Abstract
Background
Although affect dysregulation is considered a core component of borderline personality disorder (BPD) and somatoform disorders (SoD), remarkably little research has focused on the prevalence and nature of affect dysregulation in these disorders. Also, despite apparent similarities, little is known about how dysfunctional under- and overregulation of affect and positive and negative somatoform and psychoform dissociative experiences inter-relate. Prior studies suggest a clear relationship between early childhood psychological trauma and affect dysregulation, especially when the caretaker is emotionally, sexually, or physically abusing the child, but how these relate to under- and overregulation while differentiating for developmental epochs is not clear. Although an elevated risk of childhood trauma exposure or complex posttraumatic stress disorder (CPTSD) symptoms has been reported in BPD and SoD, trauma histories, dysfunctional affect regulation, dissociation, PTSD, and CPTSD were never assessed in unison in BPD and/or SoD.
Method
BPD and/or SoD diagnoses were confirmed or ruled out in 472 psychiatric inpatients using clinical interviews. Dysfunctional under- and overregulation of affect and somatoform and psychoform dissociation, childhood trauma-by-primary-caretaker (TPC), PTSD, and CPTSD were all measured using self reports.
Results
No disorder-specific form of dysfunctional affect regulation was found. Although both BPD and SoD can involve affect dysregulation and dissociation, there is a wide range of intensity of dysfunctional regulation phenomena in patients with these diagnoses. Evidence was found for the existence of three qualitatively different forms of experiencing states: inhibitory experiencing states (overregulation of affect and negative psychoform dissociation) most commonly found in SoD, excitatory experiencing states (underregulation of affect and positive psychoform dissociation) most commonly found in BPD, and combination of inhibitory and excitatory experiencing states commonly occurring in comorbid BPD+SoD. Almost two-thirds of participants reported having experienced childhood TPC. Underregulation of affect was associated with emotional TPC and TPC occurring in developmental epoch, 0–6 years of age. Overregulation of affect was associated with physical TPC. Almost a quarter of all participants met the criteria for CPTSD. BPD+SoD patients had the most extensive childhood trauma histories and were most likely to meet CPTSD criteria, followed by BPD, psychiatric comparison (PC), and SoD. The BPD+SoD and BPD reported significantly higher levels of CPTSD than the SoD or PC groups but did not differ from each other except for greater severity of CPTSD somatic symptoms by the BPD+SoD group.
Conclusion
Three qualitatively different forms of dysfunctional regulation were identified: inhibitory, excitatory, and combined inhibitory and excitatory states. Distinguishing inhibitory versus excitatory states of experiencing may help to clarify differences in dissociation and affect dysregulation between and within BPD and SoD patients. Specific interventions addressing overregulation in BPD, or underregulation in SoD, should be added to disorder-specific evidence-based treatments. CPT is particularly prevalent in BPD and BPD+SoD and is differentially associated with under- and overregulation of affect depending on the type of traumatic exposure. CPTSD warrants further investigation as a potential independent syndrome or as a marker identifying a sub-group of affectively, or both affectively and somatically, dysregulated patients diagnosed with BPD who have childhood trauma histories.
Mentors: Prof. Dr. M.J.M. van Son, Prof. Dr. O. van der Hart (Utrecht University, Department of Psychology) and Prof. Dr. P.G.M. van der Heijden (Utrecht University, Department of Methodology and Statistics). Theses defended in Utrecht University, Faculty of Social Sciences, June 10, 2011. For the abstract or full text in other languages, please see Supplementary files under Reading Tools online. (Published: 13 September 2012)
The following are three clinical vignettes: A 42-year-old woman developed a full blown pseudo-epileptic seizure. Three days later, she was able to talk about what happened that particular day. It seems that she had telephoned the receptionist of the outpatient facility on Friday at 17.00 hours because she wanted to talk to her psychotherapist. Unfortunately, the psychotherapist had already gone on weekend leave. Subsequent to hearing this, she developed the pseudo-epileptic seizure.
A 30-year-old woman flew into a rage, called names, and became hyperaroused during group therapy when she was asked to wait with her contribution to the discussion and first listen to reflections of her group members on her behavior. She continued to be highly aroused and could not return to baseline-arousal until several hours later after extensive reassurance by the group members and clinicians that she was “being a good girl.”
A 27-year-old man (semi-professional ice-skater) was admitted to the clinic when the rehabilitation of his broken leg was not progressing well. He stated that his leg continued to feel weak and unstable, and he had just heard that his potential professional career as an ice-skater was over. During his visits to the rehabilitation center he had presented with emotional explosiveness and self-harming behavior that he seemed unable to recognize as a problem.
These three vignettes can be regarded as examples of dysfunctional self-regulation and affect regulation in response to social-emotion-eliciting situations (Van Dijke, Citation2008; Van der Hart, Van Dijke, Van Son, & Steele, Citation2000). The first vignette highlights the inability to express one's emotions verbally when confronted with intolerable affect, such that emotions instead are somatically expressed and become overregulated. Difficulties differentiating, analyzing, and verbalizing emotions hinder dealing with challenges in everyday life. Here, the attempt to self-regulate is dysfunctional as the psychological burden (intolerable emotional arousal) is not contained and is being expressed in physical symptoms, while the core of the problem is left unaddressed.
The second vignette highlights underregulation of affect and the difficulties one can have regulating levels of arousal to baseline and keeping emotions within a window of tolerance in interpersonal contexts that have personal or posttraumatic significance. The agitated response elicited by what appeared to be relatively mild limit-setting from the group leader and feedback from group members is indicative of the patient's difficulty in both maintaining emotional arousal within a tolerable window and recovering from distress. The apparent regression reflected by the patient's need (or the group members’ perception of her as needing) to be soothed like a young child suggests that this underregulation of affect may have originated in much earlier life experiences in which the patient may not have been provided with (or able to accept and utilize) responsive caregiving.
The third vignette highlights the combination of a highly aroused affective experiencing combined with reporting diminished capacity for self-reflection and emotional self-awareness. It may be the case that symptoms of dysfunctional affect regulation were already present before this man broke his leg, and the intensive sports exercises that he engaged in as a result of his semi-professional athletic career may have helped him regulate himself. However, when confronted with forced immobility, arousal and distress could no longer be channeled or expressed in a physical way, leading him to have unanticipated difficulties recognizing, describing, and expressing his emotions except in the formof frustration and impulsivity. As a result, this man may be experiencing a combination of difficulties with overregulation (his characteristic mode of coping) and underregulation (his reaction to an unprecedented physical crisis that may have shaken his confidence in himself, his career, and his future).
