoraiswamyPM.Modulation of a human memory circuit by subsyndromal depression in late life: a functional magnetic resonance imaging study.Am J Geriatr Psychiatry.200917242918790875
- SambataroF.MurtyVP.CallicottJH.et al.Age-related alterations in default mode network: impact on working memory performance.Neurobiol Aging.20103183985218674847
- AndreescuC.ButtersM.LenzeEJ.et al.fMRI activation in late-life anxious depression: a potential biomarker.Int J Geriatr Psychiatiy.200924820828
- LenzeEJ.RollmanBL.ShearMK.et al.Escitalopram for older adults with Generalized Anxiety Disorder: a placebo-controlled trial.JAMA.2009301296303
- WetherellJL.GatzM.CraskeMG.Treatment of generalized anxiety disorder in older adults.J Consult Clin Psychol.200371314012602423
- ilkinsVM.KiossesD.RavdinLD.Late-life depression with comorbid cognitive impairment and disability: nonpharmacological interventions.Clin Interventions Aging.20105323331
- DeyoM.WilsonKA.OngJ.KoopmanC.Mindfulness and rumination: does mindfulness training lead to reductions in the ruminative thinking associated with depression?Explore (NY).2009526527119733812
- BishopSR.What do we really know about mindfulness-based stress reduction?Psychosom Med.200264718311818588
- Kabat-ZinnJ.MassionAO.KristellerJ.et al.Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders.Am J Psychiatry.19921499369431609875
- MillerJJ.FletcherK.Kabat-ZinnJ.Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders.Gen Hosp Psychiatry.1995171922007649463
- GoldinPR.GrossJJ.Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder.Emotion.201010839120141305
- GrossCR.KreitzerMJ.Reilly-SpongM.WinbushNY.SchomakerEK.ThomasW.Mindfulness meditation training to reduce symptom distress in transplant patients: rationale, design, and experience with a recycled waitlist.Clin Trials.20096768919254938
- NguyenHT.GrzywaczJG.LangW.WalkupM.ArcuryTA.Effects of complementary therapy on health in a national U.S. sample of older adults.J Altern Complement Med.20101670170620590482
- RyderPT.WolpertB.OrwigD.Carter-PokrasO.BlackSA.Complementary and alternative medicine use among older urban African Americans: individual and neighborhood associations.J Natl Med Assoc.20081001186119218942280
- LoeraJA.Reyes-OrtizC.KuoYF.Predictors of complementary and alternative medicine use among older Mexican Americans.Complement Ther Clin Pract.20071322423117950177
- MeeksTW.WetherellJL.IrwinMR.RedwineLS.JesteDV.Complementary and alternative treatments for late-life depression, anxiety, and sleep disturbance: a review of randomized controlled trials.J Clin Psychiatry.2007681461147117960959
- ZhangAL.XueCC.LinV.StoryDF.Complementary and alternative medicine use by older Australians.Ann N Y Acad Sci.2007111420421517986583
- DobkinPL.ZhaoQ.Increased mindfulness - The active component of the mindfulness-based stress reduction program?Complement Ther Clin Pract.201017222721168110
- BorkovecTD.InzJ.The nature of worry in generalized anxiety disorder: a predominance of thought activity.Behav Res Ther.1990281531582183759
- ShapiroSL.OmanD.ThoresenCE.PlanteTG.FlindersT.Cultivating mindfulness: effects on well-being.J Clin Psychol.20086484086218484600
- JainS.ShapiroSL.SwanickS.et al.A randomized controlled trial of mindfulness meditation versus relaxation training: effects on distress, positive states of mind, rumination, and distraction.Ann Behav Med.200733112117291166
- MatousekRH.DobkinPL.PruessnerJ.Cortisol as a marker for improvement in mindfulness-based stress reduction.Complement Ther Clin Pract.201016131920129404
- PruessnerJC.DedovicK.PruessnerM.et al.Stress regulation in the central nervous system: evidence from structural and functional neuroimaging studies in human populations - 2008 Curt Richter Award Winner.Psychoneuroendocrinology.20103517919119362426
- BenitezCI.SmithK.VasileRG.RendeR.EdelenMO.KellerMB.Use of benzodiazepines and selective serotonin reuptake inhibitors in middleaged and older adults with anxiety disorders: a longitudinal and prospective study.Am J Geriatr Psychiatry.20081651318165458