Despite a vast amount of research on the benefits of successfully regulating affect for our mental and somatic well-being (e.g., Nyklíček, Temoshok, & Vingerhoets, Citation2004), dysfunctional affect regulation for psychiatric patients remains unclear. However, it has been established that affect dysregulation is involved in the etiology of psychopathology (e.g., Bradley, Citation2000). Dysfunctional regulation is often described in patients with complex psychopathology and mental disorders, such as a combination of DSM-IV-TR axis I, axis II, and axis III disorders, and it is also considered to be a maintenance factor or predictor of attrition and poor therapy outcome (Ford & Kidd, Citation1998). Two mental disorders that have been theoretically, empirically, and historically associated with affect dysregulation are borderline personality disorder (BPD; APA, Citation2004; Silbersweig et al., Citation2007) and somatoform disorders (SoD; Roelofs, Keijsers, Hoogduin, Naring, & Moene, Citation2002). Some even considered BPD (e.g., Linehan, Citation1993; Linehan et al., Citation2006) and SoD (Waller & Scheidt, Citation2006) primarily to be disorders of affect regulation. Also, symptoms that reflect dysfunctional affect regulation and fundamentally altered beliefs about self, relationships, and the world, which go beyond the symptoms in previous conceptualizations of posttraumatic stress disorder (PTSD), have been proposed for inclusion in the complex PTSD (CPTSD; Şar, Citation2011) diagnosis (see www.dsm5.org). These dysfunctional affect regulation and altered schema symptoms were cardinal features of a separate diagnosis of CPTSD or Disorders of Extreme Stress Not Otherwise Specified (DESNOS; Van der Kolk, Roth, Pelcovitz, Sunday, & Spinazzola, Citation2005) that was proposed and tested in the PTSD field trial for the fourth revision of the Diagnostic and Statistical Manual (APA, Citation2004)—although the CPTSD symptoms ultimately were designated as associated features of PTSD rather than included as a separate diagnosis or in the PTSD diagnosis (Van der Kolk et al., Citation2005). The currently proposed revision of the PTSD diagnosis raises the possibility that these complex symptoms may now serve as a basis for extending that diagnosis beyond its traditional focus on anxiety and dysphoria symptoms.
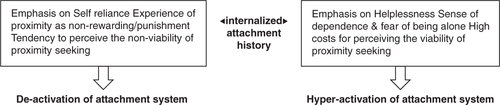
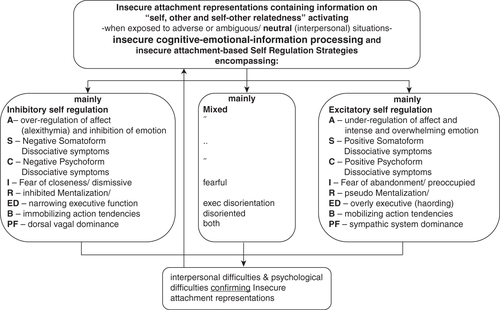
However, the nature and distribution of dysfunctional affect regulation, and its relations with associated phenomena and retrospectively reported potentially traumatizing events seems to be qualitatively different. Whereas some patients react to adversities with inhibited experiencing and social withdrawal, others react hyper-emotionally and tend to cling to a significant other to alleviate stress and regulate to base-line. Attachment theory has become a prominent conceptual framework for understanding the process of development of affect regulation and dysregulation (Allen & Fonagy, Citation2006; Mikulincer & Shaver, Citation2004; ). Bowlby (Citation1988) highlighted the anxiety-buffering and physical protection functions of close relationships and conceptualized proximity-seeking as an affectively regulated alternative to the instinctive and typically dysregulated fight–flight responses. He also emphasized the importance of interpersonal (traumatic) experiences as sources of individual differences in affect (dys)regulation across the lifespan. In line with this, Van Dijke (Citation2008) described dysfunctional regulation as operating in vicious cycles that approach the long-term sequelae of trauma-by-primary-caretaker from a developmental perspective. Dysfunctional regulation may present in patients in three qualitatively different forms: Inhibitory-, Excitatory-, and combined Inhibitory & Excitatory (IE)-regulation. Symptoms include disturbances in self-regulation across several domains of functioning, including but not limited to affective, cognitive, and somatic functioning. Activation of dysfunctional regulation seems to follow trauma-by-primary-caretaker associated negatively biased cognitive–emotional information processing (Van Harmelen, De Jong, Glashouwer, Spinhoven, Penninx, & Elzinga, Citation2010). However, when potentially neutral situations are processed and evaluated as threatening or potentially harmful, dysfunctional regulation is activated false positively. Inhibitory regulation when activated based upon biased (negative-avoidant) cognitive–emotional information processing encompasses, among others, overregulation of affect, negative psychoform and somatoform dissociation, fear of closeness in adult relationships, inhibited mentalization, narrowed executive functioning, immobilizing action tendencies, and dominance of the sympathetic system.
Table 1 Demographic characteristics of the study groups and the total sample
Consequently, this results in interpersonal misunderstanding and disappointments, which in turn condition and uphold the insecure attachment representation/working models turning into inhibitory regulation vicious circle. Excitatory regulation when activated based upon biased (negative-anxious) cognitive–emotional information processing encompasses, e.g., underregulation of affect, positive psychoform and somatoform dissociation, fear of abandonment in adult relationships, pseudo mentalization, overly executive functioning, mobilizing action tendencies, and dominance of the dorsal vagal system. Consequently, this results in interpersonal misunderstanding and disappointments, which in turn condition and uphold the insecure attachment representation/working models turning into an excitatory regulation vicious circle. Combined IE-regulation encompasses both inhibitory and excitatory domains and symptoms that can present alternating or in combinations in patients. It should be noted that dysfunctionally regulated persons, when confronted with internal or external adverse events, risk not meeting a sense of personal efficacy, resilience, and optimism (Mikulincer, Shaver, & Pereg, Citation2003). summarizes the hypothesized relationships for dysfunctional regulation operating in vicious cycles that were discussed above.
Fig.2 Dysfunctional regulation operating in vicious cycles.
Note: A=affect; S=soma; C=cognition; I=interaction; R=reflective function; ED=exec dysfunction; B=behavior; PF=psycho-physiological.
The quality of dysfunctional affect regulation seems differentially conceptualized for mental disorders. BPD has been primarily associated with hyper-arousal and being overwhelmed with emotions, while SoD has been primarily associated with numbing and difficulties differentiating, analyzing, and verbalizing emotions. Reviewing the literature, no study systematically assessed both forms of dysfunctional affect regulation in BPD and SoD in unison. This dissertation assesses the hypothesized relationships for dysfunctional regulation in BPD and SoD, under- and overregulation of affect, positive and negative psychoform and somatoform dissociation, self-reported trauma histories on trauma-by-primary-caretaker and symptoms of PTSD and CPTSD.
Paticipants and procedure
Participants were consecutive admissions to two adult inpatient psychotherapy treatment centers, Centre for Psychosomatic Medicine, Altrecht Mental Health, Utrecht (N=117), and Centre for Personality Disorders, Delta Psychiatric Hospital, Rotterdam (N=355). During intake diagnoses of BPD and SoD were made according to the DSM-IV criteria by trained and officially registered clinicians (psychiatrists, psychotherapists). Where possible, general practice and former hospital records were obtained (with patient's consent) and studied. All participants had a well-documented history of somatic and/or psychiatric symptoms. All had received previous inpatient or outpatient treatment at psychiatric or somatic hospitals and were referred for specialized psychotherapy. A total of 472 patients were included in the study. As BPD and SoD occur also comorbidly, a group consisting of patients diagnosed with comorbid BPD+SoD, as well as in a psychiatric comparison group were included (BPD=120; SoD=159; N=129; PC=64). No significant effects were found for age, gender, and level of education on the dependent variables. Final decision for inclusion in the study was after multi-disciplinary consensus on diagnoses and clinical presentation in relation to self-reported findings. After admission, all patients participated in the multi-center project “Clinical Assessment of Trauma-Related Self and Affect Dysregulation” (Van Dijke, Citation2008). This is a diagnostic and orientation period integrated in the first phase (1–6 weeks) of psychotherapeutic inpatient group treatment. Assessment was started in the second week after acclimatizing to the therapeutic milieu and was finished before the end of the fifth week. Evaluation of all assessments, multi-disciplinary observations, participants’ findings (including the findings reported by the participants’ significant other), and evaluation of the prospective treatment possibilities and treatment goals took place in the sixth week after admission and before definite admission to the full program.
For all participants, history of potential brain damage (e.g., head injury, electroshock therapy) and the use of psychotropic medications that may impair executive function (e.g., anti-psychotics, neuroleptics, lithium) were exclusion criteria. Moreover, for the PC group, severe mental illness (i.e., schizophrenia, other psychotic disorders, bipolar disorder), eating disordered with severe underweight, or imminent suicidality that would interfere with cognitive functioning, and developmental disorders (i.e., Autism Spectrum Disorders or Attention Deficit Hyperactivity Disorder) were exclusion criteria. All psychiatric control patients met DSM-IV criteria for generalized anxiety disorder and/or unipolar depression with sufficient psychosocial impairment that admission for inpatient psychiatric care was indicated.
This study was approved by the local ethics committee (Toetsingscommissie Patientgebonden Wetenschappelijk Onderzoek, Arnhem, the Netherlands). After a complete description of the study and procedure, subjects provided written informed consent to participate, according to the Declaration of Helsinki.
Summary of major findings
The first study (Chapter 2) focusses on the differentiation of two qualitatively different forms of dysfunctional affect regulation and whether these two forms are indeed differentially distributed among patients diagnosed with BPD or SoD. If BPD is indeed a disorder of affect regulation and if indeed dysfunctional affect regulation involves being overwhelmed with negative affective experiencing and having difficulties downregulating negative affect, then all patients diagnosed with BPD should report underregulation of affect and significantly more so than other study groups. Also, if SoD is indeed a disorder of affect regulation and if dysfunctional affect regulation involves being numb or inhibited, and having difficulties addressing emotions, then all patients diagnosed with SoD should report overregulation of affect, and significantly more so, than other study groups. However, if there are indeed two qualitatively different forms of dysfunctional affect regulation present in BPD and SoD, then it might be expected that the comborbid BPD+SoD study group would report both forms of dysfunctional affect regulation. Furthermore, a PC group would not or would significantly less often report these forms of dysfunctional affect regulation. The results from this study show that under- and overregulation of affect were weakly related. Using MANOVA, a statistically significant difference between all diagnostic groups was found for affect dysregulation, with a large effect size for underregulation of affect but small for overregulation of affect. Although all patients report some difficulties with affect regulation not all patients report clinically significant dysfunctional affect regulation and no disorder-specific form of dysfunctional affect regulation was found. Regression analyses using contrast testing between study groups revealed “profiles” for each disorder suggested that PC was inversely associated with overregulation of affect. BPD was associated with underregulation of affect and comorbid BPD+SoD was associated with both under- and overregulation of affect. Over a quarter of the total sample reported clinically significant high levels of under- and overregulation. Significant differences between all groups were found using contrast testing for distribution. Underregulation was most prevalent in BPD, overregulation, when prevalent, was most prevalent in SoD, and a combination of under-and overregulation was most prevalent in BPD+SoD according to study hypotheses. Three qualitatively different forms of dysfunctional affect regulation were found and discrimination of these forms is warranted.
The second study (Chapter 3) concentrates on the question if and how positive and negative psychoform and somatoform dissociative symptoms are related to over- and underregulation of affect. Trauma-related overwhelming affect and its dysfunctional regulation compromises the integrative capacities associated with cognitive–emotional information processing so that information becomes disassociated, disorganized, or disoriented (Courtois & Ford, Citation2009). A few contemporary authors have noted the existence of positive dissociative symptoms (e.g., dissociative flashback episodes; APA, Citation2004; Nijenhuis, Citation2004; Van der Hart, Nijenhuis, & Steele, Citation2006; Van der Hart et al., Citation2000). However, most have not observed this and report only of negative phenomena (e.g., Lanius et al., Citation2010). Negative dissociative symptoms refer to apparent losses of functions, for example, of memory, motor control, skills, and somatosensory awareness. Negative psychoform dissociative symptoms, among others, include loss of memory (amnesia) and loss of affective experiencing (numbness), loss of needs and will (abulia), loss of critical function (a cognitive action) resulting in suggestibility and difficulty thinking things through, loss of previously existing skills, and diminished sense of self.
Negative somatoform dissociative symptoms, among others, involve losses of sensory, perceptual or motor functions, e.g., analgesia, paralysis, and aphonia. Positive psychoform dissociative symptoms include traumatic memories and nightmares that have affective, cognitive, and somatosensory components, such as dissociative flashbacks and full re-experiencing of traumatizing events, as well as intruding voices, thoughts, and amplified affective experiencing. Positive somatoform dissociative symptoms include intrusions of sensorimotor aspects of traumatic re-experiences, including pain, uncontrolled behaviors, such as tics, sensory distortions, and pseudo-epileptic seizures. Reviewing the literature, no study systematically assessed both forms of dysfunctional affect regulation and positive and negative symptoms of psychoform and somatoform dissociation in unison in BPD or SoD. If positive dissociative symptoms can be distinguished from negative dissociative phenomena by means of self-report, and dissociation and dysfunctional affect regulation are related but distinct phenomena, patients should be able to report distinct forms of experiencing: inhibitory and excitatory experiencing. Excitatory reports (reports of positive dissociation and underregulation of affect) would be more expected in patients diagnosed with BPD. Inhibitory reports (reports of negative dissociation and overregulation of affect) would be more expected in patients diagnosed with SoD. For the comorbid BPD+SoD group, reports of combinations of both forms of dysfunctional affect regulation with both positive and negative dissociation would be more expected, when compared to all other groups of patients. Results show that positive and negative dissociative symptoms can be discriminated using self report and are related but distinct phenomena. This study found that positive and negative dissociative psychoform and somatoform symptoms can be differentiated. Affect dysregulation and dissociation are related but different phenomena; underregulation of affect was moderately to strongly related to positive psychoform and negative psychoform dissociation. Overregulation was weakly related to positive psychoform and negative psychoform dissociation.