- LandiF.OnderG.CesariM.BarillaroC.RussoA.BernabeiR.Psychotropic medications and risk for falls among community-dwelling frail older people: an observational study.J Gerontol A Biol Sci Med Sci.20056062262615972615
- GraySL.LaCroixAZ.HanlonJT.et al.Benzodiazepine use and physical disability in community-dwelling older adults.J Am Geriatr Soc.20065422423016460372
- PaternitiS.DufouilC.AlperovitchA.Long-term benzodiazepine use and cognitive decline in the elderly: the Epidemiology of Vascular Aging Study.J Clin Psychopharmacol.20022228529312006899
- LenzeEJ.MulsantBH.ShearMK.et al.Efficacy and tolerability of citalopram in the treatment of late-life anxiety disorders: results from an 8-week randomized, placebo-controlled trial.Am J Psychiatry.200516214615015625213
- NelsonJC.DelucchiK.SchneiderLS.Efficacy of second generation antidepressants in late-life depression: a meta-analysis of the evidence. AmJ Geriatr Psychiatry.200816558567
- HamiltonM.The assessment of anxiety states by rating.Br J Med Psychol.195932505513638508
- ButtersMA.BhallaRK.AndreescuC.et al.Changes in neuropsychological functioning following treatment of Generalized Anxiety Disorder.Br J Psychiatry.201119921121821727232
- KatzIR.ReynoldsCF.3rd.AlexopoulosGS.HackettD.Venlafaxine ER as a treatment for generalized anxiety disorder in older adults: pooled analysis of five randomized placebo-controlled clinical trials.J Am Geriatr Soc.200250182512028242
- DavidsonJ.AllgulanderC.PollackMH.et al.Efficacy and tolerability of duloxetine in elderly patients with generalized anxiety disorder: a pooled analysis of four randomized, double-blind, placebo-controlled studies.Hum Psychopharmacol.20082351952618478624
- Laghrissi-ThodeF.PollockBG.MillerMC.MulsantBH.AltieriL.FinkelMS.Double-blind comparison of paroxetine and nortriptyline on the postural stability of late-life depressed patients.Psychopharmacol Bull.1995316596638851637
- DiemSJ.BlackwellTL.StoneKL.et al.Use of antidepressants and rates of hip bone loss in older women: the study of osteoporotic fractures.Arch Intern Med.20071671240124517592096
- YuanY.TsoiK.HuntRH.Selective serotonin reuptake inhibitors and risk of upper Gl bleeding: confusion or confounding?Am J Med.200611971972716945603
- FabianTJ.AmicoJA.KrobothPD.et al.Paroxetine-induced hyponatremia in older adults: a 12-week prospective study.Arch intern Med.200416432733214769630
- MontgomeryS.ChatamraK.PauerL.WhalenE.BaldinettiF.Efficacy and safety of pregabalin in elderly people with generalised anxiety disorder.Br J Psychiatry.200819338939418978320
- ChungMY.MinKH.YJ.KimSS.KimWC.EM.Efficacy and tolerability of mirtazapine and sertraline in Korean veterans with posttraumatic stress disorder: a randomized open label trial.Hum Psychopharmacol.20041948949415378676
- EnglishBA.JewellM.JewellG.AmbroseS.DavisLL.Treatment of chronic posttraumatic stress disorder in combat veterans with citalopram: an open trial.J Clin Psychopharmacol.200626848816415713
- RaskindMA.PeskindER.HoffDJ.et al.A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with post-traumatic stress disorder.Biol Psychiatry.20076192893417069768
- RampelloL.AlvanoA.RaffaeleR.MalaguarneraM.VecchioI.New possibilities of treatment for panic attacks in elderly patients: escitalopram versus citalopram.J Clin Psychopharmacol.200626677016415709
- SheikhJl.LauderdaleSA.CassidyEL.Efficacy of sertraline for panic disorder in older adults: a preliminary open-label trial.Am J Geriatr Psychiatry.20041223015010352
- KimuraM.TatenoA.RobinsonRG.Treatment of poststroke generalized anxiety disorder comorbid with poststroke depression: merged analysis of nortriptyline trials.Am J Geriatr Psychiatry.20031132032712724111
- MorinigoA.BlancoM.LabradorJ.MartinJ.NovalD.Risperidone for resistant anxiety in elderly persons.Am J Geriatr Psychiatry.200513818215653944
- FavaGA.RuiniC.RafanelliC.Sequential treatment of mood and anxiety disorders.J Clin Psychiatry.2005661392140016420076