However, under- and overregulation were unrelated to positive and negative somatoform dissociation. When assessing the relative strength of inhibitory and excitatory experiencing phenomena with the presence of BPD, SoD, BPD+SOD, or other psychiatric disorders with sequential regression analyses using contrasts the inclusion of all inhibitory and excitatory experiencing phenomena (model 2) improved the fit of the model significantly, and no differences were found between BPD and BPD+SoD. Almost 10% of the total sample reported high levels of psychoform and somatoform dissociation. When comparing the groups using contrasts significant differences were found. The SoD group reported mostly low levels of dissociation, least high levels of psychoform dissociation, and least high levels of both psychoform and somatoform dissociation. In contrast, BPD+SoD reported the least low levels of dissociation, and most high levels of both psychoform and somatoform dissociation, or high levels of psychoform dissociation only that did the other groups.
The third study (Chapter 4) addressed the relation between dysfunctional affect regulation in adulthood and self-reported childhood trauma-by-primary-caretaker (CPT), while distinguishing developmental epochs vulnerable for the development of affect regulation. Several authors have addressed the negative impact of misattuned interaction and adverse interpersonal experiences on the post-natal development of the social-affective brain areas, the social-emotional personality, and the development of psychopathology (e.g., Courtois & Ford, Citation2009; Cozolino, Citation2006; Lyons-Ruth, Dutra, Schuder, & Bianchi, Citation2006). Adverse childhood interpersonal experiences when compared to interpersonal adversities later in life or natural disasters result in more complex trauma-related symptoms (e.g., Pelcovitz, Van der Kolk, Roth, Mandel, & Resick, Citation1997; Roth, Newman, Pelcovitz, Van der Kolk, & Mandel, Citation1997; Van der Kolk et al., Citation2005). However, a review of the literature revealed that no empirical study exists that specifically addressed the relations between under- and overregulation of affect and the nature of the trauma-by-primary-caregiver (emotional, physical, and sexual trauma) while distinguishing developmental epochs (0–6 years, 7–12 years, and 13–18 years) vulnerable for the development of affect regulation. Reports of potentially traumatizing events in the developmental epoch 0–6 years would be associated with both and more dysfunctional affect regulation compared to reports in the developmental epochs 7–12 years and 13–18 years.
The results proved that almost two-thirds of the participants reported at least one instance of traumatization-by-a-primary-caretaker. However, the relationships generally were not strong, with significant correlations only between physical TPC and overregulation of affect, and adolescent-epoch caretaker traumatization and emotional TPC and underregulation of affect. For a subsample of the patients meeting DSM IV-TR criteria for PTSD, analyses were repeated. On a dimensional level only associations for underregulation of affect with PTSD total score proved significant, and for overregulation with PTSD total score and with developmental epoch 0–6 years. On a categorical level only the association between PTSD-diagnoses and overregulation remained its significance. Cross-tabulation analyses of the likelihood of reporting TPC for the study groups proved that approximately half of the SoD and PC groups reported a history of TPC, compared to 70–80% of the BPD and BPD+SoD participants. The BPD+SoD group was significantly more likely than other groups to report TPC and the SoD group was significantly less likely to report TPC. The MANOVA exploring group differences in the severity of each TPC-type, the developmental epochs at which TPC occurred in childhood, and the two types of affect dysregulation resulted in a statistically significant difference overall. When the results for the dependent variables were considered separately, between group differences were found for all variables, but not for sexual TPC. After controlling for the effect of trauma history underregulation levels differed with a large effect size but overregulation differed with a smaller effect size between the diagnostic sub-groups. Overall, the BPD+SoD group reported the most complex trauma histories, with significant more reports for severe physical-TPC across all three childhood developmental epochs. Both the BPD+SoD and BPD groups reported more emotional TPC, under- and overregulation of affect than did the SoD and psychiatric control groups.
The fourth study (Chapter 5) concentrates on the presence of CPTSD in BPD and SoD. Historically, symptoms of both BPD and SoD have been associated with interpersonal trauma and hysteria (Briquet, Citation1859). Exposure to sustained, repeated or multiple potentially traumatizing events, particularly when a primary caretaker is involved, has been proposed to result in a complex symptom presentation that includes not only dissociative and posttraumatic stress symptoms, but also other symptoms reflecting disturbances predominantly in affective and interpersonal self-regulatory capacities (Cloitre et al., Citation2009; Paivio & Pascual-Leone, Citation2010). This complex symptom presentation does not seem to be encompassed by any single DSM-IV-TR or ICD-10 disorder (Ford, Citation2005; Van der Kolk et al., Citation2005). In an attempt to capture this complex symptom presentation, that includes not only posttraumatic stress symptoms and dissociative symptoms, but also disturbances in affective and interpersonal self-regulatory capacities, somatization, and shattered or altered basic beliefs, CPTSD (e.g., Pelcovitz et al., Citation1997; Roth et al., Citation1997) or Disorders of Extreme Stress Not Otherwise Specified (DESNOS; Van der Kolk et al., Citation2005) was introduced.
Some studies have reported an elevated risk of CPTSD symptoms in BPD (Ford, Citation2005) or report difficulties differentiating CPTSD from BPD (McLean & Gallop, Citation2003) and SoD (Spitzer et al., Citation2009). However, no study has systematically examined the association of BPD and SoD, separately and comorbidly, with early childhood trauma exposure, PTSD, and CPTSD symptom severity and syndromal prevalence. It was hypothesized in this study that CPTSD is more frequently displayed in the comorbid BPD+SoD groups compared to all other study groups. According to the results found almost all patients reported experiencing at least one potential traumatizing event. The BPD and BPD+SoD groups, more frequently than the SoD or PC groups, reported each type of traumatizing stressor and exposure in each childhood epoch. CPTSD-positive participants more frequently than those who did not meet criteria for CPTSD reported all types of traumatizing stressors and exposure in all childhood epochs except for developmental epoch 7–12 years. Most SoD and psychiatric comparison group members did not meet criteria for CPTSD, whereas more than one quarter of the BPD and almost half of the BPD+SoD participants met CPTSD criteria. Using the SIDES-rev-NL total and sub-scale scores as dependent variables, an overall between-groups difference was found with large between group effect sizes for all SIDES-rev-NL sub-scales and the total SIDES-rev-NL score. The BPD and especially BPD+SoD groups reported higher CPTSD scores than the SoD and PC groups. When severity of PTSD symptoms was included in the analysis as a covariate, overall group differences were no longer significant. The multivariate effect for PTSD was statistically significant, however, the univariate effects for diagnostic group remained significant for the total SIDES-rev-NL score and the affect dysregulation and dissociation sub-scores. Using a logistic regression analysis, CPTSD was associated positively with BPD+SoD and inversely with SoD, but not with BPD alone nor with or any trauma history.
Based on the existence of qualitatively different forms of trauma-related dysfunctional regulation Chapter 6 outlines the multi-disciplinary assessment and treatment protocol as implemented in two clinical settings. This protocol originally was developed at the Department of Clinical and Health Psychology, Utrecht University, and was later, in close collaboration with two multi-disciplinary teams from Delta Psychiatric Hospital, Poortugal, and Altrecht Mental Health, Zeist, the Netherlands implemented in daily clinical routine.
General discussion
Support for differentiating dysfunctional under- and overregulation
When combining the results from all the studies included in this thesis, several conclusions can be drawn. The first conclusion that can be drawn is that under- and overregulation of affect proved related but largely different phenomena, as hypothesized (Van Dijke, Ford, et al., Citation2010). Moreover, three different forms of dysfunctional self and affect regulation can be empirically identified: dysfunctional Inhibitory, Excitatory, and combined IE-regulation. However, the support for excitatory and combined IE-regulation is stronger than the support for inhibitory regulation.
Second, there is a wide range of intensity of both positive and negative somatoform and psychoform dissociative phenomena (self-dysregulation) and of under- and overregulation of affect, which were differentially distributed across diagnostic groups (Van Dijke, Van der Hart, et al., Citation2010). While underregulation is moderate to strongly related to positive and negative psychoform and somatoform dissociation, overregulation is weakly related to positive and negative psychoform and somatoform dissociation. However, overregulation of affect and negative psychoform dissociation, commonly occurring in somatoform disorder (SoD), can be understood as inhibitory regulation. And underregulation of affect and positive psychoform dissociation, commonly occurring in BPD, can be understood as excitatory regulation. Combined dysfunctional IE-regulation, commonly occurred in comorbid BPD+SoD. Thus, assessment of positive and negative somatoform and psychoform dissociative symptoms and overregulation and underregulation of affect may have utility in characterizing clinical and phenomenological features of BPD, SoD, and PC.
Third, although no disorder-specific form of dysfunctional affect regulation or dissociation was found, patients diagnosed with BPD and BPD+SoD reported more severely dysfunctional self and affect regulation when compared to SoD and PC patients. When SoD patients reported dysfunctional self and affect regulation, inhibitory regulation was prominently reported, but mostly at subclinical levels. Thus, while clinically significant underregulation and combined dysfunctional IE-regulation were associated, respectively, with BPD and BPD+SoD as hypothesized, dysfunctional affect regulation (specifically overregulation) may be less prominent as a clinical characteristic of SoD than prior studies have suggested (Van Dijke, Ford, et al., Citation2010; Van Dijke, Van der Hart, et al., Citation2010).
The role of childhood trauma-by-primary caregiver and CPTSD
The fourth conclusion based on the findings in these studies is that childhood trauma-by-primary-caretaker is highly prevalent among psychiatric patients, particularly those diagnosed with BPD, and that childhood trauma-by-primary-caretaker is differentially associated with under- and overregulation of affect depending on the type and developmental epoch of the traumatization (Van Dijke et al., Citation2011). Trauma involving violations of bodily integrity was associated with more severe overregulation of affect independently of in which developmental epoch this caregiver-caused trauma occurred. Emotional abuse or neglect by caregivers was associated with more severe underregulation of affect when this caregiver-caused trauma occurred in early childhood (ages 0–6 years of age; lack of appreciation of the Self). Thus, childhood traumatic experiences with primary caregivers may play a role in both over- and underregulation of affect in psychiatrically-impaired adults.
The fifth conclusion that can be drawn is that CPTSD (Bermond, Moormann, Albach, & Van Dijke, Citation2008) can be distinguished from BPD and/or SoD (Van Dijke et al., Citation2012). Almost a quarter of all participating patients met criteria for CPTSD (Van Dijke & Van der Hart, Citation2002). Symptoms of CPTSD were significantly and differentially distributed across diagnostic groups. Patients diagnosed with comorbid BPD+SoD most frequently met criteria for CPTSD, while also reporting the most extensive trauma histories. BPD and BPD+SoD patients reported similar CPTSD symptoms, except for subscale “alterations in one's system of meaning,” where BPD patients report the highest mean score, and subscale “total somatic complaints,” where BPD+SoD patients report the highest mean score. Thus, although a prior report with a smaller clinical sample of women diagnosed with BPD reported that CPTSD was present in all cases (McLean & Gallop, Citation2003), by including patients of both genders and other diagnoses as well as BPD, the present study demonstrated that CPTSD is not exclusively or always found with (and therefore not synonymous with) BPD.
For a subsample of patients meeting diagnostic criteria for comorbid PTSD, interestingly, overregulation of affect was significantly related to PTSD-symptom severity, but no significant associations for underregulation of affect, developmental epochs or trauma-by-primary-caretaker with PTSD-symptoms severity were found. Thus, based upon different patterns of affect dysregulation, it appears that CPTSD may be differentiated from PTSD, as well as from BPD and SoD.
Taken all together, the results of this study suggest that further clinical and research studies are needed in order to further the development of empirically-based clinical assessment and treatment protocols for trauma-related self and affect dysregulation in adults with a range of Axis I and II psychiatric disorders. Disorder-specific assessment and treatment methods and guidelines for SoD and severe affective, anxiety, and psychotic disorders, and for BPD thus may be enhanced by the addition of approaches focused on the types of dysfunctional affect- and self-regulation that were identified and examined in the present studies.
Study limitations
A primary limitation of the study is that dysfunctional affect regulation, dissociation, CPTSD, PTSD, and trauma history were all assessed using self-reports. Self-reports, especially retrospectively self-reported types and times of exposure to potentially traumatizing events and CPTSD symptoms, may be inaccurate due to the potential influence of current symptom severity. In this thesis, to overcome this limitation, trauma histories were checked with close-relatives with patients consent. However, a longitudinal study following children with objectivated childhood trauma, could contribute to the furthering of our understanding and knowledge of developmental pathways to dysfunctional regulation and the development of mental disorders across the lifespan. Other data sources such as collateral (e.g., family member) reports, psycho-physiological measures, imaging methods, or biological markers may contribute to the furthering of understanding dysfunctional regulation in psychiatric patients.
When using self-report measures it may be that the diminished capacity to self-reflect (often observed in psychiatric patients) resulted in decreased scores on and interrelations within inhibitory regulation (overregulation and negative dissociative experiences). In particular, at the beginning of treatment patients diagnosed with SoD or BPD+SoD often have impairments in self-reflection and tend to attribute psychological distress to physical complaints. Therefore, clinical observations, hetero-anamnesis/family reports, or (semi) structured interviews that assess all presentations of dysfunctional regulation (both affect dysregulation and dissociation) could provide complementary information on inhibitory regulation.