- ArceE.SimmonsAN.LoveroKL.SteinMB.PaulusMP.Escitalopram effects on insula and amygdala BOLD activation during emotional processing.Psychopharmacology (Berl).200819666167218058090
- McNallyRJ.Mechanisms of exposure therapy: how neuroscience can improve psychological treatments for anxiety disorders.Clin Psychol Rev.20072775075917292521
- FavaGA.ParkSK.SoninoN.Treatment of recurrent depression.Expert Rev Neurother.200661735174017144786
- ButlerAC.ChapmanJE.FormanEM.BeckAT.The empirical status of cognitive-behavioral therapy: a review of meta-analyses.Clin Psychol Rev.200626173116199119
- BarrowcloughC.KingP.ColvilleJ.RussellE.BurnsA.TarrierN.A randomized trial of the effectiveness of cognitive-behavioral therapy and supportive counseling for anxiety symptoms in older adults.J Consult Clin Psychol.20016975676211680552
- WestraHA.StewartSH.Cognitive behavioural therapy and pharmacotherapy: complementary or contradictory approaches to the treatment of anxiety?Clin Psychol Rev.1998183073409564583
- FoaEB.FranklinME.MoserJ.Context in the clinic: how well do cognitive-behavioral therapies and medications work in combination?Biol Psychiatry.20025298799712437939
- BarlowDH.GormanJM.ShearMK.WoodsSW.Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: a randomized controlled trial.JAMA.20002832529253610815116
- RaffaSD.StoddardJA.WhiteKS.et al.Relapse following combined treatment discontinuation in a placebo-controlled trial for panic disorder.J Nerv Ment Dis.200819654855518626295
- BryantC.Anxiety and depression in old age: challenges in recognition and diagnosis.Int Psychogeriatr.20102251151320122303
- SanislowCA.PineDS.QuinnKJ.et al.Developing constructs for psychopathology research: research domain criteria.J Abnorm Psychol.201011963163920939653
- BrownSL.SmithDM.SchulzR.et al.Caregiving behavior is associated with decreased mortality risk.Psychol Sci.20092048849419320860
- HofmannSG.SawyerAT.WittAA.OhD.The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review.J Consult Clin Psychol.20107816918320350028
- CardaciottoL.HerbertJD.FormanEM.MoitraE.FarrowV.The assessment of present-moment awareness and acceptance: the Philadelphia Mindfulness Scale.Assessment.20081520422318187399
- BrownKW.RyanRM.The benefits of being present: mindfulness and its role in psychological well-being.J Pers Soc Psychol.20038482284812703651
- BaerRA.SmithGT.AllenKB.Assessment of mindfulness by self-report: the Kentucky inventory of mindfulness skills.Assessment.20041119120615358875
- BaerRA.SmithGT.HopkinsJ.KrietemeyerJ.ToneyL.Using self-report assessment methods to explore facets of mindfulness.Assessment.200613274516443717
- WalachH.BuchheldN.ButtenmüllerV.KleinknechtN.SchmidtS.Measuring mindfulness--the freiburg mindfulness inventory (FMI).Personality Individual Differences.20064015431555
- CollinsRL.KashdanTB.GollnischG.The feasibility of using cellular phones to collect ecological momentary assessment data: application to alcohol consumption.Exp Clin Psychopharmacol.2003117312622345
- CainAE.DeppCA.JesteDV.Ecological momentary assessment in aging research: A critical review.J Psychiatr Res.20094398799619272611
- JeanneAT.Ocepek-WeliksonK.KleinmanM.et al.Analysis of differential item functioning in the depression item bank from the Patient Reported Outcome Measurement Information System (PROMIS): an item response theory approach.Psychology Science.201051
- SlaterCH.BickD.Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation.JAMA.19942711377
- HaysRD.BjornerJB.RevickiDA.SpritzerKL.CellaD.Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items.Qual Life Res.20091887388019543809
- LiJ.CowdenLG.KingJD.et al.Effects of chronic stress and interleukin-10 gene polymorphisms on antibody response to tetanus vaccine in family caregivers of patients with Alzheimer's disease.Psychosom Med.20076955117634568
- OrsilloSM.Acceptance and Mindfulness-Based Approaches to Anxiety: Conceptualization and Treatment. New York, NY; Springer Verlag;2005