One in five of the BPD and BPD+SoD patients reported both clinically significant psychoform and somatoform dissociation and may have had a comorbid dissociative disorder (Nijenhuis, Citation2004). The addition of a structured clinical diagnostic interview for the DSM-IV dissociative disorders, which was not included in the study in order to minimize participant burden, could be informative for the BPD and BPD+SoD patients who reported both clinically significant psychoform and somatoform dissociation to objectivate whether these patients have reports of dissociation that also meet criteria for a dissociative disorder. In the future, the option of assessing for dissociative disorders should be included in the protocol.
Implications for clinical practice
Although all patients reported some symptoms of dysfunctional regulation, clinical levels of under- and overregulation of affect, psychoform and somatoform dissociation were not present in all BPD or SoD patients. Therefore, it is of practical relevance to assess presence, nature and severity of dysfunctional affect and self-regulation in BPD and/or SoD patients. Less than one in three patients reports experiencing IE-regulation, suggesting that this form of dysfunctional regulation does occur but is not typical in patients with BPD and/ or SoD. However, in order to self-report symptoms of dysfunctional regulation such as inhibitory regulation, patients must be aware of their psychological burden and be somewhat “psychologically minded.” When dysfunctional regulation is apparently not present, patients (e.g., SoD patients) may be mainly bodily focused or present with a cognitive style described as “operative thinking.” Thus, clinicians and researchers should be alert for signs of the patient's unawareness of inhibitory regulation. Multi-informants reports, non-verbal assessment, or projective assessment techniques may be useful aids to assess inhibitory regulation.
Comorbid SoD in BPD patients or comorbid BPD in SoD patients seems to represent more complex symptom presentations than just comorbidity of two mental disorders. In addition to meeting diagnostic criteria for both mental disorders, these patients also reported more and differential dysfunctional regulation symptoms, more extensive trauma histories, and more often met criteria for CPTSD. Based on the main findings of this thesis, it seems warranted to thoroughly assess dysfunctional regulation, CPTSD-symptoms, and dissociative disorders when patients are characterized by BPD+SoD comorbidity. Treatment guidelines are needed for the large sub-group of such individuals with severe comorbidity who have experienced trauma-by-primary-caretaker and present with complex traumatic stress symptoms in addition to the symptoms of BPD and SoD (Courtois & Ford, Citation2009).
Also, for PTSD and CPTSD patients reporting difficulties with addressing and analyzing emotions or “mentalizing emotions” and negative dissociative symptoms (Fonagy, Gergely, Jurist, & Target, Citation2002), inhibitory regulation seem to have been overlooked and may be of particular importance in the assessment and treatment of chronic childhood trauma-related pathology such as comorbid BPD+SoD or CPTSD (Ford, Citation2005; Lanius et al., Citation2010; Lanius, Frewen, Vermetten, & Yehuda, Citation2011).
Approaches to dysfunctional regulation have been developed for patients with severe mental disorders (adults; Wolfsdorf & Zlotnick, Citation2001; youth; Ford & Russo, Citation2006; Ford, Hawke, Alessi, Ledgerwood, & Petry, Citation2007; McCullough, Kuhn, Andrews, Kaplan, Wolf, & Hurley, Citation2003), including Dialectical Behavior Therapy (Linehan et al., Citation2006), Transference Focused Psychotherapy (Levy et al., Citation2006), and Mentalization Based Treatment (Bateman & Fonagy, Citation2008). However, these treatments address underregulation of affect more explicitly than overregulation of affect. For BPD patients, especially when also diagnosed with comorbid SoD or clinically significant somatoform symptoms, as well as for PTSD, and CPTSD patients, the main findings of this thesis warrant additive assessment and treatment of overregulation of affect and negative dissociative symptoms e.g., as was outlined in the clinical assessment and treatment of trauma-related self and affect dysregulation. For patients who report inhibitory regulation therapy forms like sensory-motor therapy (Ogden, Minton, & Pain, Citation2006), accelerated experiential-dynamic psychotherapy (Fosha, Citation2003; Fosha, Paivio, Gleiser, & Ford, Citation2009), emotion-focused therapy for trauma (Greenberg & Bolger, Citation2001; Paivio & Pascual-Leone, Citation2010), and Attachment, Self-Regulation, and Competency (ARC; Kinniburgh, Blaustein, Spinazzola, & Van der Kolk, Citation2005) could contribute to the experiential process of emotional awareness and emotional growth. Even a more technical-emotional approach, such as facial affect recognition skills training (Ekman, Citation2003), or virtual-reality social-emotional skills training and perspective taking (Blakemore, Citation2010), neurofeedback and (emotional) regulation exercises like yoga (Van der Kolk, Citation2006), could facilitate functional regulation and enhance therapy process and progress.
Implications for research
Based on the main findings of the thesis, further research regarding the differentiation of dysfunctional regulation is warranted. However, no specific measure (e.g., interview, self- or hetero-report, task) is yet available that assess both inhibitory and excitatory regulation across several domains of functioning including affective, cognitive, somatic, relational, reflective, executive, behavioral, and psycho-physiological functioning. In future such a clinical instrument and/or battery of associated neuro-psychological-tasks should be developed and validated.
Also, focusing on biological and psycho-physiological aspects of regulation and dysregulation was not included in the scope of the thesis but in future should embrace the differentiation of dysfunctional regulation (see ). Lanius et al. (Citation2010; Citation2011) in their recent neuro-imaging study found support for the presence of under- and overregulation in PTSD patients. However, in contrast to differentiating positive and negative psychoform and somatoform dissociative symptoms in this thesis, they did not and concluded that overregulation was dissociative, thereby acknowledging only negative dissociative phenomena to be dissociative. Intrusive PTSD symptoms that some authors regard as positive dissociative symptoms (e.g., Van der Hart et al., Citation2006; also the DSM-IV speaks of “dissociative flashback episodes” as one of PTSD's symptoms; APA, Citation2004) were believed not to be dissociative but merely PTSD-criteria. Furthermore, they proposed the dissociative sub-type of PTSD. However, based on the main findings of this thesis, it may be concluded that although under- and overregulation are related to psychoform and somatoform dissociative symptoms, they are largely different kinds/types of phenomena. Also, based on this dissertations main findings it may be concluded that dissociation does not just pertain to negative dissociative symptoms, but also to positive dissociative symptoms. It may well be that Lanius and colleagues over-generalized the findings to be dissociative. Future imaging research should include differentiating dysfunctional regulation across several domains of functioning including affective, cognitive, somatic, relational, reflective, executive, behavioral, and psycho-physiological functioning.
Based on the main findings of this study, it may be concluded that three qualitatively different forms of dysfunctional regulation do exist. Patients are able to distinguish between under- and overregulation of affect as well as positive and negative psychoform and somatoform dissociative symptoms. However, neither the interview (SIDES) nor the self-report for CPTSD (SIDES-SR) incorporated this differentiation for inhibitory and excitatory regulation. Recently, an interview for Developmental Trauma Disorder (DTD; Van der Kolk, Citation2005) for children and adults has been developed (Ford, personal communication, Citation2011). Consistent with the findings of this study, this interview does incorporate symptoms that differentiate inhibitory and excitatory regulation as well as psychoform and somatoform dissociation. Therefore, future research should focus on tests of criterion and convergent and discriminant validity of the interview in relation to children's self-reported, and parent-, teacher-, and observer-rated inhibitory, excitatory, and combined IE-regulation. Based on the results of those studies and the main findings from this thesis, adaptation of the adult CPTSD interview and self-report measures should be considered to systematically incorporate the assessment of the different forms of affect and self-regulation.
Conclusion
Finally, when returning to and the aims of the thesis, we can conclude based upon the main findings of this thesis and related performed studies that support was found for the existence of inhibitory-, excitatory- and combined IE-regulation operating in vicious cycles. Dysfunctional inhibitory, excitatory, and combined IE-regulation in patients diagnosed with BPD, SoD, comorbid BPD+SoD and PC was found across several domains of functioning, i.e., affective, cognitive, somatic, relational, and executive functioning.
Dysfunctional regulation seems related to trauma-by-primary-caretaker: Inhibitory regulation is associated with physical trauma, and excitatory regulation is associated with emotional trauma especially when first occurring in the developmental epoch, 0–6 years of age. CPTSD is common in patients diagnosed with mental disorders, especially when diagnosed with BPD-alone or comorbid with SoD. CPTSD can be differentiated from BPD and BPD+SOD, as well as PTSD.
Thus, the development of a tailor-made assessment and treatment protocol is warranted for patients with treatment-as-usual-resistant complex symptom presentation reporting potentially traumatizing events by-primary-caregiver as outlined in the clinical assessment and treatment of trauma-related dysfunctional self- and affect regulation.
Conflict of interest and funding
There is no conflict of interest in the present study for the author.
French abstract
Download PDF (78.8 KB)Russian abstract
Download PDF (135 KB)Spanish abstract
Download PDF (21.7 KB)Turkish abstract
Download PDF (70.7 KB)Polish abstract
Download PDF (126.1 KB)Notes
Mentors: Prof. Dr. M.J.M. van Son, Prof. Dr. O. van der Hart (Utrecht University, Department of Psychology) and Prof. Dr. P.G.M. van der Heijden (Utrecht University, Department of Methodology and Statistics). Theses defended in Utrecht University, Faculty of Social Sciences, June 10, 2011. For the abstract or full text in other languages, please see Supplementary files under Reading Tools online. (Published: 13 September 2012)
References
- Allen J. G, Fonagy P. Handbook of mentalization-based treatment. 2006; Chichester, UK: Wiley.
- APA (American Psychiatric Association) (APA). Diagnostic and statistical manual of mental disorders. 2004; IV-TR ed, Washington, DC: Author.
- Bateman A, Fonagy P. Eight-year follow-up of patients treated for borderline personality disorder: Mentalization-based treatment versus treatment as usual. American Journal of Psychiatry. 2008; 165: 631–638.
- Bermond B, Moormann P. P, Albach F, Van Dijke A. Impact of severe childhood sexual abuse on the development of alexithymia in adulthood. Psychotherapy and Psychosomatics. 2008; 77: 260–262.
- Blakemore S. J. The developing social brain: Implications for education. Neuron. 2010; 65: 744–747.
- Bowlby J. A secure base: Clinical applications of attachment theory. 1988; London: Routledge.
- Bradley S. J. Affect dysregulation and the development of psychopathology. 2000; New York: The Guilford Press.
- Briquet P. Traité Clinique et thérapeutique de l'hystérie. 1859; Paris: J.-B. Baillière et fils.
- Cloitre M, Stolbach B. C, Herman J. L, Kolk B. V, Pynoos R, Wang J, etal. A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress. 2009; 22: 399–408.
- Courtois C. A, Ford J. D. Treating complex traumatic stress disorders: An evidence-based guide. 2009; New York: Guilford Press.
- Cozolino L. The neuroscience of human relationships: Attachment and the developing social brain. 2006; New York: Norton.
- Ekman P. Emotions revealed. Recognizing face and feelings to improve communication and emotional life. 2003; New York: Times Books Henry Bolt and Company.
- Fonagy P, Gergely G, Jurist E, Target M. Affect regulation, mentalization and the development of the self. 2002; New York: The Other Press.
- Ford J. D. Treatment implications of altered neurobiology, affect regulation and information processing following child maltreatment. Psychiatric Annals. 2005; 35: 410–419.
- Ford J. D, Hawke J, Alessi S, Ledgerwood D, Petry N. Psychological trauma and PTSD symptoms as predictors of substance dependence treatment outcomes. Behaviour Research and Therapy. 2007; 45: 2417–2431.
- Ford J. D, Kidd P. Early childhood trauma and disorders of extreme stress as predictors of treatment outcome with chronic posttraumatic stress disorder. Journal of Traumatic Stress. 1998; 11: 743–761.
- Ford J. D, Russo E. Trauma-focused, present-centered, emotional self-regulation approach to integrated treatment for post-traumatic stress and addiction: TARGET. American Journal of Psychotherapy. 2006; 60: 335–355.
- Fosha D, Siegel D. J, Solomon M. F. Dyadic regulation and experiential work with emotion and relatedness in trauma and disordered attachment. Healing trauma: Attachment, trauma, the brain and the mind. 2003; New York: Norton. 221–281.
- Fosha D, Paivio S. C, Gleiser K, Ford J. D, Courtois C. A, Ford J. D. Experiential and emotion-focused therapy. Treating complex traumatic stress disorders: An evidence-based guide. 2009; New York: Guilford Press. 286–311.
- Greenberg L, Borger L. An emotion-focused approach to the over-regulation of emotion and emotional pain. Journal of Clinical Psychology. 2001; 57: 197–211.
- Kinniburgh K, Blaustein M, Spinazzola J, Van der Kolk B. Attachment, self-regulation & competency. Psychiatric Annals. 2005; 5: 424–430.
- Lanius R. A, Frewen P. A, Vermetten E, Yehuda R. Fear conditioning and early life vulnerabilities: Two distinct pathways of emotional dysregulation and brain dysfunction in PTSD. European Journal of Psychotraumatology. 2011; 1 5467, doi: http://dx.doi.org/10.3402/ejpt.v1i0.5467.
- Lanius R. A, Vermetten E, Loewenstein R. J, Brand B, Schmalhl C, Bremner J. D, etal. Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissocative subtype. American Journal of Psychiatry. 2010; 167: 640–647.
- Levy K. N, Meehan K. B, Kelly K. M, Reynoso J. S, Weber M, Clarkin J. F, etal. Change in attachment patterns and reflective function in a randomized control trial of transference-focused psychotherapy for borderline personality disorder. Journal of Consulting and Clinical Psychology. 2006; 74: 1027–1040.