- LauMA.BishopSR.SegalZV.et al.The Toronto Mindfulness Scale: development and validation.J Clin Psychol.2006621445146717019673
- BaerRA.WalshE.LykinsELB.Assessment of mindfulness.Clinical Handbook of Mindfulness.2009153168
- GrossmanP.On measuring mindfulness in psychosomatic and psychological research.J Psychosom Res.20086440540818374739
- SchwartzJE.StoneAA.Strategies for analyzing ecological momentary assessment data.Health Psychology.19981769459065
- KamarckTW.ShiftmanS.WethingtonE.ContradaRJ.BaumA.Measuring Psychosocial Stress Using Ecological Momentary Assessment Methods. New York, NY: Springer Publishing Co;2011
- StoneAA.ShiftmanS.Capturing momentary, self-report data: a proposal for reporting guidelines.Ann Behav Med.20022423624312173681
- WenzeSJ.MillerIW.Use of ecological momentary assessment in mood disorders research.Clin Psychol Rev.20103079480420619520
- ShiftmanS.StoneAA.HuffordMR.Ecological momentary assessment.Annu Rev Clin Psychol.2008413218509902
- TrullTJ.Ebner-PriemerUW.Using experience sampling methods/ecological momentary assessment (ESM/EMA) in clinical assessment and clinical research: introduction to the special section.Psychol Assess20092145746219947780
- Ebner-PriemerUW.TrullTJ.Ecological momentary assessment of mood disorders and mood dysregulation.Psychol Assess.20092146347519947781
- Ramel1W.GoldinPR.CarmonaPE.McQuaidJR.The effects of mindfulness meditation on cognitive processes and affect in patients with past depression.Cognitive Ther Res.200428433455
- GoldinP.RamelW.GrossJ.Mindfulness meditation training and self-referential processing in social anxiety disorder: Behavioral and neural effects.J Cogn Psychother.200923242257
- GoldinPR.GrossJJ.Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder.Emotion.201010839120141305
- LemkeMR.BroderickA.ZeitelbergerM.HartmannW.Motor activity and daily variation of symptom intensity in depressed patients.Neuropsychobiology .19973657619267852
- RaouxN.BenoitO.DantchevN.et al.Circadian pattern of motor activity in major depressed patients undergoing antidepressant therapy: relationship between actigraphic measures and clinical course.Psychiatry Res.19945285988047624
- VolkersAC.TulenJH.Van Den BroekWW.BruijnJA.PasschierJ.PepplinkhuizenL.24-Hour motor activity after treatment with imiprarnine or fluvoxarnine in major depressive disorder.Eur Neuropsychopharmacol.20021227327812126865
- CobbJP.MindrinosMN.Miller-GrazianoC.et al.Application of genome-wide expression analysis to human health and disease.Proc Natl Acad Sci USA.20051024801480615781863
- DusekJA.OtuHH.WohlhueterAL.et al.Genomic counter-stress changes induced by the relaxation response.PLoS One.20083e257618596974
- MillerGE.ChenE.Life stress and diminished expression of genes encoding glucocorticoid receptor and beta2-adrenergic receptor in children with asthma.Proc Natl Acad Sci U S A.20061035496550116567656
- MillerGE.ChenE.SzeJ.et al.A functional genomic fingerprint of chronic stress in humans: blunted glucocorticoid and increased NF-kappaB signaling.Biol Psychiatry.20086426627218440494
- BlankS.LenzeEJ.MulsantBH.et al.Outcomes of late-life anxiety disorders during 32 weeks of citalopram treatment.J Clin Psychiatry.20066746847216649835
- LauEX.RapeeRM.Prevention of Anxiety Disorders.Curr Psychiatry Rep.20111325826621484451
- FlintAJ.Epidemiology and comorbidity of anxiety disorders in the elderly.Am J Psychiatry.19941516406498166303
- TrollorJN.AndersonTM.SachdevPS.BrodatyH.AndrewsG.Prevalence of mental disorders in the elderly: the Australian National Mental Health and Well-Being Survey.Am J Geriatr Psychiatry.20071545546617545446
- CairneyJ.CornaLM.VeldhuizenS.HerrmannN.StreinerDL.Comorbid depression and anxiety in later life: patterns of association, subjective well-being, and impairment.Am J Geriatr Psychiatry.20081620120818310551
- GumAM.King-KallimanisB.KohnR.PhilM.Prevalence of mood, anxiety, and substance abuse disorders for older Americans in the National Comorbidity Survey-replication.Am J Geriatr Psychiatry.20091276978119700949