- Linehan M. M. Cognitive-behavioral treatment of borderline personality disorder. 1993; New York: Guilford Press.
- Linehan M. M, Comtois K. A, Murray A. M, Brown M. Z, Gallop R. J, Heard H. L, etal. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs. therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry. 2006; 63: 757–766.
- Lyons-Ruth K, Dutra L, Schuder M. R, Bianchi I. From infant attachment disorganization to adult dissociation: Relational adaptations or traumatic experiences?. Psychiatric Clinics of North America. 2006; 29: 63–86.
- McCullough L, Kuhn N, Andrews S, Kaplan A, Wolf J, Hurley C.L. Treating affect phobia: A manual for short-term dynamic psychotherapy. 2003; New York: Guilford Press.
- McLean L. M, Gallop R. Implications of childhood sexual abuse for adult borderline personality disorder and complex posttraumatic stress disorder. American Journal of Psychiatry. 2003; 160: 369–371.
- Mikulincer M, Shaver P. R, Rholes W. S, Simpson J. A. Security-based self-representations in adulthood: Contents and processes. Adult attachment: Theory, research, and clinical implications. 2004; New York: Guilford Press. 159–195.
- Mikulincer M, Shaver P. R, Pereg D. Attachment theory and affect regulation: The dynamics, development, and cognitive consequences of attachment-related strategies. Motivation and Emotion. 2003; 27: 77–102.
- Nijenhuis E. R. S. Somatoform dissociation: Phenomena, measurement, and theoretical issues. 2004; New York: Norton.
- Nyklíček I, Temoshok L, Vingerhoets A. Emotional expression and health: Advances in theory, assessment and clinical applications. 2004; New York: Brunner-Routledge.
- Ogden P, Minton K, Pain C. Trauma and the body: A neurobiologically-informed approach to clinical practice. 2006; New York: Norton.
- Paivio S. C, Pascual-Leone A. Emotion focused therapy for complex trauma: An integrative approach. 2010; Washington, DC: American Psychological Association.
- Pelcovitz D, Van der Kolk B, Roth S, Mandel F, Resick P. Development of a criteria set and a Structured Interview for Disorders of Extreme Stress (SIDES). Journal of Traumatic Stress. 1997; 10: 3–16.
- Roelofs K, Keijsers G. P. J, Hoogduin K. A. L, Näring G. W. B, Moene F. C. Chilhood abuse in patients with conversion disorder. American Journal of Psychiatry. 2002; 159: 1908–1913.
- Roth S, Newman E, Pelcovitz D, Van der Kolk B, Mandel F. S. Complex PTSD in victims exposed to sexual and physical abuse: Results from the DSM-IV field trial for posttraumatic stress disorder. Journal of Traumatic Stress. 1997; 10: 539–555.
- Şar V. Developmental trauma, complex PTSD, and the current proposal of DSM-5. European Journal of Psychotraumatology. 2011; 2 5622, doi: http://dx.doi.org/10.3402/ejpt.v2i0.5622.
- Silbersweig D, Clarkin J. F, Goldstein M, Kernberg O. F, Tuescher O, Levy K. N, etal. Failure of frontolimbic inhibitory function in the context of negative emotion in borderline personality disorder. American Journal of Psychiatry. 2007; 164: 1832–1841.
- Spitzer C, Barnow S, Wingenfeld K, Rose M, Lowe B, Grabe H. J. Complex post-traumatic stress disorder in patients with somatization disorder. Australian and New Zealand Journal of Psychiatry. 2009; 43: 80–86.
- Van der Hart O, Nijenhuis E. R. S, Steele K. The haunted self: Structural dissociation and the treatment of chronic traumatization. 2006; New York: Norton.
- Van der Hart O, Van Dijke A, Van Son M. J. M, Steele K. Somatoform dissociation in traumatized World War I combat soldiers: A neglected clinical heritage. Journal of Trauma and Dissociation. 2000; 1: 33–66.
- Van der Kolk B. A. Developmental trauma disorder: Toward a rational diagnosis for children with complex trauma histories. Psychiatric Annals. 2005; 35: 401–408.
- Van der Kolk B. A. Clinical implications of neuroscience research for the treatment of PTSD. Annals New York Academy of Sciences. 2006; 1071: 1–17.
- Van der Kolk B. A, Roth S, Pelcovitz D, Sunday S, Spinazzola J. Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma. Journal of Traumatic Stress. 2005; 18: 389–399.
- Van Dijke A, Vingerhoets A, Nyklicek I, Denollet J. The clinical assessment and treatment of trauma-related self-and affect dysregulation. Emotion regulation: Conceptual and clinical issues. 2008; New York: Springer. 150–169.
- Van Dijke A, Ford J. D, Van der Hart O, Van Son M. J. M, Van der Heijden P. G. M, Bűhring M. Affect dysregulation in borderline personality disorder and somatoform disorder: Differentiating under- and over-regulation. Journal of Personality Disorders. 2010; 24: 296–311.
- Van Dijke A, Ford J. D, Van der Hart O, Van Son M. J. M, Van der Heijden P. G. M, Bűhring M. Childhood traumatization by primary caretaker and affect dysregulation in patients with borderline personality disorder and/or somatoform disorder. European Journal of Psychotraumatology. 2011; 2 5628, doi: http://dx.doi.org/10.3402/ejpt.v2i0.5628.
- Van Dijke A, Ford J. D, Van der Hart O, Van Son M. J. M, Van der Heijden P. G. M, Bűhring M. Complex posttraumatic stress disorder in patients with borderline personality disorder and somatoform disorders. Psychological Trauma: Theory, Research, Practice, and Policy. 2012; 2: 162–168.
- Van Dijke A, Van der Hart O. The Dutch self-report version of the Structured Interview for Disorders of Extreme Stress (SIDES-r-nl). 2002; Unpublished manual: Utrecht University.
- Van Dijke A, Van der Hart O, Ford J. D, Van Son M, Van der Heijden P, Bűhring M. Affect dysregulation and dissociation in borderline personality disorder and somatoform disorder: Differentiating inhibitory and excitatory experiencing states. Journal of Trauma and Dissociation. 2010; 11: 424–443.
- Van Harmelen A. L, De Jong P. J, Glashouwer K. A, Spinhoven P, Penninx B. W, Elzinga B. M. Child abuse and negative explicit and automatic self-associations: The cognitive scars of emotional maltreatment. Behaviour Research and Therapy. 2010; 48: 486–494.
- Waller E, Scheidt C. E. Somatoform disorders as disorders of affect regulation: A development perspective. International Review of Psychiatry. 2006; 18: 13–24.
- Wolfsdorf B. A, Zlotnick C. Affect management in group therapy for women with post traumatic stress disorder and histories of childhood sexual abuse. Journal of Clinical Psychology. 2001; 15: 60–71.